Ivan Drozdov 05/07/2019 0 Comments
Frontal epilepsy is a form of the disease in which the epileptogenic focus is concentrated in the frontal lobes of the brain. The disease can manifest itself at any age and regardless of gender. In terms of prevalence, frontal epilepsy ranks second after temporal lobe epilepsy. Of all cases of focal epilepsy, this type of disease occurs in 22% of patients. In 60% of cases, frontal epilepsy is symptomatic – it appears as a result of the development of other pathologies in the brain tissue. One of the main features of frontal lobe epilepsy attacks is their predominant occurrence at night.
Definition
What is cryptogenic epilepsy? This is a form of the disease, in addition to idiopathic and symptomatic, characterized by a syndrome of recurrent epileptic seizures. In this case, it is possible to identify the pathological focus, but not the cause of its occurrence.
Experts distinguish three stages of the disease:
- initial, which is characterized by convulsive seizures;
- sluggish - mental disorders of an unstable nature;
- destructive - there is a decrease in intellectual activity.
There are two types of epilepsy: temporal lobe and multifocal. Seizures are accompanied by disruption of neural connections, as a result of which brain cells die, development slows down and professional skills are lost.
Cryptogenic generalized epilepsy leads to impaired functionality of the speech apparatus, and manifestations of personality degradation are possible. Often this diagnosis is made in view of the fact that the study continues until the final and objective conclusions of specialists.
Forms of epilepsy
The etiology and clinical picture of epilepsy is heterogeneous. Highlight:
Idiopathic form . This is a hereditary variant of the disease. The patients do not have any deviations in their neurological status, and no pathological changes in the brain are detected during laboratory and instrumental research methods, however, periodically manifested epileptic paroxysms are present.
Symptomatic form . In this case, epilepsy is the clinical expression of one or another acquired brain disease. Seizures can occur as a result of a stroke, head injury, acute neuroinfection, or brain tumors. When examined by a neurologist, patients exhibit focal neurological symptoms, which makes it possible to confirm the presence of a pathological focus in the brain. Diagnostic clinical and laboratory procedures also confirm the diagnosis.
Cryptogenic form of epilepsy . It develops due to unknown reasons. This is the most controversial variant of the disease. This diagnosis is made when epilepsy cannot be classified as either idiopathic or symptomatic forms. A neurological examination provides an indication of the presence of organic manifestations of the disease. Along with this, neuroimaging does not find pathological changes in the brain. However, when recording electroencephalography, local epileptic activity is detected.
In another way, cryptogenic epilepsy is also called probably symptomatic , suggesting that with a higher level of technical capabilities of neuroimaging, the pathological focus can be found, and most cryptogenic forms will be transferred to the category of symptomatic. Therefore, the diagnosis of cryptogenic epilepsy should be considered preliminary, requiring further search for an unknown etiology.
Cryptogenic epilepsy is often accompanied by a sharp decrease in intelligence, so that it is sometimes classified as a mental illness. Cryptogenic epilepsy is characterized by fairly high resistance to anticonvulsant therapy.
Causes of the disease
There are several factors that influence the occurrence of abnormalities associated with cryptogenic epilepsy. What it is - an independent illness or a consequence of pathology - is determined by the types of observed manifestations.
Types of disease (code in the range G40.0-G40.9):
- Symptomatic (secondary). Causes: brain hemorrhages, tumors, central nervous system infection, developmental deviation, cyst, use of illegal substances, alcoholism.
- Idiopathic - occurs due to a hereditary predisposition and manifests itself at an early age. In this case, there is high neuronal activity, but there is no brain damage.
- Cryptogenic - develops in the absence of visible causes, and may remain undetected even after many examinations.
It is currently unknown how disruptions in brain activity occur. Cryptogenic epilepsy (ICD-10 code G40) has been common since ancient times among both children and adults.
Among boys, the most common age range is from 2 to 12 years with the disease of the “rolandic” type, which affects 60% of patients. In some cases, unspecified cryptogenic epilepsy is diagnosed (according to ICD-10, this is G40.9).
Cryptogenic epilepsy: how does the focal form differ from the generalized one?
Cryptogenic epilepsy is a psychoneurological pathology characterized by convulsive seizures. This is one of the common types of epilepsy, whose nature still remains unknown.
The disease manifests itself both in childhood and in old age, but most often manifests itself before the age of 20. When it lasts for a long time, it leads to personality metamorphoses called “epileptic dementia.”
Although the disease often leads to disability, favorable prognosis is not uncommon.
General characteristics of the pathology
As already mentioned, the diagnosis of cryptogenic epilepsy is established when it is impossible to identify the causes of this chronic neuropsychiatric disease.
During the acute period, the disease is accompanied by epileptic seizures (convulsions, muscle cramps), during which short-term loss of consciousness, as well as mental and autonomic disorders, are possible.
As the disease progresses, the patient's personality may change.
