Main symptoms:
- Leg muscle atrophy
- Arm muscle atrophy
- Muscle weakness
- Visual impairment
- Dysfunction of the pelvic organs
- Urinary incontinence
- Increased leg fatigue
- Increased leg muscle tone
- Decrease in intelligence
- Hearing loss
- Difficulty walking
- Difficulty moving the foot
- Difficulty bending the hip joints
- Difficulty bending your knees
- Frequent falls
- Epileptic seizures
Strumpel's disease is a disease in which weakness begins to appear in the legs. This happens due to increased muscle tone in the limbs. The disease is considered hereditary and can begin to develop at any age.
Online consultation on the disease “Strumpel’s disease”.
Ask a question to the specialists for free: Neurologist.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Possible complications
- Prevention
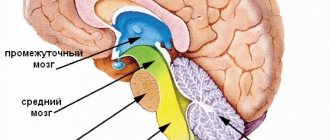
Spastic paraplegia (another name for Strumpel's disease) has been studied for more than a century, however, the research has not yet been completed. It was possible to find out that the pathology affects the functioning of the central nervous system and brain. In addition, it is slowly, but still progressing.
History of the discovery of the diagnosis
The disease was first described by the German neurologist Adolf Seligmühler in 1876. However, Adolf Strumpel studied and described it in more detail in 1883, who noted the hereditary nature of the disease.
In 1888, the study was continued by the French neurologist Maurice Laurent. In honor of the researchers, the disease was named Strumpel-Lauren disease; in modern practice, the name “Strumpel disease” is often used.
What triggers the development of the disease
The disease is genetic and hereditary. Inheritance can occur in several types:
- autosomal dominant - if one parent is a carrier of the gene, then there is a 50% -100% chance of the disease manifesting in children;
- autosomal recessive - if both parents carry a mutated gene, then there is a 25% -50% chance of the disease manifesting in children;
- X-linked type - women are carriers of the gene, and only men get sick.
In 2012, scientists at the University of Cambridge and the University of Miami identified the gene that causes Strumpell's disease. The disease occurs due to a mutation in the reticulon 2 gene on chromosome 19. Three types of mutations in the reticulon 2 gene have been discovered that lead to the disease.
Researchers suggest that the disease can be caused by defects in 17 regions of the chromosome in the case of dominant inheritance, in 29 regions in recessive inheritance, and in 4 regions in X-linked inheritance.
Treatment methods
- At the moment, there is no specific method that could accurately prevent the development of Strumpel’s disease or completely rid a person of it. There are various techniques that will reduce the manifestations of pathology, improve physical and emotional well-being, and also slightly slow down the progression of the disease.
- Doctors prescribe muscle relaxants , which are required to normalize muscle tone. Thanks to these tablets, it is possible to relax the muscles, which has a positive effect on the patient’s well-being. Popular drugs include Mydocalm, Baclofen and Scutamil. Tranquilizers such as Seduxen and Tazepam are also often used. With their help, it is possible to improve a person’s psycho-emotional state. To maintain the body, it is recommended to use B vitamins.
- At first, medications for familial spastic paraplegia are prescribed in a minimal dosage, and the dose is gradually increased. When spasticity decreases, the doctor stops adjusting the drug intake. If side effects occur, the dose increase is stopped immediately. It is quite possible that it will need to be reduced to get rid of the negative effects of the medicine. If the pills prove ineffective in a particular situation, then the person will be prescribed injections.
- In severe forms of the disease, a continuous infusion of Baclofen . It will need to be injected into the cerebrospinal fluid. In addition, Botulinum toxin ; it is injected into the posterior thigh muscles, as well as into the calves.
- In addition to drug treatment, a person is recommended to do special exercises, as well as go to physiotherapy. Often the patient needs to sign up for a massage and also take healing baths. All patients should be regularly monitored by an orthopedist. He must monitor how much the treatment helps in a particular situation. If necessary, the medical specialist will adjust the treatment regimen.
- In rare situations, a person may need to wear dentures. Some patients are also referred for surgery to treat passive joint restrictions.
It should be understood that Strumpel’s disease does not threaten human life, but the quality of existence decreases. The patient's ability to work may be significantly impaired. Pathology tends to progress, which is why the citizen’s condition gradually worsens. In most cases, patients retain the ability to move independently, but there is a loss of motor function. The pathology does not affect life expectancy if Strumpel's disease is not complicated by other abnormalities.
Modern classification
There are several classifications of Strumpel's disease, which take into account several aspects.
