Mediators of the autonomic nervous system
Definition of the concept
Autonomic nervous system neurotransmitters are transmitters that are used at synapses in the autonomic nervous system to convey excitation or induce inhibition to target cells.
It should be taken into account that the division of transmitters into mediators and modulators, into excitatory and inhibitory mediators, is conditional and very relative. The fact is that the same bioligand can perform different functions in the body: a mediator, a modulator, an excitatory mediator, an inhibitory one, a hormone, and a histohormone.
The sympathetic division of the autonomic nervous system uses norepinephrine, and the parasympathetic division uses acetylcholine.
| № | Name | Localization of synapses | Receptors | Effects |
| 1 | Acetylcholine (AC), a low molecular weight substance with a charge of +1 | a) autonomic ganglia, b) motor plates of skeletal muscles | n-cholinergic receptors (n-cholinergic receptors, nicotinic) - molecular receptors of the ionotropic type, for which acetylcholine is a mediator | Excitation of the postsynaptic membrane. |
| Postganglionic endings of the parasympathetic autonomic nervous system. | m-cholinergic receptors (m-cholinergic receptors, muscarinic) - molecular receptors of the metabotropic type, for which acetylcholine is a modulator | a) in blood vessels and the heart - an inhibitory effect: vasodilation, slowing down and weakening of heart contractions; b) in the bronchi, gastrointestinal tract, iris - stimulation of effector cells: narrowing of the bronchi, increased peristalsis and secretion of the gastrointestinal tract, constriction of the pupil. | ||
| 2 | Norepinephrine (NA), from the group of catecholamines, a derivative of the amino acid tyrosine | Postganglionic endings of the sympathetic autonomic nervous system. | α1-, α2-, β1-, β2-adrenergic receptors (all metabotropic type) | Excitation of α1- and β1-receptors has an excitatory effect, and α2- and β2-receptors have an inhibitory effect. Hence, a set of sympathetic reactions: 1) increased contractions of the heart, 2) constriction of muscle vessels, 3) dilation of the bronchi, 4) weakening of intestinal motility, 5) dilation of the pupils. |
| Typically, one organ contains several types of adrenergic receptors. In this case, α-receptors predominate in the vessels of the skin and sphincters of the gastrointestinal tract, β1-receptors - in the heart, β2-receptors - in the bronchi, intestines, uterus, and skeletal muscle vessels. | ||||
Sources:
Mushkambarov N.N., Kuznetsov S.L. Molecular biology. Textbook for medical students. M.: Medical Information Agency LLC, 2003. 544 p.
© Sazonov V.F., 2014. © kineziolog.bodhy.ru, 2014.
The main objects of VNS control.
Topic No. “Autonomic (autonomic) nervous system”
• Duration of topic study: 6 hours;
of which 4 hours per lesson; independent work 2 hours
• Venue: training room
Goal: to study the mechanisms of regulation of the body’s vegetative functions
Tasks:
Know the structural and functional features of the autonomic nervous system (ANS), the influence of the sympathetic, parasympathetic and metasympathetic departments on the innervated organs, the relative antagonism and synergism of their influences, the principles of organization of the afferent, efferent link of autonomic reflexes; organization of the autonomic ganglia, mechanisms of transmission of excitation in them, functional differences between preganglionic and postganglionic fibers, ANS mediators and the main types of their receptors; autonomic centers and their role in the regulation of autonomic functions, autonomic components of behavior in the formation of integral behavioral acts;
Be able to use this knowledge to explain the autonomic components of the body’s behavior in different conditions of its existence, assess the age-related characteristics of the autonomic regulation of functions, and understand the role of the autonomic system in ensuring homeostasis.
Motivation of the topic:
knowledge of the mechanisms of regulation of the vegetative functions of the body allows one to control homeostatic processes in the body using physiological and pharmacological influences. Knowledge of the adaptive-trophic influences of the sympathetic division of the ANS is important for understanding the mechanisms of ensuring adaptation of the body. Understanding the role of the ANS in ensuring emotional reactions and stress allows us to make the necessary corrections in vegetative processes and avoid unwanted shifts in homeostasis and dysfunction of internal organs.
• Methodological recommendations for self-training:
Task 1. Study the theoretical material of the lesson using the following logical structure of the educational material.
General characteristics of the autonomic nervous system. Vegetative and somatic functions of the body. F. Bichat (1801) proposed dividing functions into vegetative, common with plants - growth, metabolism, reproduction, and animal (somatic) - functions of skeletal muscles. I. Reil (1807) introduced the concept of the autonomic nervous system. K. Bernard considered it as a system of involuntary innervation. J. Langley (1898) identified the sympathetic, parasympathetic and enterinic divisions and proposed the name “autonomic nervous system”. Autonomic nervous system ANS )
- this is part of the nervous system that regulates the activity of internal organs, the lumen of blood vessels, metabolism, ensuring homeostasis and adaptation of the body.
