|
Types of encephalitis
There are primary and secondary encephalitis. If we are talking about the primary form of the disease, the virus affects the spinal cord and brain. The secondary form of encephalitis is called post-infectious. It occurs when other organs are infected by a virus. The infection reaches the brain through the bloodstream.
The disease leads to inflammation of nerve cells or meninges. In the latter case, they talk about viral meningitis, which has a number of significant differences from encephalitis. However, both infections are insidious in that they often accompany one another. This sometimes makes it difficult to make an accurate diagnosis.
The vast majority of clinical cases of encephalitis end in death, but if the patient is given emergency and proper treatment, recovery is quite possible.
Causes of encephalitis
Here are the most common causes of encephalitis:
- bite of arthropod insects, in particular ticks;
- entry into the blood and then into the brain of bacteria (staphylococci, streptococci, malarial plasmodium, toxoplasma, treponema pallidum, borrelia, rickettsia, etc.), viruses (herpes, in particular with chickenpox, coxsackie and ECHO, rabies, influenza, measles , rubella, cytomegalovirus, etc.) and parasites (toxoplasma, etc.);
- allergic reactions, primarily an allergic reaction to a vaccine (most often DTP, smallpox and rabies vaccines);
- intoxication;
- female tumors, in particular ovarian teratoma.
Symptoms of the disease
In many patients, the disease is indolent or asymptomatic. Flu-like symptoms may also occur:
- feverish condition;
- heat;
- pain in joints and muscles;
- headache;
- constant weakness;
- lack of appetite.
The doctor should be concerned about:
- disturbances of the nervous system in the form of confusion;
- strong psychomotor agitation;
- hallucinatory syndrome;
- presence of cramps or muscle tension;
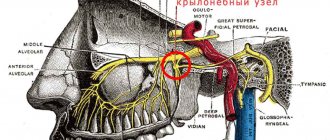
- disturbances in the sensitivity of certain parts of the body or face;
- diplopia (when the patient sees double);
- speech or hearing disorders.
Clinical manifestations of encephalitis in children in the first months and years of life may differ:
- the fontanel in babies protrudes;
- nausea and vomiting appear;
- children cry constantly;
- the child refuses to breastfeed.
It should be borne in mind that more than 90% of patients with encephalitis have symptoms similar to influenza. In the presence of both meningitis and encephalitis at the same time, a person experiences:
- Strong headache;
- fear of light;
- vomit;
- stiffness of the neck muscles.
If we are talking about a severe form of encephalitis, it may be accompanied by serious changes in behavior, ranging from mild confusion to a coma. In especially severe cases, spatial disorientation, delirium and other perception disturbances occur. Home treatment in such cases is contraindicated, since, being in such a state, the patient can cause harm to both himself and the people around him. The main thing is to hospitalize the patient faster and prevent fatal consequences for the brain.
There are several other symptoms typical of encephalitis. They are associated with which part of the brain was affected by the virus attack. Patients may use words incorrectly or not understand their meanings at all. Patients experience involuntary body movements and tremors of the limbs. Sometimes paralysis occurs on one side of the body.
Tick-borne encephalitis (IgM antibodies)
What is tick-borne encephalitis?
This is a naturally focal transmissible (transmitted by ticks) viral infection, characterized by predominant damage to the central nervous system. The disease is characterized by polymorphism of clinical manifestations and severity of the course (from mild erased forms to severe progressive ones). The first clinical description of the disease was given in 1936-1940. Currently, tick-borne encephalitis is registered in Siberia, the Far East, the Urals, Belarus, as well as in the central regions of the country.
The main reservoir and carrier of the virus in nature are ixodid ticks - Ixodes persulcatus, Ixodes ricinus with transovarial transmission. Additional reservoirs of the virus are rodents (hare, hedgehog, chipmunk, field mouse), birds (thrush, goldfinch, redpoll, finch), and predators (wolf). The disease is characterized by a strict spring-summer seasonality of the disease. The dynamics of incidence is closely related to the species composition of ticks and their greatest activity.
People aged 20-40 years are most often affected. The main route of human infection is vector-borne transmission through tick bites. It is also possible to transmit the infection through the nutritional route when eating raw milk from goats and cows, as well as when crushing a tick at the time of its removal from the human body and, finally, through airborne droplets when working conditions in laboratories are violated. In case of alimentary infection, attention is drawn to the presence of family-group cases of the disease.
The following clinical forms of the disease are distinguished:
- febrile;
- meningeal;
- meningoencephalitis;
- polio;
- polyradiculoneuritis.
In meningeal, meningoencephalitic, poliomyelitis, polyradiculoneuritic forms of tick-borne encephalitis and in cases with a two-wave course of the disease, hyperkinetic and epileptiform syndromes can be observed.
The incubation period of tick-borne encephalitis lasts on average 7-14 days with fluctuations from one day to 30 days. In a number of patients, the onset of the disease is preceded by a prodromal period, lasting 1-2 days and manifested by weakness, malaise, and weakness; Sometimes there is mild pain in the muscles of the neck and shoulder girdle, pain in the lumbar region in the form of aches and numbness, and headache. The temperature quickly (in 1 - 2 days) reaches 39 - 40°C.
Feverish form.
It is characterized by a favorable course without visible damage to the nervous system and rapid recovery. This form accounts for approximately 1/3 of the total number of tick-borne encephalitis diseases. The febrile period lasts on average 3-5 days. Sometimes there is a two-wave fever. The onset is acute, without a prodromal period. Sudden rise in temperature to 38-39°C, weakness, headache, nausea. In rare cases, meningism may occur with this form of the disease. More often, there are no symptoms characterizing local damage to the brain and spinal cord. No changes were detected in the cerebrospinal fluid.
Meningeal form.
Is the most common. The initial manifestations are almost the same as in the febrile form, but with more pronounced signs of general infectious intoxication. Rigidity of the neck muscles, Kernig's and Brudzinski's symptoms are determined. Meningeal syndrome is pronounced, the cerebrospinal fluid is transparent, sometimes slightly opalescent, its pressure is increased (200-350 mm water column). Laboratory examination of cerebrospinal fluid reveals moderate lymphocytic pleocytosis (100-600 cells per 1 μl, rarely more). In the first days of the disease, neutrophils sometimes predominate, which often completely disappear by the end of the first week of the disease. The increase in protein is observed inconsistently and usually does not exceed 1-2 g/l. Changes in the cerebrospinal fluid last a relatively long time (from 2-3 weeks to several months) and are not always accompanied by meningeal symptoms. The duration of fever is 7-14 days. Sometimes a two-wave course of this form of tick-borne encephalitis is observed. The outcome is always favorable.
