Residual encephalopathy is a brain disease caused by tissue damage and death of nerve cells (neurons). It occurs in people of all ages, including children. The disease can be congenital or acquired. Pathological changes develop if blood supply to the brain is disrupted and cells experience oxygen starvation. This condition can be provoked by traumatic brain injury, vegetative-vascular dystonia, atherosclerosis, hypertension, infections, ischemia, stroke, diabetes mellitus, toxic substances, radiation, uncontrolled medication use, use of drugs and psychotropic drugs, and brain surgery. Congenital encephalopathy can occur as a result of complicated pregnancy, intrauterine development abnormalities, bad habits of the expectant mother, or birth injuries.
Residual encephalopathy in children.
In children, a condition such as residual encephalopathy is most often a consequence of organic brain damage in the perinatal period (from 28 weeks of pregnancy to 7 days of life).
It can be:
- birth injury;
- intrauterine infection;
- hypoxia (oxygen starvation of the child during pregnancy and childbirth).
Also of considerable importance are:
- mother's age (under 20 or over 35 years);
- illnesses during pregnancy;
- drinking alcohol, smoking;
- heredity.
Most often, there are signs that the child will develop residual encephalopathy in the future from the very first days and months of life:
- anxiety, or, conversely, excessive lethargy;
- baby cries most of the time;
- frequent shuddering;
- inadequate reactions to light and sound stimuli;
- tilting the head.
If the brain damage is not too significant, then these disorders are quickly compensated, since the child’s brain has a good ability to adapt, but with age, relapses can be observed, that is, echoes of past problems.
Such children develop:
- outbursts of rage, aggression;
- poor performance at school, inability to learn the material well;
- slowness of thinking;
- memory impairment;
- headache;
- nausea, vomiting;
- episodes of loss of consciousness;
- sweating;
- sleep disorders.
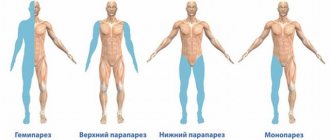
In more severe cases, movement disorders and the development of epilepsy may occur.
Diagnostics
How is this disease diagnosed? It is worth understanding that there are no established rules for the treatment of this type of disease. Perhaps this happens because it is not so widespread, but among mental disorders and illnesses, namely residual and delayed psychotic disorders, it occupies almost 80th position. It is also worth remembering that this happens precisely because of the use of doping in the form of drugs. It is worth understanding that treatment can be diagnosed, firstly, because the patient talks about himself, and in order to find out whether he has a disease or not, it is necessary to take a urine and blood test. Tests must be taken in order to identify the disease. First you need to understand whether there are traces of narcotic drugs in a person’s blood; it is worth remembering that soft drugs also leave the body for a long time.
Residual encephalopathy in adults.
In adults, the causes of development may be:
- traumatic brain injuries: repeated concussions, brain contusion;
- consumption of alcohol, psychotropic and narcotic substances;
- the effect of toxic substances (industrial poisons), ionizing radiation;
- previous strokes;
- frequent rises in blood pressure to high numbers;
- diabetes mellitus, liver and kidney diseases;
- cerebral atherosclerosis;
- meningitis, encephalitis.
Manifestations:
- persistent long-term headaches that are difficult to treat;
- migraine attacks with nausea, vomiting, photophobia, blurred vision and hearing;
- drowsiness during the day and insomnia at night;
- decrease in memory and intelligence up to the development of dementia;
- tearfulness, suspiciousness, mood instability, irritability;
- general weakness, fatigue;
- fluctuations in blood pressure and pulse;
- parkinsonism and seizures (in more severe cases).
Symptoms of the disease
Signs of schizophrenia are usually divided into several groups.
1. Positive (psychotic, productive). These include:
- hallucinations – a distorted or false perception of the world, non-existent phenomena and images. They can be tactile, visual, auditory, etc.;
- Delusional states are the patient’s false ideas about what is happening. It is almost impossible to convince a person that they are wrong;
- violation of the general rules of perception of what is happening;
- inability to concentrate - the individual is unable to organize his thoughts, so his speech becomes incoherent, meaningless, and incomprehensible to others;
- repetition of movements - the patient methodically repeats the same movements or freezes for a while in unusual positions.
