Functional neurological symptom disorder, also called conversion disorder, is a complex condition where patients experience physical neurological symptoms but no obvious structural problem in the nervous system. The exact cause is not entirely clear, although stress may be a major factor.
According to the National Organization for Rare Disorders, functional neurological symptom disorder (FND) is thought to occur in 14 to 22 cases per 100,000 people.
Although it can affect children, FND is more common among teenagers and adults. People in rural areas and military personnel may be at higher risk of developing TNF than other groups.
symptoms
Individuals who have FND experience physical symptoms. However, these symptoms do not have an underlying physical cause and are often associated with an emotional or psychological crisis.
A person with FND has no control over the symptoms they experience and does not consciously or intentionally produce them.
Typical signs and symptoms of FND include:
- deafness or difficulty hearing
- difficulty concentrating
- Difficulty swallowing
- fatigue
- movement disorder
- lack of responsiveness
- loss of balance
- loss of senses such as smell or touch
- memory problems
- numbness
- pain in muscles, skin or joints
- paralysis
- seizures
- speech problems
- tingling in the skin
- tremor
- twitching
- vision problems
- weakness
Duration and severity of symptoms
Signs may come and go, or they may persist, and they may vary depending on their severity and location.
In most cases, symptoms resolve within a short period of time. However, in some people they can last for months or years and can interfere with a person's ability to work and carry out daily activities.
According to FND Hope, a nonprofit advocacy organization for FND patients, FND symptoms can be as debilitating as multiple sclerosis (MS) or Parkinson's disease.
causes
The exact cause of FND is unknown.
One theory is that FND is the result of an "internal conflict" and the symptoms are the body's attempt to provide a solution to this stress.
For example, someone who believes violence is wrong but feels the urge to react violently to a traumatic situation may experience numbness in their hands or feet as a way to suppress the urge to hit or hit.
However, some people can develop FND even in the absence of stress or depression.
Some studies have shown that people with FND have reduced functional connectivity in certain parts of their brain, including parts that control muscles and senses. This indicates a lack of control over the body's physical movement or actions.
Hydrocephalus - is it serious?
Numerous vessels in the meninges produce a specific fluid that washes the structures of the brain and spinal cord. It is called cerebrospinal fluid, or cerebrospinal fluid. Sometimes, under the influence of certain factors, the production of cerebrospinal fluid or its absorption is disrupted. Fluid accumulates, and we see an increase in the size of the baby's head - this is a disorder called hydrocephalus. Typically, such changes are diagnosed using ultrasound during intrauterine development - we are talking about congenital hydrocephalus. However, the disease can develop after the birth of the child.
Hydrocephalus is always serious! Due to the accumulation of fluid, brain structures are compressed. It is extremely important to reliably exclude or confirm this diagnosis in order to prescribe the correct treatment if necessary.
ADVICE. Have you noticed that the baby's head is larger than expected for her age? Don’t be alarmed: not only the size matters, but also the condition of the so-called ventricles and cerebrospinal fluid spaces of the brain. Special studies (for example, neurosonography) will help clarify the situation.
diagnostics
Diagnosing FND can be time-consuming because the symptoms are not caused by an underlying physical condition and can mimic those of many other disorders. Doctors should not diagnose FND because tests for other conditions have come back negative.
In many cases, both the diagnosis and the neurologist and psychiatrist. A neurologist will help rule out underlying neurological conditions, while a psychiatrist can rule out other psychological causes and confirm the diagnosis of FND.
Although there is no standard test to check for FND, tests commonly used for diagnosis include:
Health assessment and physical examination
The doctor will note any symptoms the person is experiencing and ask about life changes, traumas, and major stressors. The doctor may also obtain a complete medical and family history.
The doctor may also perform function tests to check for normal reflexes, balance problems, and physical movement.
Image testing
X-rays and MRI scans can reveal whether symptoms are due to brain injuries or neurological abnormalities.
An EEG (electroencephalogram) scan tracks brain waves, allowing doctors to identify problems related to the electrical activity of the brain, such as epilepsy.
DSM criteria
The psychiatrist will use the diagnostic criteria outlined in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to make a diagnosis.
To be diagnosed with FND, people:
- must have one or more symptoms that affect their movement or feelings and are outside their conscious control
- should not be able to attribute their symptoms to drug use or a physical or neurological condition
- may attribute their symptoms to a traumatic or stressful event (although this does not always have to be the case)
How dangerous is hypertension in a baby?
