Causes and types of meningitis
The inflammatory process is provoked by bacteria: meningococci, pneumococci, hemophilus influenzae. In the presence of weakened immunity, these bacteria easily circulate in the bloodstream and settle in various tissues and organs, affecting the meninges.
Children under 5 years of age are at risk, as their immunity is in the process of formation. The disease also affects people with immunodeficiencies and chronic diseases of inflammatory origin.
Purulent meningitis in children is often caused by streptococcus and salmonella. In the absence of proper hygiene and frequent contact with sick people, the risk of developing meningitis increases several times.
Considering the way pathogenic bacteria enter brain cells, there are two types of meningitis:
- Primary - is a consequence of a long-term respiratory disease, when bacteria from a sick person enter the mucous membrane of the nasopharynx of a healthy person, are activated and spread along with the blood to the brain. Another cause is trauma to the skull and nose, which results in an open wound. Lack of proper processing and non-compliance with aseptic rules provokes the entry of various bacteria into the blood.
- Secondary – is a consequence of localized inflammatory purulent processes occurring in the body. Most often these are chronic sinusitis, rhinitis, and otitis media of the middle ear. As soon as the immune system weakens and is unable to contain the number of bacteria, they become active and begin to circulate freely throughout the body, ending up in the brain.
Primary meningitis is transmitted from a sick person to a healthy person.
Secondary purulent meningitis affects people at a more mature age who have chronic illnesses and do not have natural protection. This can be caused by lifestyle, as well as harmful working conditions.
An indirect reason that allows pathogenic bacteria to become active is weak immunity. The reasons may be:
- frequent stress and lack of proper rest;
- long-term respiratory diseases;
- congenital immunodeficiencies;
- poor nutrition, causing acute vitamin deficiencies.
When bacteria enter the human body, the situation can develop in two ways: either the immune system will immediately start working and prevent foreign agents from entering the brain, or, against the background of its weakening, the pathogenic microflora will quickly spread through the blood throughout the body.
Consequences of purulent meningitis
The risk group for pathogens is children under 5 years of age. Newborns can also get sick. This age group is most susceptible to infection. An immune system that is not fully formed is unable to resist pathogens. In addition, at such a young age, any changes in the lining of the brain can lead to developmental disorders.
For children
In children with meningitis, the following complications are observed:
- Meningoencephalitis. Inflammation of the membranes and substance of the brain and spinal cord, leading to paralysis.
- Infectious-toxic shock.
- Facial paresis. Complete or partial paralysis of the facial nerve.
- Hydrocephalus. Accumulation of excess fluid in the brain.
- Heart attacks, strokes, vascular disorders.
- Death.
Children are more likely to need urgent medical attention. Their body is unable to fight the disease. Therefore, a greater percentage of dangerous complications and critical forms of the disease occur in childhood.
Doctors recommend going to the hospital at the first signs of intoxication in a child.
For adults
Meningitis is one of the most dangerous diseases, distinguished by its insidiousness. The first symptoms appear a couple of days after infection. With the first attempts at treatment, the infection may disappear. But during such a “quiet” period, the most dangerous consequences develop.
Complications from the disease are as follows:
- Brain swelling. The brain stem is compressed, vital centers are damaged.
- Septic shock, general intoxication of the body.
- Subdural empyema. Represents an accumulation of pus between the meninges.
- Adrenal insufficiency.
- Infectious endocarditis.
- Pneumonia.
- Purulent arthritis.
- Pyelonephritis.
- Acute cystitis.
- Septic panophthalmitis. Inflammation of the eyeballs.
- Optic nerve palsy.
Forms of diseases
Taking into account the peculiarities of the course of the disease, the following forms are distinguished:
- Fulminant – within 2-3 hours from the moment of debut, meningeal symptoms develop with a further increase in cerebral edema. Lack of medical assistance provokes death.
- Acute - occurs with the development of all characteristic symptoms, and with early diagnosis and treatment it is well and quickly relieved, without causing life-threatening complications.
- Recurrent (chronic) – develops due to undertreatment or neglect of the acute form of the disease, as well as the progression of purulent foci in the body against the background of a pathologically weakened immune system.