2. Negative symptoms. They manifest themselves through the patient’s associativity - such a person loses the ability to show emotions, is depressed, and is cut off from reality.
3. Cognitive signs are expressed in a violation of the thought process. The patient is unable to concentrate and use the information received, and the person’s memory process significantly deteriorates.
A schizophrenic is unable to separate reality from the things and events he imagines. However, this disease is not a death sentence - it can and should be controlled. It is managed in three stages: recognizing the first signs of the disease, timely contacting a specialist, and unquestioningly following all the doctor’s recommendations and prescriptions.
Residual encephalopathy in combination with intracranial hypertension.
Intracranial hypertension is the accumulation of fluid in the cranial cavity, which compresses the brain tissue, resulting in:
- weather sensitivity (reaction to changes in atmospheric pressure);
- persistent headaches that get worse with changes in body position;
- nausea, vomiting for no reason;
- flashing “flies” before the eyes;
- heartache;
- fatigue, irritability.
Intracranial hypertension is a common “companion” of residual encephalopathy and explains many of its symptoms.
Symptoms of schizophrenia
Schizophrenia is the most common disease among endogenous pathologies. It affects about 1% of the world's population
, 2 million new cases are reported annually. Endogenous means caused by changes in internal processes in the body, in contrast to exogenous disorders caused by the influence of environmental factors. In the pathogenesis of schizophrenia, a functional disorder of the central nervous system and an imbalance in the processes of excitation and inhibition due to disturbances in the exchange of neurotransmitters are noted. The disease begins mainly at a young age, is characterized by a variety of symptoms and progression, which leads to social maladjustment of the individual. Symptoms of the disease are differentiated into three categories: positive (excess of emotions, thoughts, actions), negative (deficit of emotions, thoughts, actions) and psychomotor.
Positive symptoms
Rave –
an unfounded, firm belief in something that does not exist. Some patients have only one line of delusion affecting behavior, while others have several lines. The most common delusions of persecution, delusions of relation, or delusions of grandeur occur.
Disorganized thinking and speech.
Schizophrenics who are unable to think logically express themselves in bizarre ways. Often this is a pathological excess of neologisms, invented non-existent words, perseveration, repeated repetition of phrases, rhyming, speech confusion, rapid transitions from one topic to the opposite.
Formal thought disorder
is
a disorder in the production and organization of thought. There is no connection or meaning in the statements. In severe disorders, the associative process is loosened and the flow of thoughts is disrupted. Influx, breakage or slippage, weakening of the connection between thoughts, poverty of thinking, production of mystical or pseudoscientific ideas.
Heightened perception and hallucinations.
A variety of hallucinations, mostly auditory, a voice commenting in a third person, visual hallucinations are less common, such as unclear changes in the color or shape of an object. Olfactory and tactile in the form of fear of poisoning or persecution. Tactile hallucinations - tingling, burning, current flowing through the body, or the feeling that someone is crawling inside.
Emotional inadequacy.
Sharp groundless mood swings, demonstration of rude emotional reactions that do not correspond to the situation.
Negative symptoms
Alogia
is
a poverty of speech or its content. In some cases, it is accompanied by impoverishment of thinking or a complete lack of meaning in what is said.
Emotional dullness and emotional flattening.
Some patients show rage, sadness, jubilation, anger, to a lesser extent than most people, others do not show any emotions at all (emotional flattening). The faces of such people do not contain facial expressions and are characterized by a devastated look and a monotonous voice.
Abulia
(lack of will). Apathy, loss of desires and interest in the goal, loss of energy and ability to start something new.
Social isolation.
Shutting off from social surroundings or distancing yourself from people to avoid talking to them. This further leads to autism, withdrawal from reality, impaired communication skills and the ability to understand the feelings of other people.
