05.02.2017
Lyme disease is one of the common diseases that is transmitted through a tick bite. At the initial stage, many will not even pay attention to the symptoms of this disease, because it can be easily confused with the flu or allergic manifestations, and sometimes it looks like arthritis or arthrosis. At the initial stage, this lesion can simply not be noticed, so it often leads to disability and sometimes death. Therefore, it is important to know what Lyme disease is.
- What is Lyme disease
- How does infection occur?
- First symptoms
- How it develops
- Taking tests
- Treatment
- Consequences
Transmission routes
Ticks infected with the bacterium B. burgdorferi can attach themselves to any part of the body. Most often - in areas that are difficult to visually control on your own: the scalp, armpits and groin. For the pathogen to enter the body, the infected tick must be attached to the body for at least 36 hours.
Most people with Lyme disease are bitten by immature ticks, called nymphs. They are very difficult to notice. Adult ticks also carry bacteria, but they are easy to spot and can be removed within 36 hours. Most often, outbreaks occur in spring and summer.
There is no evidence that such a disease can be transmitted through air, food or water.
There is also no evidence of transmission between people through touch or airborne droplets
Lyme disease is not transmitted from person to person or from mother to fetus. Bacteria are found in body fluids, but are not transmitted to another person through sneezing, coughing, kissing, or touching. There is also no evidence that the disease can be contracted through sexual contact or blood transfusions.
Pregnancy and tick-borne borreliosis
It is believed that this disease has a negative impact on the course of the pregnancy period. However, it is not uncommon for sick women to bear completely healthy children.
The risk of intrauterine infection is 40%; in this case, the child is born with a congenital form of the pathology. There have also been cases when newborns died within a few hours after birth due to cardiac disorders incompatible with life due to borreliosis.
Infection of the mother during pregnancy can provoke intrauterine fetal death, miscarriages and late toxicosis.
Pathogenesis
Through the bite site, borrelia penetrate into the human blood and lymph, from where they enter all organs and tissues.
The spread of infection to the brain and heart is especially dangerous, which can lead to disability or death.
Some bacteria die, releasing toxic substances. The immune system reacts violently to this, activating lymphocytes. Antibodies are produced against toxins and particles of the dead microbe. If treatment with antibiotics is started before this point, then the chances of recovery are high with subsequent normalization of the function of the immune system.
If therapy has not been carried out, then borrelia begin to actively multiply, increasingly poisoning the body. The immune system works constantly in increased activity. Antibodies are produced and immune complexes are formed. They settle in tissues and organs, forming infiltrates - compactions. Inflammatory elements are drawn to them, which leads to swelling, scarring and tissue degeneration. The bacterium can persist in the affected area for a long time, triggering an autoimmune process.
Symptoms
Signs may vary in severity.
Some people have no symptoms at all in the initial stages.
The most common symptoms of the disease:
- fatigue;
- aching pain in joints or muscles;
- pain or swelling in the area of large joints: knees, shoulders, elbows; difficulty concentrating and short-term memory problems
- speech disorder;
- flat round or oval rash;
- headache;
- heat;
- enlarged lymph nodes.
If you have any of these symptoms after a tick bite, you should consult your doctor.
Symptoms in children
Children usually have the same symptoms as adults. The most common occurrences are:
- fatigue;
- aches in joints and muscles;
- heat.
These symptoms may occur immediately after infection or months or years later.
Also, 90% of children have a rash.
Stages of the disease
The disease occurs in three stages:
- early localized;
- early widespread;
- late widespread.
Not all patients get sick in stages. The clinical picture may vary for each patient individually. For example, a rash on the eyelids is considered one of the first signs of infection, but many people develop another type of rash or no rash at all.
In most cases, the disease begins with a flu-like state.
Stage 1: Early localized disease
The incubation period usually lasts 1-2 weeks after a tick bite. But sometimes signs appear after a few hours or a few days. One of the earliest signs of the disease is a rash at the site of the bite. A red spot appears, surrounded by white skin with a red halo; it may be warm to the touch, but it does not hurt or itch. The official name for this rash is erythema migrans. But many people do not have this symptom. A solid red rash may appear, or in people with dark skin it may appear as a bruise. Signs at the first stage:
- Erythema at the bite site.
