Signs
Symptoms of depersonalization (derealization) include:
- the feeling of existing separately from reality and the real world
- feeling of losing contact with reality
- state like in a dream
- feeling that you are not part of reality
- the feeling of looking at your body from the outside
- perception of surrounding objects as not real
- feeling separated from one's true thoughts and feelings
- the feeling of being in someone else's body
Symptoms of depersonalization may occur infrequently, frequently, or be almost constant. They can complement other symptoms of an anxiety disorder or exist in splendid isolation.
Symptoms of derealization can appear out of the blue, or they can be clearly associated with a stressful event. They can precede a given stressful event, manifest themselves simultaneously with it, or follow it.
Attention!
Since many extremely serious illnesses can cause symptoms similar to the depersonalization symptoms of anxiety, all people suffering from such conditions should be examined. And don’t rely on the fact that “it’s all nervous.”
The intensity of depersonalization can range from mild to severe. Symptoms always come in waves, changing from day to day and hour to hour.
Treatment
Treatment of the syndrome begins with diagnosis, which in some cases can be difficult due to the presence of concomitant mental pathologies and the manifestation of corresponding symptoms.
The clinical picture is compiled based on the patient’s own complaints, as well as information received from relatives and people close to the patient.
It is impossible to identify the syndrome using tests, tests and various instrumental examinations.
The nature of the treatment depends on what causes the perception disorder. If depersonalization-derealization syndrome arose due to severe emotional shock or stress, then psychotherapy is indicated for the person.
As an additional measure, the doctor may prescribe medication (antidepressants), physiotherapy, various massages and relaxation practices.
In the case of depersonalization-derealization syndrome, we can talk about good prognosis.
With correct treatment, the patient recovers completely, without associated complications.
The category of patients suffering from a protracted disorder and having a history of suicide attempts are treated in a hospital setting .
In this case, the doctor prescribes antipsychotics and tranquilizers, which stabilize the person’s condition and “return him to reality.” Next, the patient is indicated for psychotherapy.
If the disorder has developed against the background of a disease (brain damage, osteochondrosis, head injury, etc.), then during treatment the doctor focuses on combating the root cause.
Reasons for the development of depersonalization (derealization) at the time of anxiety?
The effects of stress hormones on the brain
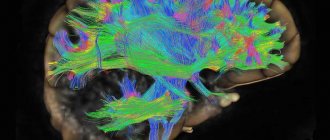
Stress hormones, which are necessarily secreted by the body into the blood at times of anxiety, stimulate an area in the brain called the amygdala. This area of the brain is responsible for the feeling of fear. At the same time, other centers of the brain, such as the area of rational perception or learning, are suppressed.
This leads to a deterioration in the ability to think clearly and retrieve information from short-term memory.
This reaction is completely normal. Since it is designed to save the body in a moment of danger. If a living organism is in danger, it does not have time to stand and think for a long time about what to do. He must either fight or run away.
Therefore, nature stimulates the amygdala at times of anxiety and suppresses areas of long-term rational thinking. However, in conditions where there is no real danger and nowhere to run, this natural defense mechanism can give a feeling of depersonalization.
When a person is in a state of anxiety for a long time, connections between areas of the brain that normally communicate very closely with each other weaken. The weakening of these connections leads to a separation of the processing of received information from its perception.
Hence those feelings of “separation,” “disconnection,” which all neurotics suffering from derealization talk about.
In this state, the brain takes a longer time to process information coming to it from the outside.
Hypo- and hyperventilation
In a state of stress, a person can begin to breathe either very shallowly and not deeply, or, conversely, very deeply. In the first case, there will be a lack of carbon dioxide in his blood, in the second - an excess.
But in both cases, changes in blood gas composition can negatively affect the brain, leading to the development of a feeling of depersonalization.
However, derealization caused by hypo- or hyperventilation is never long-lasting. It goes away as soon as breathing returns to normal. And often accompanied by a panic attack.
Medicines used to treat anxiety
For many neurotics, the feeling of depersonalization does not occur on its own, but only after taking medications that are usually prescribed for the treatment of anxiety disorders. These can be tranquilizers, antidepressants and antipsychotics. The latter cause depersonalization most quickly.
Depersonalization-derealization syndrome: causes
The cause of the development of depersonalization-derealization syndrome can be various factors:
- disorders of the brain and/or mental pathologies (schizophrenia, epilepsy, organic brain damage);
- use of drugs and alcohol with concomitant intoxication of the body;
- acute depressive states;
- history of emotional trauma;
- overwork, exhausting work, problems in the personal and social sphere.
A similar disorder can develop if a person has experienced a strong shock, after which the mental defense mechanism is triggered.
As a result, the individual seems to withdraw from the painful awareness of reality. The root cause may be episodes of physical or mental violence, the loss of a loved one, a sudden change in lifestyle, etc.
If derealization or depersonalization is temporary (against the background of severe shocks), the person is not diagnosed with the syndrome.