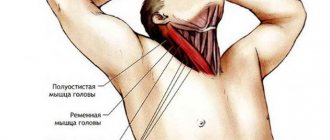
The phenomena of muscle hypertonicity are natural for a newborn and should gradually disappear by the 3rd month of life. During pregnancy or childbirth, under the influence of various negative factors, the influence of the central nervous system on muscle tone may be too great. As a result, spasticity, trembling of the arms and chin while crying, frequent and profuse regurgitation and general restlessness of the baby develop. Excessive muscle tension interferes with the normal development of the child’s motor system, which can lead to retardation in physical development.
ADVICE. Hypertonicity may be a secondary condition after any severe damage to the central nervous system. It is important that a specialist, using examination and additional research methods, exclude organic damage to brain structures. And you can cope with hypertension!
Common misdiagnoses
Due to the symptoms of FND, there is a possibility that the condition will be misdiagnosed.
A 2005 review indicated that the misdiagnosis rate for FND has averaged approximately 5 percent since 1970. Another report found that 41 percent of people with rare diseases will be misdiagnosed at least once.
Common misdiagnoses include:
- Guillain-Barré syndrome: a rare autoimmune disease characterized by muscle weakness and pain.
- HIV or AIDS.
- Health abuse: a psychological disorder characterized by excessive thoughts about having an undiagnosed illness.
- Lupus: an autoimmune disease with symptoms including fatigue and joint pain.
- Myasthenia gravis: A muscle weakness disorder.
- Neurological disorders: disorders that affect the central nervous system, such as epilepsy, multiple sclerosis, polyneuropathy and Parkinson's disease.
- Spinal cord injury.
- Stroke.
What negatively affects the development of a baby’s nervous system?
The functioning of the child’s nervous system may be negatively affected in the future by certain illnesses of the mother during pregnancy (especially of viral origin), the threat of miscarriage, or taking certain medications. Nerve cells are extremely sensitive to lack of oxygen. Severe anemia in an expectant mother can cause oxygen starvation in the baby developing in the tummy, which will ultimately affect the functioning of his nervous system.
ADVICE. A pregnant woman should carefully take care of her health. The baby is especially vulnerable in the early stages of pregnancy. If you suffered any illness while carrying your baby, be sure to tell your doctor about it!
treatment
Symptoms may resolve without treatment in some people with FND, especially after they are confident that their symptoms are not related to a more serious health condition.
However, treatment may be helpful for those who:
- other (associated) psychological conditions
- severe FND symptoms
- symptoms that resolve slowly
- recurring symptoms
In general, doctors recommend a combination of procedures. These procedures include:
- Psychotherapy. People with FND related to a stressful or traumatic event or underlying mental health condition may benefit from working with a therapist or psychologist. Some people with FND undergo cognitive behavioral therapy (CBT).
- Physiotherapy. Physical symptoms of FND, such as impaired movement or muscle weakness or pain, can be treated with physical therapy.
- Drug treatment. Anti-anxiety medications or antidepressants may help relieve the stress or anxiety that may be contributing to FND.
- Transcranial magnetic stimulation (TMS). This treatment uses magnetic fields to stimulate specific parts of the brain. TMS has been reported to be beneficial for people with FND, but there is limited evidence at this stage.
- Lifestyle changes. Participating in activities that relieve stress and anxiety, such as yoga, meditation, and progressive muscle relaxation, may be helpful for some people with FND. Eating a balanced diet, getting enough sleep, fostering positive relationships and maintaining a good quality of life also help reduce stress.
Functional disorders in neurological practice
G.M. DUKOVA
, Doctor of Medical Sciences, Professor,
First Moscow State Medical University named after.
THEM. Sechenov The article discusses the main clinical manifestations, approaches to diagnosis and modern methods of treating functional disorders.
More than 30% of patients visiting a neurologist complain of somatic symptoms that cannot be explained by any organic disease [19, 20]. Such patients are often recommended expensive research and treatment, consultations with various specialists, which, as a rule, do not lead to a positive result, causing dissatisfaction for both the patient and the doctor [1]. The most common disorders in this category of patients are tension headaches and other chronic pain syndromes, conversion disorders, hyperventilation syndrome, dizziness, asthenia, depression, anxiety and somatoform disorders [16, 19].
In domestic medicine, such disorders are most often referred to as “vegetative dystonia syndrome” (G-90.9) or “astheno-neurotic reactions”; in therapeutic practice the term “neurocirculatory dystonia” is used. Some authors use the term “psychovegetative syndrome”, proposed in the 60s of the last century by German internists [2].
In foreign literature there is also no uniform terminology to refer to this group of disorders. In recent decades, authors have increasingly resorted to terms such as “medically unexplained symptoms” [18] or “subjective health complaints” [22], however, these are not satisfactory, because they are based not on positive, but on negative criteria.