- Abortive is the most dangerous type because it has a blurred clinical picture, which prevents early diagnosis. There are signs of intoxication, and stiff neck and pain in the head are practically absent or mild.
According to the severity of the disease, purulent meningitis can be mild, moderate and severe. The prognosis of 85% depends on the degree of severity.
Clinical manifestations
The incubation period of purulent meningitis varies from 2 to 5 (sometimes 10) days, which is due to the peculiarities of immunity. The onset of the disease can take various forms, manifested by the following symptoms of general intoxication:
- A sharp increase in body temperature to critical levels, which cannot be stabilized when using any antipyretic drugs. A person suffers from chills, which is accompanied by fever and the release of profuse sticky sweat.
- Intense thirst and dryness of the mucous membranes, which cannot be eliminated even with plenty of fluids. If a person drinks a large amount of liquid at one time, vomiting immediately follows, which only intensifies the increasing dehydration.
- Severe migraine-type headache localized in the temples and back of the head. The pain intensifies when exposed to sound and light stimuli, as well as movement.
- Nausea and vomiting, cramping pain in the abdomen, which are in no way related to a disorder of the digestive tract and develop reflexively.
- Impaired consciousness, speech and quality of vision, which indicates damage to the large nerves supplying the brain.
- Shell symptoms (Guillain's, Brudzinsky's, Kernig's symptoms) are visualized in the first hours after the onset of the disease.
- Stiff neck muscles, which provokes the need to throw the head back. This position reliably indicates the presence of meningitis.
- A characteristic diffuse rash in the extremities and abdomen.
- Decreased reflexes and coma.
A sharp increase in temperature that cannot be brought down is the first symptom of meningitis.
Active secretion of pus, which is a natural process, irritates the meninges, causing an increase in intracranial pressure. This in turn causes a number of additional complications in the form of impaired visual function, deafness and impaired consciousness.
In the absence of proper treatment and the spread of pus into the deep layers of the meninges, meningoencephalitis develops. It is diagnosed by characteristic manifestations:
- paresis and paralysis of the whole body;
- absence or incoherence of speech;
- violation or lack of sensitivity of the skin;
- pathological and spontaneous reflexes;
- hallucinations;
- cardiovascular pathologies.
In some cases, characteristic meningeal symptoms may be completely absent, making diagnosis difficult. Symptoms of intoxication and severe headache should be examined by a specialist.
Diagnostics
A preliminary diagnosis is made based on an assessment of external clinical manifestations and collection of a primary medical history. The doctor examines the patient, recording three main signs of meningitis:
- severe headache and its relief when tilting the back of the head;
- reflex flexion of the second leg during mechanical flexion of the first;
- high temperature, which is not knocked down by anything.
To clarify the diagnosis, the following studies are used:
- Lumbar puncture - in the presence of purulent meningitis, the cerebrospinal fluid comes out under pressure, bubbles slightly, has a cloudy consistency and a characteristic gray-green tint. Microbiological examination reveals the causative agent of meningitis, as well as the degree of progression of the purulent-inflammatory process.
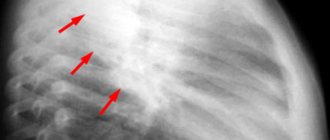
- MRI and CT - helps to determine the presence of primary and secondary inflammatory foci, as well as the degree of their progression.
Differential diagnosis requires the separation of purulent meningitis from viral meningitis, as well as diseases with similar manifestations: typhus, severe forms of influenza, leptospirosis.
Classification
According to the mechanism of development, it is customary to distinguish primary and secondary acute serous-purulent meningitis. Primary meningitis develops in situations where the pathogen, after entering the body, immediately causes damage to the membranes of the brain. It is worth noting that such cases of the disease are more severe, since most pathogens are specific and require special drug treatment.
Secondary purulent meningitis is a complication of the disease. It can be of different nature. What is common to all pathogens is that the complication develops after sepsis has developed.
The greatest danger is posed by those pathologies that are localized in the skull area. These include diseases of the ear, teeth and gums, as well as the air sinuses. This pattern is due to the fact that these areas of the human body have common branches of blood vessels with the brain.