According to the mechanism of inheritance, they are divided into the following types:
- autosomal dominant type;
- autosomal recessive type;
- X-linked type.
Depending on the clinical manifestations and specifics of the course, the following forms are distinguished:
- uncomplicated form - there is spastic lower paraparesis, without other disorders;
- complicated form - in addition to lower paraparesis, there is atrophy of the optic nerves, dysarthria, retinopathy, cerebellar ataxia, epilepsy, mental retardation, hearing disorders, cardiac malformations, foot deformities).
Based on heredity, Shtrumpel's disease is divided into:
- familial - the disease is transmitted from the older generation to the younger;
- idiopathic - the disease is undocumented in the family history.
Depending on the age at which the disease began to develop, two types are distinguished: type 1 – the disease develops before the age of 35, spasticity of the lower extremities is observed more often than weakness, walking is less difficult;
- type 2 – the disease occurs after the age of 35, muscle weakness, disturbances in the urinary tract, muscle weakness are more often observed, the development of the disease is faster than with the first type.
The disease is also classified depending on the gene defect. Types are designated by the international abbreviation of the familial spastic paraplegia gene (SPG) followed by numbers from 1 to 76 (the numbers represent the loci at which the mutation occurred). At the moment, it is believed that type 4 SPG is the most common (more than a third of cases of the disease).
Forms of the disease
Based on the characteristics of the course of pathology, in medical practice the following forms are distinguished:
- Uncomplicated (the clinical picture in patients is dominated by weakness in the muscles of the lower extremities without concomitant disorders).
- Complicated (in addition to the above symptoms, patients are also diagnosed with heart defects, foot deformities, etc.).
Depending on the presence of confirmed cases of the disease among close relatives, the following are distinguished:
- Family Strumpel's disease (inheritance is carried out from parents to children).
- Idiopathic variant of the disease (in this case, a family history of the pathology cannot be detected).
In official sources, the disease described is presented in two main forms:
- Complicated.
- No complications.
In the first case, numerous neurological and vascular pathological manifestations are added to the main symptoms of the disease. For example, the heart rhythm is disturbed, epilepsy attacks appear, vision and hearing deteriorate, signs of ataxia appear, and mental disorders are observed.
If we talk about a disease without complications, then under such circumstances the clinical picture is clear: the patient’s condition is characterized by classic symptoms, there are no abnormal manifestations in the patient’s nervous system.
Clinical picture
Symptoms of Strumpel's disease appear gradually and do not develop quickly. At the beginning of the development of the disease in childhood, the main signs are difficulties in learning to walk, developing this skill, and walking on tiptoes.
When the disease develops at an older age, the manifestations begin with difficulty walking, fatigue of the legs, cramps, problems with bending the legs at the knees and hip joint, and frequent falls.
Then the symptoms become more intense, movement becomes more difficult, and patients find it difficult to move their feet.
Muscle weakness of the lower extremities occurs long after the onset of the disease. In recessive forms of the disease, the period of decrease in muscle strength is several years, and in dominant forms this period occurs much later than in recessive forms.
Muscle tone increases from the very beginning of the disease, while the muscles cannot completely relax and are tense all the time.
Spasticity is observed in the deep part of the triceps surae muscle (soleus muscle), adductor and posterior femoral muscles.
Spasticity may be asymmetrical and present only in one limb, but upon examination an increase in tone is revealed on both sides, and hyperreflexia of both lower limbs is observed.
Hyperreflexia is accompanied by extensor and flexion pathological foot reflexes (arising due to damage to the pyramidal system, which ensures muscle movements).
In the later stages of the disease, atrophic changes occur in the leg muscles, caused by a partial or complete decrease in activity due to paresis.
In diseases of types SPG 10 and SPG 17, the muscles of the upper limbs atrophy. In the extreme stages of the disease, there is a possibility of spastic paresis of the upper extremities, disruption of the pelvic organs, and involuntary leakage of urine.
In the SPG 19 form of the disease, urinary incontinence occurs with the onset of the disease, but in other forms it is more common in older patients.
In complicated forms of Strumpel's disease, a paraplegic has neurological symptoms:
- cognitive impairment (decreased intellectual abilities, mental retardation, dementia);
- epilepsy;
- dysarthria;
- retinopathy;
- optical neuropathy;
- extrapyramidal syndromes;
- hearing impairment;
- pseudobulbar syndrome.