But to better understand the essence of the disease, it is necessary to consider the mechanism of its development. Epilepsy seizures occur due to increased activity of the brain in certain areas. Against the background of sudden impulses emanating from the source of pathology, the excitability of the nervous system increases, which is why convulsive muscle contractions begin and failure occurs in other processes of the body.
After an attack, complete amnesia sets in: the patient does not remember the events that occurred during the attack. It is also worth noting that a distinctive feature of cryptogenic epilepsy is that when examining a patient, it is impossible to identify the exact location of the pathology in the brain.
Causes of pathology
This type of epilepsy is a disease with implicit and uncertain causes.
This diagnosis is established in cases where the symptoms of the disease do not fit other types of pathology or the cause of the development of the pathology remains a mystery even after all kinds of research.
That is, experts still do not know exactly what cryptogenic epilepsy is and where it comes from.
Possible factors for the occurrence of the disease are:
- ischemia and stroke;
- tumor formations;
- genetic predisposition;
- serious mechanical head injuries;
- consequences of toxic substances.
Also, the appearance of a disease in a person can be influenced by viral infections, heart, kidney and liver diseases, sudden exposure to intense (flashing) light, sharp sound, and also due to temperature changes. In addition, in other forms of epilepsy, a focus of pathological activity usually appears in the cerebral cortex, but in the cryptogenic type it is not detected.
Kinds
In medical sources you can find a division of cryptogenic epilepsy into two types:
- focal;
- generalized.
Cryptogenic focal epilepsy is characterized by a more pronounced picture. In this type of epilepsy, the focus of electrical activity is often localized in the temporal lobe of the brain. Cryptogenic generalized epilepsy is characterized by a variable clinical picture and the presence of a huge number of pathological foci in the brain.
Focal epilepsy
As already mentioned, cryptogenic focal epilepsy has a limited scope for the manifestation of an active pathological focus.
However, there have been cases of transformation or replacement of focal epileptic seizures with paroxysmal generalized ones.
What the manifestations of a focal epileptic seizure will be will depend entirely on the localization of the focus of pathology in the cerebral cortex. So, with electrical activity:
- in pyramidal neurons – sudden motor activity is noted;
- if sensory organs are affected, hallucinations of various types appear (auditory, visual, tactile);
- in the occipital region - the patient sees non-existent things or people;
- with damage to the temporal zone - auditory hallucinations;
- in the sagittal region or the hook of the ammon's horn - gustatory and olfactory illusions;
- if the parietal region is affected - sensory type seizures (paresthesia).
Emotional polarity is a sign of focal epilepsy
Common signs of this type of epilepsy will be viscosity of thinking, impulsiveness and emotional polarity. Melancholy or, conversely, anxiety, hypochondria and intellectual degradation may also be noted.
Generalized epilepsy
This type of pathology is diagnosed mainly in children and is accompanied by polymorphism of seizures and atypical EEG changes. Another feature of the pathology is resistance to the drugs used. The pathology is diagnosed in 3-7% of cases of epilepsy and affects mainly boys.
In terms of manifestation, the following picture is noted: unexpressed convulsions are transformed into tonic seizures, which, without a latent period, gradually turn into a syndromic complex. In addition, this type of epilepsy is characterized by the following triad: paroxysms of falls, tonic-characterized seizures and abnormal absences (freezes).
Forms of the disease
Cryptogenic epilepsy is characterized by division into certain forms (syndromes). As a rule, they appear in children. Thus, West syndrome appears in babies 2-4 months old, and at the age of 1 year it can transform into another form of the disease. This syndrome is characterized by unexpectedly beginning and also suddenly ending seizures.
In children 2-4 months old, cryptogenic epilepsy manifests itself in the form of sudden seizures
Lenox-Gastaut syndrome is diagnosed in children 2-8 years old and manifests itself as a short-term imbalance or deafness. The child is conscious, but such episodes are also fraught with injury. This form of the disease, like the previous one, is accompanied by mental retardation.
Myclonic-astatic syndrome is found in children with generalized seizures from 5 to 12 months, from the moment the baby begins to walk. It manifests itself as episodic loss of balance. Other forms of cryptogenic epilepsy are similar to the classic course of the disease and have the same subtypes.
Clinical manifestations
The symptom complex goes through three successive stages:
- suddenly appearing convulsive seizures;
- mental breakdowns, unstable nature;
- destruction of the intellect and destruction of the patient’s personality.
The epileptic attack itself has the following symptoms.
- Motor. Unpleasant sensations in the body, uncontrolled running and shouting are possible.
- Autonomic, sensitive and mental disorders. Unjustified fear, visual flashes, and hallucinations appear.
- Neurological symptoms. Muscle tone decreases, problems with speech appear (delay and underdevelopment in children, degradation in adults), confusion and drowsiness.
In addition to everything, during an epileptic seizure there is complete apathy, often loss of consciousness, states of passion, accompanied by neurological breakdowns. The attack is often preceded by insomnia, tachycardia, the so-called aura state and hallucinations.
