What is akathisia
The manifestation of akathisia can vary in intensity from feelings of restlessness or anxiety to excruciating discomfort
The term “akathisia” was introduced at the beginning of the last century by the Czech psychiatrist L. Gaskovec to designate the constant need for movement in patients suffering from a number of mental disorders.
In 1923, French medical luminaries described akathisia in people suffering from secondary parkinsonism, which was a consequence of encephalitis. Over time, the same restlessness was diagnosed in drug addicts, alcoholics, people suffering from Parkinson's disease, people who had just come out of anesthesia, and then in people taking typical antipsychotics.
Reasons for the development of the disease
Today, there are several approaches to understanding the reasons why akathisia develops: pathophysiological (non-drug) and medicinal.
Non-drug akathisia is associated with insufficient nutrition of the pontine region of the brain.
Medicinal forms develop against the background of:
- taking serotonin antagonists, beta-blockers, antipsychotics (antipsychotics) involved in the processes of dopamine regulation;
- rapid withdrawal of dopaminergic drugs;
- taking medications used in the treatment of Parkinson's disease and similar syndromes (Carbidopa, Levodopa);
- use of antidepressants;
- taking Norepinephrine, which is involved in the processes of regulating alertness, aggression and awakening.
Symptoms of akathisia are usually observed when taking the following drugs:
- neuroleptics: Haloperidol, Droperidol, Pimozide, Trifluoperazine, Asenapine;
- selective reuptake inhibitors: Prozac, Citalopram, Paroxetine, Fluoxetine;
- antidepressants: Venlafaxine, Trazodone, Amitriptyline, tricyclic group;
- antiemetics: Metoclopramide, Compazine, Promethazine;
- antiallergic drugs: Diphenhydramine, Cyproheptadine;
- after withdrawal of barbiturates, opioids, cocaine, benzodiazepines;
- combinations of psychotropic drugs (serotonin syndrome).
Provoking factors may be:
- genetic predisposition;
- high dosage of the drug or rapid build-up;
- the presence of traumatic brain injury or other damage to the central nervous system;
- magnesium or iron deficiency;
- presence of cancer;
- pregnancy;
- elderly, childhood or adolescence;
- anxiety and affective disorders.
Symptoms of the disease
At high doses or when taking strong drugs such as haloperidol or chlorpromazine, the feeling of restlessness may last all day, from waking up in the morning until bedtime.
Signs of pathology can vary from increased anxiety or restlessness to severe discomfort. Unpleasant sensations are usually felt in the knees and decrease after several hours of movement. After their legs get tired, people sit or lie down, but this does not relieve the symptoms of the disease.
After taking high doses of Haloperidol or Chlorpromazine, anxiety may be felt throughout the day - from morning until bedtime.
People with akathisia say they experience:
- internal tension and torment;
- neuropathic pain similar to restless leg syndrome or fibromyalgia.
Kinds
There are several significant forms of the syndrome.
Depending on the etiology, the disease is divided into:
- parkinsonian, caused by taking psychoactive substances;
- iatrogenic;
- withdrawal symptoms;
- spontaneous, developing against the background of mental disorders;
- post-stroke.
Depending on the clinical picture of the disease, there are:
- Motor akathisia, accompanied by a tendency to constant movement - marching in place, walking (people do not experience any mental discomfort or excitement).
- Sensory-psychic (subjective) akathisia, characterized by complaints of poor health in the absence of excessive motor activity (patients experience constant discomfort, anxiety, and unpleasant sensations in the lower extremities).
- Classic akathisia, accompanied by unpleasant sensations and increased motor activity (patients feel internal discomfort that decreases with movement). Pathology is confirmed by monitoring patients.
Depending on the time factor, there are:
- acute akathisia;
- chronic;
- late;
- withdrawal akathisia.
Acute akathisia develops in the first days or weeks after starting treatment with antipsychotics. As a rule, it is provoked by the prescription of large doses of drugs and disappears after the dosage is reduced.