Functional features of the ANS.
v Relative autonomy of the ANS: the possibility of regulation (in a less perfect form) with complete disruption of communication with the central nervous system, low possibility of voluntary regulation.
v Generalized nature of excitation in the efferent-effector section.
v Low lability and speed of excitation, long latent period of vegetative reflexes.
v Main functions of the autonomic nervous system: Ensuring and restoring homeostasis, participation in adaptation processes.
The main objects of VNS control.
- Smooth myocytes of various physiological systems.
- Cells of the glands of external and internal secretion.
- Cardiac muscle.
Divisions of the ANS: sympathetic, parasympathetic, metasympathetic
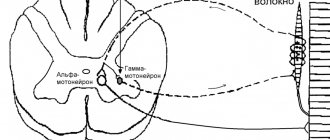
Sympathetic division of the autonomic nervous system (area of innervation - all organs and tissues). Spinal centers - preganglionic neurons of the lateral horns of the spinal cord C8 – L3
, their background activity is ~3 Hz.
(Spinociliary center – C8 – Th2, salivary center – Th 2-4, cardiac center – Th 1-5, blood vessels and sweat glands – C8-L3, etc.) They receive influences from afferent inputs to the spinal cord and overlying structures of the brain ( especially neurons of the reticular formation). Preganglionic fibers
- axons of preganglionic neurons belong to type B, the speed of excitation is ~ 10 m/s.
AP with long-term trace depolarization. The ganglia
of the sympathetic nervous system (paravertebral and prevertebral: superior and inferior mesenteric, celiac ganglia) contain ganglion neurons and interneurons.
The mechanism of excitation transmission in the sympathetic ganglia from the preganglionic to the ganglionic neuron: the mediator acetycholine
acts on the
H-cholinergic receptor,
which contains a Na+, K+ channel, the opening of which forms the incoming Na+ current and EPSP.
(Ganglion blockers - benzohexonium, hexamethonium, etc.) In the ganglia there are also inhibitory adrenergic interneurons (MIF cells), which form IPSPs on the ganlionic neurons. M-cholinergic receptors and opiate receptors on ganglion neurons are also involved in the regulation of mediator release. Postganglionic fibers
- axons of ganglionic neurons, belong to type C, the speed of excitation is ~ 1 m/s. AP with long-term trace hyperpolarization. The ratio of the number of pre- and postganglionic fibers of 1:100 ensures divergence and irradiation of excitation. This postganglionic irradiation and multiplication of excitation contributes to the mobilization of the body's functional reserves.
Neuroeffector synapses
(the axon branches of ganlion neurons have numerous varicosities, each of which forms a synapse on the executive cells).
Sympathetic adrenergic synapses
(transmitter: norepinephrine - 90%. adrenaline - 7%, dopamine - 3%, a cotransmitter - neuropeptide Y) is also released.
• The neurotransmitter norepinephrine acts on α—
and β-adrenergic receptors of the postsynaptic membrane. The effect of norepinephrine depends on the type of adrenergic receptors (for example, the mediator causes constriction of blood vessels through α-receptors, and their dilation through β1-receptors), the number of receptors and their ratio on the cell.
• Action of norepinephrine through α-adrenergic receptors
(α1 and α2, each of which has several subtypes) (blockers: phentolamine, droperidol, etc.).
Localization and effects realized through them: vessels (α 1, α2) constriction, myocytes of the intestines and stomach (α1) - decreased tone, smooth muscle sphincters (α1 - contraction, ureter (α1, α2 )
- contraction, β-cells of the pancreas (α2 ) - inhibition of insulin secretion, etc.
Mechanisms of action.
- The effect of norepinephrine through α1 - receptors is realized mainly through Gi-proteins of the membrane → ↑PL - C → ↑IF3 and DAG → ↑Ca2+ +KM → ↑LCM kinase
→ contraction of SMC of vessels, sphincters, radial muscle of the iris, etc. - The effect of norepinephrine through α2 receptors is realized primarily through GI membrane proteins → ↓AC → ↓cAMP → ↓PC-A:
in SMCs, ↑Ca2+ concentrations and activation of LCM kinase occur, which is accompanied by contraction; in endocrine cells there is a decrease in the activity of hormone synthesis enzymes (for example, insulin, angiotensin II, etc.), in adipose tissue there is inhibition of lipolysis enzymes (lipase), in the liver - glycogenolysis (phosphorylase); at the presynaptic terminal, inhibition of the synthesis and secretion of the transmitter norepinephrine.