Psychomotor symptoms
Catatonia.
A set of motor poses: stupor-excitement, numbness or posing. Stereotypes – repeated aimless movements, swaying, jumping. A person in a catatonic stupor stops responding to external signals, remaining quiet and motionless for a long time.
mannerism
. Strange movements that do not correspond to the situation - repeated raising of the hand in the form of a military salute, ambivalence - interruption of the started action to do the opposite, for example, reaching out for an object and pulling it back without taking it. People who are constrained in movement experience increased grimacing and increased gesticulation.
Diagnosis and coding according to ICD-10.
Considering the fact that the disease manifests itself years after damage to the brain tissue, it is quite difficult to diagnose it, it is very important to collect a correct history. Every mother should be well aware of the details and complications during childbirth and the postpartum period; all facts of diseases suffered by a person must be recorded in medical documentation.
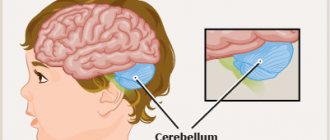
The main thing in diagnosis is a computer examination of the brain (MRI or CT), which will identify areas of brain damage and signs of intracranial hypertension.
There is no term “residual encephalopathy” in ICD-10, but doctors widely use it, coding it G93.4 (encephalopathy, unspecified).
Residual changes in the brain: what is it, how to treat encephalopathy
Residual encephalopathy is characterized by dystrophic changes in brain tissue. Changes in the morphological structure of the medulla lead to dysfunction of the central nervous system.
Organic damage to nervous tissue is characterized by signs: the fact of exogenous (external) harmful effects, the appearance of pathognomonic (typical for this disease) symptoms against the background of cerebral dysfunction, instrumental confirmation of pathomorphological changes in the brain matter.
Definition
Residual means that it arose as a result of a certain event (trauma, intoxication, neuroinfection, surgery). Encephalopathy is a disease of the central nervous system of non-inflammatory origin. Residual encephalopathy is a pathology that can include secondary brain lesions, which presupposes a history of a primary disease.
In the ICD-10 list, residual encephalopathy is listed under the code “G92” (toxic), “G93.8” (post-radiation), “G93.4” (unspecified). If the residual nature of pathological foci formed in the brain is emphasized, this means that a change in the morphological structure of the nervous tissue is associated with a primary pathology.
Classification
Residual changes in the brain of newborns lead to the development of perinatal encephalopathy.
This form of residual encephalopathy is detected in children in the first year of life, which is associated with diseases suffered by the mother during gestation and other adverse effects on the fetus (hypoxia, birth injuries, infectious lesions). Taking into account etiological factors, the main forms of residual brain damage are distinguished:
- Toxic. Exposure to harmful substances (heavy metal compounds, poisons, medications in high concentrations) provokes damage to nervous tissue.
- Alcohol, drugs. Chronic poisoning with ethyl alcohol or narcotic substances has a destructive effect on the brain matter.
- Discirculatory. It develops against the background of cardiovascular diseases, arterial hypertension, atherosclerotic damage to the vessels supplying the brain, ischemic processes and oxygen starvation of the brain.
- Post-traumatic. Mechanical damage to brain tissue leads to disturbances in the functioning of the central nervous system.
- Hepatic, renal. Develops as a result of liver or kidney failure.
- Glycine. Occurs as a result of a violation of glycine metabolism.
There is residual encephalopathy of the brain in adults, provoked by hypovitaminosis (lack of vitamins) or radiation exposure.
Cerebral infarctions and strokes often cause this type of encephalopathy.
The development of such disorders is caused by dysplasia (underdevelopment) of connective tissue, which is manifested by hemicrania (attacks of acute pain in one half of the head), vegetative-vascular dystonia, deterioration in performance, and panic attacks.
Other types: Wernicke encephalopathy, which occurs due to vitamin B1 deficiency, and Creutzfeldt-Jakob disease, which develops due to the penetration of prions into the body (an infectious agent represented by a protein of abnormal structure).