Recently, it has been proposed to use the term “functional” and designate disorders in the somatic sphere with the term “functional somatic symptoms”, and in the neurological sphere with the term “functional neurological symptoms”. The advantage of this term is its “positive” meaning and patient acceptability, since dysfunction is emphasized, there is no definition of “unexplained” that worries the patient, as well as the mention of a psychogenic factor, which usually causes internal resistance of the patient, even if this is not realized by the patient.
Main clinical manifestations of functional disorders:
— Autonomic (permanent and paroxysmal) — Chronic pain syndromes — Motivational — Functional-neurological — Emotional-affective — Behavioral
Autonomic disorders
The main characteristic of autonomic disorders is their polysystemic nature. Table 1
The main manifestations of autonomic disorders are presented.
| Table 1. Clinical syndromes of autonomic disorders |
| Cardiovascular system: cardiorhythmic, cardiac, cardiosenestopathic syndromes, as well as arterial hypertension and hypotension or amphotonia. Respiratory system: hyperventilation disorders - a feeling of lack of air, shortness of breath, a feeling of suffocation, difficulty breathing. Gastrointestinal system: dyspeptic disorders (nausea, vomiting, dry mouth, belching, etc.), abdominal pain, flatulence, rumbling, constipation, diarrhea. Thermoregulation and sweating: non-infectious low-grade fever, periodic chills, diffuse or local hyperhidrosis. Vascular regulation: distal acrocyanosis and hypothermia, Raynaud's phenomenon, hot and cold flashes. Vestibular system: non-systemic dizziness, feelings of one’s own instability and instability of the surrounding world, a feeling of “lightheadedness”, pre-fainting states. Urogenital system: pollakiuria, cystalgia, itching and pain in the anogenital area, dyspareunia. |
Analysis of the semiotics of autonomic disorders requires determining the type of their course: permanent and/or paroxysmal. Permanent autonomic disorders mean subjective and objectively recorded disorders of autonomic functions that are permanent or occur sporadically. These disorders may manifest predominantly in one system or have a distinct multisystem nature.
Paroxysmal autonomic disorders, autonomic crises or panic attacks (PA) are the most striking and dramatic manifestation of the psychovegetative syndrome.
The following criteria are used to diagnose panic disorders:
1. Sudden, sometimes unexpected appearance of 4 or more symptoms: - vegetative (cardiovascular, respiratory, vasomotor, etc.); - vestibular (dizziness, instability, etc.) - emotional-affective (panic, fear, aggression, etc.) - dissociative (derealization, depersonalization) 2. Anticipation and repetition of these episodes 3. Constant worry about the consequences of attacks 4. Behavior changes in connection with panic attacks (agoraphobia and restrictive behavior) 5. The appearance of attacks regardless of any organic factor (for example, caffeine intoxication or hyperthyroidism).
Attacks consisting of several symptoms are called “abortive” or “minor”. If during an attack the patient experiences most of the above symptoms, then they speak of “extended”, “large” PA.
There are several types of PA depending on the dominant symptoms: respiratory, vestibular, cognitive and “non-insured”, as well as by the time of occurrence: night/day attacks [9].
Outside of attacks, agoraphobic syndrome is most often observed, which ultimately manifests itself as fear of a situation potentially threatening the development of PA and difficulty in obtaining medical care. Such situations can be being in a crowded room, in a store, transport, cinema, alone at home or in the country. Agoraphobia is the factor that determines the psychological and social consequences of PA, namely restrictive behavior and secondary depression. It is these consequences that are the target for therapeutic interventions (psychotherapy and psychopharmacotherapy).
Chronic pain syndromes
In clinical practice, chronic pain syndromes make up a significant proportion of patients. Beyond the clearly defined somatogenic and neuropathic pain, there are a variety of chronic pain syndromes labeled as “functional,” “medically unexplained,” “dysfunctional,” “somatoform,” “somatized,” “psychogenic,” etc.
Chronic pain syndromes observed in clinical practice
— Headaches — Atypical facial pain — Pain in the left side of the chest (“non-cardiac pain”) — Back pain — Abdominal pain — Pain in the lower abdomen (pelvic pain) — Anogenital pain — Pain throughout the body (fibromyalgia) Currently the above chronic pain syndromes of different localization, together with other symptoms (mental, autonomic, motivational and neuroendocrine) are regarded as functional based on common factors that are naturally observed in all these forms. These include: the frequent combination of different syndromes in the same patient, both simultaneously and sequentially, the predominance of women, emotional disorders and a history of childhood psychotrauma, the leading role in the pathogenesis of these syndromes of dysfunction of certain cerebral systems (limbic parts of the brain, prefrontal and parietal cortex ) and the therapeutic effectiveness of antidepressants.
