The sympathetic trunk is part of the peripheral sympathetic nervous system, the main elements of which are the paravertebral nodes, connected to each other by internodal branches. The sympathetic part has a segmental appearance and structure, and also performs the main trophic function, consisting of increasing or slowing respiration, cardiac activity, responsible for oxidative processes and the supply of oxygen to muscle tissue, as well as for the consumption of nutrients by all elements of the body.
Anatomical structure
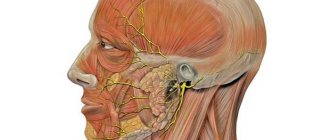
Sympathetic trunk of the cervical region
The human anatomy of the sympathetic trunk includes from 20 to 25 autonomic ganglia of the 1st order, located on the lateral parts of the spine on the anterior side. They go from the tailbone to the base of the skull. In the area of the coccyx, the trunks connect and form a ganglion. In the region of the C8-L2 vertebrae, the nodes connect to the white communicating branches of the spinal cord. Gray connective fibers depart from the ganglia, which serve as conductors for neurons. Each of the ganglia is connected by gray branches to the spinal nerves. Parasympathetic trunks are formed in the cervical, thoracic and lumbar regions. In each of them there is a different combination of nodes.
Structure of the cervical spine
In the cervical spine there are three fiber nodes located at Th7 and C8. The internodal branches of the sympathetic trunk reach the ascending trunk. The following nodes are distinguished:
- Upper. It is located in front of the C2-C3 processes, has the largest size and reaches 2.5 cm in its maximum length. It contains several postganglionic fibers that form many nerve endings, including the internal carotid nerve. This internal nerve accompanies the carotid artery and innervates the deep petrosal nerve. From here there are endings to the ophthalmic plexus and ciliary ganglion. Also, the upper cervical node is responsible for the formation of the jugular, laryngeal-pharyngeal nerve and the common carotid plexus. The external carotid nerve and its endings depart from it. In the lower part there are gray connecting nerves, which are intertwined with 1-4 chains of spinal roots. It is also responsible for the formation of the upper cervical cardiac nerve.
- Middle node. It begins in the area of the C6 process, gives off such nerves as: the middle cardiac cervical, going to the deep plexus, the gray connective, located at the 5-6 spinal roots.
- Bottom node. The element is located in the area of the head of the 1st rib and is located behind the subclavian artery. From it comes the subclavian loop, the branches of which extend from the middle cervical ganglion and envelop the subclavian artery. The lower cervical cardiac nerve, spinal nerve and gray connecting branches from the 7th and 8th spinal roots are also located here.
The cervical section of the nodes of the sympathetic trunk is the most extensive, diverges into hundreds of small endings and provides nutrition and composition of the nerves of many other elements.
Thoracic region
The structure of the sympathetic trunk
There are 10 to 12 nodes in the thoracic sympathetic trunk, which look like elongated fusiform nodules located in front of the costal heads. This is where these nerves originate:
- elements of the thoracic aorta;
- great internal nerve;
- small internal nerve;
- low splanchnic nerve 12 thoracic ganglion, which is absent in some people;
- thoracic cardiac nerves located in the zone of 2-5 nodules;
- pulmonary and esophageal endings from 2 to 5 nodes.
The position of these endings largely depends on the individual characteristics of the organism and may differ.
Lumbar and sacrococcygeal regions
In the lumbar zone there are from 3 to 5 nodes, delimited by the right and left positions with side branches. They form the lumbar splanchnic nerves. In the sacral region, the nodes are divided into 4 paired and 1 unpaired. They come from the midsacral foramen and are connected by transverse branches. From them the splanchnic nerves go to the sympathetic node.