After the attack, the pressure drops, the pulse and breathing return to normal. This is followed by complete relaxation of the body and deep sleep. After waking up, a person may experience a headache, fatigue and impaired eye contact.
Features of the manifestation of pathology in childhood
Cryptogenic epilepsy in children often occurs due to congenital pathology or due to intrauterine infection. Experts do not exclude the possibility of developing pathology due to injuries received at birth. As a rule, children are diagnosed with focal epilepsy. Much less often, in the first years of life, symptoms of West or Lenox-Gastaut syndrome are detected.
The first form of the disease is diagnosed in 2% of patients and is most often found in male infants 4-6 months old. The syndrome is characterized by myoclonic convulsions, which over time transform into clonic or tonic. Attacks often occur before or after sleep. Without timely treatment, West syndrome develops into other forms.
Quite often, after children reach the age of 3 years, Lenox-Gastaut syndrome (a generalized type of epilepsy) appears instead of West syndrome. It is found in 5% of patients.
Seizures begin with involuntary twitching of the limbs, after which absence seizures (short blackouts) occur, during which muscle tone sharply drops.
In rare cases (up to 20%), the syndrome is treatable.
Prevention
If we talk about preventive measures against epilepsy, they mainly come down to avoiding the factors of its possible occurrence:
- birth, traumatic brain injury;
- infectious diseases of the brain;
- alcohol abuse.
Genetic consultations also play a significant role in prevention.
As for the prevention of attacks, Avicena also noted the positive effect of physical activity (walking, running) and various types of work on patients.
In addition, it is important for such patients to pay attention to their diet: it is optimal to adhere to a dairy-vegetable diet, reducing the consumption of proteins, spicy, strong tea and coffee, and completely eliminating alcohol.
Source: https://NervovNet.com/kriptogennaya-epilepsiya-u-detej-i-vzroslyh-01/
General signs
How does the disease manifest itself symptomatically, what is cryptogenic epilepsy? This is a disease whose manifestations do not look the same for everyone. Thus, during a seizure, infants tilt their head or upper body; in adolescents, muscle twitching occurs; in some patients, so-called automatisms are observed, during which a person performs some actions, but then absolutely does not remember what he did.
Over time, patients develop epileptic personality traits. They are prone to frequent mood swings and can be both condescending and irritable towards others. Cryptogenic epilepsy in children is characterized by pedantry, but it is not easy for them to switch from one topic to another.
Often, disturbances in mental, autonomic, sensory, and motor functions are combined with severe speech impairment and decreased muscle tone. Sometimes cryptogenic epilepsy in adults manifests itself as a feeling of severe fatigue, after which problems with attention and mental perception begin. Apathy, dizziness, loss of consciousness, affective disorder, neurological pathologies, psychosis - among other symptoms.
A prolonged attack is preceded by stages of sleep disturbance, migraine, tachycardia, and hallucinations. Against the background of these symptoms, the patient may experience increased physical activity, as well as fear for his own life after the condition. Attacks may occur during night sleep.
Cryptogenic epilepsy. Focal generalized epilepsy in children
Focal cryptogenic epilepsy is a psychoneurological pathology that is rarely accompanied by generalized convulsive seizures, since the area of neuronal excitation (focus) is limited to one hemisphere.
Due to the nature of the disease, seizures are difficult to correct without treating the pathology that caused them.
- consequences of toxic substances;
- viral infections, in particular herpetic encephalitis;
- brain tumors;
- head injuries, even those received in the long term;
- sudden changes in temperature;
- problems during pregnancy (antenatal).
As a rule, the anamnesis of people who are diagnosed with this disease reveals more than one reason for the occurrence of epiactivity.
Finding and eliminating the source of the disease is difficult, which rules out surgery as a treatment option for seizures.
Depending on the location and number of lesions in the cerebral cortex, the scientific literature describes two types of cryptogenic epilepsy: focal and generalized.
Focal
The peculiarity of this type of disease is the clear localization of the place of negative impulses (focus).
Based on the characteristics of the manifestations and symptoms, we can assume the probable localization of the pathological focus:
- in the occipital region - clear visions of non-existent people and objects arise;
- in the temporal part – the patient is haunted by auditory hallucinations;
- parietal region – characterized by paresthesia (sensitivity disturbances in one or another part of the body;
- areas of the vegetative nuclei of the brain - sweating, spasms and vasodilatation, visual impairment, digestion;
- pyramidal neurons – uncharacteristic motor activity is observed.
There is also a phenomenon called cryptogenic focal epilepsy with secondary generalization, in which seizures from focal ones are transformed into a generalized form with tonic convulsions of the whole body.
All patients experience a change in the emotional component of their personality. Excessive impulsiveness appears, a tendency to depression appears, and intellectual abilities decrease.
This type of cryptogenic epilepsy is typical for children, and boys are more often affected. In 7% of cases, children are given this diagnosis. The pathology is considered difficult to treat due to the variability of symptoms and resistance to classical drugs.