STRUMPEL SYNDROME
The course of the disease is slowly progressive; a more malignant course is noted when it occurs at an early age. With the late development of the disease, hypertension and hyperreflexia predominate over motor disorders. The prognosis for life is favorable. The degree of disability depends on the severity of the dysfunction of the nervous system.
The development of the disease is gradual. Most often, the first symptoms appear in the second decade of life, although there is wide variation in the age at which the disease begins. Initially, stiffness in the legs and rapid fatigue when walking occur, increasing as the disease progresses. A characteristic spastic gait develops, varus and equinovarus deformities of the feet, changes in the feet of the “Friedreich’s foot” type, tendon and muscle contractures, especially in the ankle joints, are added. Weakness in the lower extremities gradually increases, but complete paralysis of the lower extremities is not observed. During a clinical examination of patients, already in the initial stages of the disease, an increase in tendon reflexes is detected, pathological reflexes of the flexion and extension groups (Babinsky, Oppenheim, Rossolimo, Gordon, Schaeffer, Bekhterev-Mendel, Zhukovsky), clonus of the feet and kneecaps appear early. In most cases, skin reflexes are preserved, the functions of the pelvic organs are not impaired. There are no sensitivity disorders. Intelligence preserved. Much later, the upper limbs are involved in the pathological process. Often, lower spastic paraparesis is accompanied by symptoms of damage to the optic and oculomotor nerves, nystagmus, dysarthria, ataxia and intention tremor
Diagnostic criteria
The first stage of diagnosis is to study the medical history (whether there are similar complaints in the family history), asking the patient about how long ago the symptoms appeared (increased muscle tone, weakness in the lower extremities, stiffness in the legs, speech difficulties).
The neurologist must assess the strength in the muscles of the upper and lower extremities, muscle tone, and determine the presence of pathological reflexes. With Strumpel's paraplegia, muscle tone decreases with repeated movements.
Spinal cord studies (computed tomography and magnetic resonance imaging) can detect disorders in the pyramidal system by examining the spinal cord layer by layer. However, the likelihood of detecting changes in the spinal cord is not high.
A study using electroneuromyography helps to identify neuropathy and its degree of development. Using the study of sensory evoked potentials, a delay in the conduction of impulses along the posterior columns of the spinal cord can be detected.
The study of cortical evoked potentials helps to detect the low speed of impulse transmission along the path from the cortex to the spinal cord.
In complex forms of the disease, differential diagnosis is carried out. The neurologist must exclude diseases such as amyotrophic lateral sclerosis, spinal multiple sclerosis, spinal cord tumor, neurosyphilis, and vascular myelopathy. Magnetic resonance imaging helps differentiate Strumpell's paraplegia from leukodystrophy.
Establishing diagnosis
When symptoms appear, it is very important not to self-medicate, but to seek help from a doctor. At the appointment, the specialist first collects the patient’s medical history, listens to complaints and asks questions (when did the weakness in the legs appear, did close relatives have similar pathologies, etc.).
The next step is a neurological examination. It involves assessing muscle strength in the arms and legs and searching for pathological reflexes. Additionally, computed tomography and magnetic resonance imaging of the spinal cord itself may be prescribed. Such a study allows us to study its structure in as much detail as possible and identify possible thinning of the pyramidal tracts. Note that in most cases no pathological changes are detected on CT and MRI.
How else can Strumpel's disease be confirmed? Diagnosis of the disease also includes the study of sensory potentials. This method allows you to assess the degree of conduction of sensory impulses throughout the spinal cord. A DNA test is mandatory to identify the presence of gene mutations.
Particular attention should be paid to differential diagnosis, which in some cases causes difficulties. It is extremely important to differentiate this disease from Mills syndrome, a degenerative lesion of the central nervous system characterized by dilation of the cerebral ventricles and atrophy of the frontal and precentral gyri. Clinically, this disease manifests itself slowly. In the last stages of the disease, bilateral paralysis is observed.
It is important to differentiate familial spastic paraplegia from the so-called spinal type of multiple sclerosis. Here it is necessary to take into account the state of abdominal reflexes, sphincters, and the course of the entire disease. In this case, special attention is paid to the patient's medical history. Only after passing all the tests can Strumpel's disease be confirmed.
What does medicine offer?
At the moment, there are no treatment methods that can prevent, slow down, or stop the development of Strumpel's disease. Existing methods of therapy are aimed at relieving the intensity of symptoms and improving physical and psycho-emotional state.