Meningoencephalitic form.
It is observed less frequently than meningeal - the national average is 15% (in the Far East up to 20-40%). It has a more severe course. Delusions, hallucinations, psychomotor agitation with loss of orientation in place and time are observed. Epileptic seizures may develop. There are diffuse and focal meningoencephalitis. With diffuse meningoencephalitis, general cerebral disorders are expressed (profound disorders of consciousness, epileptic seizures up to status epilepticus) and scattered foci of organic brain damage in the form of pseudobulbar disorders (breathing disorders in the form of brady- or tachycardia, according to the Cheyne-Stokes, Kussmaul type, etc.), cardiac -vascular system, uneven deep reflexes, asymmetric pathological reflexes, central paresis of facial muscles and tongue muscles. With focal meningoencephalitis, capsular hemiparesis, paresis after Jacksonian seizures, central monoparesis, myoclonus, epileptic seizures, and, less commonly, subcortical and cerebellar syndromes quickly develop. In rare cases (as a consequence of a violation of the autonomic centers), gastric bleeding syndrome with hematemesis may develop. Characteristic are focal lesions of cranial nerves III, IV, V, VI pairs, somewhat more often VII, IX, X, XI and XII pairs. Later, Kozhevnikov epilepsy may develop, when general epileptic seizures with loss of consciousness appear against the background of constant hyperkinesis.
Poliomyelitis form.
It is observed in almost 1/3 of patients. It is characterized by a prodromal period (1-2 days), during which general weakness and increased fatigue are noted. Then periodically occurring muscle twitching of a fibrillar or fascicular nature is detected, reflecting irritation of the cells of the anterior horns of the medulla oblongata and spinal cord. Suddenly, weakness may develop in any limb or a feeling of numbness may appear in it (in the future, severe motor disturbances often develop in these limbs). Subsequently, against the background of febrile fever (1-4 days of the first febrile wave or 1-3 days of the second febrile wave) and general cerebral symptoms, flaccid paresis of the cervicobrachial (cervicothoracic) localization develops, which can increase over several days , and sometimes up to 2 weeks. Symptoms of “head hanging down on the chest”, “proud posture”, “bent, stooped posture”, techniques of “torso throwing the arms and throwing back the head” are observed. Poliomyelitis disorders can be combined with conduction disorders, usually pyramidal: flaccid paresis of the arms and spastic paresis of the legs, combinations of amyotrophy and hyperflexion within one paretic limb. In the first days of the disease, patients with this form of tick-borne encephalitis often experience severe pain. The most typical localization of pain is in the neck muscles, especially along the back surface, in the area of the shoulders and arms. The increase in motor disorders continues for up to 7-12 days. At the end of the 2-3rd week of the disease, atrophy of the affected muscles develops.
Polyradiculoneuritic form.
Characterized by damage to peripheral nerves and roots. Patients experience pain along the nerve trunks, paresthesia (feeling of “crawling goosebumps”, tingling). The symptoms of Lasseg and Wasserman are determined. Sensitivity disorders appear in the distal parts of the extremities of the polyneural type. Like other neuroinfections, tick-borne encephalitis can occur as Landry's ascending spinal palsy. Flaccid paralysis in these cases begins from the legs and spreads to the muscles of the torso and arms. The ascent can also begin from the muscles of the shoulder girdle, involving the cervical muscles and the caudal group of nuclei of the medulla oblongata.
Complications and damage to the nervous system.
With all the above-described clinical forms of tick-borne encephalitis, epileptiform, hyperkinetic syndromes and some other signs of damage to the nervous system can be observed. This depends on the epidemic focus (western, eastern), on the method of infection (vector-borne, nutritional), on the condition of the person at the time of infection and on the methods of therapy.
Hyperkinetic syndrome is registered relatively often (in 1/4 of patients), and mainly in persons under 16 years of age. The syndrome is characterized by the appearance of spontaneous rhythmic contractions (myoclonus) in individual muscle groups of paretic limbs already in the acute period of the disease.
Progressive forms.
From the moment of infection and subsequently, even after the acute period, the tick-borne encephalitis virus can persist in the central nervous system in an active form. In these cases, the infectious process does not end, but enters the phase of chronic (progressive) infection. Chronic infection with tick-borne encephalitis can occur in a latent form and manifest itself after several months and years under the influence of provoking factors (physical and mental trauma, early spa and physiotherapeutic treatment, abortion, etc.). The following types of progressive course are possible: primary and secondary progressive, and subacute course.
Forecast.
Favorable for meningeal and febrile forms. With meningoencephalitis, poliomyelitis and polyradiculoneuritis it is significantly worse. Lethal outcomes up to 25-30%. In convalescents, pronounced organic changes in the central nervous system (convulsive syndromes, muscle atrophy, signs of dementia, etc.) persist for a long time (up to 1-2 years, and sometimes for life).
Specific IgG antibodies
to the tick-borne encephalitis virus can be detected on days 10-14 and even earlier. After a month they reach a high level and persist for 2 to 6 months after infection. After 2-3 years, antibodies are rarely detected. Specific IgG antibodies are detected after vaccination against tick-borne encephalitis. A certain percentage of the general population of healthy people may have circulating IgG antibodies to tick-borne encephalitis virus due to no significant clinical exposure to the virus in the past. The number of such individuals is higher in endemic areas.
In combination with IgM
antibodies, identifying the fact of IgG seroconversion (the appearance of specific antibodies in the dynamics of the disease in their initial absence) speaks in favor of confirming the clinical diagnosis of viral tick-borne encephalitis.
Who can get infected?
Particular risk groups include newborns and the elderly. Those who are in areas where mosquitoes or ticks live can also become infected. Weak immunity is also one of the possible causes of infection, as well as long-term use of antibacterial or chemotherapy drugs.
There is such a thing as “countries endemic for encephalitis.” Infectious disease specialists and epidemiologists use this formulation when dealing with people who have returned from tropical countries with a high risk of morbidity. And of course, we cannot help but remember the “anti-vaxxers” who are at particular risk because they refuse to vaccinate their children against measles, mumps, rubella and other “childhood” infectious diseases.
Prevention of encephalitis
• timely vaccination (against measles, tick-borne encephalitis);
• strict adherence to the vaccination schedule in children to avoid complications;
Watch a video on the topic of vaccination:
• taking precautions before and during tourist trips to countries where infection with viral encephalitis from insect bites is possible.