3. Action of norepinephrine through β-adrenergic receptors
(through β1 strong, through β2 - weak effect) (blockers: propranol, atenolol, etc.).
Localization and effects realized through them: heart (β1) -
increase in the strength and frequency of contractions, blood vessels and bronchi (β2 > β1) - expansion, intestinal myocytes (β2>β1), bladder, uterus (β2) - relaxation, adipose tissue ( β1) - lipolysis is activated, liver (β2) - glycogenolysis and gluconeogenesis, etc. Mechanisms of action: norepinephrine through β-adrenergic receptors and then the membrane GS protein activates AC and increases the level of cAMP, which stimulates PC-A, which phosphorylates various proteins:
— in the heart, phosphorylation of the EPS Ca2+ pump leads to its inhibition, which increases the level of Ca2+ in the cytosol, its connection with troponin and then the force of contraction;
— in SMCs, phosphorylation of LCM kinase makes it (the kinase) less sensitive to the Ca ++CM complex. As a result, the SMC relaxes,
- phosphorylation of enzymes increases their activity (for example, enzymes for the synthesis of hormones - liberins and statins of the hypothalamus, tropic hormones of the adenohypophysis, insulin, etc., phosphorylases in the liver and lipases in adipose tissue);
- in the presynaptic terminal of adrenergic synapses, the synthesis and secretion of the transmitter is stimulated.
Inactivation of the transmitter: about 80% of norepinephrine enters by endocytosis back into the presynaptic terminal, a small part is destroyed by monoamine oxidase of the pre- and postsynaptic membranes and catechol-O-methyltransferase of the postsynaptic membrane, part diffuses into the intercellular space and blood.
Sympathetic cholinergic synapses
(available in small quantities).
• The mediator acetylcholine acts on M- and N-cholinergic receptors of the postsynaptic membrane (also activated by muscarine and nicotine, respectively).
• M-cholinergic receptors: localization and effects realized through them - sweat gland cells (increased secretion), smooth myocytes of skeletal muscle vessels (vasodilation).
• H-cholinergic receptors are located in synapses on chromaffin cells of the adrenal glands (secretion of catecholamines). The peculiarity of this area is that neurosecretory synapses form preganglionic fibers, and chromaffin cells are an analogue of the ganglion neuron (clusters of chromaffin cells are also located on the surface of the aorta, in the carotid body, in the sympathetic ganglia).
v Autoregulation of norepinephrine secretion
at the synapse is carried out through receptors on the presynaptic membrane.
• A high concentration of norepinephrine in the synaptic cleft and adrenaline in the blood causes through α2-adrenergic receptors
inhibition of the release of norepinephrine from the presynaptic terminal.
• Low concentration of norepinephrine in the synaptic cleft and adrenaline in the blood causes through β2-adrenergic receptors
increased secretion of norepinephrine from the presynaptic terminal.
• Through M-cholinergic receptors
Reciprocal inhibition of norepinephrine secretion by acetylcholine occurs when the parasympathetic department is excited.
The main importance of the sympathetic department is to ensure urgent adaptation by mobilizing the physiological and mental reserves of the body.
The concept of the sympathoadrenal system
(L.A. Orbeli, 1926;): stimulation of the sympathetic department, which innervates the adrenal medulla, stimulates the secretion of adrenaline into the blood. Adrenaline excites the sympathetic centers through the reticular formation, which further increases its secretion. A positive feedback is formed, increasing the influence of the sympathetic nervous system on the body.
Parasympathetic division of the autonomic nervous system (the area of innervation is narrower, for example, it is not in the vessels of the skin).
Parasympathetic centers in the brain stem - nuclei III (ciliary muscle and sphincter of the pupil), VII (lacrimal, submandibular and sublingual salivary glands), IX (parotid salivary glands, vessels of the oral mucosa), X (organs of the thoracic and abdominal cavities, except for the small organs pelvis) pairs of cranial nerves, in the spinal cord - segments S2 - S4 (pelvic organs and external genitalia) contain preganglionic neurons..
Preganglionic fibers —
axons of preganglionic neurons are type B, conduction speed is 10 m/s. AP with long-term trace depolarization.
Ganglia of the parasympathetic nervous system.
♦ Located near the innervated organ or in the wall of the organ (intramural).
♦ Mechanism of excitation transmission in the ganglia: acetylcholine
acts on
the H-cholinergic receptor
(blocker - hexomethonium, etc.), which contains a Na+, K+ channel, the opening of which forms the incoming Na+ current and EPSP.
