Meningitis belongs to the category of dangerous childhood infectious diseases. It is a serious disease of the central nervous system, in which inflammation of the meninges occurs. Symptoms of meningitis in children are a complex of cerebral, meningeal and general infectious conditions that require immediate treatment. The risks of complications are quite high, so it is very important to recognize the disease in time and carry out the necessary treatment.
Pediatricians believe that this disease has three features: it is rare, quite dangerous, and requires urgent hospitalization in the infectious diseases department. Based on this, every parent should know what kind of disease this is, what are its causes, symptoms and what treatment a doctor can prescribe.
What kind of disease is this
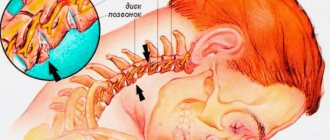
Meningitis is an acute inflammation of the membranes of the brain or spinal cord, with severe disruption of the central nervous system. Anyone can get sick, but children from birth to 7 years old, whose immune system is not able to cope with pathogenic microorganisms, are at risk. The disease develops after penetration of various pathogens into the tissue of the meninges - these can be viruses, bacteria, fungi. After infection, they produce endotoxins, which cause inflammatory processes, impair blood circulation, increase blood clotting, and in the absence of timely treatment, provoke brain edema.
Meningitis is divided into several types, has several classifications, and can lead to death within the first day.
The disease is quite dangerous, capable of causing infectious-toxic shock, disrupting the functioning of not only the brain, but also the activity of other internal organs and systems. The incubation period ranges from 3 to 10 days. Once the infection passes through the blood-brain barrier, it reaches the skull, leading to dysfunction of brain tissue, causing swelling and other problems. It is at this stage that the first symptoms appear and require immediate treatment.
Causes of development and risk factors
According to medical observations and statistics, in 60% of cases the cause is meningococcus, the source of which can be a person or an animal. Infection occurs by airborne droplets. In other cases, the causative agent may be various measles, influenza viruses, enteroviruses or bacteria, most often the same meningococcus, streptococcus, staphylococcus, pneumococcus, hemophilus influenzae and others.
The infection can penetrate into the brain structures in several ways:
- contact and household - through common objects;
- fecal-oral – with water or food;
- airborne - from a sick person or carrier;
- transmissible – from insect bites;
- hematogenous, lymphogenous - through the blood;
- intrauterine infection of the fetus from the mother.
Meningitis can develop primarily or secondary. In the first case, the disease develops independently; the entrance gates are often the mucous membranes of the nose, mouth or digestive tract. Secondary develops as a complication against the background of other viral or bacterial diseases. Those at risk for development, as well as the trigger for the development of infection, are:
- hypothermia of the body;
- decreased immunity;
- hypothermia of the body;
- frequent stressful situations;
- functional disorders in the central nervous system.
Outbreaks of meningitis more often occur in the winter-spring period, when the child’s immune system is reduced and the threshold for the incidence of acute viral infections increases.
Symptoms in adults
Best materials of the month
- Why you can't go on a diet on your own
- 21 tips on how to avoid buying stale food
- How to keep vegetables and fruits fresh: simple tricks
- How to curb your sweet cravings: 7 unexpected products
- Scientists say youth can be extended
Among adults, men aged 20-30 years are most susceptible to meningitis. The percentage of women among patients with meningitis is, as a rule, lower; only during the period of bearing a child is it easier for expectant mothers to become infected. In adults, the bacterial form of the disease caused by meningococci, pneumococci, and Haemophilus influenzae is most often diagnosed. Although in countries where vaccination against meningitis is mandatory, this figure is lower. Sometimes inflammation of the meninges appears as a complication of improper treatment of tuberculosis.
The incubation period of bacterial meningitis in adults sometimes lasts up to 12 days [2], then the temperature rises to 38 degrees and signs of nasopharyngitis appear. When the infection enters the bloodstream, the fever reaches 40 degrees and the classic symptoms of meningitis appear: headache, vomiting, neck muscle tension. Bacterial inflammation in adults is as severe as in children: up to 10% of cases of the disease result in either severe complications or death[3].
Viral meningitis always begins acutely, with severe intoxication and fever. Typically, typical meningeal symptoms appear on the second day. In most cases, it will take several weeks for an adult to recover from viral meningitis.
If the inflammatory process affects the cranial nerves, the patient may complain of blurred vision and double vision, he develops ptosis, strabismus, paresis of facial muscles, impaired auditory function, and confusion. In some cases, other nonspecific symptoms are possible: tachycardia, bradycardia, convulsions.
First signs of illness
Clinical signs of meningitis always appear quickly, the symptoms are acute and increasing. Sometimes they resemble a viral infection, but in this case the child’s condition worsens sharply, and standard pharmaceutical drugs to relieve headaches or reduce body temperature do not bring the desired result.