Small convulsions gradually turn into tonic seizures. Seizures are characterized by a combination of several symptoms: fainting, severe convulsions and absence seizures. Before the main part of the manifestations begins, the child freezes for a short time, completely disconnecting from the world. After he comes to his senses, he does not remember what just happened.
The diagnosis of cryptogenic epilepsy, despite the apparent uncertainty, requires clarification of the localization of the focus of epiactivity: frontal partial version, temporal or other.
The doctor conducts a complete thorough examination, studies the history of life, diseases, and checks the possible causes of convulsive symptoms.
The source of epiactivity is shown by the EEG. And its possible cause is ultrasound, CT, MRI.
After the localization of the focus has been established and organic lesions of the cerebral cortex have been excluded, complex treatment is prescribed. The goal of therapy is not only to slow down the progression of the disease, but also to suppress seizures.
The drug component remains the leading one. The resistance of some forms of the disease to drugs is eliminated thanks to the selection of drugs that can affect the nervous system even with such a diagnosis.
The goal is to get rid of seizures.
Several categories of drugs are used:
You can speed up recovery and achieve tangible positive changes by additionally undergoing the following procedures:
- bioresonance therapy, which allows you to normalize the electromagnetic field, reducing the risk of a seizure;
- vortex fields that normalize the human electromagnetic field;
The duration of treatment for cryptogenic epilepsy in children and adults varies individually and can last several years. In the future, the need to completely repeat the course cannot be ruled out.
This type of seizure syndrome can be cured by eliminating the primary cause that affects the brain.
Preventive measures against epilepsy are quite simple - it is necessary to avoid factors that contribute to its development. When planning a child, consult your doctor and undergo genetic testing.
As for people who have already suffered from seizures, they are recommended to follow simple rules to help prevent new attacks:
- clear daily routine;
- regular physical activity;
- following a special diet;
- absence of severe stress
Cryptogenic focal temporal lobe epilepsy in children has a generally favorable prognosis. This is in the case of timely identification and treatment of the cause of the attacks.
In an advanced stage, without the necessary relief of seizures, the disease impairs intellectual abilities, attention, and concentration. In the worst case scenario, it leads to personality changes that can no longer be reversed.
Particular attention should be paid to the frequency and duration of attacks. The more often and longer they occur, the more irreparable damage is caused to the brain.
If the seizure lasts more than 5 minutes, you must immediately contact an ambulance, as the patient may suffer damage incompatible with life.
Source: https://newneuro.ru/kriptogennaya-epilepsiya/
Types of attacks
Cryptogenic epilepsy is divided into two main groups (according to the source of the resulting discharge). With partial or focal, the temporal or frontal parts of the brain are affected, sometimes the parietal and occipital parts, but consciousness is preserved.
If the limbic system is under the influence of neurons, the person loses the sense of space, and the discharge spreads across the cortex of both hemispheres. This phenomenon is called a secondary generalized attack. Its symptoms are neurological deficits: blindness, speech impediments, Todd's palsy.
Cryptogenic focal epilepsy in children and adults is divided into the following types:
- Simple. With them, seizures pass in the presence of consciousness and with the repetition of one type of reaction. Clinical manifestations include the appearance of seizures, autonomic, sensory and mental disorders.
- Complex. Seizures are characterized by the patient being unconscious. They manifest themselves in various erratic actions, grimacing, etc.
- Secondary generalized ones are characterized by rapid spread of the discharge. The patient is not always aware of the changes before the onset of an attack. Generalized attacks cover the entire cerebral cortex, so a person is characterized by confused thinking and no premonitions of an exacerbation.
The attacks, in turn, are divided as follows:
- Tonic-clonic. They begin spontaneously, without warning, but sometimes they are preceded by malaise and discomfort. The attack begins with tonic muscle tension and screaming, increased blood pressure, increased heart rate, and biting of the tongue. The patient falls and experiences characteristic muscle cramps and profuse salivation. After the acute phase, as a rule, relaxation occurs, but the consciousness remains confused, the patient tends to sleep. Upon awakening, people cannot remember what happened.
- Absence seizures. Characteristic exclusively for childhood and early adolescence. At the same time, the patient freezes with a blank look in one position, sometimes throwing his head back. These attacks do not last long, and often loved ones do not even suspect that the child is ill; only difficulties with concentrating during the learning process can indicate the presence of a problem. Absence seizures also occur in Lennox-Gastaut syndrome.
- Myoclonic. Sudden and fleeting. In this case, an involuntary contraction of the flexor muscles occurs. The cause is a person’s fall, sometimes these symptoms are accompanied by other conditions: ischemia, Creutzfeldt-Jakob disease, etc.
- Tonic, atonic. In the latter case, the patient falls due to the sudden disappearance of postural muscle tone. And with tonic, there is an increase in tone and rigidity, causing the patient to fall backwards.
With cryptogenic temporal lobe epilepsy, paroxysms that do not fit any of the above descriptions can also be observed. In medicine they are called unclassifiable.