Postganglionic fibers —
axons of ganglion neurons are type C, excitation speed is 1 m/s. AP with long-term trace hyperpolarization. The ratio of pre- and postganglionic fibers is 1:1.
Neuroeffector synapses (terminals of postganglionic neurons on executive cells) - acetylcholine
acts on
M-cholinergic receptors
of the postsynaptic membrane (blocker - atropine).
v Localization of M-cholinergic receptors and effectors realized through them: heart (M2) - reduction in the frequency and strength of contractions, blood vessels (dilation), bronchi (constriction), bladder (contraction), salivary, lacrimal, gastric glands (M1 - stimulation of secretion and etc.
v Mechanisms of action of acetylcholine through M-cholinergic receptors:
• In the SMCs of the stomach, intestines, bladder, bronchi, etc., the effect of acetylcholine is realized through the Gq protein → ↑PL-S → ↑IFz and DAT → ↑Ca2+ +KM → ↑LCM kinase → contraction of SMCs. (In the heart, the calcium mechanism involving tropomyosin is weakly expressed, but can lead to a “paradoxical” increase in the rhythm and force of contractions.)
• In blood vessels, the effect of acetylcholine is realized through cytosolic guanylate cyclase, which is activated by NO formed in the endothelium and leads to an increase in the level of cGMP and PC-G activity. The latter inhibits myosin light chain kinase, which leads to relaxation of vascular SMCs.
• In the cardiac conduction system, the effect of acetylcholine is also realized through the guanylate cyclase system. In this case, cGMP-dependent protein kinase activates the K+ channel. The K+ current leaving the cell inhibits slow diastolic depolarization, which leads to a decrease in the rhythm and conductivity of the heart.
v Inactivation of the mediator: most of it is destroyed by acetylcholinesterase (choline and acetate are captured by the presynapse), some diffuse into the intercellular space and blood.
The importance of the parasympathetic department
autonomic nervous system.
1. Together with the metasympathetic department, it ensures the preservation and restoration of homeostasis.
2. Regulates the processes of anabolism and storage of reserves.
Metasympathetic division of the autonomic nervous system (J. Langley, 1898; A.D. Nozdrachev, 1980). Metasympathetic nervous system
is a complex of microganglia located in the walls of hollow organs that have their own motor activity (heart, gastrointestinal tract, genitourinary system).
It has the narrowest area of innervation - only organs that have their own motor activity. Organization of the reflex pathway in the metasympathetic region (all neurons in the intramural ganglia).
v Receptors and fibers of afferent neurons (afferent part of the arc).
v In the ganglia there are afferent, intercalary and efferent neurons (“center”).
v Axons of efferent neurons, nerve-effector synapse (efferent part of the arc).
Neuroeffector synapses have various mediators (ATP, serotonin, peptides, acetylcholine, norepinephrine).
The influence of the metasympathetic department (activating and inhibitory) depends on the type of mediators, the type of receptors, the included intracellular mediators, and the initial state of the organ.
1. On the motility of innervated organs.
2. For secretion and absorption.
3. On the regulation of local blood flow.
4. On the secretion of local endocrine cells.
Physiological significance of the metasympathetic division.
v Increases the reliability of the regulation of visceral functions, making it autonomous, relatively independent of the central nervous system.
v Relieves the higher parts of the central nervous system from processing unnecessary information (the number of neurons in the metasympathetic ganglia exceeds the number of neurons in the spinal cord).
Recommended pages:
Use the site search:
Coordination of motor and vegetative functions of the body
Direct stimulation of cortical neurons by electrical current, or cortical stimulation in acute experiences, can cause body movements and changes in autonomic functions. Irritation of the motor area, from which the pyramidal and extrapyramidal tracts emanate, causes contractions of skeletal muscles, and the premotor area causes changes in the functions of internal organs. In the frontal lobes of the cerebral hemispheres, somatic and autonomic functions are coordinated, as proven in animal experiments and observations in humans with lesions in these areas. For example, in the motor and premotor areas, the activity of the heart, the redistribution of blood, changes in thermoregulation and sweating are coordinated with muscle work, the motor and secretory activity of the digestive canal is coordinated with muscle work, etc. This coordination of motor and autonomic functions corresponds to the individual experience of the body. The influence of motor activity on autonomic functions is bilateral, since autonomic functions affect metabolism in skeletal muscles, their tension and contraction. But the leading role belongs to muscle activity, which ensures the behavior of the body and its interaction with the external environment.
Conditioned reflexes, which unite and coordinate muscular activity and the function of internal organs, are controlled by the cerebral hemispheres and subcortical centers.