Depending on the characteristics of the development of the clinical picture, progressive and stable forms are distinguished.
In the first case, there is an increase in neurological symptoms, in the second, the nature and severity of the symptoms remain unchanged.
Depending on the predominance of pathognomonic symptoms, the main groups of disorders are distinguished: with a dominant impairment of cognitive functions and consciousness (stupefaction, inability to concentrate) or with a prevailing disorder of perception (hallucinations - realistic perception in the absence of real stimuli), thinking (incoherent, meaningless speech), emotions.
Causes
Residual genesis means that dystrophic-atrophic changes in the nervous tissue are provoked by a primary pathology or external influence. Common reasons:
- Postnatal (in the period after birth) hypoxia, asphyxia (suffocation).
- Birth injuries.
- Encephalitis caused by vaccinations.
- History of meningoencephalitis.
- Injuries, bruises of the head and spine.
- Alcohol abuse.
- Poisoning with poisons and other harmful substances.
- History of cerebral vascular diseases.
Residual changes that have occurred in the brain are often associated with genetic mutations, abnormalities in the formation of brain structures during intrauterine development, hypoxic-ischemic processes in the fetal brain tissue, which means that the causes of occurrence correlate with perinatal pathologies. Perinatal genesis is detected in 80% of cases.
Residual phenomena can be provoked by anomalies in the development of elements of the circulatory system, these are primarily vascular malformations, aneurysms, and pathological tortuosity of the circulatory network. Other causes reflect the result of a previous disease of the nervous system - central or peripheral.
Treatment and selection of drugs.
Treatment of residual encephalopathy is symptomatic:
- analgesics for headaches (MIG-400, nimesulide);
- antimigraine (sumamigren, amigrenin);
- sedatives, anti-anxiety (Persen, Afobazole);
- sleeping pills (sonnat, zopiclone);
- to improve memory (alzepil, glycine);
- for intracranial hypertension syndrome - drugs that reduce cerebral edema (diacarb, normoven, dioflan).
In addition, you should take maintenance courses of nootropic drugs (to improve the nutrition of brain cells and increase their reserves) 2 times a year. In case of changes in the mental sphere, visits to a psychologist, psychiatrist, or psychotherapist are required. In children, with timely diagnosis and properly selected treatment, in 20-30% of cases it is possible to achieve complete recovery, and in adults, it is possible to achieve stable remission, when the manifestations of the disease are minimal or disappear altogether for a long time.
Residual period of stroke
Understanding what stage of the disease the patient is at is of fundamental importance. Treatment methods and features of patient care will depend on this. There are 5 stages of stroke: acute, acute, early recovery, late recovery, residual.
The most acute period of stroke. The patient is currently in the intensive care unit of the hospital. The patient is recommended to undergo strict bed rest and limit active movements. At this stage, the main task is the struggle for the survival of as many affected nerve cells as possible.
How quickly therapeutic measures begin depends on the consequences of the stroke. Main activities: courses of drip intravenous drugs. Their task is to eliminate cerebral edema, restore and improve the functioning of nerve cells.
Doctors continuously monitor the functioning of the main organs.
Acute period of stroke. It covers about 6 weeks. Inpatient treatment continues. Now in a regular ward. At this stage, relative stabilization of all vital functions of the body is achieved, and restoration processes in the brain begin.
At this time, physical therapy and physical therapy sessions, including massage, usually begin.
Patients take drugs from the neotropic category; these drugs stimulate regenerative processes in the brain, and also use courses of drugs whose task is to improve the process of oxygen delivery to damaged tissues.
Early recovery period of stroke. It can last for 6 months. The patient is being treated at home in a rehabilitation center. The doctor continues to prescribe courses of nootropic and vascular drugs. Active work with paralyzed limbs is important; massage and physical therapy courses are conducted. The patient begins to master lost skills.
Late recovery period of stroke. It extends up to 1 year. Some brain structures continue to recover, and the person is already able to make movements and even walk. Continue physical therapy and physiotherapy.