Sympathetic trunk
The sympathetic trunk (truncus sympathicus) is paired, formed by nodes connected by sympathetic fibers. The sympathetic trunk is located on the lateral surface of the spine along its entire length. Each node of the sympathetic trunk represents a cluster of autonomic neurons, with the help of which most of the preganglionic fibers are switched, emerging from the spinal cord and forming the white connecting branches (rr. communicantes albi). Preganglionic fibers contact vegetative cells in the corresponding node or are sent as part of internodal branches to the superior or inferior nodes of the sympathetic trunk. The white connecting branches are located in the thoracic and upper lumbar regions. There are no such connecting branches in the cervical, sacral and lower lumbar nodes. The nodes of the sympathetic trunk are also connected by special fibers to the spinal nerves - the gray connecting branches (rr. communicantes grisei), consisting mainly of postganglionic sympathetic fibers. The gray connecting branches extend from each node of the sympathetic trunk to each spinal nerve, within which they are directed to the periphery, reaching the innervated organs - striated muscles, smooth muscles and glands.
The sympathetic trunk is conventionally divided into cervical, thoracic, lumbar and sacral sections.
The cervical sympathetic trunk includes three nodes: superior, middle and inferior.
The upper node (gangl. cervicale superius) has a spindle-shaped shape measuring 5x20 mm. Located on the transverse processes of the II-III cervical vertebrae, covered with prevertebral fascia. Seven main branches depart from the node, containing postganglionic fibers to innervate the organs of the head and neck.
1. Gray connecting branches to the I, II, III cervical spinal nerves.
2. The jugular nerve (n. jugularis) is divided into two branches, the fibers of which join the vagus and glossopharyngeal nerves in the region of their lower nodes, and into a branch, the fibers of which join the hypoglossal nerve.
3. The internal carotid nerve (n. caroticus internus) penetrates the adventitia of the internal carotid artery, where its fibers form the plexus of the same name. From the plexus of this artery at the site of its entry into the carotid canal of the temporal bone, sympathetic fibers are separated, forming the deep petrosal nerve (n. petrosus profundus), passing into the pterygoid canal (canalis pterygoideus) of the sphenoid bone. Having left the canal, they pass through the pterygopalatine fossa, connecting to the postganglionic parasympathetic nerves of the pterygopalatine ganglion and the sensory nerves n. maxillaris, and diverge to the facial organs. Branches extend from the internal carotid plexus in the carotid canal, penetrating into the tympanic cavity, participating in the formation of the plexus of the tympanic cavity (plexus tympanicus). In the cranial cavity, the continuation of the internal carotid plexus is the cavernous one, the fibers of which are distributed along the branches of the cerebral vessels, forming the plexus of the anterior, middle cerebral arteries (plexus arteriae cerebri anterior et medius), as well as the plexus of the ophthalmic artery (plexus ophthalmicus). Branches extend from the cavernous plexus and pass into the ciliary parasympathetic ganglion (gangl. ciliare), connecting to its parasympathetic fibers to innervate the muscle that dilates the pupil (m. dilatator pupillae).
4. The external carotid nerve (n. caroticus externus) is thicker than the previous one. Around the artery of the same name, it forms an external plexus (plexus caroticus externus), from which the fibers are distributed to all its arterial branches, supplying blood to the facial part of the head, dura mater and neck organs.
5. The laryngopharyngeal branches (rr. laryngopharyngei) are distributed along the vessels of the pharyngeal wall, forming the pharyngeal plexus (plexus pharyngeus).
6. The superior cardiac nerve (n. cardiacus superior) is sometimes absent on the right and descends next to the cervical section of the sympathetic trunk. In the chest cavity, it participates in the formation of the superficial cardiac plexus, located under the aortic arch.
7. The branches that make up the phrenic nerve end in the pericardium, pleura, diaphragm, parietal peritoneum of the diaphragm, ligaments and liver capsule.
The middle node (gangl. cervicale medium), measuring 2×2 mm, is located at the level of the VI cervical vertebra at the intersection of the inferior thyroid and common carotid arteries; often absent. Four types of branches extend from this node:
1. Gray connecting branches to the V and VI cervical spinal nerves.
2. Middle cardiac nerve (n. cardiacus medius), located behind the common carotid artery. In the chest cavity, it takes part in the formation of the deep cardiac plexus, located between the aortic arch and the trachea.
3. Branches involved in the formation of the nerve plexus of the common carotid and subclavian arteries, as well as the plexus of the inferior thyroid artery. Autonomic plexuses are formed in these organs.