Let us remind you that we previously wrote how to recognize heat stroke: causes, symptoms, first aid.
Watch a video about the most dangerous types of ticks in the world:
Types of viral encephalitis
Viruses transmitted by insects are called arboviruses. They are the ones that are encountered most often in medical practice. Arboviruses transmitted by mosquitoes include:
- Eastern equine encephalitis. The disease is rare and affects no more than a few people around the world each year. 50% of those infected die because the brain damage is irreversible;
- La Crosse encephalitis. Typical of children and adolescents under 16 years of age living in the western United States. Deaths are rare;
- encephalitis St. Louis. Named after the American state of the same name, it is found in the south and west of the United States among people living in rural areas. Characterized by serious symptoms, especially in people over 60 years of age;
- West Nile encephalitis. It affects residents of Africa and the Middle Eastern regions. It is sometimes found in the USA. The disease is especially dangerous for children and the elderly, and the mortality rate is very high;
- equine western encephalitis. The infection is typical for the USA and Canada. The disease occurs under the guise of a regular flu or acute respiratory viral infection, but if it is not recognized in time, brain damage can become irreversible.
There are several other forms of viruses that cause encephalitis. These are viruses of measles, urogenital and common herpes, chickenpox, mononucleosis, measles, etc.
Autoimmune encephalitis of Rasmussen, Myers
Inflammation of the brain, which is characteristic of encephalitis, is considered almost a death sentence for many people. In fact, with proper treatment and timely diagnosis, the problem can be overcome.
The pathology has many causes, for example, due to bacteria or a virus, but the most dangerous type of disease is considered to be autoimmune encephalitis.
To date, no effective treatment has been invented for it, and the most common representative of this type of disease is Rasmussen's syndrome.
Rasmussen's encephalitis is an autoimmune disease of the brain in which one or both hemispheres become inflamed. Mostly teenagers under 14-16 years old suffer from this pathology.
It differs from other types of encephalitis in the persistence of epileptic seizures. It is quite difficult for sick people to get rid of seizures even with drug treatment.
The second feature of the pathology is atrophy of the tissues of one of the cerebral hemispheres, due to which it is less supplied with blood and decreases in size.
Features of the development and onset of the disease
Rasmussen's disease is still a mystery to scientists. Speaking about this syndrome, many experts cling to hypotheses and build them on the basis of available data. The most common causes of autoimmune failure leading to encephalitis are the following:
- Autoimmune antibodies;
- Viral infection;
- Cytotoxic T lymphocytes.
Autoimmune (autoaggressive) antibodies are formed spontaneously or as a consequence of infection, for example, due to bacteria from the genus Mycoplasma. They are a special structure consisting of protein. In the body, autoimmune antibodies cause damage or completely destroy healthy cells in certain organs or systems.
Cytotoxic T lymphocytes are cells responsible for the immune response. They are a major part of antiviral immunity. The target of T-lymphocytes is body cells damaged by viruses or bacteria, which is why they have the second name T-killer cells.
Against the background of a viral infection, various disruptions in the immune system often occur. Basically, it is because of it that autoimmune antibodies are synthesized and the targets of T-lymphocytes are lost.
According to most experts, the autoimmune type of encephalitis occurs due to exposure to cytotoxic T lymphocytes. This hypothesis has been tested more than once through numerous studies. The program involved many people suffering from Rasmussen's disease and a large concentration of these cells was found in their blood at the time of an epileptic attack.
A similar situation arose with autoimmune antibodies. Babies suffering from this disease had a lumbar puncture to remove some cerebrospinal fluid for analysis. In it, as in the plasma, auto-aggressive antibodies were found, but experts were unable to explain their role in the development of the pathology.
Drying of one of the hemispheres due to Rasmussen's encephalitis is an irreversible consequence.
This atrophy of brain tissue has its own reasons, for example, increased apoptosis with a progressive decrease in the number of neurons.
This phenomenon is completely natural, and it is responsible for the process of death of old cells in the nervous system. Apaptosis cannot be controlled, but does not cause neurodeficiency in healthy people.
If a person has Rasmussen's encephalitis, then a symptom such as apoptosis of astrocytes is observed.
Astrocytes are one of the components of white and gray matter located in the brain. They serve to nourish, protect and support the functions of nerve cells. If there are fewer astrocytes, this is considered a pathological change.
Based on the available information, it is known for certain that apoptosis of astrocytes against the background of an increase in the number of T-lymphocytes is a symptom of Rasmussen’s disease.
Most often this phenomenon is provoked by viruses or bacteria, but in some cases everything happens spontaneously.
The number of astrocytes is rapidly decreasing precisely because of T-lymphocytes, which perceive these cells as a threat due to a malfunction in the immune system.
Symptoms of pathology
Rasmussen's encephalitis manifests itself in the form of various pathological disorders, but the main symptom of the disease is epileptic seizures. After them, the patient most often loses consciousness. You can find out about the presence of the disease by other symptoms:
- When the disease worsens, involuntary muscle movements (hyperkinesis) occur in various parts of the body;
- Patients have unilateral weakening of the sensitivity of the upper and lower limbs (hemiparesis) or paralysis (hemiplegia);
- Due to damage to brain tissue, a person develops dementia, memory deteriorates and even basic things are forgotten, and the patient’s speech becomes incoherent. A decrease in the activity of the hemisphere affected by the disease can be seen on the EEG (electroencephalography).
In recent years, doctors have been able to identify several more signs of an autoimmune type of encephalitis. Patients have tongue spasms, as in epilepsy, and the disease can affect both hemispheres of the brain without symptoms of hemiparesis and hemiplegia.
Experts have identified 3 stages of development for Rasmussen syndrome, and each of them has its own symptoms and treatment regimen. They look like this:
- Prodromal stage. It lasts approximately 6-8 months and is mainly diagnosed in children under 7-8 years of age. In sick people at this stage of the disease, epilepsy appears quite rarely, and weakening of the muscle tissue of the arms and legs is absent or mild. In 60% of patients, this stage progresses to the next stage. For the remaining 40%, the disease begins immediately with an acute course;
- Acute stage. In people at this stage of the disease, epileptic seizures are common, and hemiparesis gradually progresses. Those affected show signs of dementia, forget the simplest things, and their speech becomes incoherent and unintelligible. This stage of development of the disease lasts about 7 months and in 95% of cases passes to the final stage. In the cooled down 5%, people continue to remain at this stage;
- Residual stage. It is also called residual and occurs mainly after treatment. The frequency of epilepsy attacks decreases, and their duration is also reduced.