What types of seizures are there?
If a person has cryptogenic epilepsy, then different types of seizures may occur. Which one a particular person will have directly depends on the area of brain damage . That is why it is difficult to say unambiguously what kind of attack a person will have to face.
It can be noted that if a person has been suffering from epilepsy for a long time, then he is able to predict the occurrence of seizures in advance. This can be done by the aura, which is a harbinger of an attack. Often a person may feel increased anxiety without an obvious reason, which will gradually increase. Panic attacks are also possible; they can also indicate an imminent attack.
In many cases, seizures appear unexpectedly for the patient, and they cannot be stopped. The more severe the disease, the more pronounced its symptoms will be. It is for this reason that it is recommended to consult a doctor in a timely manner so that you can improve your well-being.
It is not uncommon for a person to experience simple partial seizures with cryptogenic epilepsy. In some cases, they can be confused with the usual manifestations of VSD. For example, a person begins to feel chills, tremors in the limbs, nausea and increased blood pressure. To distinguish an epileptic seizure from vegetative-vascular dystonia, you will need to pay attention to the distinctive features.
What is important to consider:
- The seizure lasts no more than 10 minutes.
- Convulsions occur.
- When performing echoencephalography, you can see the presence of an epileptic episode.
- After a short seizure, the patient is unable to concentrate on anything and appears very confused.
Hallucinations may often occur, as well as the inability to navigate in space. Just focusing on symptoms is not enough to make an accurate diagnosis. You will definitely need to undergo an examination, it will allow you to understand exactly what is happening to the person.
Complex seizures cause loss of consciousness and amnesia. The attack lasts up to 5 minutes, while the patient experiences obvious convulsions. In such a situation, it is important to monitor exactly how the seizure progresses. If it drags on and the suffocation does not go away, you should immediately consult a doctor.
It also happens that absence seizure occurs with cryptogenic focal epilepsy. The patient may partially or completely lose consciousness. At the same time, there is an absent expression on the face. It also happens that convulsions occur due to pathology, and it is extremely important to ensure that the person does not bite his tongue and suffocate.
Seizures depending on the focus
Manifestations of cryptogenic epilepsy are classified according to the site of occurrence:
- frontal region, anterior part - during an attack the patient has a frozen gaze, consciousness is disturbed, the head deviates, the eyes close;
- paraorbital focus - there is a change in the sense of smell, involuntary urination, movements are automated;
- frontal lobe, middle part - cessation of speech, complex body movements, aggression, screaming, facial expressions reflect horror;
- occipital part - automatic gestures and movements.
Cryptogenic epilepsy with generalized seizures has the most severe consequences. Once the deep foci of the brain are connected, the rest are activated, and loss of awareness and convulsions occur. Over time, a person loses memory, and personality degradation is observed.
Symptoms of frontal lobe epilepsy
Seizures of frontal lobe epilepsy are characterized by certain features that distinguish them from other types of seizures:
- short duration of attacks - usually their duration does not exceed 30 seconds;
- high frequency of seizures;
- absence or partial presence of confusion immediately after the attack;
- rapid transition of an attack to secondary generalization;
- a patient falls if brain cells are damaged by a bilateral discharge;
- intense movement disorders accompanied by active gesticulation and automatisms;
- development of an epileptic seizure mainly at night.
- involuntary turning of the head and pupils of the eyes to the side;
- disturbance of speech and perception - the patient utters inarticulate sounds in an attempt to say something, but does not understand the address to himself, does not perceive incoming information;
- loud laughter and shouting, quite often manifested in the form of obscene speech and gross insults;
- automatic movements of the limbs - the patient, in a supine position, rhythmically moves his legs, imitating riding a bicycle, boxes with his hands, performs rotational movements with the pelvis;
- a posture atypical for the normal state, in which one arm, bent at the elbow, is pulled back, and the other is stretched forward in front of you.
When the described signs appear, the patient must be protected from possible injuries, and after the attack ends, they must be shown to a neurologist.
Diagnosis of the disease
To treat cryptogenic epilepsy, a step-by-step elimination of pathologies with characteristic manifestations is carried out.
To make a diagnosis, specialists collect the following data:
- Anamnesis in detail and information about perinatal pathology, birth injuries, loss of consciousness in childhood.
- Electroencephalographic study, including registration of brain biorhythms during sleep and during exercise. Additionally, a sleep deprivation study is carried out, which makes it possible to identify the convulsive readiness of the nervous system.
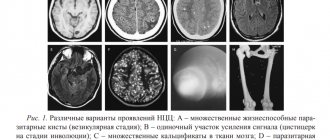
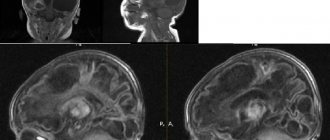
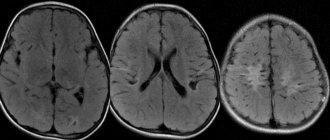
- Imaging techniques (dynamic MRI), which reveals not only focal pathology of brain tissue, but also sclerotic changes.