- Chills, increased body temperature, weakness, lethargy.
- Headache, blurred vision and stiff neck.
- Pain in muscles and joints.
- Swollen lymph nodes and sore throat.
Stage 2: early advanced
Signs of the second stage appear 3-4 weeks after the tick bite. The person feels a growing general malaise, and the rash appears not only at the site of the bite. At this stage, the disease becomes systemic in nature - the infection spreads throughout the body, and internal organs are involved in the process. Symptoms may include:
- Heart rhythm disturbances (arrhythmias) that occur as a result of inflammation of the muscle tissue of the heart.
- Chest pain, palpitations, feeling of lack of air.
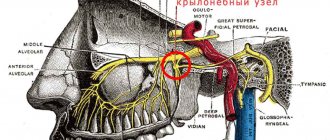
- Neurological conditions: numbness, tingling of the skin, meningitis, facial and cranial nerve palsy (Bell's palsy).
Clinical signs of the first and second stages may appear simultaneously.
Stage 3: Late disseminated Lyme
If Lyme disease is not treated promptly or effectively in the first two stages, late disseminated (after treatment, chronic or neurological) Lyme occurs weeks, months or even years after the tick bite.
Lyme bacteria have spread throughout the body, and many patients develop chronic arthritis and increased neurological and cardiac symptoms. Symptoms may include: This stage is characterized by:
- Multiple erythematous rashes on the skin surface.
- Arthritis of all joints or those located close to the bite site.
- Severe headaches, migraines, dizziness.
- Encephalopathy with short-term memory loss, impaired concentration, sleep problems.
- Aches and pain in joints and tendons, which appears in one area or another.
- Sleep disturbances, insomnia, poor concentration, memory impairment.
The third stage appears if the previous stages have not been treated. It can occur several months or years after the tick bite, becoming chronic.
Diagnostics
The diagnosis is made based on a carefully collected history and analysis of the clinical picture observed in the patient. Since the carrier of the pathology is a tick, the patient must remember whether he or she visited a forest, shelter belt, or park in the recent past. However, not all people notice a tick bite, so timely consultation with a doctor is rare.
To confirm or refute the diagnosis of Lyme disease, a specific diagnosis is carried out, which consists of the use of serological methods of blood testing - ELISA and ELISA. Performing such diagnostic manipulations helps to identify immunoglobulins (antibodies) of the IgG and IgM classes in the patient’s biomaterial.
However, in the first phase of the development of the disease, serological research methods turn out to be uninformative in 50% of cases. For this reason, blood serum is re-examined after 20-30 days.
By performing PCR, it is possible to accurately detect Borrelia DNA in a sample of skin tissue, cerebrospinal fluid, or blood.
How to identify pathology
Diagnosis of Lyme disease is based on indications of tick bites and exposure to an endemic area. The doctor completely examines the patient to detect the bite site and rash. Blood tests are most reliable several weeks after infection, when antibodies are present. The following tests are carried out:
- Enzyme immunosorbent assay - to detect antibodies against B. burgdorferi.
- Test for the presence of antibodies to specific proteins of B. burgdorferi.
- Polymerase chain reaction (PCR) is the most reliable test that is prescribed to all patients with persistent arthritis and damage to the nervous system.
Articular or cerebrospinal fluid is taken for analysis. But if the disease is present, a negative result may occur, which does not exclude the diagnosis, especially if the person took antibiotics.
Diagnostic features
Not all public and private laboratories test the tick itself for bacterial carriage.
Even if you are bitten by a tick, you can remove it from your skin and take it to the laboratory. But this does not mean one hundred percent that you are infected, for the following reasons:
- Laboratories that examine ticks often do not adhere to the strict quality standards of clinical diagnostic laboratories.
- If a tick tests positive for Borrelia carriage, this does not mean that the bacterium has entered the human blood or lymph.
- A negative result may lead you to falsely assume that everything is fine. You could have been bitten and infected by another tick.