Residual stage of stroke , it begins one year after the stroke. Most of the recovery processes are completed, the patient adapts to a new way of life.
In order for recovery to be possible, a patient with a stroke must be hospitalized for examination and treatment on the first day. Within 72 hours, it is recommended to conduct ultrasound examinations that will show the condition of the brain vessels.
They include duplex scanning of the main arteries of the head, transcranial Doppler sonography. It is necessary to examine the heart: electro- and echocardiography, study of hemorheological properties of blood (hematocrit, viscosity, fibrinogen level, platelet aggregation, erythrocytes, etc.
).
To establish an accurate diagnosis that reflects the location and nature of the stroke (ischemic or hemorrhagic), it will be necessary to perform a computed tomography of the brain or magnetic resonance imaging.
The examination plan may include cerebral angiography, electrocardiogram, daily monitoring of blood pressure, and other methods that take into account the characteristics of the disease in a particular case.
Read also: A man has a stroke
As a result of a comprehensive clinical, instrumental, and laboratory examination, it is possible to reveal the main cause and mechanisms of stroke in each patient. You need to competently assess the situation and wisely manage your chance to survive.
Periods of stroke
Among the huge number of neurological diseases, stroke is the most important problem.
Hemorrhage in the brain leads to disruption of intracranial circulation, neuronal necrosis and disruption of vital body functions.
Only 10% of patients return to a normal, full life; the rest adapt to life with lost abilities. Some patients have to relearn how to speak, walk and perform basic everyday activities.
The vast experience and high professionalism of neurologists, physiotherapists, neurosurgeons, psychologists, and speech therapists at the Yusupov Hospital allow us to achieve the highest results. Patients who were abandoned by doctors in other medical institutions successfully undergo rehabilitation at the Yusupov Hospital and begin an active life.
A stroke is a brain pathology that develops as a result of destruction or blockage of the blood vessels that supply the brain. Blood stops flowing to the neurons and they die.
Stroke is divided into two types – ischemic and hemorrhagic. The first type is also called cerebral infarction. It develops due to poor blood flow to brain cells when neurons begin to die.
Hemorrhagic stroke develops due to hemorrhage in the brain when a vessel ruptures. In this case, even capillary bleeding is enough for the development of severe disorders.
In any case, be it an ischemic or hemorrhagic stroke, they develop in a matter of minutes and the patient requires immediate hospitalization. Timely medical assistance often saves the lives of patients at the Yusupov Hospital.
Periods of ischemic stroke
In ischemic stroke, a number of processes are observed that together lead to the death of neurons. Cell destruction occurs against the background of cerebral edema. At the same time, the brain increases in volume and intracranial pressure increases.
Due to cell swelling, displacement of the temporal lobe is observed, as well as infringement of the midbrain.
Compression of the medulla oblongata may also occur due to wedging of the cerebellar tonsils into the foramen magnum. This process quite often leads to death. Therefore, early hospitalization of the patient is extremely important.
When the first signs of an ischemic stroke appear, medical assistance should be provided within the first three hours, otherwise the prognosis is disappointing.
There are several periods of ischemic stroke:
- acute;
- spicy;
- early recovery period of stroke;
- late recovery;
- stage of residual effects.
The most acute period of ischemic stroke
In the first three hours, it is possible to restore blood flow and eliminate or reduce neuronal death through the use of thrombolytics. It is also possible to administer drugs into the stroke area itself, which helps prevent the development of complications.
Then doctors take measures to restore pressure, carry out rehydration, dehydration and oxygen therapy.
Read also: Lifestyle after a stroke
During the most acute period of a stroke (from 4 to 5 hours after the attack), the patient should be under the close supervision of a doctor in a hospital setting.
Acute period of ischemic stroke
The period up to 14 days after the attack is considered acute. The patient continues to undergo treatment in a specialized department of the hospital. He is undergoing drug therapy aimed at:
- reduction of cerebral edema;
- maintaining normal blood viscosity and coagulability;
- maintaining normal functioning of the cardiovascular system;
- relapse prevention;
- maintaining normal blood pressure.
