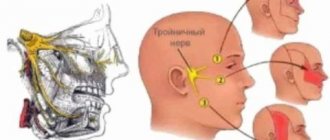
Anatomical features of N. trigeminus
The nerve roots begin from the anterior zone of the pons, located near the intermediate cerebellar peduncles. The motor root connects to another nerve and, together with it, exits the cranial cavity through the oval window.
The trigeminal nerve is part of the autonomic ganglion, from which sensory branches arise. They are responsible for ensuring the sensitivity of the skin and underlying layers.
The anatomy of the trigeminal nerve and its branches consists of structures:
- Mandibular root;
- Orbital root;
- Nerve ganglion of the corresponding nerve;
- Maxillary nerve;
The skin of the facial area, oral mucosa, eyelid and nose is innervated by these structures, which is very important for a normal and comfortable life. The semilunar ganglion consists of typical nerve cells found in the spinal cord and other nodal structures.
Remember that absolutely all ramifications, namely:
- First branch of the trigeminal nerve (orbital);
- Second branch of the trigeminal nerve (maxillary nerve);
- Third branch of the trigeminal nerve (mandibular nerve);
They are protected by the cells of the dura mater, which has a positive effect on their normal functioning. It is important to know the trigeminal nerve circuit in order to clearly differentiate the damaged branch and begin appropriate treatment.
Trigeminal nerve diseases
What processes influence the functional ability of this formation, and how can the trigeminal nerve be affected?
The anatomy of its course predisposes to the development of channelopathies - infringement of the branches of the nerve passing through the canal or opening by surrounding formations. In this case, knowledge of the topography of the nerve and some topical signs allows us to determine the level of its damage and take appropriate measures.
Another equally important factor is the influence of surrounding tissues. Most often, nerves are affected by brain tumors. As they grow, they contribute to its compression and the appearance of the corresponding clinical picture.
The anatomy of the trigeminal nerve (knowledge of its branches and the places of its projection onto the face) allows you to determine the exit points of the nerve branches and stimulate them using electrophysiological methods, or, taking into account the location of the branches, carry out appropriate treatment of the underlying disease that led to the appearance of pathological symptoms.
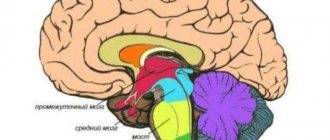
Location of nerve structures
This nerve has 4 nuclei (two motor and sensory), three of them are located in the posterior parts of the GM, and 1 is located in the middle. A feature of the trigeminal nerve is the presence near the branches of the autonomic cranial ganglia, on the structures of which the parasympathetic branches from the III, VII and IX pairs of the CN end. Postganglionic branches connect to the branches of the nerve and reach their target within them.
This nerve is formed by the fusion of two structures - the deep ophthalmic structures, which innervate the skin in front of the head, and the trigeminal nerve itself, which innervates the region of the mandibular arches.
Maxillary nerve
The maxillary nerve, by analogy with the orbital nerve, is sensitive and ensures the transmission of impulses to the brain, as well as back. This area has a complex organization. It is divided into a number of large branches. Together, they are responsible for the sensitivity of the middle part of the face, including the nose, cheekbones, and upper jaw.
The main structural elements of this section of the system are:
- middle meningeal branch;
- orbital branches;
- posterior superior nasal branches;
- palatine branch;
- zygomatic branch;
- branches of the infraorbital nerve.
Each minor branch from the central axis has its own additional processes.
Due to this structure, the maxillary nerve covers a large area of muscle and skin.
During the inflammatory process in the trigeminal nerve, its motor function is disrupted. Trigeminal nerve - treatment at home and precautions, read on our website.
Read on for methods to relieve inflammation of the trigeminal nerve.
The main methods of treating the trigeminal nerve are drug therapy and surgery. The latter is used if medications do not help relieve pain. Here you will find an overview of all methods of treating the inflammatory process.
Features of branches
As has been mentioned more than once, the trigeminal nerve has branches. The optic nerve is the first part of the nerve. It performs the sensitive functions of the eyeballs, lacrimal glands, lacrimal sacs, mucous membranes of the ethmoidal labyrinths, frontal and sphenoid sinuses, upper eyelids, glabella, dorsum of the nose, and frontal zone. Thus, it innervates all structures that are located above the palpebral fissures.
