Etiology and pathogenesis
The reason for the development of F. m is a deficiency in the body of vitamin B12 (see Cyanocobalamin), less often a deficiency of vitamin B12 and folic acid (see) or only folic acid. The pathogenesis is not fully understood. F. m. is almost always combined with pernicious anemia (see), but its role as a direct cause of damage to the nervous system is refuted by the presence of typical cases of F. m., not accompanied by pernicious anemia and changes in the red bone marrow. There is also no correlation between the severity of anemia and the frequency of development of F. m. However, vitamin B12 deficiency is a decisive link in both the pathogenesis of pernicious anemia and the pathogenesis of F. m. Vitamin B12 is utilized by the body with the help of an internal factor (gastromucoprotein) produced stomach (see Castle factors). The absence of intrinsic factor leads to impaired absorption of vitamin B12 in the intestine, as a result of which folic acid does not convert into its active form - folinic acid. At the same time, the process of blood creation changes (see), DNA synthesis in erythroblasts is disrupted. F. m. develops in cases of lack of vitamin B12 in food (for example, in vegetarians who exclude dairy products from food); in case of impaired secretion of internal factor - with achylia of the stomach (see), after gastrectomy (see), with malabsorption syndrome (see Malabsorption syndrome) caused by sprue (see), terminal ileitis (see Crohn's disease), celiac disease (see .), tuberculous enteritis (see), pellagra (see); in cases of so-called competitive consumption of vitamin B12, when the latter is absorbed by excess intestinal flora - with intestinal diverticulosis (see), "blind loop" syndrome with enteroenteroanastomosis (see) - or helminths (see Diphyllobothriasis). Immune disorders play a certain role in the pathogenesis: more than half of patients with pernicious anemia are diagnosed with autoimmune atrophic gastritis, and antibodies to the internal factor are found in the blood plasma (see Autoantibodies).
In experiments on monkeys, it was shown that the exclusion of vitamin B12 from food after 3-4 years causes changes in the nervous system identical to F. m., although anemia does not develop.
Symptoms
Symptoms of funicular myelosis may not occur immediately. If the first signs appear, then in no case should you ignore them. Symptoms may disappear already during the first stage of treatment.
Signs of vitamin B12 deficiency:
- rapid and constant fatigue;
- discomfort and itching in the fingers;
- nausea;
- lack of appetite;
- changes in the functioning of the gastrointestinal tract;
- hair loss;
- in women there is a disruption in the menstrual cycle;
- redness in the form of small pimples on the tongue;
- depression;
- fever;
- frequent colds.
If treatment is not started on time, serious problems can occur. You may begin to experience tinnitus and severe pain in the brain. Yellow skin color and darkening of palms. Memory loss and hallucinations may occur. Often troubled by insomnia and severe dizziness.
Therapy in this case may take about six months, and complications cannot be avoided. If severe anemia develops, there is a high chance of getting stomach cancer.
Pathological anatomy
Macroscopic changes consist of moderate atrophy of the spinal cord (see). Microscopic examination reveals foci of necrosis and degeneration in the gentle and wedge-shaped bundles of the posterior cords, in the pyramidal and partially spinocerebellar conductors of the lateral cords. Sections stained for myelin reveal demyelination of afferent and efferent conductors, most pronounced in the posterior and lateral cords of the spinal cord (posterolateral sclerosis). Changes first occur in the lower cervical and upper thoracic regions, then spread up and down the spinal cord (ascending and descending degeneration). Along with the disintegration of myelin, the death of axial cylinders is observed with the formation of voids (vacuoles) separated by thin glial strands. The progressive destruction of the white matter of the spinal cord is not compensated by the proliferation of glia, since the glial reaction during F. m. is insignificant. In late stages of the disease, transverse sections of the spinal cord show only a narrow band of unaffected white matter around intact gray matter. Similar morphol. changes, but much less pronounced, are sometimes found in the white matter of the cerebral hemispheres (see). Thick myelinated sensory fibers in the distal parts of the peripheral nerves are also affected. In most cases, changes characteristic of pernicious anemia are detected: glossitis, atrophy of the gastric mucosa, red bone marrow hyperplasia, enlarged spleen, and iron inclusions in the cells of the mononuclear phagocyte system.
