Discirculatory encephalopathy grade 3: how long can you live? This problem is no longer relevant for those who are sick, but for the patient’s loved ones, since this pathological process is considered a severe brain pathology. DEP grade 3 is such a serious condition that the patient is not able to realize the fact of his existence. Therefore, a detailed consideration of dyscirculatory encephalopathy of degrees 1, 2, 3, the prognosis of the patient’s life, the root causes of it is required, to learn how the pathology is classified, manifested, and treated.
Encephalopathy
Discirculatory encephalopathy is a chronic progressive pathology, which is characterized by diffuse or focal changes in the structures of the brain. The disease is a common form of progressive cerebrovascular insufficiency.
Classification
Since discirculatory encephalopathy is not a primary independent disease, but is a consequence of other pathologies that affect blood vessels, the disease is usually differentiated into types depending on the etiological causes. There are varieties:
- atherosclerotic;
- hypertensive;
- mixed;
- venous;
- a form that arose against the background of other diseases: neurocircular dystonia, rheumatism, diseases of the circulatory system.
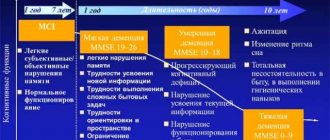
The disease is also divided into three stages with a gradual increase in clinical symptoms.
Causes
Discirculatory encephalopathy occurs as a result of a long-term chronic course of somatic ailments:
- atherosclerosis – damage to the elastic arteries of the brain;
- hypertension - persistent arterial hypertension;
- venous hyperemia – difficulty in venous outflow due to narrowing of the lumen of blood vessels;
- vegetative dystonia syndrome;
- angiodystonic crises due to disruption of systemic hemodynamics;
- diseases of the circulatory system;
- inflammatory lesions of the walls of blood vessels - vasculitis.
Symptoms
The characteristic clinical symptoms of dyscirculatory encephalopathy worsen as the disorder worsens. The main signs of pathology are the following manifestations.
- Cognitive problems (memory deterioration, decreased concentration, illogicality and inconsistency of thinking). With stage 3 disease, signs of senile dementia are observed - vascular dementia.
- Disorders of the affective sphere, manifested by abrupt changes in psycho-emotional status. Mood changes are especially pronounced during adolescence, pregnancy, and after childbirth.
- Pyramid disorders - motor dysfunctions: spasticity, paresis or paralysis, problems with coordination of movement, walking impairment, the occurrence of a pathological reflex response. Such problems arise in most cases with grade 2 disculatory encephalopathy.
- Autonomic failures and defects of the vestibular apparatus: surges in blood pressure, dizziness, nausea. They appear already in stage 1 disease.
Among other signs:
- difficulty chewing and swallowing food;
- change in timbre and speed of speech;
- irrational unnatural laughter and crying;
- decreased ability to work;
- facial asymmetry;
- cephalgia.
At the final stage, characteristic phenomena are urinary incontinence and spontaneous defecation.
Diagnostics
To make a diagnosis and determine the extent of brain damage in the presence of clinical signs of the disease, the following is carried out:
- computed tomography;
- rheoencephalography;
- Doppler ultrasound.
Laboratory blood tests are used to confirm the diagnosis.
Encephalopathy stage 2 of mixed origin
Grade 2 encephalopathy is the destruction of neurons in the brain. Previously, the disease was diagnosed only in old people, but today it occurs in 40-year-olds. Elimination of the symptoms of the disorder causes deterioration in performance and a decrease in quality of life. Preliminary diagnosis makes it possible to reduce the likelihood of negative consequences.
Stages of the disease
Stages of dyscirculatory encephalopathy:
- Organic transformations of the nervous system are mild, but symptoms are already arising. Signs of disorders are sometimes confused with the clinical picture of several lesions of the central nervous system. Often these are fatigue, deterioration of concentration and memory, tinnitus, migraines, sleep problems, nervousness, and apathy.
- A progressive disease has more pronounced symptoms. The deterioration of the nervous system is obvious. The patient manages to take care of himself without assistance. Doctors often try to distinguish between the first and second degrees. The disorder is diagnosed if symptoms persist for 6 months.
- Time for irreversible serious transformations. It is difficult for the patient to take care of himself, he behaves inappropriately, and there is a threat to the health and life of him and those around him. The patient is assigned disability status; treatment does not relieve symptoms, but helps prolong life.
The duration of the illness, individual characteristics and the nature of the assistance provided depend on the stage of the disease.
Symptoms
The disease does not have the same symptoms. Many signs at the first stage are the same as in other types of pathologies. Therefore, it is not easy to make a forecast.
- Nervous disorders at stage 2. On the 1st they do not appear.
- Memory problems.
- Apathy, lethargy.
- My head hurts.
- Poor concentration.
- It's difficult to remember a lot of information.
- Nausea, dizzy.
It should be borne in mind that symptoms begin in the evening after a long day or difficult exercise. If the duration of such symptoms corresponds to 6 months. This means stage 2 of the disease is developing. The therapeutic method is determined after diagnosis.