The orbital nerve is sensitive. It originates from the Gasserian ganglion, entering the cavernous sinuses, and upon exiting them it gives rise to the nerve of the tentorium of the cerebellum, and then through the superior orbital fissures it goes into the orbit, where it is divided into three parts:
- Nasociliary part;
- Frontal part;
- Lacrimal part;
The maxillary nerve is the second branch of the trigeminal nerve, innervating the teeth and gums of the corresponding jaw, skin, eyelids, lips, cheeks and temporal areas, mucous membranes of the palate, upper lip, nasal cavities, maxillary sinuses, cheeks. Thus, it is responsible for the innervation of the middle part of the face from the palpebral fissure to the corner of the mouth.
It is sensitive, originates in the Gasserian plexus, and from the cranial fossa passes through the foramen rotunde. In the skull, the middle nerve of the meninges branches off from it, which innervates the middle cranial fossa. After leaving the cavity, it passes into the pterygopalatine fossa. There it is divided into three parts:
- Zygomatic part;
- Infraorbital part;
- Nodal parts;
The mandibular nerve is the third branch that innervates the lower jaw, mucous membrane of the tongue, cheeks and lips, chin, salivary glands, temporomandibular joint, masticatory muscles and other structures. So, the sensory branches are responsible for the innervation of the lower part of the face.
A mixed nerve structure that has both sensory and motor branches. Sensitive ones begin from the Gasserian plexus, and motor ones - from one of the motor nuclei.
The anatomy of the trigeminal nerve is extremely complex and unusual, and can sometimes be subject to destructive influences, which significantly worsens the quality of life. The maxillary nerve plays a special role, since when it is damaged, the functioning of the mucous membranes is impaired.
V pair - trigeminal nerves
The trigeminal nerve (n. trigeminus) is mixed, contains sensory and motor fibers and parasympathetic fibers secondarily connected to some of its branches. The structure of the trigeminal nerve is similar to the structure of the spinal nerve. The sensitive part of the trigeminal nerve has a large ganglion (gangl. trigeminale) 15-30 mm long and 8-12 mm wide. It is located in the middle part of the cranial fossa in the cavum trigeminale between the layers of the dura mater. The node has dendrites that form three large nerves: the ophthalmic, maxillary and mandibular, as well as axons that form the sensory root. This root penetrates through the middle peduncle of the cerebellum, switching on three nuclei: the superior sensory (nucl. sensorius superior) and spinal (nucl. tr. spinalis) pathways - in the bridge, representing interneurons of general sensitivity; midbrain tract (nucl. tr. mesencephalic!) - in the midbrain, contains proprioceptive somatic afferent neurons. The motor part starts from nucl. motorius n. trigemini lying in the bridge. The axons form a motor root that joins the mandibular nerve.
The structure of the sensitive part is as follows. It has three nerves: ophthalmic, maxillary and mandibular (mixed) (Fig. 522 A), which are formed from the connection of many branches starting from the receptors:
1. Branches of the optic nerve (n. ophthalmicus) (Fig. 523).
523. Trigeminal nerve. 1 - n. supraorbitalis; 2-n. supratrochlearis; 3 - n. infratrochlearis; 4 - n. oculomotorius; 5 - n. infraorbitalis; 6 - gangl. pterygopalatinum; 7 - rr. alveolares superiores anteriores; 8 - pi. dentalis superior; 9 - n. lingualis; 10 - n. mylohyoideus; 11 - n. alveolaris inferior; 12 - n. mentalis; 13 - n. hypoglossus; 14 - n. mandibularis; 15 - n. maxillaris; 16 - gangl. trigeminal; 17 - n. ophthalmicus
Tentorial branch (r. tentorii). The thin branch begins from receptors located in the lateral and superior walls of the cavernous sinus. The branch enters the optic nerve as it exits the orbit.
Lacrimal nerve (n. lacrimalis). Forms fibers that contact the receptors of the lacrimal gland, skin and conjunctiva of the lateral corner of the eye. Parasympathetic fibers that leave the zygomatic nerve are connected to the lacrimal nerve. These postganglionic fibers arose from the pterygopalatine ganglion to innervate the secretory cells of the lacrimal gland.