The state at which people progress to stage 3 depends on the effectiveness of treatment. Often patients are left partially paralyzed with pronounced mental retardation. The stages of pathology development are determined mainly by the number of epileptic seizures and hemiparesis.
During an exacerbation, the disease manifests itself in the form of special symptoms. They help doctors determine the extent of brain damage.
The following signs of exacerbation should be noted:
- Epilepsy becomes characterized by polymorphism, that is, it will affect different muscle groups, disrupting their motor functions;
- The number of epileptic seizures increases significantly;
- The drugs actually stop working on epilepsy.
The phenomenon of epilepsy polymorphism in Rasmussen syndrome is common. This problem arises due to severe atrophy of the hemisphere and this process has been proven during research. Scientists even drew a parallel between this process and unilateral seizures from the damaged part of the brain.
The symptoms of autoimmune encephalitis in children and adults are the same, but they differ in the speed of manifestation. In children, the disease develops faster and symptoms are visible almost immediately. In an adult, Rasmussen's syndrome is not as pronounced and develops much more slowly. Experts attribute this phenomenon to a more developed compensatory mechanism in adulthood.
All symptoms of the disease develop smoothly, for example, at first muscle motor skills deteriorate, and only after 1-2 years the patient’s speech impairment becomes noticeable. At the same time, epilepsy attacks gradually become more frequent. That is why it is important to diagnose the disease at an early stage, so as not to wait for the full picture, as some consequences will be irreversible.
Course of therapy
This autoimmune type of encephalitis at an advanced stage is almost impossible to treat, and against its background, epilepsy attacks are virtually untreatable with drugs. They are eliminated through surgery. During the operation, the doctor will remove areas of the brain that have undergone atrophic changes.
In the early stages of development, the patient can avoid this fate by taking anti-epilepsy medications and also following a strict diet. The diet of a person suffering from Rasmussen's syndrome should include foods rich in fats and low in proteins and carbohydrates.
In recent years, new treatment methods have been introduced into the treatment of autoimmune types of encephalitis, for example, transcranial magnetic stimulation. It serves to prevent epilepsy attacks. In addition to this procedure, doctors usually prescribe blood filtration (plasmapheresis), hormonal drugs and immunomodulators.
Rasmussen's encephalitis is a typical representative of the autoimmune group of encephalitis. If not treated promptly, the disease will lead to paralysis and mental retardation. A course of therapy must be carried out in the early stages, otherwise the situation will have to be corrected by removing the damaged areas of the brain.
Source: https://NashiNervy.ru/infektsionnye-zabolevaniya/protekanie-autoimmunnogo-entsefalita.html
Diagnostic methods
In diagnosis, collecting a patient’s medical history plays an important role: for example, a person says that shortly before the illness he was bitten by a tick or mosquito. In order to clarify the diagnosis, people have their blood taken for analysis, a lumbar puncture is performed, and a CT or MRI scan is also performed. One accurate way to determine abnormalities in brain function is electroencephalography, which can show areas of abnormal activity.
Symptoms of the disease Encephalitis
Symptoms of encephalitis vary depending on the pathogen, the location of the pathological process, and the course of the disease. However, there are common clinical symptoms characteristic of encephalitis.
The prodromal period is characteristic of all infectious diseases. It lasts from several hours to several days and is manifested by increased temperature (fever), symptoms of irritation of the upper respiratory tract or gastrointestinal tract.
General cerebral symptoms are characteristic: headache, usually in the forehead and orbits, vomiting, photophobia, epileptic seizures. Impaired consciousness from mild degrees (lethargy, drowsiness) to coma. Psychomotor agitation and psychosensory disorders are possible.
Focal symptoms of central nervous system damage develop. They depend on the localization of the pathological process and the form of encephalitis; they can manifest themselves as symptoms of prolapse (paresis of the limbs, aphasia) and irritation (epileptic seizures).
In addition to the typical clinical picture of encephalitis, asymptomatic, abortive forms are often found, and less often - fulminant. In asymptomatic variants, there are no meningeal symptoms, but moderate headache and fever of unknown origin, mild transient episodes of diplopia, dizziness, paresthesia, etc. are noted. Changes in the cerebrospinal fluid clarify the nature of the disease.
In the abortive form, there are no neurological signs; the disease manifests itself as symptoms of an acute respiratory or gastrointestinal infection. Against the background of a moderate headache and low temperature, stiffness of the neck muscles may appear, which indicates the need for a lumbar puncture.
The fulminant form lasts from several hours to several days and ends in death. The disease begins with high fever and intense diffuse headache. Loss of consciousness quickly sets in, and patients fall into a coma. Rigidity of the neck muscles is pronounced. Death occurs from tabloid disorders or due to acute heart failure.
Therapeutic measures
There is no specific therapy for the treatment of encephalitis. As a rule, antiviral agents (cytoven or acyclovir) are used. It is also necessary to prescribe anticonvulsant and hormonal therapy, drugs to improve cerebral circulation and normalize the functioning of nerve cells. An important role is played by diet, special diet, vitamin and herbal medicine:
- the diet should not contain refined foods;
- do not eat red meat, sugar and pasta;
- you need to take vitamin C from 500 to 1000 mg per day;
- among probiotics, acidophilus is prescribed (it contains lactic bacteria);
- useful herbs include cat's claw, elderberry, green tea and astragalus.
Diagnosis of the disease Encephalitis
The most important and diagnostically valuable is the study of cerebrospinal fluid, which reveals lymphocytic pleocytosis (from 20 to 100 cells in 1 μl), a moderate increase in protein. Liquor flows out under increased pressure. Leukocytosis and an increase in ESR are observed in the blood. The EEG reveals diffuse nonspecific changes, dominated by slow activity (theta and delta waves). In the presence of epileptic seizures, epileptic activity is recorded. Magnetic resonance imaging reveals local hypodense changes in the brain. Sometimes a picture of a volumetric process is observed in hemorrhagic encephalitis, especially of the temporal lobe. Congestive optic discs are often detected in the fundus.
The etiological diagnosis is based, in addition to typical clinical manifestations, on the results of bacteriological (virological) and serological studies. Identifying the virus can be difficult and sometimes impossible. The virus can be isolated from feces and other environments, but the most important is the identification of specific antibodies using serological reactions: neutralization test (RN), complement fixation test (FFR), hemagglutination inhibition test (HIT), polymerase chain reaction (PCR).