How to treat without drugs?
The patient must strictly adhere to:
- Diet.
- Do not smoke or drink alcohol.
- Normalize your own weight.
- Get more physical activity.
Elimination of such a disease involves surgical intervention. The procedure is performed when 70% of the blood supply to the head is damaged.
Fill a liter jar with dried clover, add grass so that the mixture does not reach 5 cm from the top. The container is filled with alcohol, the mixture is infused for 2 weeks in a dark place. After this, strain the contents, consume 1 teaspoon 3 times a day. It is advisable to drink it with cold water. It is better to use such remedies on the recommendation of a doctor.
Stage 2 disability
The 3rd category of disability is assigned to patients with encephalopathy who are able to perform basic activities at home or at work with difficulty. Living with such a disease is possible without regular monitoring by doctors or relatives. Each individual situation requires personal consideration.
The second category is assigned to patients with other disorders other than cephalgic syndrome. Due to memory problems and limb tremors, they cannot maintain their ability to work. Patients can take care of themselves.
Treatment
A frequent question from patients: how long can you live with discirculatory encephalopathy of degrees 1, 2, 3? At the initial stage, the disease can be overcome provided that comprehensive treatment is performed, selected exclusively on an individual basis. In the final phase of the pathology, brain atrophy and impaired blood flow are clearly expressed, but consistent and long-term use of powerful modern drugs from different groups can prolong a person’s life.
- ACE inhibitors;
- calcium antagonists;
- diuretics;
- beta blockers;
- alpha1-adrenergic receptor blockers;
- antihypertensive medications;
- lipid-lowering drugs;
- antihypoxants;
- nootropics;
- preparations based on nicotinic acid.
Prevention
The main goal of preventive measures for dyscirculatory encephalopathy is to eliminate the causes of deterioration in brain activity. Even from adolescence, it is necessary to pay attention to maintaining vascular health:
- observe the work and rest schedule;
- adhere to a special diet;
- take vitamin preparations for preventive purposes;
- perform gymnastic exercises;
- pay attention to physical fitness;
- regularly spend time in the fresh air;
resort to massage and physiotherapeutic procedures.
This disease is treated by the following specialties of doctors: neurologist. neurologist (neurologist).
Looking for a doctor? Sign up right now, quickly and conveniently.
Select and make an appointment with a doctor from our rating below.
Second stage of the disease
Symptoms of discirculatory encephalopathy at the initial stage are hardly noticeable, since the function of dead cells is taken over by nearby neurons. In this case, minor signs appear that are not clearly expressed:
- headaches with a feeling of fullness;
- dizziness;
- memory loss;
- noises in the head;
- irritability;
- emotional instability.
At this stage of the disease, with timely treatment, remission for decades is possible, and in some cases, complete recovery.
When decompensation occurs and the lesions become significant, in addition the following symptoms begin to appear:
- lack of control over one's own movements;
- inhibited articulation, the person seems to forget how to speak.
Stage 2 of the disease develops, which can also manifest itself in various variants of psychopathological syndromes:
- asthenodepressive;
- asthenohypochondriacal;
- paranoid;
- affective.
The cephalgic syndrome becomes especially pronounced, in which severe headaches are felt, often vomiting and nausea. The patient may experience sudden changes in mood due to loss of communication between neurons in the brain. Speech becomes sluggish, and the patient does not always remember what he is talking about.
At this stage of the disease, disability is already assumed, although the person is still able to take care of himself and does not lose cause-and-effect relationships.
Encephalopathy
Discirculatory encephalopathy is a painful condition caused by insufficient blood flow in the brain area. Gradually leads to deviations in brain functioning, and can also cause the development of disorders of the brain structure that are diffuse in nature. The progression of the disease is slow, development lasts more than one year. The main characteristic is multifocal dysfunction of the brain.
Causes
Discircular encephalopathy of the brain does not develop as an independent disease. Its development is influenced by certain conditions of the body, namely:
- development of atherosclerosis in the vessels of the brain;
- progress of arterial hypertension;
- congestion in the cerebral vessels of a venous nature;
- development of vegetative-vascular dystonia;
- deviations of systemic hemodynamics;
- pathogenic processes in connective tissues of a systematic nature;
- development of vasculitis;
- progress of blood diseases.
In most cases, discircular encephalopathy (DE) develops due to the progress of combinations of atherosclerosis and arterial hypertension. The processes and diseases mentioned above are the causes of impaired blood circulation in the brain area, provoking oxygen starvation, microinfarctions, and changes in the density of the white brain matter. Such deviations in the functioning of the brain lead to mental disorders in humans and develop neuralgic symptoms of a microfocal nature.
Symptoms
Quite often, the symptomatic picture of this disease during the early stages of its course is not specific. The first sign indicating dyscirculatory encephalopathy syndrome is the development of asthenia. It is characterized by feelings of fatigue, irritability, and impaired ability to concentrate. Mood variability is also common, with most cases resulting in depressed mood and an increased level of reaction to external stimuli.