Frontal nerve (n. frontalis). Formed by connecting the supraorbital, supratrochlear nerves and the frontal branch: 1) the supraorbital nerve (n. supraorbitalis) starts from the receptors of the skin and tissue of the frontal region, passes into the orbit through a notch or hole in the supraorbital edge of the frontal bone; 2) the supratrochlearis nerve (n. supratrochlearis) contacts the receptors of the upper eyelid, medial corner of the eye and glabella. Penetrates into the orbit near the block of the superior oblique muscle, i.e. in the medial corner of the eye; 3) the frontal branch (r. frontalis) is thin, has receptors in the skin along the midline of the forehead. The nerve passes into the orbit closer to the medial corner of the eye. All three branches join at n. frontalis at the site of attachment of the superior rectus muscle to the eyeball.
The nasociliary nerve (n. nasociliaris) is formed from a number of branches: a) a long root (radix longa) - its fibers contact the receptors of the eyeball and are directed to the ciliary node (Fig. 523); b) long ciliary nerves (nn. ciliares) start from the receptors of the eyeball, numbering 2-3, exit through the posterior pole of the eyeball above the exit of the optic nerve; c) the posterior ethmoid nerve (n. ethmoidalis posterior) has receptors in the mucous membrane of the sphenoid sinus, the posterior cells of the ethmoid bone. Penetrates from the nasal cavity into the orbit through the posterior ethmoidal openings; d) the anterior ethmoidal nerve (n. ethmoidalis anterior) has receptors in the mucous membrane of the frontal sinus, in the ciliary ganglion, the skin of the tip of the nose and the nasal mucosa; dendrites pass into the cranial cavity through holes in the horizontal plate of the ethmoid bone, where fibers innervating the dura mater of the anterior cranial fossa are connected to them. The anterior ethmoidal nerve then passes through the anterior ethmoidal foramen into the orbit; e) subtrochlear nerve (n. infratrochlearis) starts from the skin receptors of the upper eyelid, medial corner of the eye and nose. Penetrates into the orbit under the block of the superior oblique muscle.
523A. Scheme of the first branch of the trigeminal nerve. 1 - n. supratrochlearis; 2 - n. frontalis; 3 - n. lacrimalis; 4 - fissura orbitalis superior; 5 - r. meningeus; 6 - n. ophthalmicus; 7 - gangl. trigeminal; 8 - n. nasociliaris; 9 - radix oculomotoria; 10 - n. oculomotorius; 11 - gangl. ciliare; 12 - nn. ciliares breves; 13 - n. ethmoidalis posterior; 14 - n. ethmoidalis anterior; 15 - n. zygomaticus; 16 - r. communicans cum n. zygomatico; 17 - n. infratrochlearis
The ophthalmic nerve (n. ophtlalmicus) is sensitive, 2-3 mm in diameter, formed by the fusion of the lacrimal, frontal and nasociliary nerves lateral to the trochlear and abducens nerves in front of the superior orbital fissure. In the cranial cavity, the optic nerve is located in the lateral wall of the cavernous sinus together with n. trochlearis and n. abducens. Next, it enters the anterior pole gangl. n. trigemini.
2. Branches of the maxillary nerve (n. maxillaris) (Fig. 524). The middle meningeal branch (r. meningeus medius) starts from the receptors of the dura mater of the middle cranial fossa and joins the maxillary nerve near the round foramen of the sphenoid bone.
524. Scheme of the second branch of the trigeminal nerve. I - pes anserinus minor; 2 - rr. labiales superiores; 3 - rr. nasales externi; 4 - rr. palpebrals inferiores; 5 - for. infraorbitals; 6 - n. infraorbitalis: 7 - n. zygomaticofacial; 8 - for zygomaticofacial; 9 - n. zygomaticotemporal; 10 - for. zygomaticotemporale; II - for zygomaticoorbital; 12 - n. lacrimalis; 13 - r. communicans cum n. lacrimalis; 14 - fissura orbitalis inferior; 15 - n. zygomaticus; 16 - nn. pterygopalatine 17 - for. rotundum; 18 - r. meningeus medius; 19 - gangl. pterygopalatinum; 20 - nn. palatini; 21 - nn. nasales posteriores; 22 - rr. orbitales; 23 - rr. alveolares superiores posteriores; 24 - rr. alveolares superior medius et anteriores; 25 - pi. dentalis superior; 26 - rr. dentales superiores
The orbital branches (rr. orbitales) have receptors in the mucous membrane of the posterior cells of the ethmoid bone and the sphenoid sinus. Their fibers penetrate through the openings in the sutura sphenoethmoidalis into the posterior part of the orbit, through the inferior orbital fissure into the pterygopalatine ganglion and further into the pterygopalatine nerves (nn. pterygopalatine, which enter the maxillary nerve within the pterygopalatine fossa. The orbital branches include parasympathetic fibers from the pterygopalatine ganglion and sympathetic fibers from n. petrosus profundus, passing through the pterygopalatine ganglion.