Preventive measures
You can avoid the disease by using mosquito and tick protection. First of all, these are protective clothing and repellents. In areas where mosquitoes or ticks live, you need to be careful and ensure that most of the body areas are covered with thick clothing.
Vaccinations are the most important part of prevention. They are especially relevant for children. Parents should follow the vaccination calendar, showing their child to a pediatrician in a timely manner. The child should be taught to take regular walks in the fresh air, exercise, and exercise, since high immunity is always a reliable protector, including against dangerous viral infections.
Do you like the material?
Comments to the article 0
Autoimmune encephalitis - what happens if the immune system “attacks” its own nerve cells?
Autoimmune encephalitis is a neurological disease. It is dangerous for humans, since it is impossible to achieve complete recovery.
Doctors use symptomatic therapy aimed at alleviating the patient's suffering.
The disease is manifested by the production of antibodies (cells of the immune system), which are directed not against foreign microorganisms, but against the body’s own structures (in this case, nervous tissue).
Pathogenesis (mechanism of development)
As a result of exposure to a damaging factor, which is often a virus, the immune system begins to produce T-killers (cells that destroy viruses and infections). If too many of them are produced, the immune response becomes aggressive, it begins to act against its own cells.
When the cells of the gray and white matter of the brain (GM) are destroyed, the organ shrinks. The processes of atrophy begin in it (decreased vascular nutrition, decreased function). The disease affects one of the hemispheres. With necrosis of astrocytes (neuron cell processes), the connection between neurons is disrupted. The signal is not transmitted, so information from the outside world does not reach the person.
The destruction of neurons is an irreversible process, so the disease cannot be cured. Since the brain is responsible for the functionality of all body systems, the symptoms of autoimmune encephalitis are pronounced; the doctor will suspect it based on clinical manifestations and confirm it using laboratory and instrumental tests.
Differential diagnosis
Differential diagnosis is carried out on the basis of diagnostic methods. It is necessary to exclude infection, mycoses, injuries, tumors, viruses that cause the same signs of neuralgia as autoimmune encephalitis. Hereditary disorders of brain structures, autoimmune diseases of other organs, inflammation of blood vessels (vasculitis) of the brain, and sclerosing conditions of the brain have similar symptoms.
The main distinguishing feature of autoimmune encephalitis is the presence of inflammation in the blood, cerebrospinal fluid, leukocytosis (increased white blood cells), and the absence of a bacterial focus.
No other data on laboratory signs are revealed. CT and MRI scans show foci of brain inflammation in the early stages, and atrophy of one hemisphere in the later stages.
With age, characteristic symptoms of a neurological disorder are added.
Treatment
Treatment of autoimmune encephalitis is reduced to improving the quality of life, reducing tremor and pain. There is no complete cure.
The following principles of therapy apply:
- Bed rest.
- Walks in the open air.
- Drink plenty of fluids.
- Antipyretic drugs for body temperature above 38°.
- Painkillers analgesics (with severe cramps, muscle pain appears).
- Antiepileptic drugs.
- A diet containing high amounts of fatty acids and reduced amounts of proteins and carbohydrates.
- Purification of blood from immune complexes using plasmapheresis (liquid from the vessels is poured into a special preparation, purified, and returned back to the patient through a catheter).
- Medicines that improve the quality of the vascular wall (angioprotectors).
- Improving GM nutrition with the help of nootropic drugs (the more blood enters the organ, the more efficiently it works, the risk of atrophy decreases).
- Hormonal therapy (for damage to the pituitary gland).
- Drugs that inhibit (suppress) immunity.
- Corticosteroids.
Complications
The consequences of autoimmune encephalitis always occur. But in the absence of therapy they appear earlier. These include:
- short or long-term loss of consciousness;
- vegetative state of the body (a person is unconscious, connected to artificial ventilation);
- decreased intelligence;
- severe neurological disorders (lack of sensation in the legs, hand tremors, nystagmus);
- death.
If one of the symptoms of a neurological disorder appears, you should immediately consult a doctor. Timely therapy will improve the patient’s quality of life and prevent lethal effects at an early age.
Self-medication is not acceptable; the patient must strictly adhere to the therapy prescribed by the attending physician. It must be carried out throughout life; stopping taking the drugs is fraught with complications and death. The prognosis for autoimmune encephalitis is not good.
Patients in advanced stages are unable to walk, fall into a vegetative state, and then die.
Source: https://ponervam.ru/autoimmunnyj-encefalit.html
Treatment of Encephalitis disease
Pathogenetic therapy
Oral and parenteral administration of fluid is carried out, taking into account the water-electrolyte balance and acid-base state.
In severe cases of the disease, glucocorticoids are used. If the patient does not have bulbar disorders or disorders of consciousness, then prednisolone is used in tablets at the rate of 1.5-2 mg/kg per day. The drug is prescribed in equal doses in 4-6 doses over 5-6 days, then the dosage is gradually reduced (the total course of treatment is 10-14 days). For bulbar disorders and disorders of consciousness, prednisolone is administered parenterally at a rate of 6-8 mg/kg. Lumbar puncture is contraindicated. To combat hypoxia, humidified oxygen is administered through nasal catheters (20-30 minutes every hour), hyperbaric oxygenation will be performed (10 sessions at a pressure of p 02-0.25 MPa), sodium hydroxybutyrate will also be administered intravenously at 50 mg/kg per day or Seduxen 20-30 mg per day.
Indications. Allergic reactions, blood transfusion shock, anaphylactic shock, anaphylactoid reactions, cerebral edema, bronchial asthma, status asthmaticus, acute hepatitis, hepatic coma.
Contraindications. Hypersensitivity, previous arthroplasty, pathological bleeding, transarticular bone fracture, aseptic necrosis of the epiphyses of the bones that form the joint. Carefully. Parasitic and infectious diseases of a viral, fungal or bacterial nature: herpes simplex, chicken pox, measles; amebiasis, strongyloidiasis (established or suspected); systemic mycosis; active and latent tuberculosis, gastric and duodenal ulcers, esophagitis, gastritis, acute or latent peptic ulcers, diverticulitis, arterial hypertension, hyperlipidemia, diabetes mellitus, severe chronic renal and/or liver failure, nephrourolithiasis.
Side effects. Nausea, vomiting, increased or decreased appetite, bradycardia, insomnia, dizziness.