Chronic akathisia occurs during prolonged treatment with antipsychotics. Discontinuation of the drug leads to the gradual disappearance of all symptoms.
Late akathisia develops during prolonged treatment. Discontinuation of medications in this case leads to an increase in neurological manifestations, increasing dosages leads to a short-term improvement in the condition followed by an increase in the severity of symptoms. Some time after discontinuation of the drug that led to the development of pathology, the manifestations gradually decrease, but in some cases they can persist until the end of life.
Withdrawal akathisia develops in the first few weeks after taking medications and persists for one and a half to two months. A longer course of pathology usually indicates its transition to a later form.
Despite the fact that the symptoms of akathisia, which developed while taking certain medications, disappear quite quickly, the manifestations of a late form of pathology can remind of themselves for several years with internal tension, insomnia, discomfort, motor restlessness, and panic attacks.
Clinical picture
Akathisia usually has two main components. Moreover, one of them is leading, and the second is not so strongly expressed.
So, the first component is called sensory or cognitive. It manifests itself in the form of uncomfortable internal sensations that force a person to perform certain actions. The patient is aware of these symptoms and can keep them under control.
The sensory component usually manifests itself in the form of a feeling of anxiety, tension, and increased irritability. Sometimes people experience clear somatic disorders - for example, pain in the legs or lower back.
The second component is motor. It consists in the fact that patients perform repetitive standard movements, which are individual for each person. Some people constantly walk, others sway their bodies or kick their feet, and still others itch or pick their nose.
Quite often, at the very beginning of a motor act, people cry out. They can also make mooing sounds. After motor activity begins to decline, vocalization disappears. It may appear at the beginning of the next motor act.
Complications
Alcoholism and drug addiction may occur as a result of attempts to alleviate the symptoms of the disease.
Complications of akathisia include:
- depressive states accompanied by suicidal thoughts and attempts to commit suicide;
- impulsiveness of actions;
- aggressiveness, danger to others;
- intolerance to psychopharmacological drugs;
- alcoholism, drug addiction, nicotine addiction, caused by attempts to alleviate symptoms by drinking alcohol, drugs, smoking.
Symptoms
If akathisia develops in the classic form, then it is characterized by the presence of anxiety combined with hyperactivity. At the very beginning of the development of the pathology, the patient is disturbed by motor disturbances in the legs, which is why the person cannot be at rest while standing, lying or sitting. Such patients are in constant motion, sometimes even marking time in the same place. If the patient occupies a horizontal position, then he constantly changes the position of his body; if he is in a sitting position, then he constantly swings his legs.
Over time, the pathology progresses, causing akathisia to spread from the lower extremities to the upper extremities. In the absence of proper treatment, the patient begins to wriggle his whole body, move in jumps, and in extreme cases, even involuntary movement of the eyeballs is observed.
Sensory akathisia manifests itself in the presence of unpleasant sensations throughout the body. The mental component is expressed in excessive anxiety syndrome, impossibility, tension. Patients claim that while they are in motion, it becomes much easier for them, but as soon as they stop, anxiety and fear begin to increase, which acts as a provoking factor for the start of new movements.
Akathisia often provokes sleep disturbances. A pathology that occurs over a long period of time without proper treatment causes significant changes in a person’s character. Such patients become suspicious, anxious, annoying, and nervous. Unrecognized pathology in time provokes the development of a number of complications.
Diagnostics
It is quite difficult to determine the presence of akathisia in the initial stages. Patients restrain excessive motor activity, hide the sensations they experience, have difficulty describing them verbally, and do not understand the changes occurring in the body due to the characteristics of the underlying psychiatric disease.
Often the only clinical manifestation of pathology is an irrational change in attitude towards treatment (it becomes extremely negative).
Instrumental examination tools (IT, CT, MSCT of the brain, REG, EEG) are informative only in terms of differential diagnosis.
Diagnosis of the disease is carried out by a psychiatrist based on a patient interview and clinical observation. Interviewing close relatives and friends and observing a person’s behavior without his or her consent are widely practiced.