Patients are prescribed to take muscle relaxants (Mydocalm, Scutamil, Baclofen), tranquilizers (Seduxen, Tazepam), and B vitamins.
Treatment begins with the lowest dosage of drugs, and then gradually increases the dosage. After spasticity decreases, the dosage is no longer increased.
If side effects occur, the dose increase is stopped and, if necessary, gradually reduced. If it is impossible or ineffective to take tablets, injections are prescribed, including endolumbarally.
In severe cases of spasticity, continuous intrathecal infusion of Baclofen (injection into the cerebrospinal fluid) is prescribed. Botulinum toxin injections are also used in the calf and hamstring muscles.
In addition to drug treatment, it is recommended to use physical therapy and physiotherapy. Physiotherapeutic methods include therapeutic baths, massage, and paraffin treatment. Patients should be observed by an orthopedist.
If necessary, wearing orthoses is recommended, as well as surgical treatment of passive restrictions in the joint.
Treatment of pathology
Is it possible to cure Strumpel's disease? The treatment that modern medical science can offer cannot be called 100% effective. The main goal of the therapy is to reduce the symptoms and improve the patient’s quality of life.
The patient takes medications whose action is aimed at reducing muscle tone. For example, Baclofen. The group of recommended medications includes various tranquilizers and vitamins. Physiotherapeutic procedures, pine needle baths, applications on the legs using paraffin will alleviate the patient’s condition. Sometimes it makes sense to undergo reflexology, acupressure, or physical therapy.
The importance of orthopedic therapy, which involves the use of special prostheses that help the patient move, cannot be underestimated.
Some experts recommend a simulator for Strumpel's disease, exercises on which are aimed at reducing muscle tone.
It is worth knowing that therapy in each clinical case is individual. The doctor takes into account not only the results of diagnostic measures, but also the current condition of the person, the severity of the clinical picture, and existing diseases.
Consequences and prognosis
Strumpel's disease is not life-threatening, but it reduces the patient's quality of life and ability to work. Hereditary spastic paraplegia can progress and have varying degrees of symptom severity. The prognosis for the development of the disease is individual in each specific case.
The most severe disease occurs when it occurs at an early age. During puberty, the condition of patients with uncomplicated forms may become stable.
In most cases, patients are able to walk independently, but complete loss of the ability to move is also possible.
Patients often have a normal life expectancy.
Ankylosing spondylitis - ankylosing spondylitis: a complete analysis of the disease
A person experiences constant tension in the back muscles and severe discomfort. Later, in the last stages, the vertebrae begin to fuse and ossify (ankylose), which is clearly visible during x-ray examination. This disease is characterized by slow development; the disease can behave quite passively for several years, occasionally only worsening.
If medication is aimed at eliminating signs of the disease, easing pain, and reducing the severity of inflammation, then exercise therapy allows you to restore normal joint mobility and improve the quality of life. The therapeutic exercise plan should be drawn up individually and only by a professional (orthopedist/traumatologist or rehabilitation specialist). The goal of exercise therapy is to strengthen the muscle corset and increase the patient’s motor capabilities.
We recommend reading: Whether a Seizure is Imposed on a Safe Deposit Box
Classification of Strumpel's disease
In clinical practice, a classification of familial spastic paraplegia is used, which takes into account several different aspects. Depending on the mechanism of inheritance, autosomal dominant, autosomal recessive and X-linked forms are distinguished. In the first case, if one of the parents has Strumpel’s disease, then the probability of the disease in the offspring is 50%. In the second, a disease in a child is possible if both parents are carriers of the defective gene, the risk of having a sick child is 25%. In X-linked inheritance, only males are affected; women are carriers of the pathological gene.
According to clinical manifestations, Strumpel's disease is classified into uncomplicated (simple) and complicated (complex) forms. The former are not accompanied by other leading symptoms other than spastic lower paraparesis, the latter are its combination with other neurological disorders (epilepsy, mental retardation, hearing impairment, optic nerve atrophy, retinopathy, cerebellar ataxia, dysarthria). There are also Strumpell's disease with onset in childhood, adolescence and adulthood.
Based on the type of gene defect, the classification is constructed in the form of a numerical sequence. The English abbreviation for the familial spastic paraplegia gene is SPG, followed by a number from 1 to 56 or more (due to the constant discovery of new types of mutations). Studies have shown that the most common type is SPG4, which accounts for up to 40% of cases.