- Angiography, ultrasound examination of the blood supply to the brain, and, if necessary, duplex scanning combined with MRI in angiographic mode.
- Neuropsychological examination.
- Serological blood test for the presence of viruses. This technique makes it possible to identify infectious pathologies of the central nervous system.
- Laboratory tests, including general and biochemical blood tests (for immunoglobulins, glucose, amylase, lactic acid, coagulability, hemoglobin, hematocrit, leukocyte formula, platelets), urinalysis and genetic testing.
Epilepsy
Epilepsy is a neurological disease in which the patient’s brain is capable of generating a hypersynchronous neuronal discharge in response to changes in the constancy of the internal environment of the central nervous system. This is manifested by suddenly occurring paroxysms (fits). When recording the bioelectrical activity of the brain at the time of an attack, patterns typical for the disease are recorded.
Treatment of cryptogenic epilepsy
Conventional methods are ineffective in the case of this type of epilepsy. As a rule, monotherapy is recommended, due to which it is possible to reduce the development of side effects, which can negatively affect the condition. There are no other methods other than classical ones.
Among the antiepileptic drugs, carbamazepine or valproate are used, and in case of low effectiveness, they resort to their combination or other types. At the same time, other types of disorders are relieved. Since it is often unknown what cryptogenic epilepsy is, these abnormalities are carefully examined by qualified specialists without disturbing the patient’s usual lifestyle.
Symptomatic temporal lobe epilepsy.
The clinical manifestations of symptomatic temporal lobe epilepsy (TLE) are extremely varied. In some cases, atypical febrile seizures precede the development of the disease. VE manifests itself as simple, complex partial, secondary generalized seizures, or a combination thereof. Particularly characteristic is the presence of complex partial seizures occurring with a disorder of consciousness, combined with preserved but automated motor activity. Automatisms in complex partial seizures can be unilateral, occurring on the side homolateral to the lesion, and are often combined with dystonic placement of the hand on the contralateral side. TE is divided into amygdala-hippocampal (paleocortical) and lateral (neocortical) epilepsy. Amygdala-hippocampal TLE is characterized by the occurrence of attacks with an isolated disorder of consciousness. Patients are observed to freeze with a mask-like face, wide-open eyes and gaze fixed at one point (he seems to be “staring” - “staring” in English literature). In this case, various vegetative phenomena may be observed: paleness of the face, dilated pupils, sweating, tachycardia. There are 3 types of SSP with an isolated disorder of consciousness: 1. Switching off consciousness with freezing and sudden interruption of motor and mental activity. 2. Turning off consciousness without interrupting motor activity. 3. Switching off consciousness with a slow fall (“limp”) without convulsions (“temporal syncopation”). Vegetative-visceral paroxysms are also characteristic. The attacks are manifested by a feeling of abdominal discomfort, pain in the navel or epigastrium, rumbling in the abdomen, the urge to defecate, and the passage of gas (epigastric attacks). An “ascending epileptic sensation” may appear, described by patients as pain, heartburn, nausea, emanating from the abdomen and rising to the throat, with a feeling of constriction, compression of the neck, a lump in the throat, often followed by loss of consciousness and convulsions. When the amygdala complex is involved in the process, attacks of fear, panic or rage occur; irritation of the hook causes olfactory hallucinations. Possible attacks with mental dysfunction (dreaming states, already seen or never seen, etc.). Lateral VE is manifested by attacks with impaired hearing, vision and speech. The appearance of bright colored structural (as opposed to occipital epilepsy) visual hallucinations, as well as complex auditory hallucinations, is characteristic. About 1/3 of women suffering from VE note an increase in attacks during the perimenstrual period. During a neurological examination of children suffering from VE, microfocal symptoms are often detected, contralateral to the lesion: insufficiency of the function of the 7th and 12th pairs of cranial nerves according to the central type, revival of tendon reflexes, the appearance of pathological reflexes, mild coordination disorders, etc. With age, most patients develop persistent disorders mental disorders, manifested mainly by intellectual-mnestic or emotional-personal disorders; The appearance of severe memory disorders is characteristic. The preservation of intelligence depends mainly on the nature of structural changes in the brain. An EEG study reveals peak-wave or, more often, persistent regional slow-wave (theta) activity in the temporal leads, usually extending anteriorly. In 70% of patients, a pronounced slowdown in the main activity of background recording is detected. In most patients, over time, epileptic activity occurs bitemporally. To identify a lesion localized in the medio-basal regions, the use of invasive sphenoidal electrodes is preferable. Neuroradiological examination reveals various macrostructural abnormalities in the brain. A common finding on MRI is medial temporal (incisural) sclerosis. Often there is also a local widening of the grooves, a decrease in the volume of the involved temporal lobe, and partial ventriculomegaly. Treating EV is challenging; many patients are resistant to therapy. Basic drugs are carbamazepine derivatives. The average daily dosage is 20 mg/kg. If ineffective, increase the dose to 30-35 mg/kg/day and higher until a positive effect or the first signs of intoxication appear. If there is no effect, you should abandon the use of carbamazepine, prescribing instead diphenin for complex partial seizures or valproate for secondary generalized paroxysms. The dosage of diphenine per day in the treatment of VE is 8-15 mg/kg, valproate – 50-100 mg/kg/day. If there is no effect from monotherapy, it is possible to use polytherapy: finlepsin + depakine, finlepsin + phenobarbital, finlepsin + lamictal, phenobarbital + diphenine (the latter combination causes a significant decrease in attention and memory, especially in children). In addition to basic anticonvulsant therapy, sex hormones can be used in women, which are especially effective for menstrual epilepsy. Oxyprogesterone capronate 12.5% solution 1-2 ml intramuscularly is used once on days 20-22 of the menstrual cycle. The prognosis depends on the nature of the structural damage to the brain. With age, most patients develop persistent mental disorders that significantly complicate social adaptation. In general, about 30% of patients suffering from TLE are resistant to traditional anticonvulsant therapy and are candidates for neurosurgical intervention.