4. Internodular branch to the superior cervical sympathetic node.
The lower node (gangl. cervicale inferius) is located above the subclavian artery and behind the vertebral artery. Sometimes it connects with the first thoracic sympathetic node and is called the cervicothoracic (stellate) node (gangl. cervicothoracicum s. stellatum). 6 branches extend from the lower node.
1. Gray connecting branches to the VII and VIII cervical spinal nerves.
2. Branch to the plexus of the vertebral artery (plexus vertebralis), which extends into the skull, where it forms the basilar plexus and the plexus of the posterior cerebral artery.
3. Lower cardiac nerve (n. cardiacus inferior), located on the left behind the aorta, on the right - behind the brachiocephalic artery; takes part in the formation of the deep plexus of the heart.
4. Branches to the phrenic nerve do not form a plexus. Reach the pleura, pericardium and diaphragm.
5. Branches to the plexus of the common carotid artery (plexus caroticus communis).
6. Branches to the subclavian artery (plexus subclavius).
Thoracic nodes (ganglia thoracica) are located on the sides of the thoracic vertebrae on the necks of the ribs, covered with the parietal pleura and intrathoracic fascia (f. endothoracalis). The thoracic sympathetic ganglia have mainly six groups of branches:
1. The white connecting branches enter the nodes from the anterior roots of the intercostal nerves (Fig. 532).
2. Gray connecting branches extend from the nodes to the intercostal nerves.
3. Mediastinal branches (rr. mediastinales) start from the V superior sympathetic nodes and enter the region of the posterior mediastinum. They take part in the formation of the esophageal and bronchial plexuses.
4. Thoracic cardiac nerves (nn. cardiaci thoracici) start from the IV-V superior sympathetic nodes and are part of the deep cardiac plexus and the thoracic aortic plexus.
5. The great splanchnic nerve (n. splanchnicus major) is formed from the branches of the V-IX thoracic sympathetic nodes. The nerve is located under the intrathoracic fascia. Through the hole between the medial and intermediate crura of the diaphragm, the large splanchnic nerve penetrates the abdominal cavity, ending in the celiac plexus nodes. The nerve contains a large number of preganglionic fibers, which switch in the nodes of the celiac plexus to postganglionic fibers, and fewer postganglionic fibers, which have already switched in the thoracic nodes of the sympathetic trunk.
6. The small splanchnic nerve (n. splanchnicus minor) is formed from the branches of the X-XII nodes. It descends through the diaphragm lateral to the greater splanchnic nerve and reaches the celiac plexus. Preganglionic fibers switch to postganglionic fibers in the sympathetic ganglia, and another group of preganglionic fibers, switched in the thoracic ganglia, are sent to the organs.
The lumbar nodes (ganglia, lumbalia) of the sympathetic trunk are a continuation of the chain of nodes of the thoracic part, located between the lateral and intermediate legs of the diaphragm. They include 3-4 nodes located on the sides of the spine on the medial edge of m. psoas major. On the right, the nodes are visible lateral to the inferior vena cava, and on the left, lateral to the aorta. Branches of the lumbar sympathetic ganglia:
1. White connecting branches approach only the I, II nodes from the I and II lumbar spinal nerves.
2. The gray communicating rami connects the lumbar ganglia with all lumbar spinal nerves.
3. Lumbar splanchnic nerves (nn. splanchnici lumbales) from all nodes are connected to the celiac (plexus celiacus), renal (plexus renalis), superior mesenteric (plexus mesetericus superior), abdominal aortic (plexus aorticus) and superior hypogastric (plexus hypogastricus superior) , plexuses.
The sacral nodes (ganglia sacralia) of the sympathetic trunk include 3-4 paired sacral and 1 unpaired coccygeal nodes, which are located medial to the anterior sacral foramina.
1. Gray communicating branches go to the spinal and sacral nerves.
2. The splanchnic nerves (nn. splanchnici sacrales) participate in the formation of the autonomic plexuses of the pelvis. The visceral branches form the inferior hypogastric plexus (plexus hypogastricus inferior), located on the branches of the internal iliac artery; along its branches, the sympathetic nerves reach the pelvic organs.