A short-term course always ends in recovery , even in the absence of specialist intervention.
Experts identify several forms of the disorder :
- Autopsychic . A person withdraws into himself, does not make contact and tries to protect himself from society. This is explained by the fact that the individual does not feel confident due to the fact that he cannot control what is happening. He begins to have “strange” and “unreal” thoughts. Feelings change, and emotions become distorted or disappear altogether. The patient may also complain of incomplete amnesia.
- Allopsychic .
We are talking specifically about derealization, in which the world seems fabulous, fantastic, cloudy, unreal, strange, etc. to the patient. The individual can observe people and events as if they were all present in some old film. Or in another reality, to which the patient does not have access. In this state, a person finds it difficult to distinguish faces, identify objects and even familiar places. - Somatopsychic . This type of syndrome manifests itself in the form of a violation of the perception of one’s body and its boundaries. The complaints in this case are very specific. For example, an individual may complain about missing eyes, limbs, clothing, hair, etc. His own body may seem to him to be fragmented into separate fragments.
How to get rid of symptoms of depersonalization (derealization)?
Complete relief from the symptoms described above is only possible when the anxiety has gone completely. Therefore, depersonalization cannot be treated separately. The anxiety disorder itself must be treated, not its symptom.
Moreover, unlike many other manifestations of chronic anxiety, derealization is a fairly stable condition. That is, even if you have eased your anxiety a little, but are still in a state of defense from the environment and your inner world, depersonalization will weaken, but will not go away completely.
The brain needs time to restore all its connections. And if, at the moment of restoring these connections, you are again overwhelmed by anxiety, then depersonalization will again manifest itself in all its glory.
Great article 0
Derealization and cervical osteochondrosis
In some diseases, a mental disorder such as derealization can also be observed, with cervical osteochondrosis, for example. This disease is characterized by damage to the intervertebral discs in the cervical spine. This often leads to pinched nerve endings and blood vessels, which, in turn, contributes to the appearance of derealization symptoms. Cervical osteochondrosis is provoked by: incorrect position of the head on the pillow, neck injuries, stooping or scoliosis, regular forced holding of the neck and head in uncomfortable positions (for example, at work). If derealization is associated specifically with cervical osteochondrosis, the patient is prescribed appropriate treatment. The patient's psyche is restored.
What is derealization?
Psychosensory disorders are a group of pathologies that are studied in the psychiatric section of perceptual disorders. Perception is a person’s ability to sense and summarize what has been experienced, processing all external influences and the ability to sense them. This mechanism gives the individual primary interaction with the world and allows him to perceive external factors based on experience and already acquired experiences. Psychosensory disorders are a large group of perceptual disorders that have many subtypes of disorders, they manifest themselves in many structures. This may be a violation of temporal, color, spatial, or self-perception. These species are very bright in their manifestations and, as a rule, very frightening, since the very familiar world structure is changing. Such states are very attractive for various types of fine art, since they give a feeling of a kind of “breaking of the world.” The danger of these disorders lies in separation from the world, in the fact that the individual is left alone with a frightening and unstructured world.
Such images are very well conveyed by the artist Dali, who changes the very course of space and time in his art. Since ancient times, humanity has been inclined to change its consciousness in order to think more sublimely and remove stereotyped perceptions. But in fact, an individual who has at least once experienced a feeling of derealization will not recommend this to anyone, since due to complete lack of perception and a break with the outside world, the individual remains completely alone and with his fear.
Derealization syndrome is not a separate pathology included in the classifications of psychiatric disorders. It is rather a symptom that is inherent in a fairly large number of pathologies and it manifests itself to varying degrees, always greatly disrupting the normal course of life of the individual suffering from it. This is just a peculiar component of the disorder. Derealization and depersonalization always go hand in hand, leaving the individual no chance for a real perception of the world.
The most striking manifestations of psychosensory disorders include: chromopsia, rubropsia, bathmopsia, metamorphopsia, micropsia, macropsia, megalopsia, poropsia, dysmorphopsia, tachychronia, bradychronia, xanthopsia. Deja vu and jamais vu are also common conditions that can be part of the same alienation syndrome.
Derealization is of Latin origin and means “de”, as a particle that negates “realis”, which means real. That is, derealization is the alienation of the material.
Derealization and depersonalization have always been widely studied, and Dugas was the first author to describe these symptoms. And it must be said that these concepts follow inextricably and many authors are inclined to combine these concepts due to the totality of symptoms and manifestations. Derealization often manifests itself as allopsychic depersonalization and is, as it were, a subtype of it. That is, one comes from the other. There the individual feels the alienation of his Self, and with derealization - the world from himself.
Derealization and depersonalization are studied from a large number of angles; psychiatrists of the existential direction have become especially interested in these conditions. Later, this pathology was considered in a sensualistic direction, where Griesinger and Krizgaber worked with it. Their research and philosophical notes were the first to identify some features of psychosensory disorders. Further, associational directions, emotional, psychoanalytic and phenomenological, worked in the same direction.