Meningitis in a child can be recognized by the following signs:
- increased body temperature from 38 to 40 degrees;
- blue discoloration of nasolabial folds;
- headache;
- screaming, continuous crying (in infants);
- vomit;
- pale skin;
- dyspnea;
- lack of appetite;
- skin rash (sometimes);
- photophobia.
All these symptoms may be the first signs of brain inflammation, which parents can observe for 2 days, then more pronounced and dangerous signs will join them.
If the cause is a bacterial infection, then the clinical picture is acute and pronounced already in the first hours of the illness.
Pathology can be recognized by general signs, which are caused by the rigidity of muscle tissue. Here we are talking about a forced position that the child takes: lying on the bed, throwing his head back. This symptom indicates increased intracranial pressure.
If the cause of the disease is meningococcal infection, in addition to all the general symptoms, there will be a skin rash all over the body, including the abdomen, upper and lower extremities, back, and buttocks.
Pediatricians believe that the younger and weaker the child, the more difficult it is for him to endure the disease. Children under 5 years of age have a high risk of developing coma or death, so at the first signs of illness there is no need to hesitate to call an ambulance.
We diagnose at home
The main task of parents is to promptly recognize the appearance of meningitis in a child 1-2 years old by signs and symptoms and seek qualified help from a medical institution.
We recommend using the step-by-step steps below.
Take the baby's temperature: with meningitis it is high and is accompanied by the child's lethargy and weakness.
- Pay attention to the baby’s consciousness: when inflammation of the meninges develops, it is confused, and he does not make contact with an adult.
- See if there is any strange position of the baby's body. Meningitis is characterized by a peculiar position when he lies on his side for a long time, bending his knees and pressing them to his body, while his head is thrown back.
- If convulsions occur , they may indicate a serious condition.
Important! Don't wait for your child to get worse. At the slightest suspicion of the development of meningitis, consult a specialist immediately!
Differences from ARVI
Serous and meningococcal forms at an early stage often resemble colds. They are accompanied by elevated body temperature and the appearance of weakness, as with ARVI.
However, parents should be wary if the disease develops rapidly. The baby is capricious and refuses to eat. Loud noises and bright lights irritate him.
When a child has a cold, he takes a characteristic position : on his side in a lying position, he brings his legs to his stomach and throws his head back. Any change in posture is accompanied by the appearance of wild pain.
To confirm the diagnosis, the doctor performs tests to confirm inflammation of the meninges. The most common test for neck stiffness is that the doctor places one hand on the upper chest and the other on the back of the baby's head. Then the specialist presses on the back of the head, bending the neck, and the chin reaches the palm that lies on the chest. If a baby develops meningitis, such a test cannot be performed.
Types of meningitis
Meningitis is usually understood as a complex of symptoms and disorders occurring in parts of the brain or spinal cord. The disease is divided into several types and can develop primarily or secondary. In the first case, it manifests itself independently against the background of infection penetration into the brain structures. The secondary form develops as a complication after an infectious disease: measles, influenza, sinusitis, pneumonia and other diseases.
In making a diagnosis, it is important to identify the pathogen, which will allow the doctor to determine the form of the disease and carry out the necessary treatment.
Bacterial meningitis
Inflammation of the brain develops against the background of infection. The causative agent is often meningococcus, staphylococcus, streptococcus. The disease has a rapid course, rapidly increasing symptoms:
- increase in body temperature to high levels, which is poorly controlled by antipyretic drugs;
- vomiting that does not bring relief;
- headache due to increased intracranial pressure;
- tension in the neck muscles, which leads to a forced posture;
- small skin rash, which is characteristic only of meningococcal infection;
- redness of the back of the throat;
- signs of ARVI: runny nose, sore throat, nasal congestion, cough;
- rapid pulse;
- muscle cramps in severe disease.
If the cause of the disease is meningococcal infection, the symptoms are most pronounced, the condition worsens sharply, and the small patient requires immediate hospitalization.
Specific symptoms of the disease include:
- skin necrosis with the development of vascular thrombosis;
- strabismus due to damage to the cranial nerves;
- conjunctivitis (inflammation of the lining of the eyes);
- panophthalmitis (sharp decrease in vision).
A feature of bacterial meningitis is considered to be increased excitability, which is manifested by strong screaming and crying with any soothing movements. Infants have a bulging fontanelle, and adolescents complain of unbearable headaches that worsen with bright lighting or loud noises.
Viral meningitis
The viral form is less common than the bacterial one and has increasing symptoms, which at first resemble a banal ARVI. A few days later it is noted:
- a sharp increase in body temperature;
- general weakness;
- nausea, vomiting;
- inflammation of the mucous membrane of the throat;
- conjunctivitis;
- muscle weakness.