Also, in the treatment of encephalitis, diuretics are used to dehydrate and combat edema and swelling of the brain (10-20% solution of mannitol 1-1.5 g/kg intravenously; furosemide 20-40 mg intravenously or intramuscularly, 30% glycerol 1-1 .5 g/kg orally, diacarb, brinaldix).
Indications. Cerebral edema, hypertension, acute renal failure, epilepsy, Meniere's disease, glaucoma, gout.
Contraindications. Hypersensitivity, acute renal failure, liver failure, hypokalemia, acidosis, hypocortisolism, Addison's disease, uremia, diabetes mellitus, pregnancy (first trimester), nephritis, hypochloremia, hemorrhagic stroke.
Side effects. Hypokalemia, myasthenia gravis, convulsions, dehydration, tachycardia, nausea, vomiting.
A number of Russian pharmacologists and clinicians claim the existence of a highly effective antiviral drug, yodantipirin. It is stated that it has an etiotropic effect against flavivirus infection, but it should be noted that this drug is not used anywhere in the world for antiviral purposes, and there is no reliable data from evidence-based medicine confirming its clinical effectiveness.
Indications: Tick-borne encephalitis (treatment and prevention in adults).
Contraindications: Hypersensitivity, hyperfunction of the thyroid gland.
Side effects: Allergic reactions, swelling, nausea.
Etiotropic therapy
Etiotropic therapy consists of prescribing homologous gamma globulin titrated against the tick-borne encephalitis virus. The drug has a clear therapeutic effect, especially in moderate and severe cases of the disease. Gamma globulin is recommended to be administered 6 ml intramuscularly, daily for 3 days. The therapeutic effect occurs 12-24 hours after its administration: body temperature decreases, the patient's condition improves, headaches and meningeal symptoms decrease. The sooner gamma globulin is administered, the faster the therapeutic effect occurs. In recent years, serum immunoglobulin and homologous polyglobulin, which are obtained from the blood plasma of donors living in natural foci of tick-borne encephalitis, have been used to treat tick-borne encephalitis. On the first day of treatment, serum immunoglobulin is recommended to be administered 2 times at intervals of 10-12 hours, 3 ml for mild cases, 6 ml for moderate cases and 12 ml for severe cases. In the next 2 days, the drug is prescribed 3 ml once intramuscularly. Homologous polyglobulin is administered intravenously at 60-100 ml. It is believed that antibodies neutralize the virus, protect the cell from the virus by binding to its surface membrane receptors, and neutralize the virus inside the cell, penetrating it by binding to cytoplasmic receptors.
Antiviral drugs are also used - nucleases that inhibit the replication of the virus. RNase is used intramuscularly in an isotonic solution, 30 mg 5-6 times a day. Per course - 800-1000 mg of the drug. The antiviral effect is exerted by the drug cytosine arabinose, which is administered intravenously for 4-5 days at the rate of 2-3 mg per 1 kg of body weight per day.
Infusion therapy
In case of severe symptoms of intoxication, infusion therapy is carried out. For cerebral edema and bulbar disorders, the most rapid effect is provided by intravenous administration of prednisolone (2-5 mg/kg) or dexazone, hydrocortisone. For psychomotor agitation, epileptic seizures, seduxen is administered intravenously or intramuscularly - 0.3-0.4 mg/kg, sodium hydroxybutyrate - 50-100 mg/kg, droperidol - from 0.5 to 6-8 ml, hexenal - 10% solution 0.5 ml/kg (with preliminary administration of atropine); in enemas - chloral hydrate 2% solution 50-100 ml.
The complex of therapy should include antihistamines - calcium chloride solution, diphenhydramine, diprazine, pipolfen or suprastin, B vitamins, especially B6 and B12, ATP. With the development of flaccid paresis, the use of dibazole, galantamine, prozerin, oxazil is indicated.
Symptomatic therapy
— Antipyretic drugs
— Anti-inflammatory (glucocorticoids)
— Anticonvulsant therapy (benzonal, diphenin, finlepsin)
— Detoxification therapy (saline solutions, protein preparations, plasma substitutes)
— Resuscitation measures (ventilation, cardiotropic drugs)
— Prevention of secondary bacterial complications (broad-spectrum antibiotics)
Rehabilitation treatment
After discharge from the hospital, in the presence of neurological disorders, a course of rehabilitation treatment is carried out. Patients may be prescribed B vitamins, aloe extract, Cerebrolysin (contraindicated in the presence of seizures), aminalon, piracetam, pyriditol, pantogam.
Treatment of parkinsonism . An effective treatment for parkinsonism is taking L-DOPA (a dopamine precursor). The drug penetrates the blood-brain barrier and compensates for the lack of dopamine in the basal ganglia.
The most effective is combination treatment, which allows you to equalize the balance by strengthening the dopaminergic system (using L-DOPA or L-DOPA-containing drugs and meditane) and suppressing the cholinergic system (using cyclodol).
Treatment with L-DOPA is carried out according to a specific scheme, which involves gradually increasing the dosage and amount of the drug over several weeks. To reduce irritation of the walls of the gastrointestinal tract, the drug is prescribed after meals. The initial dose is 0.125 g per day, with a gradual increase by 0.125-0.25 g per day. The therapeutic effect is observed at different dosages, usually from 2 g to 5-6 g per day. With prolonged use of the drug over many years, its effectiveness decreases.
Contraindications to such treatment are bleeding stomach ulcers, severe liver and kidney diseases, decompensated state of the cardiovascular system, gloucoma, and mental illness.
Positive results from the use of L-DOPA or its derivatives are observed in approximately 70% of patients. Some of them return to work.
Treatment of hyperkinesis . Metabolic drugs, α-blockers, neuroleptics (haloperidol, chlorpromazine) and tranquilizers are prescribed.
Treatment of Kozhevnikov epilepsy . Metabolic drugs, anticonvulsants (Depakine, Tegretol, Sereysky mixture), tranquilizers (Elenium, meprobamate, trioxazine, gindarine, mebikar) and antipsychotics (aminazine) are also prescribed.
Encephalitis of the brain - causes, signs and treatment
Inflammation of the brain is accompanied by destruction of nerve tissue and disruption of the functioning of the nervous system. Typically, cerebral encephalitis is infectious. The disease manifests itself independently or as a result of a previous illness. Recovery depends on promptly seeking medical help.
Characteristics and causes of pathology
The concept includes a number of inflammatory diseases of the brain. Inflammation of the brain develops as a result of the penetration of a pathogen into the human body or as a result of allergic phenomena. The main reason for the development of the disease is neuroinfection.