Tension and contractions of skeletal muscles and the work of internal organs are coordinated through unconditioned and conditioned reflexes due to the entry of afferent impulses into the cerebral hemispheres from the organs of vision, vestibular apparatus, skin receptors, muscles, tendons, joints and internal organs. For example, at the school of V.M. Bekhterev, motor and secretory conditioned reflexes were formed in children to irritation of stomach receptors. The area of the cerebral cortex, which receives afferent impulses from internal organs, was designated by I. P. Pavlov as a “cortical representation”, or “internal analyzer”.
Conditioned and unconditioned reflexes subtly and accurately coordinate the function of internal organs and the chemical composition of the internal environment with contractions of skeletal muscles, which ensures the unity and integrity of the body in its relationship with the external environment, maintains homeostasis - the relative constancy of the internal environment of the body.
The location of higher centers coordinating motor and autonomic functions in the frontal lobes of the brain was proven back in the last century.
Irritation of the cortex of the frontal lobes of the brain changes cardiac activity and respiration (V. Ya. Danilevsky, 1874), slows down and quickens the pulse, increases and decreases blood pressure, causes salivation, changes the tone and peristalsis of the stomach and intestines, contracts the bladder, vagina, constricts and dilates the pupils (V.M. Bekhterev and P.A. Mislavsky, 1886, 1888, 1890; A. Cherevkov, 1892), changes body temperature (V.M. Bekhterev, 1881). In the school of V. M. Bekhterev, acute experiments proved the effect of irritation of the cerebral cortex on gastric secretion, urination, contraction of the spleen and all other autonomic functions.
At the school of I.P. Pavlov, conditioned reflexes were formed to skeletal muscles, to the glands of the digestive canal, to the smooth muscles of blood vessels, to the kidneys, to changes in the content of leukocytes in the blood and to immunity (to the formation of antibodies).
In the school of V. M. Bekhterev, conditioned (combinative) reflexes to contractions of skeletal muscles, as well as the function of the cardiovascular system, breathing, milk secretion and other vegetative functions were also developed in humans and animals, and their disappearance was proven after the removal of certain areas of the cerebral cortex .
Coordination of motor and autonomic functions in people is observed during hypnosis. With suggestions, the metabolism changes, the secretion of urine and sweat increase, and the blood vessels narrow and dilate. In very rare cases, people could, at will, change the functioning of the heart, the lumen of the pupil, or raise their hair. Suggestion causes changes in muscle function, pulmonary ventilation and gas exchange. It has been proven that coordination of motor and autonomic functions is carried out by the olfactory lobes (G.I. Bukhovets, 1947, S.I. Galperin and K.P. Golysheva, 1949), as well as all subcortical formations.
The preganglionic region of the parasympathetic nervous system includes neurons of the motor nuclei of the III, VII, IX and X pairs of cranial nerves in the brainstem, as well as the second, third and fourth sacral segments of the spinal cord. Therefore, the parasympathetic system is often called the craniosacral half of the autonomic nervous system. Preganglionic fibers extend to the innervated organs, next to which the ganglia are located. In the ganglia there is a synaptic connection between preganglionic and postganglionic fibers, the latter directly innervating the effector organs. Ganglion cells can be grouped in one place (plexus in the muscular lining of the intestine), or located diffusely (in the bladder, blood vessels). The III, VII and IX pairs of cranial nerves innervate the pupil and the secretions of the salivary glands, while the vagus (X pair) nerve gives branches to the heart, lungs, stomach, upper intestines and ureter. Fibers in the sacral region form the pelvic plexuses, which innervate the large intestine, rectum, bladder and genitals. From a physiological point of view, the activity of the parasympathetic nervous system is aimed at preserving and renewing energy reserves in the body. In particular, it reduces heart rate and blood pressure, facilitates the digestion process, absorption of nutrients and excretion of waste.
