Structure of the autonomic nervous system
The autonomic nervous system is a part of the nervous system and is, like any other part of the nervous system, under the influence of the cerebral cortex. Through the autonomic nervous system, the activity of the circulatory, respiratory, excretory, reproduction, and metabolic organs is regulated. But the role of the autonomic nervous system is not limited to the listed functions, since it also affects the processes occurring in the skeletal muscles and sensory organs.
The autonomic nervous system in its structure and properties differs from the somatic nervous system, which innervates the striated muscles and provides sensitivity to our body. The autonomic nervous system is divided into the parasympathetic and sympathetic nervous systems. Unlike the somatic nervous system, whose nerve fibers arise from each segment of the spinal cord, the autonomic nervous system emerges in bundles from different parts of the central nervous system.
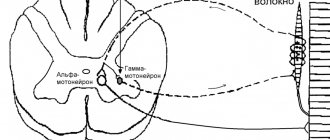
Rice. DIAGRAM OF THE PARASYMPATHETIC NERVOUS SYSTEM.
The autonomic nervous system originates in the midbrain, medulla oblongata, sternolumbar and sacral parts of the spinal cord.
Fibers arising in the central nervous system from the midbrain and medulla oblongata and from the sacral spinal cord form the parasympathetic nervous system. The same part of the autonomic nervous system that begins in the sternolumbar region is called the sympathetic nervous system.
Another feature of the structure of the autonomic nervous system is that the nerve fibers, after exiting the central nervous system, end before reaching the organ they supply. However, they immediately come into contact with another nerve cell, the process of which already reaches the organ. Thus, the fibers of the autonomic nervous system, after leaving the brain and spinal cord on the way to the innervated organ, are interrupted once.
Therefore, unlike somatic nerves, which go without interruption, autonomic nerves consist of two neurons, between which there is a synapse.
At the break points there is a large accumulation of nerve cells that form nodes, or ganglia, of the autonomic nervous system.
Nerve fibers that leave the central nervous system and end in the ganglia are called preganglionic. The same fibers that extend from the ganglion and reach a specific organ are called postganglionic fibers.
The presence of a break was proven by cutting. The method is based on the fact that if a nerve fiber is cut, the part of it that is separated from the body of the nerve cell degenerates and dies. When the preganglionic (prenodal) fiber is cut, the cut off part is degenerated, but the degeneration extends only to the ganglion and does not go further. Transection of the postganglionic (post-nodal) fiber is accompanied by degeneration of the part that goes to the organ. This part is reborn entirely up to the end formations.
Thus, the cutting method gives grounds to assert that a break occurs in the ganglion and that the second nerve cell is located in the ganglion.
Rice. 2 SCHEME OF THE SYMPATHETIC NERVOUS SYSTEM.
The ganglia of the autonomic nervous system are located at different distances from the central nervous system. There are ganglia located directly next to the spinal column; another group of ganglia is located relatively far from the spinal column, at approximately the same distance between the organ and the spinal column: the third group of ganglia is located directly in the organs themselves.
The ganglia of the sympathetic nervous system are located near the spinal column and form a chain to the right and left of it. Some of the nodes are moved to a greater distance.
Intervertebral nodes should not be mixed with the nodes of the sympathetic chains. The intervertebral nodes, which we became acquainted with when considering the reflex arc, are the site of accumulation of sensitive cells and have nothing to do with the nodes of the sympathetic chain.
The ganglia of the parasympathetic nervous system are located in or near organs.
The autonomic nervous system differs from the somatic one not only in the structural features that we discussed above, but also in a number of physiological properties.
The fibers of the autonomic nervous system are 2-5 times thinner than the fibers of the somatic nerves. The diameter of the somatic nerve fibers is 10-14µ, the diameter of the autonomic nervous system fibers is 2-7µ.
Autonomic nerve fibers are less excitable than somatic ones. To cause excitation in the autonomic nerve fiber, stronger stimulation must be applied.
Excitation along the autonomic nerves is carried out more slowly. The refractory period is longer.
Parasympathetic nervous system
The parasympathetic nervous system originates from the midbrain and medulla oblongata and from the sacral part of the spinal cord (Fig. DIAGRAM OF THE PARASYMPATHETIC NERVOUS SYSTEM. III - oculomotor; VII - facial; XI - glossopharyngeal and X - vagus nerves. From the sacral part of the spinal cord the pelvic nerve begins - 1 - eye; 2, 3 and 4 - salivary glands; 5 - lungs; 6 - heart; 7 - liver; 8 - stomach; 9 - pancreas; 10 - small intestine; 11 - large intestines; 12 - bladder.) .