Functions of the sympathetic trunk
Functions for which the sympathetic trunk of the cervical spine is responsible
Based on the anatomical features of the sympathetic trunk, ganglia and nerves, it is clear that its main function is innervation, which is responsible for the following zones:
- head and neck – contraction of blood vessels, their narrowing and dilation as part of a normal reaction to external stimuli;
- providing impulse reactions to the vascular walls of the thyroid, subclavian and carotid arteries, as well as the largest artery in the body - the aorta;
- supplying the organs of the thoracic cavity - the branches of the sympathetic trunk are part of the pericardium, liver, nerves of the pleura and diaphragm;
- innervation of ganglia and their connection with nerve endings, including in the solar coupling zone;
- formation of plexuses - aortic, renal, celiac, superior mesenteric;
- innervation of the pelvic organs due to the origin of branches to the lower hypogastric plexuses.
Violation of these functions can lead to serious consequences and syndromes requiring medical correction.
The functioning of the sympathetic trunk affects the overall correctness of the parasympathetic nervous system. Lack of innervation can lead to vasospasm, which can be caused by tumors, vascular disorders and diseases of the nervous system.
Effect of the sympathetic nervous system on organs
Excitation of the structures of the nervous system affects the functioning of internal organs. In order to understand how sympathetic nerves influence internal organs, it is necessary to consider each anatomical formation separately. However, it is necessary to take into account that the sympathetic nervous system acts in different directions and in a variety of ways, so we will consider its influence on the main anatomical structures.
Effect of the sympathetic nervous system on the heart
This section of the autonomic nervous system takes an active part in the regulation of cardiac activity. The sympathetic nervous system reduces the heart rate, regulates its rhythm and strength. This is due to the fact that the ventricles are controlled primarily by sympathetic nerves. The cardiovascular center is localized in the medulla oblongata, combining the parasympathetic, vasomotor and sympathetic centers.
The influence of the sympathetic nervous system on blood vessels
As a result of excitation of adrenergic fibers, the tone of blood vessels increases. Adrenaline is released in the area of nerve endings. This causes irritation of the sympathetic nerves and increases blood pressure. When nerve impulses in the sympathetic fibers are inhibited, a decrease in the tone of the muscle fibers is observed, which dilates the blood vessels. As a result, the opposite effect is observed - a decrease in blood pressure. The sympathetic nervous system regulates the increase in vascular resistance:
- skeletal muscles;
- skin;
- spleen;
- intestines;
- kidney;
- liver.
How does the sympathetic nervous system affect diuresis?
The influence of the sympathetic nervous system on the kidneys is manifested in changes in diuresis. Changes are possible both smaller and larger. When the arteries of the afferent section narrow, a decrease in filtration pressure is observed. As a result, the sympathetic nervous system reduces urine production. When the lumen of the efferent arteries of the glomerular system decreases, the pressure in the urinary system increases, which leads to an increase in the volume of urine excreted by the body.
How does the sympathetic nervous system affect breathing?
By expanding the lumen of the bronchi, the sympathetic nervous system increases ventilation of the lungs. Irritation of the fibers leads to an increase in the frequency of respiratory movements and the depth of inspiration. This helps saturate the bloodstream and internal organs with oxygen. The sympathetic nervous system enhances respiratory processes in situations of stress, which are accompanied by an increase in the concentration of adrenaline in the blood.
Anatomy and nodes of the sympathetic trunk
The sympathetic trunk (also called the borderline sympathetic trunk) is a paired organ, part of the body’s sympathetic system, located on the anterolateral part of the spine. Below you will find out what role the sympathetic trunk plays in the human body and what are the consequences of disruption of its functions.
Superior cervical sympathetic ganglion syndrome
Symptoms of the development of the syndrome are:
- disturbances in the functioning of the facial muscles;
- paroxysmal pain of a burning nature. In this case, the attack can pass in either a couple of hours or several days;
- radiating pain to the neck and shoulders. In this case, the pain is usually localized in the back of the head;
- drooping of the upper and raising of the lower eyelid, which reduces the size of the palpebral fissure;
- decreased tone of the orbital muscle;
- the color of the iris becomes lighter;
- reduction or cessation of sweating.