Over time, neuropsychiatric disorders of organic origin, as well as deviations in the functioning of motivation, attention, memory and emotions, are added to the symptomatic picture. In addition, there is insomnia, headaches, a feeling of dizziness and noise in the head. Symptoms tend to increase during the second half of the day during the processes of mental and physical labor.
Degrees
The course of the disease is staged. Experts have identified three stages of the disease.
- Discirculatory encephalopathy of the 1st degree manifests itself through a syndrome of a neurasthenic nature with a subsequent decrease in the patient’s performance. This stage is also characterized by dizziness, insomnia, noise in the head, and headaches. Objectively, one can attest to varying degrees of severity of reflexes on the patient’s face or the occurrence of reflexes that are pathological in nature. However, the occurrence of such signs is not mandatory. Quite often, they can be of an accompanying nature during processes of deviation of blood circulation in the brain, for example, during a transient ischemic attack.
- Discirculatory encephalopathy of the 2nd degree has a fairly similar symptomatic picture of the disease. Progression of existing symptoms is observed. Brain damage that is organic in nature is more pronounced. There may be deviations in the coordination of the patient's movements, paralysis of the limbs, paresis, tendon reflexes become more active, and pathological type reflexes occur. Examination of the fundus shows dilated veins, narrowed arteries, and the development of angiosclerosis.
- Discirculatory encephalopathy of the 3rd degree is characterized by the obligatory obvious progression of syndromes of a neurological nature, for example, pyramidal, amyostatic, pseudoboulevard and others. Epileptimorphic seizures also develop. Stable symptoms include headache, decreased memory, insomnia, noise in the head, and impaired coordination of movements. Among other things, there is the development of dcoenemia and a decrease in the patient’s level of intelligence.
Causes of DEP 2nd degree
The mechanism of development of the disease is based on deterioration of blood flow in the brain, which leads to oxygen starvation and irreversible changes in the structures of the organ. The causes of dyscirculatory encephalopathy include:
- dysfunction of the arteries (atherosclerosis);
- arterial hypertension;
- vegetative-vascular dystonia;
- stagnation of blood in the vessels due to inflammation, injury or other factors;
- osteochondrosis of the cervical spine, which causes pinched nerves and vascular spasm;
- deposition of cholesterol on the walls of blood vessels;
- toxic damage to the body by bacteria (with bark, botulism and other ailments), exposure to chemicals;
- diseases of connective tissue, hematopoietic system.
In addition, alcohol abuse, improper treatment of certain diseases, and constant mental stress can lead to the development of the disease.
The most common cause of DEP is atherosclerosis, especially in cases where it is accompanied by surges in blood pressure and constant stress.
Encephalopathy
Signs of discirculatory encephalopathy increase gradually.
Discirculatory encephalopathy is a very common disease in middle-aged and older people. The main reason for the development of dyscirculatory encephalopathy is vascular damage. Without the results of a thorough examination, one cannot say that a person has dyscirculatory encephalopathy. With age, the risk of developing discirculatory encephalopathy increases several times. This disease is one of the main causes of senile dementia. Unlike a stroke, when only one part of the brain is destroyed, with dyscirculatory encephalopathy there are many micro-strokes. This leads to the fact that several functions are disrupted at the same time.
Signs and manifestations of dyscirculatory encephalopathy
The nervous tissue in this place swells, ceases to perform its functions and is destroyed. At first, the disease manifests itself as headache, weakness and decreased performance. It occurs after 45 years and half of patients have not yet reached retirement age. Often these are people of mental work and creative professions. Their brains work hard, but they lack physical activity.
How long do people live with dyscirculatory encephalopathy?
Over the past ten years, the number of patients has doubled. It is believed that the number of people who have this disease is more than 6% of the total population of the planet. The disease can be caused by unsuccessful treatment by massage therapists and chiropractors, injuries to the spine and head. This is because a thorough examination must first be carried out. In addition, they must be examined using special psychological tests that identify disorders of memory, thinking and emotions.
If you notice signs of this disease, do not rush to get upset. The brain is a complex mechanism that is constantly evolving and finding workarounds to perform its functions despite the affected areas.
Let's figure out what processes occur in the brain and lead to the development of the disease. The brain needs a constant flow of blood to bring it oxygen and nutrients. Nutrition for each nerve cell (neuron) is provided by many large vessels and small capillaries. The capillary does not bring enough blood to some part of the brain. At this point the vessel wall begins to work poorly. It allows excess fluid to enter the brain tissue.
They starve and die. The patient becomes unable to concentrate on anything. Over time, other vessels become blocked and new foci of necrosis appear. Therefore, with this disease, disorders in coordination of movements, memory, and thinking are simultaneously noticeable; behavior also changes and the person is constantly in a depressed mood.
What is the prognosis for dyscirculatory encephalopathy?