Parasympathetic fibers that form the oculomotor nerve depart from the midbrain. These fibers innervate the smooth muscles of the eye. The impulses coming through these nerves constrict the pupil. From a group of cells located in the medulla oblongata, parasympathetic fibers originate, which go as part of the facial and vagus nerves. The facial nerve contains fibers that form a nerve called the chorda tympani. It is the secretory nerve of the submandibular salivary gland and its stimulation causes salivation.
Another part of the medulla oblongata cell gives rise to the vagus nerve, which branches widely; the numerous branches formed innervate the heart, esophagus, bronchi, stomach, small intestines, upper parts of the large intestines, pancreas, adrenal glands, kidneys, liver, spleen.
Parasympathetic fibers originate from the sacral part of the spinal cord and travel as part of the pelvic nerve. These fibers innervate the sigmoid colon, rectum, genitals and bladder.
List the nuclei of the parasympathetic and sympathetic divisions of the ANS
Parasympathetic Division:
The central section is the cranial and sacral foci.
Cranial lesion:
- 3 pair - Yakubovich kernel
- 7th pair - superior salivary nucleus
- 9 pair - lower salivary nucleus
- 10th pair - dorsal nucleus (largest)
Sacral hearth:
- Sacral parasympathetic nuclei of SM segments 2-4.
Sympathetic division of the ANS:
- Lateral intermediate nuclei C8, all Th, L1-2.
Sympathetic nervous system
The sympathetic nervous system originates from the last cervical to the third lumbar segment of the spinal cord. A significant part of these fibers, leaving the spinal cord, enters the nodes located near the spine. These nodes, or ganglia, form the border sympathetic chain. A significant part of these fibers are interrupted here, while the rest are interrupted in the ganglia located further from the spinal column. These nodes include the upper and middle cervical nodes, the stellate or lower cervical node, the solar plexus nodes, the superior and inferior mesenteric nodes, etc.
The sympathetic nervous system innervates all tissues and organs. It affects the activity of the digestive organs, smooth muscles, heart, blood vessels, kidneys, bladder, endocrine glands, genitals, sensory organs, sweat glands, etc. (Fig. 2).
The sympathetic nervous system affects not only the work of the listed organs: the activity of all striated muscles is under its influence; it affects muscle tone, the metabolic processes that occur in the muscle, and the restoration of the activity of a tired muscle.
L. A. Orbeli created a theory about the adaptive-trophic function of the sympathetic nervous system. According to this theory, the sympathetic nervous system plays a dual role in the body. It affects the metabolism occurring in the muscles, which affects the functioning of muscle tissue. This function was called trophic (from the Greek word “trophos” - nourishing).
The adaptive, i.e. adaptive, influence of the sympathetic nervous system lies in the fact that under its action a number of changes occur in organs and tissues that prepare the organ to work in new changed conditions.
All activity of the sympathetic, as well as parasympathetic, nervous system is under the influence of the cerebral cortex and must be considered in inextricable connection with the activity of the entire central nervous system.
There is a certain relationship between the emotional state and the activity of the sympathetic nervous system.
A state of fear, anger, rage, etc. causes a number of changes in the body: cold sweat appears, dilation or constriction of blood vessels occurs, resulting in redness or paleness of the skin; violent movements occur or, conversely, movements are slowed down, etc.
All these external expressions of certain emotions are due to the influence of the cerebral hemispheres, primarily through the sympathetic nervous system on the activity of organs. When excited, the sympathetic nervous system also enhances the work of the adrenal medulla, which produces adrenaline. Thus, simultaneously with the stimulation of the sympathetic nervous system, the amount of adrenaline in the blood increases, a hormone that acts like the sympathetic nervous system.
The parasympathetic and sympathetic nervous systems are a single nervous system. The influence of these systems is often opposite, for example, under the influence of parasympathetic nerves, the activity of the heart is inhibited, and under the influence of sympathetic nerves it is enhanced; under the influence of parasympathetic nerves, intestinal movements are enhanced, and under the influence of sympathetic nerves, they are inhibited. In regulating the functions of the whole organism, the activity of both one and the other system is important.
During large physical work, the sympathetic nervous system is very important, but large and long-term work depends on the timely entry into action of the parasympathetic nervous system. Only as a result of the coordinated activity of both systems is long-term physical work possible. The coordinated activity of the parasympathetic and sympathetic nervous systems determines the normal functioning of the body.