Table 1. Reactions of various organs to stimulation from the autonomic
nervous system
| Organ | Sympathetic stimulation | Parasympathetic stimulation |
| Heart | Heart rate b1 (and b2) contractility b1 (and b2) conductivity | ° Heart rate ° contractility ° conductivity |
| Arteries | vasoconstriction (a) vasodilation (b2) | Vasodilation |
| Vienna | vasoconstriction (a1) vasodilation (b2) | |
| Lungs | bronchodilation (b2) | Bronchoconstriction secretion in the bronchi |
| Gastrointestinal tract | °motor activity (b2) contraction of the sphincters (a) | physical activity sphincter relaxation |
| Liver | glycogenolysis (b2 and a) gluconeogenesis (b2 and a) lipolysis (b2 and a) | glycogen synthesis |
| Kidneys | Renin secretion (b2) | |
| Bladder | detrusor relaxation (b2) sphincter contraction (a) | detrusor contraction sphincter relaxation |
| Uterus | pregnancy contraction uterus (a) relaxation of pregnant and non-pregnant uterus (b2) | |
| Eyes | dilated pupils (a) | constriction of the pupils secretion of lacrimal glands |
| Submandibular and parotid glands | saliva viscosity | ° saliva viscosity |
The chemical transmitter at both pre- and postganglionic synapses of the parasympathetic system is acetylcholine. In addition, acetylcholine serves as a transmitter in preganglionic sympathetic synapses, in a number of postganglionic sympathetic synapses, neuromuscular synapses (somatic nervous system), as well as in some areas of the central nervous system. Nerve fibers that release acetylcholine from their endings are called cholinergic. Acetylcholine synthesis occurs in the cytoplasm of nerve endings; its reserves are stored in the form of vesicles in presynaptic terminals. The occurrence of a presynaptic action potential leads to the release of the contents of several hundred vesicles into the synaptic cleft. Acetylcholine released from these vesicles binds to specific receptors on the postsynaptic membrane, which increases its permeability to sodium, potassium and calcium ions and leads to the appearance of an excitatory postsynaptic potential. The action of acetylcholine is limited by its hydrolysis by the enzyme acetylcholinesterase. From a pharmacological point of view, specific cholinergic receptors are divided according to the action of the alkaloids muscarine and nicotine. The effects of acetylcholine at the preganglionic synapses of the parasympathetic and sympathetic systems can be reproduced by administering nicotine, which is why all autonomic ganglia are called nicotinic ganglia. Nicotine-like transmission of nerve impulses also occurs at the neuromuscular junction, the central nervous system, the adrenal medulla, and in some sympathetic postganglionic areas (see below). However, the action of acetylcholine in the area of postganglionic nerve endings is reproduced by another alkaloid = muscarine. In addition to postganglionic synapses, muscarinic-like transmission of nerve impulses occurs in some areas of the central nervous system.
Pages: 1
see also
Restoring physical performance One of the main and urgent tasks of sports psychology is the development of effective practical methods of psychological training that would help athletes adapt...
Occupational health in the production of ammonia and nitric acid. Course work The production of ammonia and nitric acid at most plants is combined, since the final product of the first production - ammonia - is the raw material of the second. Nitric acid is...
Healthy lifestyle and psychology The end of the 20th century is characterized, in particular, by an increase in morbidity and mortality of the population against the background of high achievements in medicine, the improvement of technical means for diagnosing and treating diseases...
Anatomy
The sympathetic nervous system is divided into central, located in the spinal cord, and peripheral, which includes numerous nerve branches and nodes connected to each other. The centers of the sympathetic system (Jacobson's spinal center) are located in the lateral horns of the thoracic and lumbar segments. Sympathetic fibers exit the spinal cord from the I-II thoracic to the II-IV lumbar segment. Along their course, the sympathetic fibers are separated from the motor somatic ones, and then, in the form of white connecting branches, they enter the nodes of the borderline sympathetic trunk.
The peripheral part of the sympathetic nervous system is formed by efferent and sensory neurons with their processes located in the paravertebral and prevertebral nodes remote from the spinal cord.
The sympathetic nervous system is activated during stress reactions. It is characterized by a generalized influence, with sympathetic fibers innervating all organs without exception.
The main transmitter released by preganglionic fibers, as in the parasympathetic nervous system, is acetylcholine, and by postganglionic fibers - norepinephrine.