Capillaries stop delivering enough blood to different parts of the brain. Let's figure out why this happens. Atherosclerosis is a disease in which a blood vessel becomes clogged with cholesterol plaques.
High blood pressure (arterial hypertension) causes the blood vessel to close or burst. In this case, brain tissue is saturated with blood or plasma. Increased blood viscosity and it circulates poorly through narrow capillaries and stagnates in them. Platelets stick together and form blood clots.
With this disease, the vessels are not sufficiently filled with blood; it moves slowly through the capillaries. Spinal and brain injuries. Their result can be hematomas - areas filled with stagnant blood.
Congenital characteristics of the body (angiodysplasia, anomalies in the development of arteries and veins) can cause the vessels to not work well enough. Especially in the brain. In long-term smokers, the blood vessels become spasmodic and no longer expand to their normal size. But over time, the destruction in the brain becomes more extensive, and the manifestations of the disease become more noticeable.
The white matter (subcortical layer of the brain) contains centers for processing information that comes from the environment and from the senses, centers for sleep and daytime activity, and emotions. In the cortex there are centers responsible for higher mental activity, which only humans have.
Do a diagnosis of dyscirculatory encephalopathy give you disability?
She becomes shaky and unstable. Pyramidal disorders cause muscle paralysis on one side of the body, muscle spasms, and tendon tension. The cerebral cortex and its deep subcortical structures can no longer work coherently. The cortical-nuclear pathways through which the signal passes from the brain to the muscles of the head and neck are disrupted. As a result, symptoms of oral automatism appear. These are involuntary movements of the mouth that occur in response to irritation of different areas of the skin. The voice also becomes dull and nasal, and swallowing becomes difficult.
At-risk groups
The risk group for the development of discirculatory encephalopathy includes people aged 35 to 55 years, and representatives of the Caucasian race are more prone to it than everyone else.
After 70 years, the likelihood of getting sick and becoming disabled increases several times.
Most patients with DEP are people whose professional activities involve mental work, when the brain is constantly under stress and there is no physical activity. In addition, those who suffer from diabetes, alcoholism and neurological disorders are prone to developing the disease.
Encephalopathy is damage to the blood vessels of the brain. Discirculatory encephalopathy of the 3rd degree leads to severe disorders.
You will learn everything about the treatment of toxic encephalopathy from this article.
You will find an overview of traditional methods of treating cerebral encephalopathy here.
Development of grade 3 encephalopathy
The brain needs oxygen and nutrients more than other organs. Poor cerebral circulation occurs due to vasoconstriction, blockage by plaque or compression. The brain is supplied by the carotid and vertebral arteries. In addition to the main vessels, there are smaller ones (arterioles, capillaries).
Encephalopathy is a pathological condition characterized by chronic cerebral ischemia and the formation of small foci of tissue necrosis. This condition progresses very slowly. Stage 3 DEP can develop several decades after the onset of hemodynamic disorders.
Most often, older people get sick. This is not an independent disease. In more than half of the cases, encephalopathy develops in people with atherosclerosis of the vessels supplying the brain. The prevalence of encephalopathy is more than 6%. Stage 3 encephalopathy is one of the main causes of dementia in older people. This condition, along with stroke, is classified as a vascular neurological pathology.
Risk of disability: statistics
Discirculatory encephalopathy today is one of the main causes of disability and sometimes death.
The issue of obtaining disability and the group is decided in each case individually, depending on the severity of symptoms and the general condition of the patient.
- Usually, with DEP of the 2nd degree, a third disability group is given - in such cases, the quality of life at the everyday level does not deteriorate, but fulfilling work duties is difficult.
- The second group is given to people suffering from dyscirculatory encephalopathy of 2 or 3 degrees, accompanied by impairments, memory loss and loss of ability to work.
- The first disability group is assigned to a person when the disease has reached the most serious, third stage.
According to statistics, at a young age (25-45 years), the disease progresses quickly, but responds well to treatment, and after 60 years, disability occurs in 70-80% of cases.
Causes of the disease
Chronic oxygen deficiency is due to several reasons. The main etiological factors are:
- atherosclerosis;
- osteochondrosis;
- systemic vasculitis;
- diabetic angiopathy;
- hypertonic disease;
- secondary arterial hypertension;
- low pressure;
- blockage of blood vessels by blood clots;
- spinal injuries in the cervical region;
- traumatic brain injuries;
- congenital developmental anomalies;
- diseases of the endocrine glands;
- thrombophlebitis;
- hormonal disorders;
- chronic heart failure;
- renal pathology;
- tumor of the adrenal medulla;
- Itsenko-Cushing syndrome;
- spinal instability;
- heart rhythm disturbance;
- Kimerli anomaly.
Increase the risk of developing this pathology:
- smoking;
- alcoholism;
- violation of fat metabolism;
- overweight;
- physical inactivity;
- intense mental work;
- non-compliance with sleep and wakefulness;
- regular stress;
- overwork.