Bladder dysfunction
Bladder function disorders are most often observed in the clinic. Its innervation is shown in Fig. 1.5.3.
Excitation of parasympathetic fibers causes contraction of the detrusor and relaxation of the sphincter of the bladder, which leads to the act of urination, and in pathological conditions can provoke urgency and even urinary incontinence. The opposite phenomenon, i.e., urinary retention, is observed when sympathetic influences predominate due to the loss of parasympathetic ones with damage to preganglionic neurons caused by pathological processes in the caudal part of the spinal cord - its conus. The act of urination is under voluntary control, with the main role played by the external sphincter of the bladder, represented by the striated muscle. The cortical micturition center is located on the inner surface of the cerebral hemispheres in the paracentral lobule (central motor neuron). Material from the site https://wiki-med.com
The peripheral neuron is located in the anterior horns of the lower lumbar segments of the spinal cord, the fibers reach the sphincter as part of the pelvic nerve. Damage to the paracentral lobes (parasagittal tumor) is characterized by bilateral foot paralysis and urinary incontinence (see Fig. 1.2.9).
Types of Pelvic Disorders
Three main types of neurogenic pelvic disorders can be distinguished, most demonstrative of bladder dysfunction.
- When the path of voluntary control of bladder emptying is affected (its course is assumed to be part of the pyramidal tract), difficulties in voluntary control are observed, imperative urges arise (impossibility of voluntary full control of the urge to urinate), which is usually combined with difficulties in emptying the bladder (the patient has to push for a long time). One or the other influence may predominate. With the complete loss of voluntary control of urination, the phenomenon of the so-called autonomous bladder occurs, when periodically, as the bladder fills, it is reflexively emptied (incontinentia intermittens). Most often this is observed in patients with multiple sclerosis (cerebrospinal and spinal forms).
- With incomplete damage (irritation) to the sacral segments or their roots associated with the innervation of the bladder, spasm of the bladder sphincters may develop. The bladder is full and urine comes out in drops (ischuria paradoxa).
- When autonomic pregayaglionic neurons are damaged (usually in cases of involvement of the caudal parts of the spinal cord), so-called true urinary incontinence (incontinentia vera) occurs, in which there is a constant release of urine.
Categories: Nervous system Neurology Autonomic nervous system
On this page there is material on the following topics:
dysfunction of the mesencephalic parts of the trunk
What does parasympathetic nervous system mean?
parasympathetic system anatomy
mesencephalic centers of the parasympathetic division
Relation of the sympathetic and parasympathetic nervous system to certain poisons
Some poisons selectively act on different parts of the autonomic nervous system. The nodes, nerve fibers and endings of the autonomic nervous system are differently excited and paralyzed by one or another poison. For example, nicotine is a poison found in tobacco.
, paralyzes the sympathetic nodes, but does not affect the fibers. Nodes poisoned by nicotine lose their ability to conduct excitation, and therefore the impulse received from the preganglionic fiber is not transmitted to the postganglionic fiber and does not reach the organ.
Another poison, atropine, acts on the parasympathetic part of the autonomic nervous system. It stops the transmission of excitation from the nerve endings of the parasympathetic fibers to the working organ. For example, after an injection of atropine, the endings of the vagus nerve are paralyzed and the heart stops receiving inhibitory impulses, as a result of which its work increases.
Article on the topic Autonomic nervous system
Classification of ANS nodes, their location. What are the autonomic nerves divided into in relation to the nodes?
In relation to the spinal column and organs:
- Nodes of the 1st order - paravertebral - on the sides of the vertebral bodies (sympathetic trunk - truncus sympaticus),
- Nodes of the 2nd order - prevertebral (celiac nodes - 2; superior mesenteric node - 1; inferior mesenteric node - 1) - in the plexus of the abdominal cavity,
- Nodes of the 3rd order - terminal - closer to the organs: Extramural,
- Intramural.
1st and 2nd order – sympathetic , 3rd – parasympathetic nodes.
In relation to the nodes, preganglionic and postganglionic parts of the autonomic nerves are distinguished.
Notes[ | ]
- Lapin S.K., Mikhailovsky V.S., Plechkova E.K., Shefer D.G.
Autonomic nervous system // Great Medical Encyclopedia, 3rd ed. - M.: Soviet Encyclopedia. - T. 4. - Brief medical encyclopedia.
- Biologist's Dictionary. (unavailable link)
- For example, in the book “Human Physiology / Ed. V. M. Pokrovsky, G. F. Korotko. - M.: Medicine, 1997. - T. 1 - 448 p.; T. 2 - 368 pp.”