To determine the severity of the syndrome, the Burns scale is used, which includes:
- objective assessment of motor activity;
- determining the severity of unpleasant sensations;
- general conclusion about the degree of akathisia.
Differential diagnosis
Differential diagnosis allows you to exclude pathologies such as:
- anxiety states;
- psychomotor agitation;
- hyperkinesis;
- Tourette's syndrome.
Anxiety states are characterized by a lesser need for movement, the presence of reactions from the autonomic nervous system, and a predominance of obsessive hand movements (fiddle with rosary beads, twisting buttons).
Psychomotor agitation is accompanied by a diffuse increase in motor skills and does not have a specific subjective coloring (increased motor activity does not bring visible relief).
Hyperkinesis has a typical motor pattern and can be partially contained.
Tourette's syndrome is manifested by the presence of facial and vocal tics, the desire to make a particular movement when trying to restrain the tic.
Causes
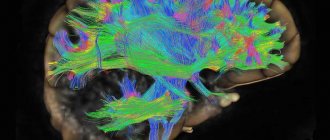
The development of akathisia is associated with dysfunction of dopaminergic pathways responsible for feeding certain areas of the brain.
The formation of the pathological condition is based on a disturbance in the serotonin networks, noradrenergic, opioid and GABA systems and neurokinin receptors. Such transformations provoke oxidative stress in neurons. A decrease in dopaminergic dynamics of the central nervous system leads to the inclusion of adaptation mechanisms to changes. One of these processes is an increase in the level of noradrenergic activity of the central nervous system, which leads to an increase in the secretion of adrenaline by the adrenal glands. An increase in the neurotransmitter in the systemic bloodstream leads to an increase in the psycho-emotional state, the appearance of anxiety and fear. Patients at risk include those with a history of:
- treatment with high dosages of antipsychotics or a sharp increase in dosage
- therapy with long-acting or atypical antipsychotics
- mood disorders
- mental disorders
- oncology
- pregnancy
- organic brain lesions
- chronic alcoholism
- deficiency of iron, magnesium
Also at risk are women, elderly patients and children.
Treatment
When determining the cause of akathisia, first of all, pay attention to whether the patient is taking medications that could provoke it
Treatment of akathisia begins with establishing the causes that led to the development of the syndrome. In the vast majority of cases, existing therapeutic regimens are reviewed for the presence of medications that can lead to the development of pathology.
If such drugs are detected, dosages are adjusted or drugs are replaced with drugs with less extrapyramidal effect. Almost all patients are prescribed magnesium supplements. Subsequent treatment is carried out using the following medications:
- central anticholinergics, prescribed when the pathology is combined with tremor or drug-induced parkinsonism and are used, as a rule, in conjunction with other medications due to lack of effectiveness;
- beta-blockers - lipophilic drugs that penetrate the barrier between the blood and the nervous system;
- GABA-ergic drugs that reduce anxiety, normalize sleep, relieve agitation (due to their weak effect, they are used in conjunction with central anticholinergics and beta-blockers);
- 5-HT2 blockers;
- antiadrenergic agents, which have an antiakathisic effect and reduce the severity of nightmares;
- dopaminergic drugs prescribed for persistent symptoms, eliminating dysphoric and depressive disorders.
Attention! A doctor must prescribe certain medications, as well as calculate their dosage. Self-medication is unacceptable due to the fact that it can aggravate existing health problems.
Pathogenesis
Akathisia is a vicious circle disease. It is caused mainly by medications, but the patient’s mental state itself suffers due to the fact that he cannot control his movements. This creates even more stress for the body, which leads to worsening mental health.
The chain of pathological reactions is closed, and it is no longer only treatment with antipsychotics that causes the disease. Therefore, when treating neuroleptic syndrome, it is necessary to focus not only on the abolition of pharmaceutical drugs, but also on the correction of the psycho-emotional background. If the cause of the occurrence is a disease of the central nervous system, then it is necessary to influence its cause, otherwise therapy for akathisia will not bring the desired results.