Are medications always needed?
There is a list of cases when there is no need for anticonvulsants:
- the child's only seizure;
- pregnancy without complications;
- absence of risk factors, family history;
- seizure after prolonged sleep deprivation.
Situations in which anticonvulsants will be required for cryptogenic focal epilepsy in children and adults:
- confirmation of a history of epileptic seizures;
- presence of neurological pathology;
- manifestations of idiopathic generalized epilepsy;
- characteristic changes in encephalogram data;
- birth trauma in a child;
- organic pathology of the central nervous system from early childhood;
- epileptic stigmas;
- severe, life-threatening seizures;
- personality changes (most informative in adults);
- mental states equivalent to seizures;
- inadmissibility of a repeated seizure.
The choice of drug is made taking into account gender, age, the presence of concomitant conditions, and the type of seizure.
How to treat?
Treatment of cryptogenic epilepsy is carried out using modern anticonvulsants, after the patient has undergone a full examination using modern equipment. They help reduce the duration and frequency of nerve impulses. To suppress excitation, neurotropic drugs, as well as psychoactive drugs, are used.
If the conservative method is not effective and there is a threat to the patient’s life, surgical intervention is used to remove the source of excitation. It is best to carry out such an operation in a specialized clinic.
Treatment of cryptogenic epilepsy should be carried out constantly, under the constant supervision and supervision of a specialist. In some cases, after a certain period of time, it is possible to identify the cause of the disease, and the diagnosis is revised in favor of symptomatic epilepsy.
Rate this article:
(votes: 1 , average: 5.00 out of 5)
Loading...
Related posts:
- How does idiopathic generalized epilepsy manifest?
- How does occipital epilepsy manifest?
- What is focal epilepsy and how does it manifest?
- Causes, symptoms, types, main methods of treatment and prevention of epilepsy in children
- Kozhevnikov epilepsy: why it occurs and how this pathology manifests itself
- Causes, features of the course and methods of treatment of myoclonic epilepsy
Disability
Registration of disability for cryptogenic epilepsy is indicated if a threat to the health and life of the patient is confirmed. The specialist you should contact is a neurologist.
The amount of the labor pension is determined by the disability group. Complete loss of working capacity corresponds to the first or second group. The patient's condition requires hospitalization and outpatient examination.
To receive a referral for a special examination, you must have a constant deterioration in your condition with complications.
Disability groups, depending on the patient’s condition, are determined as follows:
- The third is the mildest, attacks occur rarely and without complications, the person remains able to work.
- The second is that it is characterized by frequent attacks and changes in the patient’s personality.
- The first is the most severe, a person is limited in caring for himself, is considered disabled, and has dementia. If the cause was a head injury, the brain has a high probability of degeneration. Convulsions, memory loss, and mental disorders are observed.
The most common factors influencing disability are seizures, injuries, occupational diseases, physical disabilities from childhood or as a result of military service.
Diagnostics
If signs of epilepsy occur, you should seek help from a neurologist.
At the appointment, anamnesis will be collected and complaints will be clarified. The presence of symptoms can be traced:
- Automatism of gestural nature;
- Confusion and retardation of consciousness;
- Changes in behavior.
A series of special reaction tests will be carried out to determine muscle strength, sensitivity, auditory and visual reactions, and the accuracy of coordination of movements. Mental changes in personality are analyzed.