Atherosclerosis plays a leading role in disrupting the blood supply to the brain. With this disease, the patency of blood vessels is impaired. Atherosclerotic plaques appear that cannot be removed even with the most modern medications. Encephalopathy of the 3rd degree of severity develops in people who self-medicate or do not consult a specialist. It all starts from the 1st stage. Over the years, the disease progresses, and the person’s condition worsens.
Encephalopathy differs from stroke in the many small infarcts. They occur at sites where brain cells die. The temporal and frontal areas are most often affected. The functioning of the cerebral cortex and subcortical structures is disrupted. There are various centers that regulate vital functions. Against the background of chronic hypoxia, edema occurs. The reason is increased vascular permeability. Against the background of hypoxia, signal transmission is disrupted.
Kinds
Discirculatory encephalopathy most often occurs as an acquired disease, but cases of congenital pathology are possible. The latter is caused by unfavorable factors accompanying pregnancy and childbirth.
The speed of onset of symptoms allows us to talk about slowly progressing, remitting and rapidly progressing pathology. The duration of the first is measured in years. It may take 15 years between the appearance of the first symptoms and disability.
Remitting dyscirculatory encephalopathy leads to a faster deterioration of the patient's condition. Its peculiarity is the alternation of periods of exacerbation and normalization of the condition. Typically, persistent, permanent defects occur within 10 years.
The galloping (rapidly developing) form can lead to disability or even death within 2-3 years.
Depending on the leading cause, the following types of discirculatory encephalopathy are distinguished:
- Atherosclerotic. It develops due to the appearance of protein and lipid compounds on the walls of blood vessels. They reduce the lumen of blood vessels, thereby reducing the volume of circulating blood. The main highways that provide blood flow to the brain and regulate its volume are damaged.
- Venous. The main cause of the disease is a violation of the outflow of venous blood. Stagnation occurs, poisoning the brain with toxins and causing inflammation.
- Hypertensive. Associated with spasms, thickening and rupture of the walls of blood vessels. The disease progresses rapidly. It can develop in young people. The acute form of the disease occurs immediately following an increase in pressure and can be accompanied by epileptic seizures and agitation. In a chronic course, there is gradual damage to small vessels.
- Mixed. This form contains signs of hypertensive and atherosclerotic forms. A decrease in blood flow through the main vessels is accompanied by hypertensive crises.
In some cases, encephalopathy of combined genesis is isolated. The disease develops when the blood supply is disrupted, toxic exposure or injury.
Clinical signs of the disease
Symptoms of grade 3 encephalopathy are quite specific. The main clinical signs are:
- aggressiveness;
- conflict;
- hearing loss;
- blurred vision;
- presence of spots before the eyes;
- unsteady gait;
- loss of interest in life and hobbies;
- paresis;
- paralysis;
- thinking disorder;
- apathy;
- lack of motivation;
- indifference to current events;
- decreased intelligence;
- voice change;
- slurred speech.
People with stage 3 encephalopathy are unable to work or carry out daily activities.
They need care. Such people are not aware of the disease and do not make any complaints about feeling unwell. Habitual mental work becomes overwhelming. Such people most often do nothing. A personality disorder occurs. Brain hypoxia causes praxis impairment. Slowness and unsteadiness of gait are observed. The steps become small. Shuffling is often observed. It is very difficult for patients to start moving forward and suddenly stop. Encephalopathy of the 3rd degree in its course resembles Parkinson's disease.
Along with impaired coordination of movements, tremors, urinary incontinence, headache, nausea, vomiting and epileptic seizures are possible. Sometimes pseudobulbar syndrome occurs. It manifests as dysphagia (difficulty swallowing food), dysarthria (speech disturbance) and dysphonia (change in voice). When dementia develops, a person cannot count, write, remember information, speak or read normally. Characterized by severe memory impairment and decreased intelligence.
Symptoms and main emerging syndromes
Sometimes it is very difficult to determine the symptoms of stage 2 DEP, since they can also be characteristic of other diseases associated with circulatory or brain dysfunction.
The main features include:
- memory problems;
- nausea;
- vomit;
- dizziness;
- loss of consciousness;
- sclerosis;
- loss of coordination;
- decreased concentration, problems with thinking;
- nervousness;
- mental or emotional disorders;
- dilatation of veins in the fundus.
The main syndromes of grade 2 DEP are distinguished:
- Cephalgic syndrome, which manifests itself in headaches, vomiting, and tinnitus.
- Dissomnia syndrome includes various types of problems associated with sleep disturbances.
- Vistibular-coordinating syndrome, it in turn concerns problems that are associated with the position of the body in space, when walking, dizziness and coordination in general.
- Cognitive syndrome, which includes problems with memory, thinking, concentration and much more.
It is worth mentioning that these symptoms of grade 2 discirculatory encephalopathy appear in the late afternoon, due to the moral and physical stress to which the body was subjected during the day.
What is hyperventilation syndrome or why there is not enough air - you can find out from our article. What you need to do if you suffer from a nervous tic of the eye - treatment methods and psychological influence. Why does eye trembling occur?