Heredity of the disease
This disease can be transmitted exclusively by inheritance. In total, experts distinguish several types:
- Autosomal dominant (in a married couple where one of the parents suffers from this pathology, the probability of having a child with this diagnosis ranges from 50 to 100%).
- Autosomal recessive (the probability of giving birth to an unhealthy child in a couple where one of the parents is already sick can be from 0 to 50%).
- X-linked (most often the disease is diagnosed in males).
In medical practice, there are special cases (for example, Beer's syndrome, which is manifested by atrophy of the optic nerve), when the symptoms of the disease are very similar to familial spastic paraplegia, but are still independent diseases.
Symptoms of Strumpel's disease
With the early onset of the disease, the first symptoms are a delay in the formation of walking skills and tiptoeing. When starting at an older age, the clinic manifests itself as difficulty walking with frequent falls. Often the first complaint of patients is “poor support of the feet when walking,” “stiffness in the legs.” Increased muscle tone in the legs is present from the very beginning of the disease. During its debut, it can be transient in nature: it intensifies when walking and disappears at rest. Spasticity predominates in the soleus muscles of the leg, adductors and posterior muscles of the thigh. It may be asymmetrical. In some cases, the patient complains of problems with only one leg. However, a neurological examination reveals a bilateral increase in tone and hyperreflexia of both legs with the presence of pyramidal foot signs (Oppenheim, Babinsky, Bekhterev, Rossolimo, etc.), foot clonus can be caused.
Strumpel's disease is characterized by gradual development. A decrease in strength in the leg muscles (paresis) appears after a fairly long period. In autosomal recessive forms it is several years, in dominant forms it is even longer. Among sensory disorders, some patients experience mild disturbances in vibration perception, and sometimes paresthesia in the legs and feet. More pronounced sensory disturbances are observed with the addition of polyneuropathy, usually in complicated forms.
Atrophic changes in the leg muscles, as a rule, occur in the late stages of Strumpel's disease and are caused by immobility due to severe paresis. Some forms of familial hereditary paraplegia (SPG10 and SPG17) are accompanied by atrophy of the arm muscles. In an advanced stage of the disease, spastic paresis of the upper limbs and urinary incontinence may occur. The latter is more typical for elderly patients, but with SPG19 it manifests itself at the onset of the disease. Complex forms of the disease are accompanied by a number of additional neurological symptoms, primarily cognitive decline from mild mental retardation to severe dementia. Possible epilepsy, optic neuropathy, congenital retinopathy, dysarthria, cerebellar syndrome, extrapyramidal disorders, hearing loss, pseudobulbar syndrome.
Strumpell's disease is a genetically determined disease that can be either autosomal recessive or autosomal dominant, characterized by damage to the pyramidal tracts and manifested by a progressive increase in muscle tone in the lower extremities [3].
This disease was first described in 1883. It was described by A. Strumpel. He indicated the presence of hereditary forms of paraplegia, presenting descriptions of clinical cases of patients who were characterized by the progression of spasticity and weakness in the lower extremities. In this case, mild disturbances in vibration sensitivity and disturbances in the functioning of the bladder were noted.
It is difficult to find accurate data on the prevalence of this pathology; they vary from 6 to 8 cases per 100,000 of the general population.
It is customary to distinguish two main classifications: according to the type of inheritance and according to the clinical principle [2].
According to the first classification, this disease is divided into autosomal dominant forms, autosomal recessive and X-linked. When making a diagnosis, the symbol of the disease gene is noted. Referring to English-language sources - SPG, which means “spastic paraplegia gene” - spastic paraplegia gene. A number from 1 to 32 is indicated to indicate the chronological order of the description of the locus [2].
According to the second classification, simple and complex forms of the disease are distinguished. Simple ones are those in which hereditary spastic paraplegia is the main symptom, and complex ones are a combination with symptoms such as mental retardation, decreased hearing acuity, retinal degeneration, optic disc atrophy, epilepsy, cerebral ataxia, peripheral neuropathy. According to statistics, complex forms do not exceed 10% of the total number of diseases [2].
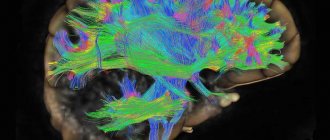
The pathogenesis of Strumpel's disease has not been sufficiently studied. At the moment, there are four mechanisms for the development of the disease, which consist in the functioning of certain genes. During embryogenesis, the development of the SPG1 gene is disrupted, resulting in incorrect formation of axons of nerve cells in the brain, cerebellum, and spinal cord. An error in the L1CAM gene leads to a failure in the mechanism of cell differentiation and axon growth [1].