Currently, there are 2 groups of factors that are involved in the chronicization of pain syndromes: biological and psychosocial, the structure of which is presented in Table 2
.
| Table 2. Biological and psychosocial factors of pain chronification | |
| Biological factors | Psychosocial factors |
| Genetically inherited features of nociceptive and antinociceptive systems | Psychogenic factors of childhood (physical, moral and sexual abuse) |
| Processes of peripheral and central sensitization, inflation (Wind-up) | Personality characteristics of patients (anxious suspiciousness, sensitivity, passive-aggressive traits, masochism, hypochondriasis, social dependence, pessimism, demonstrativeness) |
| Inclusion of muscle factor | Current stress and conflicts |
| Abuse factor (abuse of analgesics) | Rental installations |
| Availability of medical care | |
Diagnosis of chronic pain syndrome includes the following:
1. Exclusion of possible somatic (organic) factors causing pain. 2. Clarification of the temporal characteristics of pain. Duration of pain: most of the day, at least 15 days per month, lasting at least 6 months. 3. Qualitative characteristics of pain: monotonous pain, periodically intensifying before an attack, in the description of pain the use of non-pain terms (“cotton head”, “stuffiness” in the left half of the chest, “unpleasant tickling” in the lumbar region, etc.), senestopathic coloring of pain. 4. The localization of pain during examination and palpation is always much wider than the patient presents. 5. Painful behavior - marking a “sick” organ - immobilizing it, constantly rubbing the skin in the heart area, regularly taking analgesics, and if they have no effect, regularly calling an ambulance. 6. Psychogenesis of pain. Presence of close relatives suffering from pain. Often the patient himself experienced pain, or observed it in emotionally charged situations, for example, the death of a parent from a myocardial infarction with severe pain. 7. Beaten paths. Debut or exacerbation of chronic pain after injuries, surgical interventions, infectious diseases. 8. Syndromic environment, including psychovegetative and motivational disorders.
Functional neurological symptoms
This term refers to neurological symptoms that do not have an underlying organic cause. In the practice of a neurologist, such symptoms account for up to 19% of outpatient visits [16] and 9% of hospitalized patients [10]. In modern classifications, they belong to the headings of “dissociative (conversion)” disorders in ICD-10 or “somatoform” disorders in DSM-IV.
The clinical phenomenology of functional neurological disorders (FNS) is presented as follows:
1. Paralysis and paresis 2. Paroxysmal disorders (seizures) 3. Gait disorders 4. Sensory disorders 5. Visual and oculomotor disorders 6. Dyskinesia 7. Speech and voice disorders 8. Impairments of consciousness 9. Cognitive impairments
Functional neurological disorders can be observed both in the structure of PA and in the permanent version. A special study showed that in the structure of a typical panic attack, up to 30% of symptoms can be classified as FNS [23]. Often they are the subject of special concern for relatives and diagnostic errors of doctors.
Diagnosis of these disorders requires special awareness of the typical neurological manifestations of hysteria, as well as the use of specific tests and samples [25, 21].
Violation of biological motivations
There are 4 basic biological motivations that are basic for preserving life, the full functioning of the body and procreation. These include the need for food intake, the need for sleep and sexual activity. Separate and important for human existence is the need for activity, action, participation in society, etc. The mechanisms of motivation at the cerebral level are primarily associated with the activity of the limbic-reticular complex systems, which regulate adaptive behavior in response to any type of stress.
With functional disorders, disturbances occur in the sphere of motivation. Their syndrology is presented below:
— Eating disorders (anorexia with weight loss or bulimia with weight gain) — Dissomnia disorders (difficulty falling asleep, early awakenings, shallow sleep, hypersomnia, parasomnia) — Sexual disorders (decreased libido, potency, anorgasmia, etc.) — Asthenia (weakness, fatigue) As a rule, patients do not focus attention on them, but with active questioning it is possible to reveal that “there is no appetite, and even the smell of food causes nausea” or, conversely, “you constantly want to eat and even have to get up at night to do this” , patients often talk about certain sleep disorders. Problems in the area of intimate life often appear before the onset of the disease, and during the course of the disease, sometimes sexual life “comes to naught.”