Microbes and viruses interfere with the activity of nerve fibers, neurons and blood vessels, negatively affecting the functioning of the nervous system. Signs of intoxication appear, the membrane and certain areas of the brain are affected.
Depending on the affected area, meningitis and encephalitis are distinguished. Meningitis is accompanied by inflammation of the cerebral cortex, which develops as a result of hypothermia, the penetration of fungi, viruses, and bacteria. Encephalitis is a serious condition in which the brain becomes inflamed. The disease is characterized by severe course and high mortality.
Encephalitis can be primary or secondary. The source of infection in the primary form is usually insects. An infected individual bites a person, then the virus spreads through the bloodstream to the brain and other organs. This form manifests itself as a result of the rabies virus (from the bite of an infected dog), herpes, influenza, and Coxsackie. Microbial encephalitis is formed as a result, for example, of syphilis.
Based on the causes of the primary form of the disease, epidemic, tick-borne, herpetic, mosquito, and viral encephalitis are distinguished.
DTP vaccination, smallpox and rabies vaccines can cause the development of encephalitis.
Since vaccination can cause brain pathology in infants, a thorough examination of newborns by a pediatrician and neurologist is necessary.
Secondary encephalitis forms as a complication of another disease: toxoplasmosis, malaria, measles, rubella. You can become infected through airborne droplets or through consumption of contaminated food.
Risk factors
There are several factors that increase the risk of pathology:
- children under 1 year of age, elderly people;
- presence of herpes simplex virus;
- decreased immune status;
- summer-autumn period, when insect carriers of neuroinfection are most active.
Based on the location of the pathogen, subcortical, cerebellar, mesencephalic, and brainstem encephalitis are distinguished.
Types of disease
Each type of pathology is characterized by certain signs and a special course of the pathological process.
Epidemic
Another name is lethargic. Diagnosed in both children and adults. Symptoms manifest themselves in a sharp increase in temperature, intense headaches, and pain in the joint tissue.
The patient experiences confusion, delusions, and hallucinations. Later, squint, difficulty breathing, and excessive sweating are added.
Kleshchevoy
The frequency of detection of this species increases in spring and summer, when infected ticks are most active. The causative agent of the disease is transmitted through the bite of an encephalitis tick.
Once ingested, the infection enters the brain through the bloodstream. The person begins to be afraid of bright light, pain in the head increases, and vomiting develops. Numbness of the limbs occurs, muscle structures are paralyzed.
Komariny
Another name for the species is Japanese. Infected mosquitoes transmit the virus. The disease is accompanied by high body temperature, vomiting, and confusion. Tremors of the limbs and convulsive seizures are recorded. The species is characterized by a high mortality rate.
Flu-like
Develops as a complication of influenza. Manifested by nausea, headache, weight loss, weakness. The disease often puts the victim in a comatose state.
Measles
Since measles is a childhood disease, this type of encephalitis is characteristic of children. Inflammation of the brain begins to develop several days after measles.
The patient becomes weaker, develops a feverish state, and suffers from epileptic attacks. The disease damages the nerves of the skull, causing paralysis and myelitis.
Anti-receptor encephalitis: what is this disease and how to treat it
Chickenpox
Progresses due to chicken pox. The disease is more often diagnosed in childhood. The child weakens and becomes drowsy. Coordination of movements is gradually impaired, paralysis of the arms and legs, and epileptic seizures develop.
Herpetic
The herpes virus attacks the cerebral cortex. This type progresses slowly, leading to impaired consciousness, painful headaches, and chaotic movements of the limbs.
Signs of the disease
Symptoms of encephalitis are differentiated depending on the causative agent of the disease and its location. There are also general manifestations of pathology. Like other infectious diseases, encephalitis affects the increase in body temperature, indigestion, and disturbances in the functioning of the respiratory tract.
Vomiting, photophobia, epilepsy attacks appear, and headache increases. Patients' consciousness is impaired and the person may fall into a coma. There are problems with psychomotor and sensory perception of reality: physical hyperactivity, incorrect understanding of the parameters and shapes of objects.
Encephalitis can be asymptomatic, fulminant, or abortive. The asymptomatic course is accompanied by slight pain in the head and slight dizziness. Abortive forms cause symptoms of colds or stomach infections.
The most dangerous form is fulminant, which progresses over several hours. The temperature rises sharply, the person falls into a coma. Deaths are recorded as a result of heart failure.
Possible complications
Mild inflammation of the brain resolves without significant complications. Treatment of a severe form of the disease can last several years. The consequences of cerebral encephalitis do not develop in all people; they depend on the individual characteristics of the body.
The most dangerous situation is when the patient does not feel painful signs, while the virus spreads throughout the structure of the brain. In this case, irreversible complications develop:
- chronic fatigue;
- personality changes;
- inability to concentrate;
- amnesia, which over time leads to problems with short-term memory;
- impairment of motor activity;
- mental disorders;
- loss of sensory sensitivity.
Degenerative processes in brain structures lead to disability and death.
Diagnostic methods
The dominant diagnostic method is puncture, during which a specialist takes cerebrospinal fluid (CSF). The biological material is examined and lymphocytic pleocytosis and protein concentration are detected.
A blood test reveals a high number of leukocytes, and the erythrocyte sedimentation rate increases. Epileptic activity is recorded. During magnetic resonance imaging, pathological changes in the brain are recorded. When examining the fundus, congestion of the optic nerve is determined.
The disease is diagnosed based on the results obtained from bacteriological and serological tests. Virological identification is very difficult.
Methods of therapy
If painful signs are detected, you must urgently call an ambulance. The patient is placed in the infectious diseases department. The outcome of treatment depends on the speed of treatment. Often the patient requires the help of a resuscitator.
Treatment of encephalitis includes etiotropic, pathogenetic and symptomatic methods.
Etiotropic treatment
Eliminates the causes of brain inflammation, one of which is the penetration of an infectious agent. To eliminate the infection, antibacterial drugs, antiviral agents and human immunoglobulin, which is necessary for tick-borne encephalitis, are used.
Antibiotics are used for bacterial encephalitis and are administered intravenously. Antiviral medications include Acyclovir, Cycloferon, Viferon, and Proteflazid.