Meningitis is one of the possible complications of dental diseases
Classification of meningitis by nature of origin is important only when prescribing treatment. Thus, we distinguish:
- Bacterial.
- Viral.
- Fungal.
Regardless of the nature of the origin of the disease, the clinical picture is practically the same. The only thing that matters is the age of the patient.
Symptoms of meningitis are the same for all forms of the disease
Treatment options
Treatment of purulent meningitis, regardless of severity, is carried out in a hospital setting, where the initial diagnostic procedure is a lumbar puncture. As soon as data is obtained about which pathogenic microorganisms provoked meningitis, appropriate antibiotic therapy is selected. Preference is given to cephalosporin antibiotics, which have an extended spectrum of action: Ceftriaxone, Cefazolin, Cefix, Cefotaxime.
In case of unknown etiology of the disease or doubts on the part of doctors, which requires a number of additional diagnostic procedures, the patient is initially administered Gentamicin or Kanamycin. After confirmation of the etiology of the disease, treatment is continued with other antibiotics that have a less harmful effect on the body.
Antibacterial therapy involves the administration of maximum doses of drugs, which will quickly eliminate the spread of pathogenic microbes throughout the body.
Along with antibiotics, the patient undergoes detox therapy, which is aimed at removing waste and toxins from the body, as well as replenishing the lytic composition of the blood. Infusion solutions are prescribed that help normalize the condition in the shortest possible time.
In cases where there are kidney problems, as confirmed by a urine test, hemodialysis may be required. Artificial cleansing of the blood from waste and toxins greatly facilitates the work of the paired organ, normalizing all metabolic processes.
To reduce brain swelling and prevent the development of hydrocephalus, diuretics are prescribed. With their help, all liquid entering the body by infusion is freely excreted naturally, without accumulating in tissues and organs.
Glucocorticosteroids are prescribed to block the body's reaction, which in the presence of purulent meningitis can be pathological. Hormonal agents control the functioning of brain centers and also reduce pain.
Symptomatic therapy involves the use of painkillers, anticonvulsants and muscle relaxants. In the presence of high blood pressure, antihypertensive drugs are used in combination with diuretics.
In a state of infectious-toxic shock, resuscitation measures are carried out aimed at maintaining all vital processes in the body. Surgery may be required to repair localized lesions in the brain.
After the acute period has stopped and the patient’s general condition has improved, the doctor may prescribe antipsychotics and nootropics that improve cerebral circulation, as well as normalize the functioning of the central and peripheral nervous system.
general description
Acute purulent meningitis is a pathological process characterized by damage to the meninges. Its peculiarity is that purulent exudate leads not only to functional disorders, but also to structural ones. A purulent process is usually a consequence of serous inflammation when adequate treatment is not carried out.
In most cases, meningitis develops against the background of other pathologies of a viral, bacterial or fungal nature. Most of these diseases are relatively mild and rarely cause brain damage. The causative agents of meningitis have one feature - they must have trophism for nervous tissue. The membranes of the brain have a number of features that increase the risk of infection and make the course of the disease especially severe. These include:
- Good blood supply. Since nerve cells are extremely sensitive to changes in the concentration of nutrients and oxygen in the blood, nature has created an extremely extensive blood supply system. The human brain has the densest circulatory system compared to other vital organs. The entry of the pathogen into the bloodstream creates a high probability of tissue infection.
The membranes of the brain have a developed blood supply network and are therefore susceptible to infection
- High permeability of the vascular wall in children. It is worth noting the fact that meningitis is much more common in children than in adults. This is due to the fact that the child’s circulatory system is imperfect, and the walls of the vessels of the cerebral circulatory system are extremely thin. Through them, the pathogen can penetrate tissue almost unhindered.
- The presence of a large amount of nutrients in the liquor. Cerebrospinal fluid is an excellent breeding ground for various pathogens. Once in the cerebrospinal fluid, they begin to actively multiply and develop, which makes the development of the disease possible.