Based on the results of the consultation, the patient will be sent for research:
- Differential method - diagnostics to exclude cerebral, vegetative-visceral changes;
- MRI, CT - scanning of brain structures to determine abnormal processes associated with oncology, the structure and patency of blood vessels, and identify other causes;
- EEG - recording of impulse activity and the speed of transmission of nerve currents. For the frontal type of epilepsy, the examination is not considered sufficiently informative, so it is carried out daily, after a sleepless night, during the night's rest to register complexes of the bilateral type;
- Angiography - x-ray assessment of the state of the circulatory system, central nervous system;
- Neuroradiological examination is a method for detecting abnormal processes in cerebral structures, spinal cord, peripheral nerve ganglia;
- Video monitoring - tracking changes in the patient’s condition throughout the day, while simultaneously recording increased excitability in cerebral structures. Based on the data, a comparative analysis is carried out and a conclusion is given.
How to reduce the frequency of attacks
It is impossible to get rid of epilepsy if you have this disease, but you can do everything that affects the frequency of parocrisis:
- provide yourself with adequate sleep;
- avoid physical overexertion;
- exclude alcoholic drinks;
- reduce the amount of meat dishes in the diet, exclude salted and smoked foods, consume onions and spinach juice;
- women during menstruation use natural diuretics (decoction of bearberry, borage, lingonberry leaf);
- in the event of the development of epilepsy as a result of injury or infection, it is recommended to carry foods containing sugar with you to prevent its decrease in the blood and an attack;
- protect your eyes from bright sunlight (wear dark glasses), avoid places with flashing lights;
- use products that help delay an attack (lavender oil);
- take baths with valerian every other day;
- work and have hobbies that distract and improve well-being.
Traditional medicine recommends the following remedy: boil 30 g of wolf bast root, insist, take a teaspoon three times a day.
What is frontal lobe epilepsy?
Frontal epilepsy accounts for 1-2% of epilepsy cases, and 22% of focal epilepsy cases. This is the second most common form of epilepsy after temporal lobe epilepsy.
Frontal epilepsy can debut at any age; the proportion of affected men and women is approximately equal.
The mental and neurological status of the disease depends on the etiology.
Clinical manifestations include, first of all, such characteristic ictal symptoms as motor manifestations (account for 90% of cases).
A frontal attack can occur in several forms:
motor phenomenon (tonic, clonic or postural), often accompanied by gestural automatisms at the onset of the attack;
the duration of the attack is several seconds;
rapid secondary generalization, which is observed more often than during attacks of temporal lobe epilepsy;
no or minimal postictal confusion;
high frequency of attacks, mainly developing at night. Consciousness is preserved or partially impaired. The clinical pattern of the attack depends on the location of the lesion.
Diagnosis of frontal epilepsy is carried out using an MRI study, which in approximately 60% of cases reveals changes in the structure. Functional neuroimaging methods help to localize the focus.
The prognosis for seizure frequency and response to therapy in cases of frontal lobe epilepsy is generally unfavorable.
Differential diagnosis often mistakenly classifies hypermotor seizures as psychogenic, and they can also be confused with familial paroxysmal dystonic choreoathetosis, paroxysmal kinesiogenic choreoathetosis, or episodic ataxia. Frontal absence seizures of symptomatic etiology can be mistaken for typical absence seizures, because their clinical characteristics and EEG are similar.
The zone of irritation in frontal lobe epilepsy determines the clinical manifestations of this type of epilepsy. These zones, in turn, allow us to distinguish several forms:
motor, accompanied by convulsions in the half of the body that is opposite to the lesion;
dorsolateral paroxysms, expressed as violent turns of the head and eyes in the direction, most often opposite to the focus of the disease. If Broca's center - the posterior parts of the inferior frontal gyrus - is also involved, then the patient experiences motor aphasia - a violation of oral speech while maintaining the functions of the articulatory apparatus;
orbitofrontal paroxysms, which manifest themselves as cardiovascular, epigastric or respiratory attacks. Sometimes pharyngeal-oral automatisms may appear, accompanied by copious salivation;
anterior, or frontopolar attacks with mental dysfunction;
cingulate attacks that disrupt a person’s emotions and behavior;
seizures that arise from the supplementary motor area of the brain. Thus, it happens that paroxysms from different parts of the frontal lobe of the brain spread to the additional motor area. In this case, the person suffers from frequent, usually nocturnal, simple partial seizures, which alternate with archaic movements and hemiconvulsions. Often, attacks are accompanied by aphasia - a speech disorder caused by damage to certain areas of the cerebral cortex, unclear sensations in the torso, arms and legs. In addition, tonic convulsions appear - one by one in any half of the body, or in the entire body at once, which resembles generalization.
“inhibitory” attacks, paroxysmal hemiparesis. A rather rare phenomenon in which, most often at night, paroxysms of archaic movements are observed. The frequency of attacks is high, up to 10 times per night, and attacks are often repeated every night.
Frontal epilepsy is treated with drug therapy (anticonvulsants), in full accordance with the principles of treatment of focal or partial epilepsies. Antiepileptic drugs - AEDs, first of all, do not treat the seizures themselves, they prevent secondary generalized tonic-clonic seizures.
If drug treatment does not bring the desired effect, surgical intervention is required, but frontal lobe epilepsy is less amenable to surgical treatment than temporal lobe epilepsy.