Changes in the SPG2 gene lead to disruption of myelin production and oligodendrocyte maturation [1].
Table 1 | Localization, mode of inheritance and SPG gene products
However, regardless of which link of pathogenesis is involved in the development of Strumpel’s disease, in all described cases, degeneration of axons entering the pyramidal tracts and middle columns of the spinal cord occurs [3].
There are descriptions of a decrease in the number of neurons in the fifth layer of the motor cortex and the basal ganglia of the brain, the cerebellum, and the anterior horn of the spinal cord [3].
Despite the fact that most often the disease manifests itself in the second decade of life, there are also asymptomatic carriers of genetic changes. Patients with early onset of the disease tend to tiptoe. Those who are struck by the disease at a later age most often complain of gait disturbances and frequent falls, loss of balance when walking, as if they have difficulty feeling the support of their feet. Muscle tone in the legs increases; in the early stages of the disease, spasticity is observed only during walking, but as Strumpel's disease progresses, it becomes noticeable at rest. Muscle tone is increased in the adductor muscles of the thighs, the posterior group of thigh muscles, and the soleus muscles [1,3].
The onset of muscle weakness occurs later than the onset of spasticity. A characteristic symptom is hyperreflexia, and possible foot clonus.
Some forms of the disease are characterized by pseudobulbar disorders, characterized by impaired bladder function. It is worth noting that most often such manifestations occur in elderly women at advanced stages of the disease [3].
The dynamics and speed of development of certain symptoms of the disease vary greatly. If the patient has a simple form, progression is slow. Such patients only lose the ability to move independently without appropriate treatment. In complex forms, secondary symptoms are added to the main symptom, usually from the nervous system. Dementia manifests itself first [2].
Diagnosis of Strumpel's disease is problematic. It is necessary to pay attention to the manifestations of the disease and family history. The leading symptom is progressive spastic paraplegia [2].
Instrumental research methods do not always provide sufficient evidence to make a diagnosis. The use of MRI of the spinal cord allows us to identify its dystrophy. Electroneuromyography can be used as one of the diagnostic methods, but it is rarely used and, first of all, is necessary in order to characterize concomitant neuropathy, if, of course, it exists. Determination of somatosensory evoked potentials of the lower extremities demonstrates a delay in impulse conduction along the posterior columns of the SC. Cortical evoked potentials demonstrate a significant decrease in corticospinal conduction velocity and a decrease in the amplitude of evoked potentials. Molecular diagnostics can be used, but due to its high cost and low availability, it is practically not used [1,2].
There is no specific treatment for Strumpell's disease. Any treatment is aimed at eliminating the symptoms of the disease. Drugs such as baclofen, diazepam, and dantrolene are used. They are used both orally and endolumbarally for severe forms of spasticity. When prescribing any form of drugs, the principle “from least to most” is adhered to. Start with the minimum dose and increase it if there is no effect. Drug withdrawal is carried out gradually to reduce the likelihood of withdrawal syndrome [1].
Table 2 | Principles of drug therapy for Strumpel's disease
Botulinum toxin is also often used to treat spasticity. It is injected into the calf muscles, the posterior thigh muscles. After its introduction, an improvement in mobility is observed. Botulinum toxin is also a preventive measure for shortening muscle tendons along with physical therapy [1].
Sources:
- E. D. Belousova. Hereditary spastic paraplegia. / E. D. Belousova // Russian Bulletin of Pediatrics - 2010 - P. 63–69.
- E. I. Elagina. Hereditary degenerative diseases of the nervous system. Shtrumpel's disease or familial spastic paraplegia./ E. I. Elagina, E. Yu. Kurytsina // Problems of medicine in modern conditions - 2014 - pp. 205–209
- G. E. Rudenskaya. Common forms of hereditary spastic paraplegia./ G.E. Rudenskaya, I. G. Sermyagina, S. N. Illarioshkin // Journal of Neurology and Psychiatry named after. S.S. Korsakova - 2020 - pp. 94–104
Diagnosis of Strumpel's disease
The presence of lower central paraplegia as a basic symptom and its familial nature are of decisive diagnostic importance. In sporadic and complicated forms, the neurologist has to carry out differential diagnosis with ALS, spinal cord tumor, spinal variant of multiple sclerosis, vascular myelopathy, and neurosyphilis. To differentiate Strumpell's paraplegia from leukodystrophies, an MRI of the brain is performed. In some cases, it reveals atrophic changes in the cerebral cortex. MRI of the spine visualizes degenerative-atrophic processes in the lateral and anterior columns at the level of the thoracic and/or lumbar segments of the spinal cord.