Complications
The consequences of purulent meningitis can be the most unpredictable. The mild form usually resolves quickly and does not cause life-threatening complications. In the presence of a weakened immune system, an advanced form of meningitis and improper treatment, complications such as:
- visual and hearing impairment;
- paresis of the limbs without the possibility of full restoration of motor activity;
- problems with speech and coordination of movement;
- swelling of the brain (hydrocephalus);
- partial or complete absence of reflexes;
- death.
If you suspect meningitis, you should immediately consult a doctor.
Since the characteristic symptoms of purulent meningitis may be absent for quite a long time, it is important not to forget about the need to consult a specialist. If there is any suspicion of meningitis, treatment should be started only after a comprehensive diagnosis and specialist recommendations. Self-medication can be ineffective and life-threatening.
Assistance in a medical facility
The main method of diagnosis in adults and children is the examination of cerebrospinal fluid, for which a puncture is performed. Computed tomography, ultrasound of the head, and MRI are also performed - intended for differential diagnosis of meningitis from tumors, abscesses, encephalitis, and strokes.
Secondary meningitis can be detected by congestion in the fundus. In children, in addition to taking a puncture, blood is taken for analysis - a large number of leukocytes and neutrophils determines an accurate diagnosis.
Treatment of severe forms of purulent meningitis is carried out only in a hospital. If the baby’s disease is mild, it can be treated at home. Adults are treated only in a hospital. The main goal in the treatment of purulent meningitis is timely hospitalization of the patient and the selection of the correct methods of therapy.
The outcome of the disease depends on how timely therapy is started. When hospitalized, it is important to identify the source and cause of infection in order to prescribe effective medications.
Traditional medicine
Treatment of purulent meningitis in both adults and children begins as soon as the doctor suspects an inflammatory process in the brain. To begin therapy, a broad-spectrum antibiotic is administered, after which the patient is hospitalized. While the diagnosis is being carried out, the patient continues to be given antibiotics. Having established an accurate diagnosis, treatment is prescribed.
Therapy involves the use of antibiotics from the cephalosporin, penicillin and macrolide groups. They are administered in the maximum permissible doses, every 4 hours, and after a noticeable improvement, treatment with antibiotics continues for up to a month.
Other medications are also prescribed to relieve unpleasant symptoms:
- stop vomiting and relieve nausea - Cerucal;
- Baralgin or Ketanol will help relieve headaches
- eliminate intoxication and prevent dehydration - sodium chloride solution, glucose, osmotic compounds;
- prevent cerebral edema .
Article on the topic: How to treat a severe and dry throat cough in an adult?
For purulent meningitis, a craniotomy is performed to remove the pus. If this is a secondary form of the disorder, then medications are prescribed to treat the underlying disease.
After improvement of health, the patient is sent for home treatment and subsequent dispensary observation.
Children are observed by a pediatrician, infectious disease specialist and neurologist for 2 years with regular examinations, first every 3 months, then once every six months. After discharge from the hospital, adults are observed by a therapist, neurologist, infectious disease specialist and psychiatrist for two years.
For the first 3 months, the patient must visit specialists 2 times a month, and then once every three months. In the second year of observation, one visit to doctors every six months is sufficient. The terms are valid in the absence of deterioration in health.
ethnoscience
Traditional methods of treatment help alleviate the patient’s condition, but do not help cure the disease itself. Apply:
- An infusion of thistle herb is good for relieving cramps.
- Chamomile tea helps the patient relieve stress and calm down .
- Lavender infusion relieves cramps and is a diuretic : 3 teaspoons of dried flowers in 2 cups of boiled water, leave for 30 minutes.
- A collection of lavender flowers, primrose and valerian roots, mint and rosemary leaves, taken 20 g each and poured with a glass of boiling water, will help relieve irritation and headaches Drink 500 ml per day of this infusion after cooling and filtering.
At home, before the ambulance arrives, the patient must be provided with mental and physical peace. Close the windows with curtains so that the light does not intensify the headache and does not blind the eyes, and ensure silence.
Place ice or rags soaked in cold water on your head, arms to the elbows and legs to the knees, along the spine and change them as you warm up. You can give the patient a headache medication.