Stellate (cervicothoracic) node syndrome
This syndrome manifests itself with the following symptoms:
- pain in the area of the 5th-6th pair of ribs;
- pain in the arm on the affected side;
- impaired sweating in the affected area;
- reduction in pain sensation.
Posterior cervical syndrome
This syndrome occurs due to compression, the development of an infectious or inflammatory process, or a violation of the circulatory process. Most often, damage to the sympathetic plexus occurs due to the development of osteochondrosis.
Symptoms of the development of posterior cervical sympathetic syndrome are:
- severe headache that does not go away for a day or more. As a rule, pain is localized on the affected side and has an increasing or paroxysmal character;
- vomiting caused by a very severe headache;
- tinnitus, hearing loss;
- hot flashes, sudden redness of the face;
- numbness or shaking of the hands;
- pain in the face in the throat area;
- unnatural tilt of the head in the affected area;
- photophobia;
- pain in the area of the eyeball;
- blurred vision.
Jugular foramen syndrome
This disease occurs due to damage to the accessory, vagus or glossopharyngeal nerve. The syndrome is usually caused by trauma or tumors.
Treatment
Treatment is aimed simultaneously at:
- anesthesia. In this case, painkillers are prescribed, and in severe cases, tranquilizers. To speed up the effect, medications are administered intravenously;
- treatment of a viral or bacterial infection. For this, antiviral drugs or antibiotics are prescribed;
- To normalize the tone of sympathetic structures, cholinomimetic drugs are prescribed.
Physiotherapy procedures have a good effect: cold mud applications, UV irradiation, radon baths. It is advisable to take a massage course.
So, the sympathetic trunk is an element of the human sympathetic nervous system, which is responsible for the constancy of the internal environment of any person. Any problems with this organ are fraught with serious systemic disorders in the patient’s body and require immediate intervention.
You have no rights to post comments
Feb 03, 2020 4158
in Vessels
Treatment of carotid cavernous anastomosis Carotid cavernous anastomosis is a vascular intracranial acquired pathology in which a communication is formed…
Jan 05, 2020 7639
in Muscles of the neck and head: anatomy, tables and functions
Sleepy triangle Most people are not familiar with the definition of a sleepy triangle. But, despite its little fame, this area of the bodily structure...
Feb 01, 2020 7394
in Vessels
Where is the vena cava located: functions, diseases The human circulatory system consists of many vessels that differ in size and function. The largest vessel...
Source: https://sheia.ru/sosudy/228-simpaticheskij-stvol.html
Sympathetic nervous system disorder
Improper functioning of the sympathetic nervous system leads to failure in all internal organs. However, it is not always possible to immediately identify deviations: the symptoms of the disorder are similar to multinomial pathologies. Only after a comprehensive diagnosis and identification of the possible cause of the deviation can it be possible to prescribe effective treatment. In this case, the sympathetic nervous system is often treated with non-drug methods.
Sympathetic nervous system disorder - causes
Among the pathological factors that, under certain conditions, affect the sympathetic nervous system, there are many causes. Often doctors are unable to accurately determine what causes the disease. However, in most cases, doctors associate deviations with:
- chronic stress;
- bad heredity;
- hormonal imbalances;
- unhealthy lifestyle (sedentary lifestyle, unbalanced diet);
- allergic reactions;
- therapy with potent drugs.
Sympathetic nervous system disorder - symptoms
The fact that the sympathetic autonomic nervous system is affected can be assumed by certain clinical signs. Pathological conditions provoked by damage to the sympathetic nervous system are accompanied by the development of the following syndromes:
- Cardiovascular
- manifests itself in changes affecting the functioning of the heart: heart rhythm disturbances, bradycardia, pressure changes, sudden periodic pain in the heart. - Digestive disorders
- abdominal discomfort, loss of appetite, nausea, feeling of a lump in the throat may indicate problems with the sympathetic nervous system. - Disruption of the urinary system
- frequent pain, frequent urination, increased volume of urine released by the body. - Violation of thermoregulatory processes
- the appearance of a feeling of heat or, on the contrary, chills.
