What is a disease?
In neurology, Horner's syndrome is a clinical syndrome that is associated with damage to the sympathetic nervous system. It is also often called oculosympathetic, as it manifests itself before the eyes. Although it affects the nervous system, the syndrome can also affect the eye itself.
In neurology, Horner's syndrome is a clinical syndrome that is associated with damage to the sympathetic nervous system
Doctors usually distinguish two types of origin of this disease:
- idiopathic;
- secondary.
Idiopathic is a term known in medicine that explains the independent origin of the disease. In the case of Horner's syndrome, this type of origin suggests that the disease did not arise from other diseases or pathogenic factors, but is an independent disease.
This classification is very important in further treatment, so the doctor must first determine the type of origin of the syndrome. Secondary Horner's syndrome develops as a symptom of other diseases, sometimes due to a number of different processes.
Causes
There are many causes of Horner's syndrome, ranging from damage to the nervous system to congenital defects and pathologies.
Let's look at them in more detail:
- Physical impact directly on the thoracic or cervical circuits of the sympathetic system. This can be either compression or direct damage. Often symptoms occur on the side where the impact was made.
- With damage to brain tissue due to lateral medullary syndrome.
- The cause of the syndrome may be cluster headache. These are very severe headaches that are felt on the walls of the skull. The pain is so severe that there are frequent cases of suicide in order to get rid of such pain.
- Traumatic cause associated with severe bruising directly to the base of the neck. Surgical trauma is also possible.
- Due to various tumors. In particular, this is a Pancoast tumor.
- Manifestation of an aneurysm. Very often, Horner's syndrome occurs after an aortic aneurysm.
- Inflammatory processes in the middle ear area.
- The cause may also be direct dissection of the aneurysm.
- Tumor of the thyroid gland.
- The occurrence of this syndrome may be associated with an autoimmune disease, such as multiple sclerosis.
- Tension of the stellate nerve due to the presence of an additional cervical rib.
- The cause may also be a blockage of nerve centers.
- In case of a cut in the sympathetic nerve of the neck.
- The cause may be an inherited disease that can cause tumors throughout the body. This is the so-called neurofibromatosis type 1.
Rapid destruction of the meninges or serous meningitis in children - treatment and prevention of the disease.
A particularly dangerous cerebrospinal fluid cyst of the brain, the treatment of which can only be done surgically, has its own characteristics of diagnosis and symptoms.
Causes and signs of Horner's syndrome
The main cause of this syndrome is considered to be drug treatment of diseases related to neurology, or surgical intervention. But doctors identify three groups of causes for the syndrome:
- Congenital.
- Iatrogenic.
- Acquired.
Causes and signs of Horner's syndrome
The latter is one of the most common, but congenital, on the contrary, is very rare. At birth, the disease manifests itself due to various pathological processes during embryonic development. The syndrome can be acquired due to:
Prevention of enophthalmos
As is clear from the above, there is no particular risk group when it comes to enophthalmos. This pathology can develop in anyone. The congenital form is usually diagnosed at an early age. In older people, enophthalmos occurs mainly due to tissue drying and a decrease in the volume of retrobulbar tissue, which is a natural shock absorber for the eye.
The nature of the development of enophthalmos depends on the degree of damage. Atrophic processes are always irreversible. Those tissues that die as a result of atrophy cannot be restored. Along with them, visual functions are also lost forever. However, enophthalmos is often treated quickly and successfully.
Symptoms of Horner's syndrome
Since this syndrome is directly related to the oculosympathetic nerves, the eyes are examined for signs. Horner's syndrome is easy to recognize from a photo, as there is a clear imbalance in the size of the pupils and drooping eyelids:
- The pupil of a healthy person quickly reacts to changes in light. In bright light it narrows, and in the dark it widens for better visibility. The affected pupil does not respond to changes in light or reacts slowly, that is, it is not able to adapt to external conditions (pathology of the sphincter of the pupil).
- Many children who were born with the syndrome have complete or partial heterochromia of the eyes. This is due to the fact that there is no sympathetic innervation, which makes melanin pigmentation of the iris impossible.
- Also associated with this disease is miosis - constriction of the pupil with a further inability to respond to light.