Early recovery period of stroke
The early recovery period is considered to be the period from 2 to 6 months after a stroke. At this stage, complex treatment is carried out:
- the patient takes medications according to an individual treatment regimen;
- in case of speech impairment, a speech therapist works with the patient;
- various manipulations are prescribed to restore sensitivity of the limbs and other parts of the body (massages, baths, acupuncture and others);
- physical therapy – the method helps strengthen ligaments and muscles.
Late recovery period of stroke
The late recovery period is the time six months after the stroke. At this stage, the results of treatment and rehabilitation measures taken during the early recovery period are already visible. The patient's finger sensitivity is restored and motor skills improve. It is extremely important not to stop the complex of procedures. Rehabilitation after a stroke is a long and labor-intensive process.
Period of residual effects of stroke
The time from one to two years after a stroke is considered the residual period. At this stage, it is important to follow all doctor’s instructions and take measures to prevent a recurrent stroke.
Rehabilitation specialists and neurologists at the Yusupov Hospital create a treatment and rehabilitation program individually for each patient, which allows achieving high results in recovery after a stroke. You can make an appointment by phone.
Recovery and dangerous periods of stroke
Successful recovery and the effectiveness of treatment for the consequences of a stroke largely depend on the severity of the disease and on how timely therapy is started. An important factor is the patient’s psychological mood, his motivation for a speedy and full recovery.
The disease occurs in several stages, during which various changes occur in the functional structures of the brain:
Time is the main factor in successful recovery after a stroke! Rehabilitation will be more effective if it is carried out in the early stages and the consequences of the disease are not advanced.
- All information on the site is for informational purposes only and is NOT a guide to action!
- can give you an ACCURATE DIAGNOSIS !
- We kindly ask you NOT to self-medicate, but to make an appointment with a specialist !
- Health to you and your loved ones!
General signs
To avoid serious complications and difficulties in the recovery period, you need to know the signs of a stroke:
- clouded consciousness of the patient, fainting;
- facial redness;
- increased body temperature;
- impairment of motor functions of the limbs;
- tactile sensitivity decreases or completely disappears;
- on the affected side, the corner of the mouth droops, the eyes do not close, and the face becomes asymmetrical.
It is those around you who should notice the changes happening to the patient. He himself is able to objectively notice such violations due to the specific nature of the disease.
What is the most dangerous period after a stroke?
Medical science recognizes two periods of stroke as the most dangerous - acute and acute.
It is at these stages that serious complications may occur, such as a recurrent stroke, the formation of blood clots and their blockage of the lumens of blood vessels, and an increase in cerebral edema.
This state of affairs is more typical for severe strokes, accompanied by paralysis and impaired consciousness.
Actions in a given period of time
Patients in the acute period of a stroke should be immediately hospitalized. The first 3 hours after the onset of the disease is a sensitive period for effective recovery.
Hospitalization is excluded only in one case - if the patient is in a state of agony.
The optimal option for hospitalization is placement in a multidisciplinary hospital, where it is possible to carry out the maximum number of diagnostic measures and receive advice from a neurosurgeon.
Emergency actions carried out by an ambulance team or other persons transporting a patient to a hospital include:
- correction of oxygenation, i.e. increasing the volume of oxygen supplied to brain cells;
- maintaining normal blood pressure;
- exclusion of seizures.
Upon admission to the hospital, emergency measures are as follows:
- diagnostics of oxygenation level;
- assessment of blood pressure levels;
- examination by a neurologist;
- carrying out a minimum set of laboratory tests;
- the use of MRI to build a program of adequate treatment and recovery;
- making a decision about the patient’s further place of stay.
Treatment in a hospital can take from several days to several months. In any case, after discharge, rehabilitation measures must be continued at home or by visiting specialized centers.
Recovery period
Recovery after a stroke is a complex and long-term process. Often weakened patients cannot find positive motivation to continue the necessary procedures and activities, so during this period they especially need support and assistance.
Rehabilitation center after stroke