Test with answers: “Autonomic nervous system”
1. The centers of the sympathetic nervous system are located in: a) Lateral horns of the spinal cord + b) Anterior horns of the spinal cord c) Brain stem
2. The centers of the parasympathetic nervous system are located in: a) Anterior horns of the spinal cord b) Brain stem + c) Lateral horns of the spinal cord +
3. The main transmitter of the sympathetic nervous system is: a) Serotonin b) Adrenaline c) Norepinephrine +
4. Coordination of the work of all parts of the autonomic nervous system is carried out by: a) Hypothalamus + b) Spinal cord c) Cerebral cortex +
5. Sequence of sections of the autonomic nervous system: 1 – Autonomic nuclei in the spinal cord and brain; 2 – Autonomic nodes (ganglia); 3 – Postganglionic fibers; 4 – Preganglionic fibers: a) 2, 4, 3, 1 b) 3, 2, 1, 4 c) 1, 4, 2, 3 +
6. The nuclei of the parasympathetic nervous system are part of the following cranial nerves: a) Oculomotor + b) Trigeminal c) Vagus +
7. The plexus, which surrounds the end of the abdominal aorta, innervates the rectum, bladder, genitals: a) Inferior mesenteric b) Celiac c) Hypogastric +
8. Between the adrenal glands there is: a) Celiac plexus + b) Hepatic plexus c) Diaphragmatic plexus
9. What are the names of the nerve plexuses that are located around the vessels: a) Intramural b) Extramural c) Extraorgan +
10. Pelvic splanchnic nerves are just such fibers of the parasympathetic nervous system: a) Postganglionic b) Preganglionic + c) no correct answer
11. Indicate the anatomical structures related to the central part of the autonomic nervous system: a) Superior salivary nucleus b) Nuclei parasympathici sacrales c) Nucleus accessorius d) all options are correct + e) there is no correct answer
12. Indicate the internal organs innervated from the nucleus dorsalis nervi vagi: a) Transverse colon b) Esophagus c) Sigmoid colon d) all options are correct + e) there is no correct answer
13. Specify the prevertebral autonomic nodes: a) Cervicothoracic ganglion b) Aorticorenal ganglion c) Superior mesenteric ganglion
14. Indicate the anatomical structures innervated from the submandibular ganglion: a) Sublingual salivary gland + b) Submandibular salivary gland + c) Tongue
15. Indicate the anatomical structures through which nerve impulses pass from the parasympathetic nuclei of the spinal cord to the rectum: a) Plexus pelvinus + b) Lumbar plexus c) Lumbar splanchnic nerves +
16. Indicate the nuclei of the head section of the parasympathetic nervous system: a) Nucleus of the accessory nerve + b) Dorsal nucleus of the vagus nerve + c) no correct answer
17. Indicate the branches that extend from the nodes of the sympathetic trunk: a) Rami communicantes grisei b) Nervi splanchnici c) Rami interganglionares d) all options are correct + e) there is no correct answer
18. Indicate the branches extending from the ganglion cervicothoracicum: a) Rami communicantes grisei b) Nervus cardiacus cervicalis medius c) Rami communicantes albi, Nervus vertebralis +
19. Indicate the parasympathetic nodes on the head: a) Ganglion pterygopalatinum b) Ganglion ciliare c) Ganglion stellatum d) all options are correct + e) there is no correct answer
20. Indicate the anatomical structures innervated from the ciliary ganglion: a) Pupil sphincter + b) Pupil dilator muscle c) Ciliary muscle +
21. Indicate the branches extending from the middle cervical ganglion: a) Rami communicantes grisei + b) Nervus cardiacus cervicalis superior c) Rami communicantes albi
22. Indicate the branches that approach the nodes of the sympathetic trunk: a) Rami interganglionares + b) Rami communicantes albi + c) Rami communicantes grisei
23. Indicate the anatomical structures through which nerve impulses pass from the sympathetic nuclei of the spinal cord to the stomach: a) Nervus splanchnicus minor b) Ganglia coeliaca c) Ganglia trunci sympathici
24. Indicate the anatomical structures through which nerve impulses pass from the sympathetic nuclei of the spinal cord to the stomach: a) Nervus splanchnicus minor b) Ganglion mesentericum inferius c) Ganglia trunci sympathici d) all options are correct + e) there is no correct answer
25. Indicate the anatomical structures related to the peripheral part of the autonomic nervous system: a) Pravertebral sympathetic ganglia b) Autonomic ganglia c) Intramuscular plexus d) all options are correct + e) there is no correct answer
26. Indicate the branches of the nodes of the thoracic sympathetic trunk: a) Nervi cardiaci thoracici b) Rami communicantes albi c) Rami communicantes grisei d) all options are correct + e) there is no correct answer
27. Indicate the anatomical structures through which nerve impulses pass from the sympathetic nucleus of the spinal cord to the parotid gland: a) Rami communicantes albi b) Rami communicantes grisei c) Rami interganglionares d) all options are correct + e) there is no correct answer
28. Indicate the anatomical structures that make up the solar plexus: a) Iliohypogastric nerve b) Vagus nerve c) Aorticorenal ganglion d) all options are correct + e) there is no correct answer
29. Indicate the anatomical structures through which nerve impulses pass from the sympathetic nuclei of the spinal cord to the rectum: a) Inferior mesenteric plexus b) Inferior infraorbital plexus c) Lubosacral plexus d) all options are correct + e) there is no correct answer
30. Indicate the peripheral nodes belonging to the parasympathetic part of the autonomic nervous system: a) Ganglia intramuralia + b) Ganglia prevertebralia c) Ganglia paraorgana +
Mediators of the sympathetic and parasympathetic nervous system
Read:- I. Neurogenic tumors from the nervous tissue itself.