Treatment tactics
Treatment of funicular myelosis is carried out with replacement therapy - long-term intake of vitamin B12. Sometimes therapy is recommended throughout the patient's life. The vitamin is administered through intramuscular injections of cyanocobalamin according to the scheme. At the beginning of treatment, the body is saturated with the drug. It is prescribed daily or every other day for a week, then the frequency of administration is reduced to one injection every 7-10 days. In case of development of pernicious anemia, folic acid and iron supplements are also recommended. Achilles gastritis is subject to replacement treatment with pepsin and hydrochloric acid.
Combined sclerosis is treated with cyanocobalamin preparations
To eliminate neurological symptoms, massage courses are prescribed that reduce muscle spasticity or increase the tone of muscle tissue, depending on the stage of the pathological process. To prevent joint contractures, restore motor skills and prevent disability, therapeutic exercises are performed using an individual method for each patient.
It should be remembered that the disease responds well to treatment in the first few months from the onset of the disease. At a later date, the chances of recovery are significantly reduced.
Funicular myelosis is a severe lesion of the spinal cord, which in 90% of cases develops against the background of pernicious anemia. Timely diagnosis and treatment of the pathological process increases the chances of recovery and prevents the occurrence of disability due to the formation of paralysis of the lower and upper extremities.
With changes in the central nervous system. A pathological examination revealed in all Lichtheim's cases (there were only 3) diffuse degeneration of the posterior columns (as in tabes), as well as clearly visible foci of degeneration in the lateral columns of the spinal cord. The name “funicular myelosis” emphasizes the presence of a degenerative process in the spinal cord, affecting its long fascicles.
Pathological anatomy
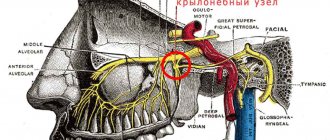
At the center of the histopathological picture of funicular myelosis is the degeneration of the lateral and posterior columns of the spinal cord. The process involves the Gaulle and Burdach fascicles in the posterior columns, the pyramidal fascicles of the lateral columns and partially the spinocerebellar fascicles. There are also degenerative changes in peripheral nerves.
Clinical picture
F. m. occurs equally often in men and women. In approximately 90% of cases, the first signs of the disease appear over the age of 40, but can be observed in childhood and old age. Paresthesias (see) appear in the form of a feeling of numbness, heat, tingling, crawling, usually occurring in the toes, less often in the fingers, hands, which gradually spread upward to the proximal limbs, and then to the stomach and chest. Sometimes there is aching pain in the legs. Gradually, progressive disturbances of the muscular-articular sense (see Proprioceptors) and vibration sensitivity (see), also more pronounced in the legs, develop, and sensitive ataxia develops (see). Sometimes there is a decrease in superficial sensitivity in the extremities with spread to the trunk, usually without a clear upper border. There is often pain when the calf muscles are compressed. Along with sensory disturbances, movement disorders also appear, which are manifested by weakness of the legs and, less often, of the arms. With moderately severe damage to the spinal cord, paresis is spastic in nature; with more severe damage to the posterior cords, muscle hypotonia occurs and paresis becomes flaccid (see Paralysis, paresis). The gradually increasing severity of damage to the posterior and lateral cords of the spinal cord determines the nature of the change in tendon reflexes (see): in the initial stages of F. m. tendon reflexes are increased, but in more than half of the patients there is a decrease and then loss of Achilles reflexes; later the knee reflexes also disappear. In the advanced stage of the disease, foot patols are constantly detected. reflexes (see Pathological reflexes) - Babinsky's symptom (see Babinsky reflex), etc. The combination of pyramidal symptoms with flaccid paresis is a feature of the wedge, the picture of F. m. There are also dysfunctions of the pelvic organs (impotence, imperative urge to urinate, retention or urinary and fecal incontinence). Typical forms of F. m. are characterized by a combination of sensitive ataxia and paraplegia (see), expressed mainly in yoga (atactic paraplegia). However, neurol. disorders can also be dissociated: isolated sensitive ataxia or spastic para- or tetraparesis are possible. Often F. m is combined with complete neuropathy (see Neuropathy), when peripheral nerves are also involved in the process along with the spinal cord. In approximately 5% of cases of F. m. there is a decrease in vision due to the development of atrophy of the optic nerves (see Optic Nerve) and the appearance of central scotomas (see Scotoma), and occasionally miosis occurs (see) with preserved pupillary reactions. In some cases, drowsiness develops. apathy, mental disorders occur, manifested by depression, emotional lability, and sometimes acute psychotic reactions. In the cerebrospinal fluid (see) there is sometimes a slight increase in protein content. An electroencephalogram (see Electroencephalography) may reveal diffuse slow activity that disappears when taking vitamin B12.