Often in patients with dyscirculatory encephalopathy, symptoms are combined into syndromes. In the second degree, 4 main syndromes can be observed:
- Cephalgic. It is characterized by intense pain in the head, accompanied by tinnitus and nausea.
- Vestibulo-atactic. Consists of impaired coordination of movement in space, dizziness, unsteadiness when walking, instability.
- Dissomnic. Presented with sleep-related disorders and biorhythms. There is severe daytime sleepiness and at the same time the inability to fall asleep at night, frequent waking up, and difficulty getting up in the morning.
- Cognitive. A person loses the ability to remember information, his thought process is disrupted, and it becomes difficult to concentrate on anything.
As the disorders progress, nervousness, irritability, and aggressiveness appear. Fainting, mental abnormalities, and emotional disorders are possible.
Examination and treatment tactics
You need to know not only the symptoms of grade 3 encephalopathy, what it is, but also how to make a diagnosis. For this you will need:
- electroencephalography;
- Doppler ultrasound of cerebral vessels;
- magnetic resonance or computed tomography;
- complete neurological examination;
- interviewing the patient and his relatives;
- physical examination;
- radiography;
- Ultrasound;
- duplex scanning;
- electrocardiography;
- angiography with contrast agent;
- perimetry;
- ophthalmoscopy;
- visual acuity test;
- blood pressure measurement;
- coagulogram;
- lipid profile;
- general and biochemical blood tests;
- general urine analysis.
Treatment is carried out after excluding meningitis, encephalitis, multiple sclerosis, encephalomyelitis, strokes and hypertensive crisis. Patients with encephalopathy of mixed origin require complex therapy. The main aspects of treatment are:
- neuroprotection;
- normalization of blood pressure;
- treatment of diseases leading to brain hypoxia;
- prevention of complications.
For encephalopathy due to atherosclerosis, statins are indicated. These are drugs that normalize the lipid spectrum. Medicines must be taken constantly, otherwise the plaques will increase in size. This is fraught with a stroke. Statins include Torvacard, Atorvastatin-Teva, Aterostat, Simvor and Vero-Lovastatin. For high blood pressure, beta-blockers or ACE inhibitors are indicated.
To prevent thrombosis, antiplatelet agents (Ticlopidine-Ratiopharm, Clopidogrel) and anticoagulants are used. In order to dilate blood vessels and improve blood supply to the brain, calcium channel blockers (Nimotop) are often prescribed. Additionally, you need to drink vitamins and take cofactors. To prevent disability from occurring, neuroprotectors are prescribed.
These include vascular drugs, adaptogens, antioxidants and nootropics. The most commonly used are Gemfibrozil, Cavinton, Semax, Ginkgo Biloba, Piracetam, Glycine, Cerebrolysin, Trental, Pentoxifylline, Mexidol and Eleutherococcus tincture. If you have encephalopathy, you need to stick to a diet, control your blood sugar levels, body weight, and move more. Relaxation in a sanatorium, physiotherapy and neck massage are recommended. In severe cases, surgery is required.
Prevention of DEP 2nd degree
To prevent the development of dyscirculatory encephalopathy, it is necessary to treat cardiovascular diseases in a timely manner, monitor blood pressure and cholesterol levels in the blood.
An important role is played by a correct lifestyle, giving up bad habits and the ability to cope with stress (for this you can use breathing exercises, psychotherapeutic techniques, yoga).
People who are at risk need to carefully monitor their psycho-emotional state and visit a neurologist once a year.
Discirculatory encephalopathy is a dangerous disease that can lead to serious complications and consequences. With timely diagnosis, proper treatment and adherence to preventive measures, the progression of DEP symptoms can be significantly slowed down or even stopped.
What are we talking about?
With dyscirculatory encephalopathy changes, cerebral vessels are affected, and brain damage is irreversible. This pathological condition is chronic and progresses over time. Symptoms of the disease appear due to poor oxygen saturation of the brain and nutrition, which will lead to hypoxic, edematous and necrotic changes in the cellular structures of the brain.
Dyscirculatory encephalopathic changes affect vessels of different sizes. This disease is observed in 6% of people on the planet; it usually affects old people, but increasingly, symptoms appear in young people.
Discirculatory encephalopathy of the third degree is of great danger. With dyscirculatory encephalopathy of the 3rd degree, how long can you live?
The outcome of the pathology is unfavorable, so none of the doctors will give an exact or approximate answer to this question.
Dyscirculatory encephalopathy processes are formed as a result of pathological changes in cerebral vascular tissues. The root causes are of mixed origin, usually they are other pathologies of the body:
- Hypertensive processes, characterized by abrupt changes in blood pressure, which negatively affect blood vessels. They become less elastic and small cracks form in them. Through these cracks, blood or its components penetrate into the brain tissue. This liquor gradually accumulates, and the trophic processes of the brain are disrupted.