In the absence of proper treatment, the risk of encephalitis with convulsive syndrome, severe neurological disorders, loss of consciousness and other dangerous signs increases. Unlike bacterial, this form of brain inflammation has less dangerous symptoms and is highly treatable in the early stages.
Purulent meningitis
The severe form includes the purulent form, which develops against the background of a secondary infection as a complication. Symptoms appear acutely and are accompanied by:
- high body temperature;
- chills;
- repeated vomiting without relief;
- Kernig's sign (the child's inability to bend or straighten the leg at the knee);
- tachycardia, bradycardia;
- hemorrhagic rash.
The purulent form of meningitis is divided into three main forms:
- lightning;
- acute;
- chronic.
If we talk about the first form of the disease, it develops only in newborns. Any type of purulent inflammation of the brain is quite dangerous for the health and life of a child and can lead to irreparable consequences, disability or death.
Serous meningitis
Develops as a result of serous inflammation of the soft membrane of the brain with subsequent accumulation of serous exudate. The course of the disease is much simpler than with purulent meningitis. It can be of infectious or non-infectious origin; more often the cause of its development is viruses or brain tumors. Serous meningitis affects children from 2 to 6 years old, less often - adolescents and adults.
The first signs of the disease are cold symptoms, then they are joined by elevated body temperature, nausea, vomiting and other typical symptoms. The child is constantly lethargic, sleepy, and refuses to eat.
Clinical manifestations
Regardless of the nature of its occurrence, the clinical picture of meningitis has a set of common symptoms:
- General infectious symptoms - the most serious symptom is the occurrence of intoxication, which leads to the development of various disorders in the body (for example, hormonal disorders, water-salt disorders, etc.).
- Meningeal syndrome - this process is caused by the occurrence of inflammatory processes in the meninges. Conventionally, it is divided into general cerebral symptoms (photophobia, dizziness, headache) and meningeal symptoms (Kernig's, Brudzinski's symptoms, etc.).
- Changes in the cerebrospinal fluid (for example, with purulent meningitis, turbidity of the cerebrospinal fluid is observed, the amount of protein increases, etc.).
Features of symptoms by age
Clinical signs of meningitis in children depend not only on the causative agent of the infection and the stage at which the disease is located, but also on age. The younger the child, the more severely he suffers it; it requires immediate hospitalization, since there is a high probability of complications, even death.
Signs of meningitis in infants
In children from birth to 2 years of age, symptoms of meningitis appear acutely, a couple of days after contact with the pathogen. The difficulty of primary diagnosis lies in the fact that the baby is not able to explain or show the localization of the pain syndrome. Therefore, it is extremely important for parents to monitor the child’s condition and consult a doctor if there is the slightest change in his behavior. Meningitis in infants is manifested by the following symptoms:
- constant monotonous crying;
- breast and bottle refusal;
- frequent regurgitation;
- characteristic pose (the child lies on his side, head thrown back, legs bent at the knees;
- convulsions;
- protrusion of soft tissue between the bones of the skull;
- diarrhea;
- vomit;
- chills;
- heat;
- rashes on the skin or mucous membranes;
- loss of consciousness.
Signs of the disease in children from 3 to 8 years old
Inflammation of the brain in children of primary preschool age is characterized by severe symptoms, and their state of health sharply worsens:
- Strong headache;
- lack of appetite;
- lethargy;
- high body temperature;
- vomiting that does not bring relief;
- throwing the head back;
- arching of the back;
- blue lips;
- rapid pulse;
- diarrhea;
- whitish spots on the skin.
Symptoms in teenagers
Older children can talk about their symptoms, which will allow the doctor to make an initial diagnosis before receiving test results.
The characteristic features are:
- headache;
- repeated vomiting without nausea;
- increased sensitivity to light;
- mental disorders: hallucinations;
- increased irritability;
- loss of consciousness.
At an older age, the symptoms may be more pronounced, but if not properly treated, the child may fall into a coma and there is a high risk of death.
How to recognize at home?
There are several of the most striking childhood symptoms of meningitis, the appearance of which directly signals a developing disease. As mentioned above, these symptoms are called meningeal. Thus, knowing the meningeal symptoms, you can check for meningitis in your child at home . So, let's look at them in detail.
Kernig's symptom - is expressed in the fact that the patient, lying on his back with his leg bent at the knee and also at the hip joint, cannot straighten it due to the fact that the muscles of the back of the thigh are in severe spasm. At the same time, trying to bend one leg, the second also begins to reflexively bend.
Brudzinski's symptoms contain a set of signs indicating damage to the membranes of the brain.
So, there are the following 4 symptoms that can be used to identify meningitis in a child, even at home:
The upper Brudzinski symptom is expressed in the fact that when trying to bring the patient’s chin closer to the chest, there is strong resistance from the neck muscles, as well as flexion of both legs at the knee and hip joint.