The course of F. m. is different. Along with the usual gradual development of the disease, in some cases there is an acute development of neurol. violations, with Krom for 2-3 weeks. A picture of a transverse lesion of the spinal cord with lower paraplegia, loss of all types of sensitivity, and pelvic disorders appears.
Currently, F. m is characterized by a polymorphic wedge, a picture with an atypical course in almost 50% of cases. In connection with the use of vitamin B12, classic expanded forms of F. m. rarely develop.
Diagnosis
The diagnosis with a typical wedge, picture of F. m., which developed against the background of pernicious anemia, does not present any difficulties. It should be differentiated from B12-deficiency polyneuropathy, which is observed in approximately 40% of patients with pernicious anemia and is also characterized by distal paresthesia, sensory ataxia and areflexia. A differential diagnostic sign in favor of F. m. is damage to the pyramidal system, and above all the presence of patol. Babinsky reflex or other foot pathol. reflexes.
The main difficulties of differential diagnosis arise in cases where neurol. symptoms of F. m. develop before the appearance of signs of pernicious anemia. The diagnosis of F. m. is confirmed by the detection of achilic gastritis and mega lobes in the material obtained during sternal puncture.
F. m., occurring with a dominant wedge, symptoms of damage to the posterior cords, resembles tabes dorsalis (see), however, with F. m.
there is no Argyll Robertson syndrome (see Argyll Robertson syndrome) and serological tests for syphilis (see) in the blood and cerebrospinal fluid are negative. Wedge, F.'s form of m with predominant damage to the lateral cords may resemble multiple sclerosis (see). Multiple sclerosis, in contrast to F. m., is characterized by multifocality of the lesion (including symptoms of brain damage), an increase in Achilles reflexes in most cases, and also, as a rule, a remitting course. Combined damage to the posterior and lateral cords is observed with compression of the spinal cord by a tumor or with vertebrogenic cervical myelopathy (see). Diagnosis of spinal cord compression is based on detection of blockade of the subarachnoid space using liquorodynamic tests (see) and identification of a characteristic pattern with myelography, spinal radioisotope scintigraphy, and computed tomography. In many cases of compression of the spinal cord of various origins, in contrast to F. m., a clear upper limit of sensitivity disorders is determined. The assumption of F. m. often arises when examining patients suffering from the so-called. paraplegia of middle or old age, in which spastic para- or tetraparesis progressing over many years develops with a normal composition of the cerebrospinal fluid and negative data from a myelographic study. The diagnosis of F. m. in these cases is made on the basis of identifying a deficiency of vitamin B12. An important criterion in the diagnosis of F. m. is the symmetry of the resulting neurol. defects. Pronounced asymmetry of paresis or sensitivity disorders, existing for any long time, testifies against F. m.
Diagnostics
If mental disorders are present along with anemia, the doctor suspects the development of funicular myelosis. To confirm an accurate diagnosis, it is necessary to undergo an examination. First of all, a special blood test is taken, which shows the level of vitamin B12. Then the patient is sent to a neurologist or gastroenterologist. A blood test is taken and a complete examination of the stomach and intestines is carried out.