An auxiliary method in the diagnosis of Strumpel's disease is electroneuromyography (ENMG) and the study of evoked potentials. ENMG allows you to determine the presence and degree of neuropathy. The study of somatosensory EPs demonstrates a delay in conduction along the posterior spinal columns, while the study of cortical EPs demonstrates a decrease in the speed of conduction along the corticospinal tract. Genealogical analysis and molecular genetic studies are of great diagnostic importance. Due to the great heterogeneity of pathology, the latter are carried out only for the most common types of disease. Prenatal diagnosis is possible.
What diseases give the right to disability
You should also take into account the fact that doctors and ITU experts examine not only aspects of the patient’s disease, but also his financial security. If the patient claims that his relatives help him or he has large bank deposits, then most likely he will be denied disability, citing that he will not use his benefits, providing himself with better medicines and other methods of treating his disease.
We recommend reading: List of subsidies available to large families but not to the poor in 2019-2019
For disabled people of group 2, deviations from the norm according to the main criteria are provided at a level of 70 to 80%. That is, a person must be able to perform basic self-care activities, including partially with the help of other persons or using special technical means (for example, visually impaired or hearing impaired citizens).
Erb Strumpell's disease: symptoms and treatment
The type of illness, which is characterized by weakening phenomena in the lower extremities of a gradual nature, against the background of the concept of the tone of muscle fibers in the legs, is called spastic paraplegia, or Strumpel's disease.
Pathological processes affecting the lower extremity girdle appear after abnormalities begin in the development of the spinal cord columns and nerve cords in the region of the lumbar column. The disease was named after the medical worker Erb Strumpel, who devoted a lot of time to studying the nature of the pathological condition. In the course of experiments and special studies, he found out that the disease is hereditary.
In addition, patients have hypertonicity of muscle fibers in the lower extremities, destruction of the cerebellar canals, and a decrease in the number of structural units of nerve fibers located in the cerebral cortex. But the basic symptom that medical scientists have discovered is a change in cellular structures in the sternum, on the side of the spinal cord.
The appearance of symptoms is caused by the participation of processes of genetic origin and the disease can be transmitted from one generation to another in the same family, and can also occur due to chromosomal abnormalities. More than 100 years have passed since the world first learned about the disease, but it continues to be studied in the modern world. The main factors are the influence of the brain and the central nervous system in particular on increasing muscle tone in the lower extremities. The disease progresses slowly but steadily.
Forms of Strumpel's disease
In official medical sources, the disease is divided into several forms:
- With possible complications;
- No complications
The form of the disease with developing complications is expressed not only by the main symptoms, including severe paresis of the lower girdle of the limbs and increased muscle tension in the legs. Additional disorders are disturbances in the functioning of the heart muscle, epileptic seizures, visual and hearing impairment, as well as various mental abnormalities.
A form of the disease that develops without complications can be characterized only by basic manifestations of the clinical picture, which can cause the occurrence of other types of abnormal phenomena in the nervous system.
One of the classifications comes down to genetic predisposition. But despite the fact that the disease is considered genetically hereditary, in some clinical cases there is no component of the genetic type. This is what determines the division of Strumpel's disease into hereditary and non-hereditary (idiopathic type).
Causes of Strumpel's disease
No matter how hard modern scientists tried, using advanced technologies, to find out the causes of Strumpel’s disease, they failed. Thus, there is an assumption that the transmission of the disease in a hereditary manner may be due to gene abnormalities:
- Dominant-autosomal - in this case, one of the parents of the unborn child has an unusually high probability of being affected;
- Recessive autosomal - with this type of inheritance, the likelihood of a child becoming infected from the parents is not high enough;
- Chromosomal feature of the X chromosome - there is an assumption that men are more often susceptible to the disease than the female half of humanity
If the disease does not have a genetic type of inheritance, possible causes could not be identified at all. Many experts are discussing this matter, putting forward various versions, but they have not yet been able to come to a consensus.
Symptoms of the disease
The picture of clinical manifestations for this type of pathology is quite simple. If Strumpel's disease proceeds without visible complications, it ultimately leads to paresis in the lower extremity girdle, as well as pain in the lumbar column. In addition, the symptoms characteristic of Strumpel's disease are constant increased tone in the limbs. The basic symptoms are: Problems with walking – these come in various forms and usually depend on the age of the patient. If the disease began to develop in childhood or even in a newborn, then difficulties will begin to appear already in the process of the child learning to walk.