Sympathetic nervous system disorder - treatment
When a person's sympathetic nervous system begins to malfunction, it provokes the development of a large number of pathological conditions. It is important to determine what caused the violation. The treatment algorithm will depend directly on the cause. All therapy methods can be divided into:
- Non-drug
- lifestyle changes, balanced diet, sufficient level of physical activity. - Medication
– determined by the nature of the disorder and the cause of its development. Pathologies in which there is a violation of the sympathetic nervous system often require the prescription of drugs to normalize the cardiovascular system, antidepressants, herbal remedies, and vitamins.
Autonomic nervous system, structure and functions that regulate
The autonomic nervous system (ANS) is an autonomous part responsible for the functioning of absolutely all internal human organs, adequate metabolism, blood circulation and adaptation to constantly changing environmental conditions.
Structure
The anatomy of the ANS is quite complex and confusing; to facilitate its study, it is usually divided into several sections; first of all, it is necessary to consider the central and peripheral ones.
The central part is represented by the nuclei of some pairs of cranial nerves, which lie deep in the tissues of the brain and spinal cord. The midbrain contains centers responsible for the diameter of the pupil and the functioning of the eye; in the nervous tissue of the medulla oblongata and the sacral segment of the spinal cord there are fibers responsible for the functioning of the gastrointestinal tract, heart, liver and other organs.
A special place in the central department is occupied by the hypothalamus and limbic structure. The first has three groups of nuclei, is responsible for the work of all endocrine and exocrine glands, regulates the act of breathing, the tone of the arteries and veins. The limbic structure is involved in behavioral reactions, with its help a person is able to make plans, dreams and can stay awake during the day.
The peripheral section consists of autonomic nerves, plexuses, endings, sympathetic trunk and parasympathetic ganglia. The first three parts bring the electrical impulse to the required target, that is, to a certain area of the body, organ, and so on. The next two parts are part of two fundamentally different, but very important divisions of the ANS: parasympathetic and sympathetic.
- The parasympathetic autonomic nervous system transmits its impulses through the production of a special transmitter – acetylcholine. Consists of long presynaptic and short postsynaptic fibers. It does not innervate the brain, the smooth muscle wall of blood vessels, with the exception of some organs, skeletal muscles, and almost all sensory organs. This department is responsible for the release of saliva into the oral cavity, reducing heart rate and blood pressure, providing bronchospasm, peristalsis of the small and large intestines and other necessary functions.
- The sympathetic autonomic nervous system consists of sympathetic chains, ganglia connected by nerve fibers and located on either side of the spine, as well as the celiac plexus and mesenteric ganglia. Adrenal hormones participate in the transmission of nerve impulses: adrenaline and norepinephrine, therefore they are activated in stressful situations. Basically it enhances the work of internal organs, but there are exceptions, which are discussed below.
Functions
The autonomic nervous system regulates the functioning of almost every cell in the body and normalizes metabolic processes. If we consider the influence of each of the departments, we can form a whole list of systems that affect the production of certain biologically active substances. The functions of the autonomic system are also divided into two large parts.
When the sympathetic part functions:
- From the side of the cardiovascular system: the heart rate increases, the pressure on the walls of the arteries increases due to a decrease in their lumen, the force and release of blood into the main vessels (aorta and pulmonary artery) increases;
- On the part of the respiratory system: increases the respiratory rate, expands the bronchi, thereby providing increased ventilation of the lungs and greater oxygen delivery to the organ systems, the secretion of the glands of the ciliated epithelium is reduced;
- From the side of the bladder: the ducts and the wall of the bladder itself relax;
- From the digestive system: peristalsis of the small and large intestines decreases, the tone of the sphincters of the gastrointestinal tract and the secretion of accessory glands of the stomach increases, the gallbladder itself and its ducts relax;
- On the part of the external and internal secretion glands: the production of both enzymes and hormones increases, and metabolism accelerates accordingly - protein synthesis, energy supply and other vital processes;
- From the senses: affects mainly the eye, or rather dilates the pupil, contracts the oculomotor muscles.