Separately, it is necessary to dwell on the violation of motivation for activity. Clinically, this manifests itself as asthenic syndrome. Asthenic syndrome is one of the most common syndromes in the clinical practice of any doctor. The key words in asthenia are “weakness” and “fatigue,” which are characterized by the fact that they occur not only with exertion, but also without it, and do not go away after rest. Since the feeling of fatigue is a key trigger for rest, the essence and meaning of the feeling of fatigue and weariness is an urge to stop activity, activity, any effort, etc. Reducing activity is a universal psychophysiological mechanism for preserving the vital activity of the system in the event of any threatening situation, operating according to the principle : less activity means less energy requirement. With asthenia, not only the real threat of depletion of energy reserves, but also an imaginary threat (emotional overstrain, stress, conflicts) are triggers for feelings of fatigue and weakness. It has been shown that changes in the sphere of motivation are key to the formation of asthenia in humans [26, 27, 6].
Emotional, affective and behavioral disorders
Patients with functional disorders usually turn to a neurologist with specific somatic complaints, such as pain, dizziness, shortness of breath, lump in the throat, sleep disturbances, etc. and, as a rule, do not complain about emotional disorders and do not associate symptoms that worry them with them. Moreover, they regard even fear in the structure of PA as secondary to “increased pressure,” “choking,” “palpitations,” or “dizziness.” This is what causes misdiagnosis and inadequate treatment. The identification of emotional disorders is complicated by the alexithymia inherent in such patients. Alexithymia refers to the patient’s difficulty in recognizing, expressing and describing (verbalizing) his own feelings, state of mind and emotions experienced by himself or other people, as well as difficulties in distinguishing between emotions and bodily sensations. Psychometric tests are usually used to identify emotional disorders and alexithymia. However, clinically it is also possible to get an idea of the patient’s disturbing thoughts, threats, perceptions and associated emotions. To do this, it is enough to purposefully ask the patient how he behaves at the moment the symptom appears, in what situation the symptom appears, how the symptom affects his physical and social functioning, what actions the patient takes to avoid the “consequences of the disease” he imagines. It is often possible to identify distinct restrictive behavior, repeated tests that bring relief for a short time, obsessive rituals (constant measurement of blood pressure, precautionary use of painkillers), etc.
Thus, in the practice of a neurologist, many patients experience a variety of autonomic, neurological, motivational and behavioral disorders, in which all available research methods do not reveal an organic cause and which today are designated as functional disorders.
Therapy for functional disorders
The vast majority of patients with functional disorders are observed and treated either by neurologists or general practitioners. The dominance of asthenia, pain and autonomic syndromes in the clinical picture, the hidden nature of emotional disorders often prompts doctors to use predominantly somatotropic drugs in therapy: antihypertensive and vegetotropic drugs, analgesics, vascular-metabolic therapy, antioxidants, adaptogens, etc. And only in the case of obvious For emotional disorders, tranquilizers may be included in therapy. Such therapy often turns out to be ineffective, undermining the patient’s faith in the possibility of a cure and contributing to the chronicity of the process.
Already at the first contact, the doctor must determine the further strategy for managing the patient. At the first stage, it is absolutely necessary to exclude an organic disease, which can manifest itself with similar symptoms. A detailed clinical and paraclinical examination of the patient also has a psychotherapeutic value, showing the seriousness of the doctor’s attitude towards the patient and objectively convincing the patient of the absence of a threatening disease.
Despite the fact that pain and autonomic disorders are the most obvious in the clinical picture, psychopharmacology is currently the basic method of treatment. Psychotherapy also plays a significant role.
The main goals of therapy for functional disorders are:
1. Relief of the leading symptom or syndrome 2. Impact on secondary syndromes (agoraphobia, depression, anxiety, asthenia). 3. Prevention of relapses and further progression of the disease. For this purpose, symptomatic, pathogenetic and preventive therapy is used. Sometimes an explanatory conversation with a doctor about the essence of the disease, possibly in combination with placebo therapy, is sufficient. Our studies have shown that in 35-42% of patients suffering from panic disorder, significant improvement was achieved only with the help of placebo therapy [4].
Symptomatic therapy
aimed at quickly relieving the leading symptom. This stage of therapy has several goals. Firstly, rapid relief of the patient’s condition, which in itself has a psychotherapeutic effect, since it removes the fear of a threatened and incurable disease. Secondly, relief of the leading symptom prevents the process from becoming chronic. Thus, rapid and early relief of acute back pain prevents the development of persistent muscle spasm, which is an important pathogenetic mechanism for the formation of chronic back pain. Early and successful relief of panic attacks prevents the development of agoraphobic syndrome and restrictive behavior, which are the main factors of social disability in patients with panic disorders.