- I. Opposing Philosophical Systems
- II. Immune system cells
- IV. Anatomy of the organs of the cardiovascular system
- IV. Endocrine system response to hypoglycemia
- V. Organs of the lymphatic system, immune system
- VI. Anatomy of the central nervous system
- VII. Anatomy of the peripheral nervous system
- A) with increased tone of the sympathetic nervous system
- A. Assessment of the state of the hypothalamic-pituitary-adrenal system
Acetylcholine is released in preganglionic fibers of both the sympathetic and parasympathetic nervous systems. It interacts with H-cholinergic receptors (nicotine-sensitive receptors) of neurons of the autonomic ganglia. As a result, excitation is transferred from the preganglionic fiber to the ganglion neuron. N-cholinergic receptors of ganglia, as a rule, are not blocked by curare-like substances (unlike skeletal muscles, where N-cholinergic receptors are highly sensitive to curare), but are blocked under the influence of ganglion blockers, for example, benzohexonium. Regarding nicotine, in small concentrations it excites H-cholinergic receptors, and in large concentrations it inhibits and blocks (including those contained in tobacco smoke).
In addition, the autonomic ganglion contains neuropeptides: methenkephalin, neurotensin, cholecystokinin, substance P, but they have a modulating effect.
Postganglionic fibers of the sympathetic nervous system, as a rule, are monoaminergic (the main transmitter is norepinephrine - 90%, adrenaline - 7% and dopamine - 3%). An exception is that acetylcholine is released in the postganglionic sympathetic fibers of the sweat glands, which interacts with M-cholinergic receptors (muscarine-sensitive), causing stimulation of the sweat glands and sweating.
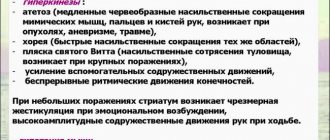
In order for the effect of norepinephrine to manifest itself, it must interact with adrenergic receptors. There are alpha and beta adrenergic receptors. When interacting with the alpha adrenergic receptor, the permeability of the membrane for sodium ions changes, depolarization occurs and, as a result, excitation and enhancement of organ function. When interacting with beta-adrenergic receptors, there is an increase in potassium flow, hyperpolarization and, accordingly, inhibition and decrease in organ function. An exception is that the interaction of norepinephrine with cardiac beta-AR causes increased cardiac activity. In addition, NA, when interacting with the adrenergic receptor, can increase the activity of adenylate cyclase, which leads to the formation of cAMP (an intracellular messenger - intermediary). This leads to the activation of protein kinases, which are intracellular regulators of the synthesis of various proteins.
The mechanism of self-regulation of transmitter release - NA acts on the presynaptic membrane, which has alpha and beta AR. Interaction with alpha-AR reduces the release of the transmitter, and interaction with beta-AR increases the release of the transmitter (positive feedback).
The final effect depends on which population of adrenergic receptors predominates in the organ on the pre- and postsynaptic membrane.
Alpha-AR blockers - phentolamine, beta-AR - anaprilin (widely used to lower heart rate and blood pressure). Both types of receptors are divided into two subtypes alpha-1 and alpha-2, beta-1 and beta-2 AR. Antagonists:
alpha-1-AR - prazosin, droperidol
alpha-2-AR - rauwolsin, yohimbine
beta-1-AR - practolol, atenolol
beta-2-AR - butoxamine
In general, the sympathetic nervous system contributes to a significant increase in the body’s performance - glycogenolysis, lipolysis, and cardiovascular activity are enhanced, pulmonary ventilation is improved, and blood is redistributed from areas resistant to hypoxia to organs that need oxygen. At the same time, there is inhibition of the gastrointestinal tract, relaxation of the bladder, uterus, spasm of the sphincters, and dilation of the bronchi.
Postganglionic fibers of the parasympathetic nervous system are cholinergic. Acetylcholine, released in nerve endings, interacts with M-cholinoreceptors (muscarine-sensitive) of the effector organ. Muscarine is a fly agaric toxin that activates this type of receptor and causes the same effects as acetylcholine. There are 5 subtypes of M1-M5 cholinergic receptors.
M-ChR blockers - atropine and scopolamine, hemicholine.
Effects of the parasympathetic nervous system: increased gastrointestinal motility, contraction of the bladder muscles, relaxation of the sphincters, narrowing of the lumen of the bronchi, constriction of the pupil, inhibition of cardiac activity, dilation of the vessels of the genital organs, erection, increased secretion of all glands.
Date added: 2015-01-12 | Views: 2361 | Copyright infringement
| | | 4 | | | |