- If you are infected with this disease, symptoms will appear before you receive test results.
Therefore, you should not waste time and delay the start of treatment.
False negative test results can occur in 50% of cases, and the symptoms of the disease are similar to other pathologies, which makes diagnosis difficult. Without the typical ring-shaped rash, Lyme disease often goes undiagnosed and untreated, leading to deep lesions and becoming chronic. Therefore, it is important to remember the time and place of the tick bite and monitor whether a rash appears.
It is advisable to photograph the bite site and rash, and then contact a doctor to make notes in the medical documentation.
If any changes in condition occur, it is advisable to record them. Signs may come and go, which is typical for Lyme disease.
You should also write down all the names and dosages of the medications you take.
Diagnosis in children
Diagnosing pathology in a child can be especially difficult. Unlike adults, children often cannot explain what has changed in their well-being. The child becomes nervous, excitable or lethargic, and night sleep is disturbed. Infected children have difficulty studying at school and cannot withstand physical activity. Because some of their symptoms, such as irritability, joint pain and difficulty concentrating, may reflect “growing pains,” legitimately ill children are often told that their problems are “all in your head.” Parents and teachers often tell children that they are naughty and do not want to go to school, when in fact the cause may be tick-borne borreliosis.
Causes
The causative agent of the disease is bacteria of the genus Borrelia from the family Spirochaetaceae. Carriers of pathogenic microorganisms are ixodid ticks (I.ricinus, I.pacificus, I.damini). An infected tick is infectious at any stage of its development. This means that larvae, nymphs, and adult arthropods are quite capable of leading to human infection with Borrelia with the further development of Lyme disease.
Human infection occurs when the tick's saliva gets into damaged areas of the skin. Another possible route of infection is contamination, when the contents of a crushed tick are rubbed into the skin while scratching itchy areas. In addition, there are known cases of pathology transmission through the placental route. A surge in pathology is observed in the spring-autumn period.
Treatment
Any disease is best treated in the early stages.
The early localized stage is easily treated with 10-14 days of oral antibiotics. Features of therapy:
- First-line drugs in adults and children are doxycycline, amoxicillin or cefuroxime.
- Amoxicillin and cefuroxime are used to treat women who are breastfeeding.
- People with damage to the nervous or cardiovascular systems may require intravenous antibiotic treatment, such as ceftriaxone or penicillin.
Regimens and dosages for adult patients
- Doxycycline 100 mg twice a day for 10-21 days.
- Cefuroxime 500 mg twice a day for 2-3 weeks.
- Amoxicillin 500 mg three times a day for 2-3 weeks.
Antibiotic treatment regimens for children
- Doxycycline - 4.4 mg/kg per day, divided into 2 doses for 10-21 days.
- Amoxicillin – 50 mg/kg per day in 3 doses for 2-3 weeks, maximum daily dose 500 mg. The maximum daily dose is up to 100 mg.
- Cefuroxime – 30 mg/kg per day orally 2 times a day. The maximum allowable intake is 500 mg per day.
Patients who are intolerant to amoxicillin, doxycycline and cefuroxime are prescribed macrolides.
For example, azithromycin, clarithromycin or erythromycin, but they are less effective in treatment.
People being treated with macrolides should be hospitalized and closely monitored by medical professionals.
Intravenous antibiotics are rarely used and only in cases of brain or heart involvement. After one to two weeks of intravenous medications, the patient is switched to oral antibiotics for another one to two weeks. Thus, the full course of therapy usually takes 14-28 days. If arthritis is present, antibiotics are prescribed for oral administration for a month.
Chronic syndrome
If a patient is treated with antibiotics for Lyme disease, but symptoms persist and new ones appear, it is called chronic syndrome. The chronic form affects the ability to perform physical and mental activity. A person is most often worried about fatigue, muscle pain, and slow thinking. Treatment is symptomatic, which is aimed primarily at relieving pain and discomfort.
Most people recover, but it may take months or even years.