- The average Brudzinski symptom is when light pressure is applied to the patient’s pubic bone, and the leg is pulled toward the abdomen. This is a positive sign.
- The lower Brudzinski symptom is a kind of Kering symptom. If, when trying to bend the patient’s leg at a right angle at the knee and hip joints, the second leg involuntarily begins to be pulled towards the stomach, then, accordingly, the lower sign can be considered positive.
- Brudzinski's buccal symptom - if, when pressing on a point located just below the zygomatic arch, the patient bends the arm at the elbow joint and raises the wrist, then accordingly this sign can be considered positive.
Brudzinski's symptoms in children at an early age are usually very mild.
Ankylosing spondylitis's symptom is called the zygomatic symptom , and is expressed in the fact that when lightly tapping the cheekbones with a hammer, the patient experiences a severe headache, and a painful grimace appears on the face. This indicates pathological processes occurring in the brain.
Expert opinion
Zemlyanukhina Tatyana Vyacheslavovna
Ambulance and emergency paramedic at the Clinical Emergency Hospital #7 in Volgograd.
Ask an expert
Meningitis has its own set of symptoms by which you can determine the presence of the disease at home. But most often, especially in children, the disease begins asymptomatically or is accompanied by such nonspecific manifestations as irritability or drowsiness.
Complications and consequences
Meningitis in children is an extremely serious disease, as it has a high risk of complications, especially in cases where treatment is not carried out on time. Common consequences include:
- damage to cranial nerves and brain centers;
- cerebral edema;
- pulmonary edema;
- acute adrenal insufficiency;
- panophthalmitis;
- hearing and vision impairment;
- epilepsy;
- vestibular disorders;
- mental changes;
- paresis and paralysis;
- impaired mental function;
- coma.
In severe cases, irreversible changes occur in the structures of the brain, which can lead to the death of the child in the first days after the first signs of the disease appear.
Causes of the disease
The main cause of meningitis in adults is infection in the membranes of the brain, the causative agents of which can be:
- Viruses – herpetic, mumps.
- Bacteria – staphylococci, meningococci, streptococci, Escherichia coli and tuberculosis.
- Fungal infections - mycoses, candida.
The factors under which pathogens are activated are:
- immunity weakened by chronic diseases or long-term use of chemicals;
- chronic fatigue;
- poor diet;
- metabolic disorders, diabetes mellitus;
- gastrointestinal diseases;
- presence of HIV infection;
- insect bites (such as ticks or mosquitoes);
Also, meningitis in adults can manifest itself as a complication after sinusitis, pneumonia, purulent otitis media or head injury.
Diagnostics
Meningitis can be recognized by external signs, but to obtain a complete clinical picture and determine the causative agent, the doctor prescribes a series of laboratory and instrumental examinations:
- general blood analysis;
- Analysis of urine;
- serological blood test.
- swab from the throat and nose for bacterial culture;
- X-ray of the skull;
- MRI or CT;
- Lumbar puncture.
The results of the study will help the doctor determine the type of pathogen, form, and severity of the disease. Based on the diagnosis, the doctor will draw up a treatment plan.
Treatment of meningitis in children
The nature of treatment directly depends on the type of meningitis, the age of the patient, and the characteristics of the body. Therapy is carried out in a hospital setting under the supervision of a doctor and medical staff.
If the cause of the disease is a viral infection, antibiotic treatment is contraindicated, as they may do more harm than good. Viral meningitis is treated with dehydration therapy, diuretics are prescribed to reduce intracranial pressure, as well as anticonvulsants and antiallergic drugs. To relieve pain and inflammation, antipyretics and analgesics are prescribed.
With the bacterial form, which occurs in 80% of cases, antibiotics, to which the bacteria that caused the disease are sensitive, are important in treatment. In addition to antimicrobial therapy, other medications are prescribed to relieve symptoms and exclude pathological changes in brain structures.
All prescribed drugs are administered to children intravenously or intramuscularly. The choice of any medicine, dose and duration of use is determined by the doctor individually. On average, treatment for meningitis is 2-3 weeks .
General recommendations for the treatment of meningitis in children
To speed up recovery after therapy, parents should adhere to some rules for caring for their child:
- Create a healthy psychological environment. The child should not be nervous or cry.
- A gentle diet should include eating only high-quality and healthy food without adding any chemical compounds.
- Taking vitamin complexes will help boost immunity and provide the body with necessary nutrients.
- Regular cleaning and ventilation of the room where the child sleeps.
- Walks in the open air.
- Compliance with all medical recommendations.
Only an integrated approach to treatment will help minimize complications and speed up recovery. In severe cases, disruption or damage to brain structures, long-term rehabilitation under the supervision of specialists will be required.