- Hypotonic processes. With hypotension, insufficient blood flows to the brain, resulting in nutrient deficiency and cerebral hypoxia.
- Atherosclerotic changes. The vascular lumen is blocked by plaques, which include cholesterol. The amount of blood supplied to the brain with oxygen and nutrients will decrease.
- Osteochondrotic changes. Osteochondrosis causes discomfort to a person; the spinal column loses its natural flexibility. The vertebral arterial vessel is compressed, which leads to worse blood supply to the brain.
- High blood density, leading to thrombosis. A segment of the brain that does not receive blood flow due to the closure of a vessel by a blood clot dies over time.
- Vascular pathologies (VSD, thrombophlebitis changes).
- Inherited abnormal conditions that have a destructive effect on vascular tissue.
- TBI and spinal column injuries also cause vascular disorders.
- Disturbances of the endocrine system. Hormonal compounds synthesize various substances beneficial to the body, including elastin and collagen protein components. Deficiency of these substances leads to destruction of vascular walls. This root cause causes dyscirculatory encephalopathy in women during menopause.
Prognosis and prevention
With DEP 1, the prognosis is favorable. The progression of the disease is unlikely to be stopped, but it is possible to reduce the severity of symptoms and lead a full life. To do this, it is important to maintain a healthy lifestyle and adhere to medical recommendations.
When the disease moves to the second stage, recovery can only be said if the cause that caused it can be eliminated surgically. Otherwise, the disease progresses. Gradually the patient's condition will worsen and lead to disability. Timely comprehensive treatment of DEP 2 allows you to delay the appearance of signs of the third stage for up to 10 years.
Discirculatory encephalopathy is a complex disease that destroys the emotional, cognitive and motor spheres of human life. The prognosis can be favorable with early detection of pathology, its treatment and prevention. Pronounced symptoms indicate an organic lesion and are difficult to treat.
The prognosis of dyscirculatory encephalopathy of the second degree depends on several factors: how quickly the disease progresses, the degree of brain damage, the presence of concomitant diseases and the development of consequences. The main point that determines the possibility of stopping the pathology is the desire of the patient himself and his willingness to change his lifestyle and follow the doctor’s recommendations.
Remission in grade 2 DEP can occur with timely consultation with a specialist and a competent approach to therapy. The third stage of the disease is not amenable to therapeutic intervention, therefore, for a patient with the second stage of DEP, the main task is to stop the pathological processes in the brain.
Many patients are interested in the question of how long they live with stage 2 DEP. Without therapy and with rapid progression of the disease, the presence of concomitant chronic decompensated diseases, life expectancy is significantly reduced. This is associated with a high risk of possible stroke and myocardial infarction. At the same time, by changing your lifestyle and listening to the recommendations of your doctor, you can extend your life for many more years.
How are they classified?
There are the following types of discirculatory encephalopathies, based on the root causes of the formation of the pathological process:
- Atherosclerotic form of DEP. A common type of encephalopathy. Affects large cerebral vessels.
- Venous form. The functioning of the venous vessels is impaired. Venous outflow is slow. There is stagnation in the brain tissue, leading to edematous changes.
- Hypertensive form. It affects young people and leads to sudden changes in blood pressure. If blood pressure is elevated, the patient’s well-being worsens; accordingly, when blood pressure decreases, the patient’s condition normalizes. But this happens with the primary manifestations of the pathology; over time, the patient’s condition will worsen.
- Encephalopathy of mixed origin. Treatment of this form is problematic. Venous and arterial vessels are involved in the pathological process. Constantly occurring spasmodic changes in blood pressure aggravate the patient's condition. The third stage of dyscirculatory encephalopathy guarantees a negative outcome for the patient due to the dominance of neurological disorders.
Dyscirculatory encephalopathic changes from stages 1 to 3 develop both in a matter of months and in a couple of years. Sometimes the progress of the pathological process stops at some stage. This often happens with a correct diagnosis in the initial stages of the disease, and also if appropriate treatment has been carried out.
It is impossible to completely cure this pathology.
Symptoms
The second degree of DEP is accompanied by a number of neurological defects, in particular:
- Dizziness.
- Constant headaches.
- Noise in ears.
- Fatigue and lethargy.
- Drowsiness and insomnia.
- Mood swings, tearfulness.
- Visual impairment (including glaucoma) and hearing, the diagnosis of “DEP 2 degrees” and glaucoma are often interrelated.
- Poor gestures and facial expressions, unclear speech.
- Impaired fine motor skills of the hands (for example, it is difficult for the patient to thread a needle) and coordination (the gait becomes unsteady), slow movements;
- Poor time orientation and forgetfulness.
- In some cases - convulsive attacks.
About the stages of pathology development
The stages of dyscirculatory encephalopathy depend on how the symptoms manifest:
- At the beginning of the disease, the patient feels that he can work less than usual, his mood often changes, and his sleep is disturbed. Symptoms do not appear in the first degree.