- Romer A., Parsons T. Anatomy of vertebrates. - T. 2. - P. 260.
- I. Espinosa-Medina, O. Saha, F. Boismoreau, Z. Chettouh, F. Rossi.
The sacral autonomic outflow is sympathetic (English) // Science. — 2016-11-18. - Vol. 354, iss. 6314. - P. 893–897. — ISSN 1095-9203 0036-8075, 1095-9203. - doi:10.1126/science.aah5454. - Brin V.B. et al. Fundamentals of human physiology in 2 volumes. Textbook for higher educational institutions. Ed. B. I. Tkachenko. St. Petersburg, 1994. T.1 - 567 p. T.2 - 413 p.
- Stefan Boehm, Sigismund Huck. Receptors controlling transmitter release from sympathetic neurons in vitro // Progress in Neurobiology. — Volume 51, Issue 3, February 1997, Pages 225-242. (unavailable link)
- G. Ross, C. Ross, D. Ross. Entomology. - M.: Mir, 1985. - P.109.
Development in embryogenesis[ | ]
- Development of the peripheral (somatic) and autonomic nervous system.
The peripheral (somatic) and autonomic nervous system develops from the outer germ layer - the ectoderm. Cranial and spinal nerves in the fetus are formed very early (5-6 weeks). Myelination of nerve fibers occurs later (for the vestibular nerve - 4 months; for most nerves - at 6-7 months).
Spinal and peripheral autonomic ganglia are formed simultaneously with the development of the spinal cord. The starting material for them is the cellular elements of the ganglion plate, its neuroblasts and glioblasts, from which the cellular elements of the spinal ganglia are formed. Some of them are shifted to the periphery to the localization of the autonomic nerve ganglia
| This section of the article has not been written. According to the plan of one or more Wikipedia contributors, a special section should be located in this place. You can help by writing this section. This mark was set on October 31, 2020 . |
Morphology[ | ]
The distinction of the autonomous (autonomic) nervous system is due to certain features of its structure. These features include the following:
- focal localization of vegetative nuclei in the central nervous system;
- accumulation of bodies of effector neurons in the form of nodes (ganglia) as part of the autonomic plexuses;
- two-neuronality of the nerve pathway from the autonomic nucleus in the central nervous system to the innervated organ.
The fibers of the autonomic nervous system do not emerge segmentally, as in the somatic nervous system, but from three limited areas of the brain spaced apart from each other: cranial, sternolumbar and sacral.
The autonomic nervous system is divided into sympathetic, parasympathetic and metasympathetic parts. In the sympathetic part, the processes of spinal neurons are shorter, while the ganglion ones are longer. In the parasympathetic system, on the contrary, the processes of spinal cells are longer, those of ganglion cells are shorter. Sympathetic fibers innervate all organs without exception, while the area of innervation of parasympathetic fibers is more limited.
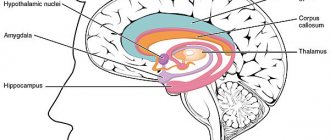
Central and peripheral sections[ | ]
The autonomic (autonomic) nervous system is divided according to topographical characteristics into central and peripheral sections.
Central department[ | ]
- parasympathetic nuclei of 3, 7, 9 and 10 pairs of cranial nerves lying in the brain stem (craniobulbar region); nuclei lying in the midbrain (mesoencephalic region).; nuclei located in the gray matter of the three sacral segments (sacral section)[6]
- sympathetic nuclei located in the lateral horns of the thoracolumbar spinal cord;
Peripheral department[ | ]
- autonomic (autonomic) nerves, branches and nerve fibers emerging from the brain and spinal cord;
- vegetative (autonomous, visceral) plexuses;
- nodes (ganglia) of the autonomic (autonomous, visceral) plexuses;
- sympathetic trunk (right and left) with its nodes (ganglia), internodal and connecting branches and sympathetic nerves;
- terminal nodes (ganglia) of the parasympathetic part of the autonomic nervous system.
Sympathetic, parasympathetic and metasympathetic divisions[ | ]
Based on the topography of the autonomic nuclei and nodes, differences in the length of the axons of the first and second neurons of the efferent pathway, as well as the characteristics of the function, the autonomic nervous system is divided into sympathetic, parasympathetic and metasympathetic.