The posterior superior nasal branches (rr. nasales posteriores superiores) contain sensory receptors in the mucous membrane of the nasal cavity and are formed from 8-15 branches in the form of three nerves: 1) nasopalatine nerve (n. nasopalatinus), the sensory fibers of which begin from receptors located in mucous membrane of the hard palate of the oral cavity. Its branches are through for. incisivum pass into the nasal cavity, located in the submucosal layer of the nasal septum, accompanying a. nasalis posterior septi; 2) in the nasal cavity, the medial branches of the posterior superior nasal nerve (rr. nasales posteriores superiores mediates), innervating the mucous membrane of the nasal septum in the upper nasal passage, join the nasopalatine nerve; 3) the lateral branches of the posterior superior nasal nerve (rr. nasales posteriores superiores laterales) contact receptors in the mucous membrane of the upper and middle nasal passages, the posterior cells of the ethmoid bone, the vault of the pharynx, the auditory tube, the choanae and the sinus of the sphenoid bone. Sensory fibers of these three nerves through for. sphenopalatinum penetrate the pterygopalatine fossa, pass by the pterygopalatine node and through the nn. pterygopalatini reach the maxillary nerve. In the pterygopalatine fossa, from its node, parasympathetic postganglionic and sympathetic fibers from n penetrate into the posterior superior nasal branches. petrosus profundus for the innervation of mucous glands located in the zone of sensitive innervation (Fig. 525).
525. Scheme of the structure of the pterygopalatine node. Red lines are parasympathetic fibers; blue - sensitive; blue (intermittent) - sympathetic. 1 - gangl trigeminale; 2 - n. petrosus major; 3 - petrosus profundus; 4 - gangl. pterygopalatinum; 5 - nn. palatini minores; 6 - rr. nasajes; 7 - nn. pterygopalatini; 8 - n. zygomaticus
The palatine nerves (nn. palatini) are formed from three nerves:
1) the greater palatine nerve (n. palatinus major) starts from the receptors of the mucous membrane of the hard and soft palate. The axons of sensory cells form 3-4 trunks, which through for. palatinum majus penetrate the canalis palatinus major, and then into the pterygopalatine fossa and then enter the maxillary nerve;
2) small palatine nerves (nn. palatini minores) contact the receptors of the mucous membrane of the soft palate, palatine tonsil. They contain motor fibers from n. facialis, penetrating into m. levator veli palatini as part of n. petrosus major. The fibers of the lesser palatine nerve enter through the lesser palatine foramina into the canalis palatinus minor and reach the maxillary nerve;
3) the lower posterior lateral nasal branches (rr. nasales posteriores inferiores laterales) contain sensory fibers starting from receptors in the mucous membrane of the walls of the lower and middle nasal passages, the maxillary sinus. Through small openings between the palatine bone and the pterygoid processes they penetrate the canalis palatinus major, reach the pterygopalatine fossa and through the nn. pterygopalatini reach the maxillary nerve;
4) pterygopalatine nerves (nn. pterygopalatini) are sensory fibers of the orbital branches, posterior superior nasal branches and palatine nerves, connecting above the pterygopalatine ganglion into the pterygopalatine nerves entering the maxillary nerve.
All branches of the palatine nerves contain parasympathetic fibers emerging from the pterygopalatine ganglion, and sympathetic fibers from n. petrosus profundus, which reach the mucous glands of the oral and nasal cavities. Thus, nn. palatini are mixed.
The zygomatic nerve (n. zygomaticus) is formed from two nerves: 1) the zygomaticofacial branch (r. zygomaticofacialis) contacts the skin receptors of the upper part of the cheek and the lateral canthus. Its fibers penetrate through for. zygomaticofacial into the thickness of the zygomatic bone, where they connect with n. zygomaticotemporalis, which penetrates through for. zygomaticoorbital into the orbit; 2) the zygomaticotemporal branch (r. zygomaticotemporalis) starts from receptors located in the skin of the temporal and frontal regions. The nerve enters through for. zygomaticotemporal into the thickness of the zygomatic bone, uniting with the zygomaticofacial nerve into the zygomatic nerve. The zygomatic nerve passes into the orbit through the for. zygomaticoorbitale, located outside the eyeball. The zygomatic nerve leaves the orbit through the inferior orbital fissure and, within the pterygopalatine fossa, enters the maxillary nerve. As part of the zygomatic nerve, and then the zygomaticotemporal branch, parasympathetic fibers pass from the pterygopalatine nerve. In the orbit they leave the zygomaticotemporal branch and go to n. lacrimalis, which reaches the lacrimal gland. This transition of parasympathetic fibers from one nerve to another is called the connective branch.