- For the second degree, clinical manifestations become more obvious. Pathological changes of a neurological nature are observed. During an examination of a patient, a neurologist notes the presence of mental abnormalities and instability of the patient’s emotions.
- In the third degree of dyscirculatory encephalopathy, neurological symptoms manifest themselves most clearly. The patient has an unstable psyche, he is aggressive, his movements are not coordinated. Sometimes vision and sensitivity are impaired. The patient has an abnormal mental state, he is inhibited, and loses consciousness.
In the third stage, the patient develops dementia due to vascular changes. Symptoms worsen, seizures are expressed. The patient is not able to care for himself; he must be constantly monitored and cared for. His life is dependent on loved ones.
The patient urinates in his pants, his movements are uncoordinated, he becomes weak-minded. In this state he is unable to learn. The patient becomes disabled, and if the condition is very severe, he dies.
When the structure of capillary vessels is disrupted, microstroke changes appear. In this case, the center of thinking suffers. The patient is unable to concentrate on certain actions, he remembers poorly, and it is difficult for him to imagine the consequences of his actions.
When the brain substance of the frontal segment is damaged, the patient’s unstable emotional state is observed. He becomes depressed, indifferent, hysterical, apathetic, and displays of aggression are also observed.
Impulses from neurons to internal organs are transmitted incorrectly. Coordination of motor activity is impaired, the patient has a staggering gait. Tendon and muscle tissues are in a spasmodic state.
Due to the clinical manifestations of grade 3 dyscirculatory encephalopathy, the patient becomes incapacitated. If the occipital area is affected, then visual function is impaired. In some cases, there is a nasal voice; the patient also opens his mouth when a certain area of the body is irritated; the patient may find it difficult to swallow.
Disability with a diagnosis of “DEP 2nd degree”
The third disability group is assigned to patients who are capable of self-care and performing certain professional activities. At the same time, constant monitoring from relatives and specialists is not required. The second group is given to patients suffering from problems with memory and concentration, severe headaches and tremors of the limbs. The quality of life deteriorates, but the ability to self-care is preserved.
Symptoms may improve during treatment, resulting in a person’s quality of life improving. If the necessary therapy is not available, the signs continue to progress, more and more new symptoms are added to them, and then the pathology develops into the third stage.
Among the expected complications is ischemic stroke, which can develop at any stage of the disease with a diagnosis of “DEP of the 2nd degree of mixed origin.”
At the second stage of the disease, many patients may already be assigned a disability. The group will depend on the severity of the symptoms.
The third group is assigned when diagnosed with DEP stage 2. Its symptoms are so pronounced that they interfere with ability to work. But the patient has not yet lost the ability to self-care; he rarely needs outside help in everyday life.
The second group is assigned to the third degree of DEP. Symptoms suddenly limit a person's ability to live. As a result of his illness, he had already suffered a mini-stroke.
So, we explained that this is a diagnosis of “DEP of the 2nd degree”.
About treatment
Treatment is aimed at eliminating the underlying pathological process, eliminating affected areas of the brain, restoring brain activity, and preventing hypoxic changes. Treatment of dyscirculatory encephalopathy manifestations is complex. To eliminate the pathological process and restore the cellular structures of the brain, it is necessary to strictly follow all medical prescriptions.
A diet is prescribed that limits salty and fatty foods. Taking vitamin supplements is mandatory. The patient requires psychotherapeutic help.
It is easier for the patient to recover if he engages in activities that are easy for him to carry out. This is the only way he realizes that he has a chance of recovery.
Medication therapy
The patient is prescribed treatment with several medications. As a rule, they treat:
- Lisinopril, which lowers blood pressure, provided that the cause of dyscirculatory encephalopathy is hypertension.
- Aspirin (acetylsalicylic acid). With its help, the blood will become more liquid, platelets will not stick together, and vascular blockage will be eliminated.
- Chimes. This remedy will help increase the capillary lumen and strengthen the walls of these vessels.
- Nimodipine. This drug blocks the flow of calcium into muscle tissue, muscles relax, and blood supply improves. As a result, the patient’s motor activity and mental function are normalized.
- Atenol. The product removes excess fluid, normalizes cardiac activity, increases blood flow, and decreases blood pressure.
- Vasobram. The drug protects cerebral cellular structures, prevents thrombus formation, and improves metabolic processes in the subcortical medulla.
- Ginseng tincture. This natural drug will increase performance, improve brain activity, vascular and heart function. It will reduce blood cholesterol levels, and the patient will also be less tired. But it is worth remembering that in case of hypertension, this remedy is prohibited.
If treatment with medications does not bring a pronounced effect, then surgical intervention is used on large cerebral vessels.
Diagnostics
The diagnosis is made after studying the symptoms. The same diagnostics are performed to determine the cause of circulatory problems in the nervous system.
For this we use:
- Blood test to study atherosclerosis.
- Assessment of the condition of the fundus veins.
- Duplex scanning.
- MRI.
- Angiography.
- For hypertension, a blood urea test is performed.
- ECG, ultrasound of the heart.