In middle age, there may be unexpected manifestations of falls during normal walking, as well as chronic pain in the joints and muscles of the legs. In practice, it also happens that a patient may talk about pain in only one leg, but this is not entirely true. After all, a feature of Erb Strumpel’s disease is the presence of synchronous damage to two lower extremities at once.
- Weakness in the muscle fibers of the legs, or increased tone due to excessive tension;
- Increased fatigue of the lower extremities;
- Chronic fatigue;
- Increased irritability;
- Pain in the hip and knee joints;
- Beginning of foot deformation;
- Atrophic changes in muscle fibers (in some cases, the upper limbs are also affected);
- Continuous slow progression of symptoms
Advanced stages of Shtrumpel's disease can manifest themselves in the form of urinary incontinence and convulsive phenomena in the legs. In old age, other types of symptoms associated with neurological disorders may appear. Such signs of Strumpel's disease are:
- Epileptic seizures;
- Madness;
- Mild mental retardation;
- Movement disorders
It is important to know that signs of illness never appear out of nowhere - abruptly and suddenly. They develop gradually in most cases.
Manifestations of the disease
How does Strumpel's disease manifest itself? The symptoms of the pathology are simple. In the case of an uncomplicated form of the disease, symptoms are limited to paraparesis of the lower extremities, pain in the lumbar area, and increased tone of the leg muscles.
Let us note the symptoms that characterize all forms of the disease:
- difficulty walking (the nature depends on the age of the patient). In the case of a small child, difficulties arise at the stage of the baby learning to walk. Sick children are delayed in starting to move independently on their feet. While walking, the baby timidly steps over and transfers his body weight to his tiptoes. From infancy, the child loses the ability to have a correct gait. A middle-aged person may fall when walking and experience chronic pain in the lower extremities. The nature of the pain depends on the position and current condition of the patient. An elderly patient may experience a state of partial (complete) immobility. A person experiences joint pain, sometimes there is deformation of the joints;
- weakness of the leg muscles, increased muscle tone due to excessive tension;
- leg fatigue;
- chronic fatigue, nervousness;
- joint ailments;
- foot deformity;
- paraparesis of the lower extremities;
- paresthesia;
- atrophy of the leg muscles (sometimes arms);
- synchronicity of symptomatic manifestations;
- progressive nature of symptoms.
An advanced form of the disease can lead to urinary incontinence and leg cramps. Senile age is an additional complication of the pathology, which leads to the development of epilepsy, the appearance of disorders in the motor system, etc.
All symptoms of the disease are gradual and progress over time. For this reason, the disease may remain undetected for a long time.
Diagnosis of the disease
To make a correct diagnosis in a pathological process, it is necessary to go through several successive stages. So, at the first stage, the specialist must conduct a thorough examination of the patient, interviewing and collecting a detailed history.
After this, as a rule, the second stage begins, including an examination by a specialist - a neurologist. Based on the results of specific physical exercises, a specialist can determine the level of tone of the muscle fibers of the upper and lower extremities. In addition, an important step is to monitor the presence of reflexes and the presence of synchrony in the affected girdle of the lower extremities.
Additional methods for making a diagnosis are:
- Magnetic resonance imaging;
- CT scan;
- Ultrasound examination of the spinal cord;
- DNA research on hereditary factors.
This type of pathology is quite rare and has a blurred course, so it is not possible to identify it in the early stages. It is difficult for doctors to predict in advance the degree of progress of Strumpel's disease and to find out the reasons for its appearance.
Treatment of the disease Strumpel's familial spastic paralysis
The prognosis for life is favorable. The degree of disability depends on the severity of the dysfunction of the nervous system.
Treatment is symptomatic. Prescribed drugs that reduce muscle tone are mydocalm, baclofen, isoprotan (scutamil), tranquilizers: sibazon (seduxen), nozepam (tazepam), chlozepid (elenium). Physiotherapeutic procedures and paraffin applications on the muscles of the lower extremities are indicated. Acupressure, reflexology, physical therapy, and, if necessary, orthopedic measures are used. Courses of general strengthening treatment are indicated: B vitamins, metabolic drugs: piracetam (nootropil), pyriditol (encephabol), aminalon, cerebrolysin, amino acids, ATP, cocarboxylase, drugs that improve microcirculation.