- Most often, the disease can be diagnosed due to ptosis (drooping of the upper eyelid), which is why the eyes appear asymmetrical and have a different shape. This occurs due to insufficient sympathetic innervation of the Müller muscle (superior muscle).
- Inverted ptosis is characterized by raising of the lower eyelid.
- When sympathetic innervation is disrupted, the eyeball sinks more than in ordinary people (enophthalmos).
- A person’s sweating on the affected side of the face is impaired, that is, dyshidrosis occurs.
Symptoms of Horner's syndrome
Symptoms of damage to the oculomotor nerve
To determine the presence of such a syndrome, a visual examination is sufficient. In most cases, the lesion occurs unilaterally. The severity of the manifestations often leads to the development of complexes about the patient’s appearance.
Characteristic symptoms:
- ptosis of the upper or lower eyelid;
- impaired visual acuity;
- narrowing and asymmetry of the pupils;
- impaired photoreaction;
- the pupils slowly adapt to changes in lighting;
- lack of eye reaction to the use of medications;
- hardening of the eyeball;
- decreased or complete absence of sweating on one side of the face;
- red color of the affected eye;
- difference in eye color in pediatric patients;
- chaotic placement of color pigments;
- dry eye syndrome;
- the affected part of the face sags;
- doubling of objects before the eyes.
The disease is accompanied by characteristic signs that will help diagnose the presence of this pathology. Even the presence of 1-2 symptoms may indicate the presence of this syndrome. Therefore, if there are suspicions, you should consult a doctor. Timely diagnosis will help avoid the development of complications and severe forms.
Doctors share another form - this is an incomplete syndrome. In this case, characteristic symptoms are completely absent. This leads to the danger of this pathology. Only an experienced ophthalmologist can diagnose this type of syndrome. It is difficult to cure any form of this syndrome. Initially, the doctor must determine the cause of its development, and then prescribe treatment. Efficiency is observed when using minimal electrical currents.
First order nerve fibers are the path from the hypothalamus to the Budje-Weller center, which is located in the spinal cord at the level of the cervical and thoracic vertebrae. It is called the “ciliospinal center”. First order neurons pass through the brainstem.
Next, the nerve fibers as part of the spinal nerves and nerve roots leave the spine and spread further to the stellate and middle sympathetic cervical nodes. They end in the superior cervical sympathetic node, and this pathway is called preganglionic.
From there, third-order nerve fibers, as the choroid plexus of the internal and common carotid arteries, reach the cavernous sinus, and together with the ophthalmic artery, the orbit. In this segment they are called postganglionic.
Nerve fibers regulate the functioning of the following muscles:
- The muscle that dilates the pupil.
- Muscles of the cartilage of the upper eyelid.
- Smooth muscle tissue of the orbit.
Diagnostics
It is customary to resort to tests to determine the cause of the syndrome and the delay in pupil reaction:
- A century ago, a popular method was when cocaine drops were instilled into the patient, which in a healthy person led to dilation of the pupil.
- A test using paredrin (oxamphetamine) can determine the cause of miosis (constriction of the pupil). Thanks to this method, you can find out the reaction of the third neuron, since in case of illness the pupil will not react. There are no tests to determine damage to the first and second neurons.
- The third test determines the delay in pupil reaction, which also helps in making a final diagnosis.
Diagnostic techniques
Interruption of sympathetic pathways leads to several consequences:
- Inactivates the muscle dilator and thereby provokes miosis.
- Inactivates the superior tarsal muscles, which cause ptosis.
- Inactivates the orbital muscles, which produce the effect of enophthalmos.
- Reduces the secretion of sweat on the face.
There are three main tests used to confirm Horner's syndrome:
- Cocaine drop test to cause pupil dilation. With this syndrome, the pupil does not dilate. Another method involves administering the alpha agonist Apraclonidine to both eyes and observing increased dilation (due to hypersensitivity) of the affected pupil.
- Paredrin test: The test helps to localize the cause of miosis. If the third-order neuron is not damaged, a stable dilation of the affected pupil occurs.
- Delay dilatation test.
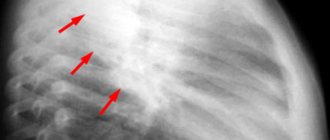
Imaging often indicates incident Horner's syndrome if it occurs in the setting of trauma or surgical manipulation.
Radiography may include, but is not limited to, radiological evaluation of the brain, cervical spinal cord, cerebral vessels, neck, head and chest.