Location of ganglia and structure of pathways[ | ]
Neurons
nuclei of the central part of the autonomic nervous system are the first efferent neurons on the way from the central nervous system (spinal cord and brain) to the innervated organ. The nerve fibers formed by the processes of these neurons are called prenodal (preganglionic) fibers, since they go to the nodes of the peripheral part of the autonomic nervous system and end with synapses on the cells of these nodes. Preganglionic fibers have a myelin sheath, which makes them whitish in color. They leave the brain as part of the roots of the corresponding cranial nerves and the anterior roots of the spinal nerves.
Vegetative nodes
(ganglia): are part of the sympathetic trunks (present in most vertebrates, except cyclostomes and cartilaginous fish), large vegetative plexuses of the abdominal cavity and pelvis, located in the head and in the thickness or near the organs of the digestive and respiratory systems, as well as the genitourinary system, which are innervated by the autonomic nervous system. The nodes of the peripheral part of the autonomic nervous system contain the bodies of second (effector) neurons lying on the way to the innervated organs. The processes of these second neurons of the efferent pathway, carrying nerve impulses from the autonomic ganglia to the working organs (smooth muscles, glands, tissues), are post-nodular (postganglionic) nerve fibers. Due to the absence of the myelin sheath, they are gray in color. Postganglionic fibers of the autonomic nervous system are mostly thin (most often their diameter does not exceed 7 µm) and do not have a myelin sheath. Therefore, excitation spreads slowly through them, and the nerves of the autonomic nervous system are characterized by a longer refractory period and greater chronaxis.
Reflex arc[ | ]
The structure of the reflex arcs of the autonomic part differs from the structure of the reflex arcs of the somatic part of the nervous system. In the reflex arc of the autonomic part of the nervous system, the efferent link consists not of one neuron, but of two, one of which is located outside the central nervous system. In general, a simple autonomic reflex arc is represented by three neurons.
The first link of the reflex arc is a sensory neuron, the body of which is located in the spinal ganglia and in the sensory ganglia of the cranial nerves. The peripheral process of such a neuron, which has a sensitive ending - a receptor, originates in organs and tissues. The central process, as part of the dorsal roots of the spinal nerves or sensory roots of the cranial nerves, is directed to the corresponding nuclei in the spinal cord or brain.
The second link of the reflex arc is efferent, since it carries impulses from the spinal cord or brain to the working organ. This efferent pathway of the autonomic reflex arc is represented by two neurons. The first of these neurons, the second in a simple autonomic reflex arc, is located in the autonomic nuclei of the central nervous system. It can be called intercalary, since it is located between the sensitive (afferent) link of the reflex arc and the second (efferent) neuron of the efferent pathway.
The effector neuron is the third neuron of the autonomic reflex arc. The bodies of effector (third) neurons lie in the peripheral nodes of the autonomic nervous system (sympathetic trunk, autonomic ganglia of cranial nerves, nodes of extraorgan and intraorgan autonomic plexuses). The processes of these neurons are directed to organs and tissues as part of organ autonomic or mixed nerves. Postganglionic nerve fibers end on smooth muscles, glands and other tissues with the corresponding terminal nerve apparatus.
Embryology
The ganglion plate is the embryonic source for the sympathetic system. It is divided into somites, which differentiate into the sympathetic and parasympathetic systems. The sympathetic level includes the cervical and thoracic somites.
During embryogenesis, the peripheral part of the sympathetic nervous system is formed as a result of the migration of sympathetic neuroblasts. Migration occurs along the fibers of the spinal cord segmentally. There are several “waves of migration”. As a result of the first wave, a “primary” sympathetic trunk is formed, represented in the neck by the superior (cranial), inferior (posterior), cervical and stellate ganglia. The second wave arises from the primary one, mainly from the dorsal sections. As a result, a “secondary” sympathetic trunk is formed.
The structure of a nice department
Each of the 4 sections (with nodes and many branches) of the peripheral part are responsible for certain areas:
- cervical (has 3 nodes), responsible for the functioning of the brain and heart;
- thoracic (9-12 nodes) controls the organs of the chest, parts of the abdominal cavity;
- lumbar (3-4 nodes) ensures the production of adrenaline, controls the intestines, pancreas;
- sacral (3-4 nodes) connects together the nerve branches of both trunks, innervates the pelvic organs (rectum, uterus, prostate).
The nerve fibers of the 1st section are located behind the arteries in the muscles of the neck. The thoracic branches of the 2nd extend to the heart, lungs, esophagus and control the plexuses: pulmonary and cardiac.
The lumbar (3rd) section consists of plexuses (celiac and mesenteric) formed by visceral cells in front of the spine. Pelvic (sacral) - the 4th section is found in front of the coccyx.