Pathological changes are detected using magnetic resonance imaging. This diagnostic method will help to accurately identify funicular myelosis from malignant and benign tumors. A lumbar puncture is taken to exclude bacterial hematomyelia and myelitis.
An examination of the oral cavity is carried out, this makes it possible to understand changes in the tongue. If the vitamin B12 level is reduced, this indicates the presence of vitamin deficiency. If the doctor sees visual changes, then it is necessary to visit an ophthalmologist . At the first appearance, you need to visit a specialist as soon as possible. If you start the disease, complications can no longer be avoided.
Treatment
Treatment is aimed at eliminating vitamin B12 deficiency in the body.
Treatment begins with intramuscular injection of 500-1000 mcg of vitamin B12 (cyanocobalamin) daily or every 1-2 days. After 5 injections of the drug at this dose, vitamin B12 is administered at a dose of 100 mcg once a week for six months. Maintenance therapy in subsequent years consists of injections of 100 mcg of vitamin B12 once a month. In the event of an infectious disease or renal failure, the dose of vitamin B12 should be increased. If possible, it is necessary to eliminate the causes of impaired absorption of vitamin B12 in the gastrointestinal tract. tract. A diet high in B vitamins is indicated; parenteral administration of vitamins B1 and B6, as well as phosphaden 60 mg twice a day for 4-8 weeks is advisable. (repeated cycles). Prescription of folic acid in a dose of 5-15 mg per day is permissible only in cases of rarely detected folic-deficient form of F. m. Otherwise, exacerbation of neurol is possible. process. Massage and exercise therapy are prescribed. If there is a significant increase in muscle tone in the affected limbs, the use of seduxen, baclofen, and mydocalm is indicated. With paraplegia, careful skin care is necessary to prevent the development of bedsores and the prevention of urogenic infections.
Prognosis and Prevention
The forecast is determined by Ch. arr. duration of existence nevrol. symptoms before treatment; the age of patients and the severity of anemia do not play a significant prognostic role. If treatment is started a few weeks after the onset of symptoms of a spinal lesion, patients can be expected to recover; if treatment was started after a few months, there was a significant improvement. In the later stages of F. m. only a slight improvement or stabilization of the process is possible. The main regression of symptoms is noted in the first 3-6 months. treatment, further restoration of impaired functions occurs more slowly.
Prevention involves timely detection and adequate treatment of pernicious anemia, as well as careful monitoring of neurol. status of such patients in order to detect symptoms of spinal cord damage as early as possible.
Bibliography:
Alimov I. Yu. and Mandrichenko V. M. Funicular myelosis in Addison’s disease, Zdravookhr. Tajikistan, No. 1, p. 90, 1983; Davgadenkov S.N. Clinical lectures on nervous diseases, V. 4, p. 172, JI., 1961; Martynov Yu. S., Malkova E. V. and Chekneva N. S. Changes in the nervous system in diseases of internal organs, M., 1980; Multi-volume guide to neurology, ed. S. N. Davidenkova, vol. 3, book. 2, p. 902, M., 1962, bibliogr.; Guide to Hematology, ed. A. Vorobyova and Yu. I. Lorie, p. 376, M., 1979; Evans DL, E del sohn G. A. a. Golden RN Organic psychosis without anemia or spinal cord symptoms in patients with vitamin B12 deficiency, Amer. J. Psychiat., v. 140, p. 218, 1983; Folic acid in neurology, psychiatry, and internal medicine, ed. by M. I. Botez a. E. H. Reynolds, p. 427, NY 1979; Reynolds EH Pathogenesis of subacute combined degeneration, Lancet, v. 2, p. 1109, 1981; Shorvon SD ao The neuropsychiatry of megaloblastic anemia, Brit. med. J., v. 281, p. 1036, 1980.
D. P. Shtulman.