Symptomatic therapy can be represented by a variety of techniques. Thus, to relieve hyperventilation disorders, it is advisable to teach the patient breathing exercises, which he can use both to relieve panic attacks and to correct respiratory disorders outside of an attack. For most functional symptoms, pharmacological drugs are used as symptomatic therapy - the so-called “treatment on demand”: to relieve nausea - prokinetics (cerucal), to reduce tachycardia - beta-blockers, to relieve pain - non-steroidal anti-inflammatory drugs and muscle relaxants, for relief paroxysms (panic attacks) - tranquilizers. It is necessary to remember and explain to the patient that this treatment operates on the “here and now” principle and is a short-term therapy, which will be canceled as the main pathogenetic therapy takes effect. Moreover, the patient’s healing process is characterized by a decrease in the need for these “life-saving” drugs. Often the patient himself does not yet realize a noticeable improvement in his condition, and the doctor can make him understand this if in a conversation he focuses the patient’s attention on the number of symptomatic medications taken in the last week. Thus, the effectiveness of pathogenetic therapy is substantively proven to the patient.
Pathogenetic therapy
is focused on preventing the reappearance of paroxysmal manifestations (panic attacks, psychogenic seizures, pain attacks, etc.), regression of the abusive factor, relief of anticipation anxiety, agoraphobic syndrome and restrictive behavior, secondary depression, asthenia and other motivational disorders.
Therapy aimed at the formation of new patterns and stereotypes
of motor behavior, cognitive aspects of thinking, motivation, emotional-affective and behavioral reactions is important.
Numerous multicenter placebo-controlled studies have shown that antidepressants (ADs) are the basic drugs in the treatment of functional disorders. It has been found that AD can be effective in chronic pain syndromes of various localizations [3], panic disorders [8, 7, 17], asthenia [15] and appetite disorders [11]. Moreover, ADs are effective regardless of whether these syndromes are combined with depression or not, and the doses used for the treatment of functional disorders are lower than for the treatment of depression.
It should be noted that the pronounced side effects of a number of ADs, in particular tricyclic ADs, significantly reduce the possibility of their use, especially in outpatient practice. Therefore, the drugs of first choice are currently drugs from the group of selective serotonin reuptake inhibitors - SSRIs (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram and escitalopram).
Escitalopram belongs to the second generation of SSRIs, since it has a slightly different mechanism of action than other serotonergic antidepressants: it interacts not only with the primary binding locus of the serotonin transporter protein, but also with the secondary (allosteric) one, which leads to faster, more powerful and persistent blockade of serotonin reuptake due to the modulating effect of allosteric binding. At the same time, escitalopram is the most selective of the SSRI antidepressants, since it practically does not bind to serotonin (5-HT), dopamine (D-1 and D-2), α-adrenergic, histamine, m-cholinergic receptors, as well as benzodiazepine and opiate receptors. receptors [14].
M. Mazza et al. [12] revealed the effectiveness of escitalopram at a daily dose of 20 mg in the treatment of chronic lumbar pain. Therapy with escitalapram has been shown to be effective in patients with panic disorders [24]. Muller et al. studied the effectiveness of escitolapram in patients with “multisomatoform disorders,” which refers to “medically unexplained symptoms,” in a double-blind, placebo-controlled manner. At the 12th week of treatment, escitalopram was effective in 84.0% of patients, in contrast to 26.9% on placebo [13].
The most common side effects when taking escitalopram were nausea and headache, which were mild, transient and disappeared within 2-3 weeks. Escitalopram does not cause significant inhibition of the activity of the main isoenzymes of the cytochrome P 450 family in vitro, and therefore it is unlikely to be involved in clinically important pharmacokinetic drug interactions in patients.
Thus, high efficiency at a minimum dose, minor and quickly passing side effects, as well as the absence of drug interactions make escitalopram an indispensable drug in the treatment of elderly and somatically burdened patients. Treatment adherence in patients taking escitalopram is significantly higher than in similar studies with other antidepressants.
In 2014, a domestic generic version of escitalopram appeared on our market - the drug Asipi (JSC Veropharm). Based on comparative pharmacokinetics, it is shown that the drug Asipi is bioequivalent to the original drug Cipralex.
When determining the tactics of blood pressure therapy, it is necessary to resolve two main issues: choosing a drug and determining the dose.
The choice of drug is determined mainly by the clinical picture of the disease and the characteristics of the drug. When determining the dose of the drug, the following rules may be useful:
1. Taking into account the individual sensitivity and anxious suspiciousness of this category of patients, it is advisable to begin therapy with small doses (1/2-1/4 of the planned dose) with a gradual increase over 3-5 days. 2. The criterion for limiting the dose may be the severity of side effects that do not disappear within 3-5 days. 3. A daily distribution of the drug is recommended depending on the hypnogenic effect.