Pathogenetic treatment
It is based on the use of medications that restore damaged brain structures. These medications include:
- hormonal agents;
- anti-edema drugs - Mannitol, Diacarb, Furosemide;
- antihistamines - Suprastin, Loratadine, Zodak, Tavegil;
- infusions that correct metabolic processes - Dextran, Trisol, potassium;
- angioprotectors – Cavinton, Instenon;
- antihypoxants – Cytochrome, Mexidol, Actovegin;
- anti-inflammatory medications - Xefocam, Nurofen.
The patient is given vitamin preparations, drugs that correct the functioning of the heart and respiratory tract.
Symptomatic treatment
Eliminates the manifestations of individual symptoms resulting from encephalitis. Doctors prescribe anticonvulsants, antipyretics, and antipsychotic drugs. It is necessary to take drugs that activate the functioning of the neuromuscular system (Neuromidin) and reduce muscle tone (Sirdalud).
Note! Epilepsy attacks can remain with a person forever, requiring the use of anticonvulsants for the rest of their life.
The victim is prescribed physiotherapeutic measures: massage, acupuncture, physical therapy, electrical stimulation. The patient should work with a psychotherapist or speech therapist.
At the initial stage, encephalitis does not manifest itself with characteristic symptoms; the symptoms are similar to a cold. Therefore, a person goes to the doctor late, when the brain cells are already destroyed. Emergency medical care can save the patient.
Source: https://neuromed.online/entsefalit-golovnogo-mozga/
Encephalitis of the brain
Encephalitis of the brain is a brain disease associated with inflammatory reactions and is caused by the penetration of an infection, virus or foreign protein into the brain substance and affecting the nervous system.
Symptoms of the disease in adults
Signs of brain encephalitis in adults include general infectious, general cerebral, meningeal (in special cases) and focal signs.
Common infectious symptoms in adults include:
- general impotence;
- feeling unwell;
- brokenness.
Characterized by sleep disturbances and decreased appetite. Pain appears in muscles, joints, and bones. Body temperature rises to febrile levels and higher, chills appear. The development of rhinorrhea is possible, characterized by the appearance of dryness, soreness, and pain in the throat.
This group also includes dyspeptic syndrome (nausea, vomiting, diarrhea, flatulence, rumbling).
In a clinical and biochemical blood test, you can see changes that are characteristic not only of encephalitis, but of any other somatic pathology.
Common brain symptoms include: headache, nausea, vomiting, non-systemic dizziness, mental disorders, generalized epileptic seizures. Characteristic is a disturbance of consciousness, which can be caused by its suppression (stunning, blocking, coma), or its change (delirium, hallucinations).
Meningeal signs include: a triad of symptoms (headache, vomiting, fever), stiff neck, positive Kernig, Brudzinski and Lessage signs.
Focal symptoms are characterized by: local sensitivity disorders, decreased muscle strength, hypotonicity, muscle hypertonicity, speech disorders. The patient is unable to read anything, write any word, ceases to recognize objects, and to say what they are intended for.
Characterized by impaired coordination of movements, decreased memory or its loss up to amnesia, ringing in the ears, impaired movements of the eyeballs, control over the functions of the pelvic organs is impaired, and the cranial nerves are affected.
Symptoms of the disease in newborns
The clinical picture of brain encephalitis in children should be determined by the duration of the process, its localization in combination with another disease, or whether it is an independent disease.
It often happens that few people can immediately distinguish encephalitis of the brain in mice from a common cold. The disease can show different manifestations. First, you can detect signs of a common acute respiratory infection in a newborn baby, and not brain encephalitis.
Signs of encephalitis in children:
- epidemic encephalitis: strabismus, ptosis, drowsiness and apathy;
- herpetic encephalitis also has its own symptoms: an attack of epilepsy is characteristic, in the foreground are general infectious symptoms, and then everything else, paralysis and paresis.
Encephalitis
The health of the central nervous system is the health of not only the body, but also the mental state of a person. When the brain substance is damaged, various unpleasant symptoms develop. A person is not able to control his body and his own emotional mood. What happens to a person and how to eliminate it? Read all about encephalitis on vospalenia.ru.
What is encephalitis? This term is used in relation to the inflammatory process occurring in the substance of the brain. The causes and forms of its manifestation are very diverse. Let's look at them all:
- According to localization, the following types are distinguished:
- General cerebral.
- Focal - itself is divided into the following areas:
- Frontal lobe.
- Temporal lobe.
- Parietal lobe.
- Occipital lobe.
- The presence of affected areas of the meningeal membranes:
- Isolated.
- Meningoencephalitis.
- For reasons of occurrence:
- Infectious: viral, bacterial, fungal.
- Autoimmune – an attack of the immune system on its own cells. This includes demyelizing encephalitis and leukoencephalitis.
- Post-vaccination (post-vaccination) – a complication after vaccination.
- Toxic – severe poisoning.
- According to the area of the affected brain, the following types are divided:
- Cortical.
- Subcortical.
- Stem.
- Cerebellum.
- Epidemic (Economeau's disease, encephalitis A, lethargic) - provoked by a filterable virus transmitted by airborne droplets.
- Tick-borne (spring-summer, taiga) is an infection transmitted through ticks. Forms of development of this type: Febrile - fever, mild neurology.
- Meningeal - pain in the head, stiff neck, inability to straighten the legs when lying on the back.
- Meningoencephalic – fever, delirium, hallucinations, twitching, paresis, psychomotor agitation, epileptic seizures. Deadly form.
- Poliomyelitis - atrophy and paralysis of the muscles of the arms and neck: the head hangs, the arms fall.
- Polyradiculoneurotic – damage to peripheral nerves, their tingling and numbness.
- According to the development mechanism, it happens:
- Primary is damage to the brain itself.
- Secondary - brain damage - a symptom or complication of another disease.
- Complicated.
- Uncomplicated.
go to top
Encephalitis in children and adults
Encephalitis appears at any age. Infection can occur at any age. Countries where infection carriers are located become dangerous. There is no division into gender and age: lesions are observed in everyone - men, women, children. If strange symptoms are detected, you should contact a neurologist or therapist.
go to top
Lifespan
Encephalitis is a dangerous disease that gradually destroys the structure of the brain. How long do patients live? It all depends on the measures taken. Without treatment, life expectancy becomes short. The brain gradually deteriorates and complications develop:
- Autonomic disorders.
- Severe neurological symptoms.
- Paralysis.
- Paresis.
- Organic brain damage.
- Death.
Prevention of the disease can only consist of refusing to visit those countries where the development of encephalitis is possible, and vaccination in moderate quantities.
Source: https://vospalenia.ru/encefalit.html