It is necessary to distinguish between ptosis (sagging eyelid) associated with Horner's syndrome and ptosis caused by damage to the optic nerve.
In the first case, drooping of the eyelid occurs with a narrowing of the pupil, and in the second case, drooping occurs with a dilated pupil.
In addition to a direct visual examination of the patient, in order to identify obvious symptoms, as well as compiling a detailed history, there are certain diagnostic techniques, the purpose of which is to unambiguously determine the disease:
- Instillation of an M-anticholinergic solution into the eyes. With such manipulations, Horner's syndrome can be unambiguously determined, since the action of this solution causes dilation of the pupils of the eye. If the pupil does not respond, then there is a syndrome or another reason.
- Determination of eye retention time - as already noted in the symptoms, in the presence of eye syndrome, the eyes have a reduced adaptive ability to changes in light intensity. As a result, knowing the adequate adaptation time, it is possible to determine the adaptation time of the patient's eye by measuring the time.
- MRI - magnetic resonance imaging allows you to identify the formations that caused the occurrence of Horner's syndrome.
Treatment of Horner's syndrome
If the disease is idiopathic in nature, that is, it formed on its own, without the influence of other diseases, then it does not pose a danger. But if the damaged area causes severe cosmetic discomfort, then you can influence it by:
- neurostimulation;
- plastic surgery;
- medicines;
- kinesitherapy.
In neurostimulation, electrodes are applied to the affected muscles and weak electrical impulses are sent. During kinesitherapy, various massages are performed aimed at stimulating muscles and improving blood circulation in them. When prescribing treatment, the doctor will describe the disadvantages and advantages of each method so that you can choose the optimal path to recovery.
If Horner's syndrome was caused by other diseases, then the doctor conducts a full analysis using MRI, X-ray or other diagnostic tools, and only then agrees with the patient on the need for surgical intervention or other methods of eliminating the cause.
Before visiting the doctor
If you do not require immediate medical attention, you should start by consulting your GP or ophthalmologist. If necessary, you will be referred to a specialist in nervous system disorders (neurologist).
Before visiting your doctor, make a list of the following points:
- signs and symptoms of a disorder (any abnormality) that is bothering you;
- past and current illnesses or injuries;
- all medications you take, including over-the-counter medications and dietary supplements, with dosage instructions;
- any significant changes in your life, including recent stress.
Preventive measures
The specificity of Horner's syndrome is that it does not have special courses of treatment and prevention.
After all, it is often a symptom of a more complex and systemic disease, which already has direct methods of treatment and prevention.
The presence of the syndrome is very often determined only for the sake of exclusion or detection of a possible more serious disease that can threaten the patient’s life.
Bernard Horner syndrome is a specific disease associated with complications in the functioning of the sympathetic nerves , or their damage.
It has a number of specific symptoms, as well as methods of treatment and diagnosis of the disease. As a separate disease, it does not threaten the patient’s life, but only causes cosmetic and physical discomfort.
If the syndrome is caused by another, more serious disease, it can already pose a threat to a person’s life.
Treatment of this syndrome is carried out by stimulating the affected tissues or eliminating the cause of its occurrence. When treating this disease, it is important to consult a specialist in time to prevent truly dangerous complications.
Pathophysiology[edit | edit code]
Horner's syndrome occurs due to insufficient sympathetic innervation. The site of damage to the sympathetic pathways is on the ipsilateral side of the symptoms. The following are examples of conditions that cause clinical manifestations of Horner's syndrome:
- First neuron lesion (the portion of the pathway between the hypothalamus and the cervical ciliospinal center is called the first neuron (although it is probably interrupted by several synapses in the pons and tegmental region of the midbrain): central lesions involving the hypothalamospinal tract (eg, dissection of the cervical spinal cord).
- Damage to the second neuron (the area from the ciliospinal center to the superior cervical ganglion is called the second neuron (that is, these are preganglionic fibers)): preganglionic damage (for example, compression of the sympathetic pathway by a tumor of the apex of the lung).
- Damage to the third neuron (the area from the superior ganglion to the muscle that dilates the pupil is called the third neuron (these are postganglionic fibers)): postganglionic lesions at the level of the internal carotid artery (for example, a tumor of the cavernous sinus).