When the parasympathetic department is turned on:
- From the cardiovascular system: a decrease in heart rate up to cardiac arrest, the strength of contractions also decreases, the conduction of impulses slows down, atrioventricular block may develop, blood pressure drops;
- On the part of the respiratory system: the tone of the smooth muscle wall of the bronchi increases, bronchospasm forms, the secretion of glands secreted from goblet cells increases, the respiratory rate becomes lower;
- From the senses: the diameter of the pupil decreases, the oculomotor muscles relax;
- From the digestive system: motility of the gastrointestinal tract increases, sphincter tone decreases, secretion production from the main and parietal glands of the stomach increases, the ducts of the gallbladder and the organ itself contract;
- From the side of the external and internal secretion glands: metabolism decreases, glycogen is synthesized to a greater extent in the liver, the concentration of glucose in the blood falls, the amount of hormones secreted also decreases;
- From the bladder: the bladder wall contracts, the sphincter relaxes, which facilitates urination.
Differences from the somatic nervous system
The somatic nervous system (SNS) is voluntary, that is, controlled by the human consciousness. It is responsible for the contraction of striated muscle tissue, that is, mainly for the motor activity of the musculoskeletal system.
The autonomic nervous system is very different in structure and function. As far as anatomy is concerned, the differences mainly concern the reflex arcs and the origin of the nerve fibers. The reflex arc itself in both parts consists of three parts: sensitive, intercalary and executive.
In most cases, the sensitive link is common in both types, but the executive link has a different localization. In the case of the ANS, it is located outside the central nervous system, that is, in close proximity to the target organ.
The SNS arc ends in the spinal cord, in its gray matter.
The nerve fibers of the ANS are smaller in diameter, they are not fully covered with the myelin sheath, and have a lower speed of electrical impulse conduction, so a more powerful irritating factor is needed to conduct it . The axons of neurons are short and interrupted in the ganglia. The SNS is the complete opposite: the fibers are larger, all myelinated, the speed is higher, the axons are continuous and longer.
As for neurotransmitters, the biologically active substance of the somatic nervous system is acetylcholine alone, which regulates the transmission of all impulses. The autonomic nervous system is very diverse; its mediators are norepinephrine and adrenaline, histamine, acetylcholine, serotonin, adenosine triphosphoric acid and others.
Formation during embryogenesis
The nervous system itself is formed from the ectoderm. In the third week of fetal growth, sympathetic trunks and nodes begin to form from neuroblasts migrating from the neural tube, at the same time they strive to localize future internal organs.
Initially, sympathetic nodes form in the intestinal wall, then in the heart tube. All processes end by the end of the seventh week of embryo development.
The parasympathetic nervous system initially appears in the facial area from the same neuroblasts separated from the head end of the neural tube.
At the same time, the autonomic centers of the spinal cord develop; they originate from sympathoblasts. Here embryonic development begins from the thoracic to lumbar segment.
The formation of higher nervous activity begins with the formation of the brain, and this is the second month of embryogenesis.
It is during this period that the limbic system, hippocampus, hypothalamus and cerebral cortex acquire the necessary structure.
Further differentiation of nerve fibers occurs together with the growth of internal organs and the fetal body.
Possible deviations in operation
Since people, especially in the modern world, are always susceptible to stress, the human nervous system ceases to adequately regulate body processes, and the state of health decreases sharply.
The most common disorders include autonomic dysfunction syndrome, previously called vegetative-vascular dystonia.
Its symptoms may include digestive disorders, changes in blood pressure up or down, increased ventilation of the lungs due to an increase in breathing rate, or, conversely, a subjective feeling of lack of air.
Behavior changes dramatically, as the autonomic nervous system is responsible for mood, perception of the surrounding world and adaptation.
The patient may become apathetic, suspicious, his behavior and views on certain things will change.
The main problem in diagnosis is the similarity of the clinical picture of autonomic dysfunction with other serious pathologies of the gastrointestinal tract, heart, blood vessels, endocrine glands and other organs.
Treatment is mainly carried out by a neurologist, psychotherapist and psychiatrist; they build the correct treatment regimen and partly help the patient cope with emotional experiences.
Source: https://NashiNervy.ru/o-nervnoj-sisteme/stroenie-i-funktsii-vegetativnoj-nervnoj-sistemy.html