Neuroleptic malignant syndrome occurs in response to an inadequate dose of neuroleptics; the condition requires timely correction, as death is possible. At the slightest suspicion of a drug overdose, it is necessary to hospitalize patients on an emergency basis.
Serotonin syndrome sometimes goes away on its own after stopping the drug.
Prevention
A number of studies have shown that vitamin B6 can reduce the activity of akathisia.
Due to the fact that akathisia usually develops during treatment with medications, measures to prevent it are:
- competent use of antidepressants and antipsychotic medications;
- meticulous selection of dosages;
- drawing up combined therapeutic regimens taking into account the interaction of drugs with each other;
- preference for atypical antipsychotics that have minimal potential for developing extrapyramidal symptoms;
- inclusion of anticholinergics, beta-blockers or GABA-ergic drugs in treatment regimens if it is necessary to use drugs whose action is likely to lead to the development of akathisia.
Correction and therapy of deviations
Therapy for this disease should be selected individually, taking into account the clinical picture and severity of the disease.
The most effective treatment method is complete withdrawal or significant reduction in the dosage of the drug that triggered the appearance of these symptoms. However, in practice this is not always possible, due to the mental state of the patient. Canceling medications can lead to a serious deterioration in his well-being.
The main component of therapy is the prescription of medications that can increase the effectiveness of antidepressants or antipsychotics without causing their side effects. Thanks to this, it is possible to significantly reduce the dosage of drugs that provoke akathisia.
There are a number of treatments for the disease. Antiparkinsonian drugs, such as Biperiden, Benztropine, etc., help to cope with the disorder. Such drugs are often prescribed as an addition to antipsychotics, which eliminates their side effects. The dosage should be selected by the attending physician.
Experts also prescribe the following groups of medications:
- Antihistamines and anticholinergic drugs . They are not included in the category of powerful medications, but they can be part of effective therapy. In this case, the use of Diphenhydramine and Atarax is indicated. An additional advantage of this treatment is the fact that such drugs have a slight sedative effect, which helps calm the person. The drugs reduce agitation and restore sleep.
- Tranquilizers . Such remedies significantly reduce the activity of the disease, eliminating feelings of anxiety, sleep disturbances and spontaneous arousal. Such medications are usually prescribed if the doctor is unable to conduct a detailed diagnosis.
- Beta blockers . A number of experts claim that drugs such as Metoprolol and Propranolol help reduce the effect of neuroleptics and eliminate anxiety.
- Anticonvulsants . Such products are highly effective. Recommended drugs include Pregabalin and Valproate. They help cope with feelings of anxiety.
- Weak opioids . Such drugs as Codeine and Hydrocodone are highly effective for this diagnosis.
In late forms of the disease, discontinuation of the main drug is indicated. It should be replaced with an atypical antipsychotic. Your doctor may prescribe Olanzapine or Clozapine.
With this diagnosis, the prognosis directly depends on the type of disease and the causes of its occurrence. For example, drug-induced akathisia can last from 1 month to six months. In this case, the withdrawal form of the disease lasts about 15-20 days.
Forecast
The success of treatment for akathisia largely depends on both the timeliness of its onset and the causes, form and severity of the disease itself. In the vast majority of cases, the disease can be cured - correctly prescribed therapy can improve the condition of patients, eliminate the manifestations of the disease and prevent the development of complications.
Related Articles
Neuroleptics for schizophrenia: mechanism of action and review of the best drugs
Neuroleptic malignant syndrome: what it is, symptoms, ICD-10 code, treatment, consequences
Depersonalization syndrome: symptoms, causes and treatment methods
What is derealization and how to get rid of it?
Blepharospasm: causes of development, main signs and methods of treatment
Astheno-vegetative syndrome: what is it, ICD-10 code, causes of development, distinctive symptoms and methods of treating the disorder
Classification
Acute
Chronic
| Pseudoakathisia
Late akathisia
Returnable
|