Before prescribing a course of drug therapy, the doctor must explain to the patient the basic principles of treatment and warn about possible difficulties in the treatment process. In this conversation, it is necessary to emphasize the following points:
1. The essence of the treatment is that it is aimed at preventing the recurrence of attacks and the social adaptation of the patient. 2. The effect of therapy may be delayed, since in most ADs the effect appears with a latent period of 14-21 days from the start of their use. 3. The course of treatment should be long, sometimes it can last up to a year. 4. Abrupt withdrawal of drugs at any stage of treatment can lead to exacerbation of the disease, therefore, at the end of treatment, drug withdrawal is carried out very gradually. Psychotherapeutic approaches to the treatment of functional disorders
can be conditionally divided into 3 types: 1) psychotherapy aimed at relieving individual symptoms and improving the general condition of the patient 2) aimed at pathogenetic mechanisms; 3) person-oriented (reconstructive) psychotherapy.
Symptomatic psychotherapy includes techniques aimed at influencing individual neurotic symptoms and the general condition of the patient. This is auto-training (in individual and group modes), hypnosis, suggestion and self-hypnosis. With the help of such techniques, anxiety is relieved, optimism and self-confidence are imparted, and the patient’s motivation for recovery is enhanced.
The second group includes cognitive behavioral psychotherapy, conditioned reflex techniques, body-oriented methods, and neurolinguistic programming. The main goal of cognitive behavioral therapy is to help the patient change the pathological perception and interpretation of painful sensations, since these factors play a significant role in the maintenance of symptoms. Cognitive behavioral therapy may also be useful in teaching the patient more effective coping strategies, which in turn may lead to increased adaptive capacity.
The third group consists of methods aimed directly at the etiological factor. The essence of these techniques is person-oriented psychotherapy with the reconstruction of the basic motivations of the individual. These techniques are aimed at revealing early childhood conflicts or current personality problems; their main goal is the reconstruction of personality. This group of methods includes psychodynamic therapy, Gestalt therapy, and family psychotherapy.
When functional disorders are combined with obvious hysterical, senesto-hypochondriacal, obsessive and/or phobic manifestations, small doses of antipsychotics are used as an addition to basic pharmacotherapy with antidepressants - Melleril (Sonapax), Theralen, Eglonil, Tiapridal, Chlorprothixene, Seroquel, Etaparazine, Neuleptil.
Non-drug therapy
Methods of non-drug therapy include information and educational programs, physical training, massage, therapeutic exercises, hydrotherapy (water gymnastics, swimming, contrast showers, Charcot shower), breathing exercises, acupuncture, complex treatment with thermo-, odorous, music and light effects carried out in a specially designed capsule, biofeedback methods, exposure to transcranial magnetic stimulation, etc. Thus, most modern researchers believe that physical activity is a priority in the treatment of asthenia. Empirical evidence and analysis of randomized controlled trials suggest that 12 weeks of graded exercise therapy, especially when accompanied by patient education programs, can significantly reduce feelings of fatigue and tiredness.
Thus, at present, a large group of patient complaints and physical symptoms are united on the basis of the absence of organic pathology and the presence of common pathophysiological mechanisms in their origin. Comprehensive treatment, in which the treatment of blood pressure is a priority, makes it possible to successfully cope with these socially disabling sufferings.
Literature