The complication develops in 10-20% of people; the cause of this condition is not fully known. Experts speculate that Borrelia burgdorferi may cause an autoimmune response. Thus, symptoms persist much longer, even if the bacteria are no longer in the body. Other experts hypothesize that the chronic form is the result of the bacteria being present in the body, but in such low concentrations that it is difficult to diagnose. Patients with chronic syndrome usually recover within 6 months. But it may take several years to feel well and lead a fulfilling lifestyle.
It is recommended to consult your doctor to prescribe additional examinations and supportive medications.
.Main complications of Lyme disease
- degenerative changes in joints, arthritis;
- disorders of the nervous system, changes in cognitive abilities, even dementia;
- peripheral nerve palsy;
- disturbances in the functioning of the heart muscle, arrhythmias;
- loss of hearing, vision;
- benign skin tumors at the site of the tick bite;
- disability;
- death.
There is good news: Stanford researchers have found an antibiotic that completely destroys Borrelia - azlocillin.
It was found among 8,000 formulas, and research lasted six years. A scientific report on this was published on March 2, 2020. Standard therapy copes with the pathogen in 80% of cases; in other patients there is a tendency for the process to become chronic. We now believe that 300,000 people worldwide are infected with Lyme disease every year. A constant feeling of fatigue, weakness, and impaired mental functioning remain for many years and even for life.
Azlocillin completely destroys Borrelia burgdorferi, even those resistant to antibacterial drugs.
To date, the formula has been patented, and negotiations are underway with pharmaceutical companies about the production of the drug.
Perspective
If you diagnose the presence of Lyme disease in time and start using antibacterial agents, you can significantly reduce the duration of treatment and prevent the development of the third stage of the disease. Unfortunately, intervention at later stages does not always lead to successful treatment results. If the central nervous system has been affected during the course of the disease, a very sad prospect lies ahead. Unfortunately, some of the sick cannot avoid serious health consequences, and there are cases of disability.
It could be:
- muscle paralysis;
- paresis of facial nerves;
- hearing loss;
- damage to the soft membranes of the brain;
- arthritis;
- joint deformation;
- dementia;
- endocarditis;
- pericarditis;
- miscarriage.
The disease causes disorders not only of a physical nature, but also psychological. Having seen photographs of Lyme disease, these terrible spots characteristic of its course, I really want to make every effort to protect myself and my loved ones from such infections.
Prevention
You can get sick throughout the year, but the likelihood is highest in warm weather, especially in summer.
Before going out
take the following measures:
- Understand where ticks live: in grass, bushes, forests, on animals. You can pick up a carrier of the disease in your own garden.
- Treat things with permethrin. Its peculiarity is that the protective effect is maintained even after several washes.
- Everyone over three years old can apply picaridin and menthadiol to their skin.
- Walk along paths and well-trodden paths without tall grass, bushes, or fallen leaves.
Upon arrival home
- Inspect clothing for ticks. If you notice, delete it. Sometimes you can visually miss the carrier of the infection. Therefore, after visiting nature, it is recommended to wash clothes at maximum temperature and dry them in the dryer for ten minutes.
- If you were walking with your pet, check it for ticks.
- Shower yourself and bathe your pet within two hours of your walk. This will help wash away any mites if there are any.
- Examine your body yourself in front of a mirror, or team up with a relative and check each other out. Pay attention to areas with thin skin: neck, near the ears, stomach, inner thighs, flexor surfaces of the elbows and knees.
If you live in a private house
You can use the following tips:
- Mow the tall grass near your home.
- If there is a lawn or play area near the forest, then fence off the area with gravel.
- Periodically rake fallen leaves into one pile.
- If you have firewood, keep it in a dry place. Moist environments tend to harbor rodents that carry ticks.
- If there are items for outdoor games, then keep them in a bright place where the sun's rays penetrate.
- Do not keep old furniture, mattresses, or a pile of fallen leaves on the site. Take everything to the trash.
There used to be a vaccine for Lyme disease. But its production ceased in 2002. The official reason is low consumer demand. In addition, immunity from its use was unstable.
Even if you were vaccinated against Lyme disease before 2002, that doesn't mean you can't get it now.