1. Barsky AJ, Orav EJ, Bates DW: Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Archives of General Psychiatry, 2005, 62: 903-910. 2. Delius L. Fahrenberg J. Psychovegetative Syndrome Thieme, 1966: 290. 3. Dharmshaktu P, Tayal V, Kalra BS. Efficacy of antidepressants as analgesics: a review. J Clin Pharmacol, 2012, 52(1): 6-17. Epub 2011 Mar 17. 4. Dyukova GM, Shepeleva IP, Vorob'eva OV. Treatment of vegetative crises (panic attacks). Neurosci Behav Physiol, 1992, 22(4): 343-5. 5. Fishbain D. Evidence-based data on pain relief with antidepressants. Ann Med, 2000, 32(5): 305-16. 6. Floris P de Lange, Joke S Kalkman, Gijs Bleijenberg, Peter Hagoort, Sieberen P vd Werf, Jos WM van der Meer and Ivan Toni Neural correlates of the chronic fatigue syndrome—an fMRI study. Brain, 2004, 127(9): 1948-1957. 7. Freire RC, Hallak JE, Crippa JA, Nardi AE. New treatment options for panic disorder: clinical trials from 2000 to 2010. Expert Opin Pharmacother, 2011, 12(9): 1419-28. 8. Gorman JM. The use of newer antidepressants for panic disorder. J Clin Psychiatry 1997, 58 Suppl 14:54-8; discussion 59. 9. Kircanski K. Craske MG, Epstein A. Wittchen HU. Subtypes of Panic Attacks: A critical review of the empirical literature. Depression and Anxiety, 2009, 26: 878–887. 10. Lempert T, Dieterich M, Huppert D, Brandt T. Psychogenic disorders in neurology. Frequency and clinical spectrum. Acta Neurol Scand 1990, 82: 335–340. 11. Leombruni P, Piero A, Lavagnino L, Brustolin A, Campisi S, Fassino S. A randomized, double-blind trial comparing sertraline and fluoxetine 6-month treatment in obese patients with binge eating disorder. Prog Neuropsychopharmacol Biol Psychiatry, 2008, 32(6): 1599–1605. 12. Mazza M, Mazza O, Pazzaglia C, Padua L, Mazza S. Escitalopram 20 mg versus duloxetine 60 mg for the treatment of chronic low back pain. Expert Opin Pharmacother, 2010, 11(7): 1049-52. 13. Muller JE, Wentzel I, Koen L, Niehausb DJH. Seedat S and Stein DJ. Escitalopram in the treatment of multisomatoform disorder: a double-blind, placebo-controlled trial. Int Clin Psychopharmacol 2008, 23: 43–48. 14. Owens MJ, Knight DL, Nemeroff CB. Second-generation SSRIs: human monoamine transporter binding profile of escitalopram and R-fluoxetine. Biol.Ps., 2001, 50: 345–50. 15. Pae CU, Marks DM, Patkar AA, Masand PS, Luyten P, Serretti A.Pharmacological treatment of chronic fatigue syndrome: focusing on the role of antidepressants. Expert Opin Pharmacother, 2009, 10(10): 1561-70. 16. Perkin GD. An analysis of 7836 successful new outpatient referrals. J Neurol Neurosurg Psychiatr 1989, 52:447-448. 17. Pollack MH, Allgulander C, Bandelow B, Cassano GB, Greist JH, Hollander E, Nutt DJ, Okasha A, Swinson RP; World Council of Anxiety. WCA recommendations for the long-term treatment of panic disorder. CNS Spectr, 2003, 8(8): 17-30. 18. Sharpe M, Mayou R, Bass C. Concepts, theories and terminology. In: Mayou R, Bass C, Sharpe M, eds. Treatment of functional somatic symptoms. Oxford: Oxford University Press, 1995: 3–16. 19. Stone J, Carson A, Duncan R, Coleman R, Roberts R, Warlow C, Hibberd C, Murray G, Cull R, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker J, MacMahon AD. Sharpe M. Symptoms 'unexplained by organic disease' in 1144 new neurology out-patients: how often does the diagnosis change at follow-up? Brain, 2009, 132: 2878–2888. 20. Stone J et al. “Who is referred to neurology clinics?—the diagnoses made in 3781 new patients.” Clin Neurol Neurosurg, 2010, 112(9): 747-51. 21. Stone J, Carson A, Sharpe M. Functional symptoms and signs in neurology: assessment and diagnosis. J Neurol Neurosurg Psychiatry 2005, 76: 2-12. 22. Ursin H, Eriksen HR. Sensitization, subjective health complaints, and sustained arousal. Ann NY Acad Sci 2001, 933: 119-29. 23. Vein AM, Dyukova GM, Vorobieva OV. Is panic attack a mask of psychogenic seizures? A comparative analysis of phenomenology of psychogenic seizures and panic attacks. Functional neurology, 1994, IX(3): 153-161. 24. Waugh J, Goa KL. Escitalopram: a review of its use in the management of major depressive and anxiety disorders. CNS Drugs, 2003, 17(5): 343-62. 25. Dyukova G. M. Basic principles for diagnosing hysteria in neurology. Selected lectures. Eidos-Media, 2006: 316-337. 26. Kulikovsky V.V. Clinical and pathogenetic aspects of asthenic syndrome of psychogenic and somatogenic genesis. Moscow, 1994. Diss. doc. med. sc. P. 482. 27. Rodshtat I.V. Questions of the clinic and pathogenesis of asthenic conditions (neurological and psychological analysis). M. Diss. Ph.D. med. sc. 1967. P. 265.
Source
: Medical Council, No. 5, 2015
forecast
The duration and severity of symptoms vary from person to person. Typically, symptoms are not life-threatening, but complications that arise can be debilitating or reduce a person's quality of life.
Once reassured that their symptoms are not related to a physical condition or serious illness, many people with FND recover.
However, some people may experience persistent symptoms, recurring symptoms, or the development of new symptoms at a later stage, especially if:
- treatment is delayed
- symptoms develop slowly
- symptoms do not improve quickly
- symptoms are not related to stress
- symptoms include tremors or seizures
- there are accompanying psychological conditions