The branches of the infraorbital nerve (n. infraorbitalis) are divided into two groups: the first has receptors in the soft tissues of the upper jaw, the second - in the teeth and gums of the upper jaw.
Branches of the first group: a) upper labial branches (rr. labiales superiores) have their receptors in the skin and mucous membrane of the upper lip. Nerve fibers unite into 3-5 branches located under the quadratus superior labii muscle in fossa canina. These branches reach for. infraorbital and are part of the infraorbital nerve; b) internal nasal branches (rr. nasales interni) begin from receptors located in the mucous membrane of the vestibule of the nose. The branches emerge through the openings between the nasal cartilage and the nasal bone and connect with the external nasal branches; c) external nasal branches (rr. nasales externi) contact the skin receptors of the wings of the nose; d) the lower branches of the eyelids (rr. palpebrales inferiores) begin from the receptors located in the skin of the lower eyelid. The nerve descends, passing through the beginning of the quadratus superior labii muscle, and enters the infraorbital nerve.
Branches of the second group: a) anterior superior alveolar branches (rr. alveolares superiores anteriores) begin from receptors located in the pulp of the upper incisors and canines, gums, periodontium and the mucous membrane of the anterior nasal cavity. Then their fibers enter the alveolar process of the upper jaw, participating in the formation of the upper dental plexus (plexus dentalis superior). From the dental plexus, 1-2 branches of the anterior superior alveolar branches are formed, which pass along the canalis alveolaris in the upper jaw. Via for. alveolaria anteriora they exit into the orbit, where they unite with the infraorbital nerve in the inferoorbital canal; b) the middle upper alveolar branch (r. alveolaris superior medius) has receptors in the pulp of the upper small molars, gums, periodontal and periodontal tissues, then the fibers participate in the formation of the upper dental plexus (plexus dentalis superior). From this plexus, 1-2 branches emerge along the alveolar canal in the thickness of the body of the upper jaw and enter the terminal part of the infraorbital nerve in the region of the pterygopalatine fossa; c) posterior superior alveolar branches (rr. alveolares su-periores posteriores) contact the receptors of the mucous membrane of the maxillary sinus, the pulp of large molars, gums, periodontal and periodontal tissues. The nerve fibers of the receptors participate in the formation of the superior dental plexus, located at the apexes of the roots in the alveolar process. The posterior superior alveolar nerve is formed from the plexus, which reaches the posterior alveolar openings of the tubercle of the upper jaw through the canalis alveolaris. Having entered the infratemporal fossa, with up to 8 branches, the nerve enters the pterygopalatine fossa and unites with the infraorbital nerve.
Thus, from the fusion of many branches, the infraorbital nerve is formed, initially located in the sulcus infraorbital, in the space from the infraorbital foramen to the pterygopalatine fossa. In this fossa it participates in the formation of the maxillary nerve.
The maxillary nerve is formed by connecting the pterygopalatine, zygomatic, infraorbital nerves and the meningeal branch within the pterygopalatine fossa. The nerve has a diameter of 2.5-4 mm, a length of 12-15 mm and passes through the round foramen of the sphenoid bone into the cranial cavity, where it enters the ganglion. trigeminale.
3. The branches of the mandibular nerve (n. mandibularis) are mostly mixed, consisting of sensory and motor fibers (Fig. 526). Parasympathetic fibers are secondarily attached to some branches. Motor fibers start from the motor nucleus (n. totorius), exit the pons, connecting to the incoming axons of the sensory root. Motor fibers are located next to the trigeminal ganglion, then exit into the infratemporal fossa. Its branches are as follows.
526. Scheme of the structure of the third branch of the trigeminal nerve. 1 - for. ovale; 2 - g. trigeminal; 3 - r. mandibularis; 4 - rr. temporales superficialises; 5 - nn. auriculares anteriores; 6 - f. spinosum; 7 - r. communicans cum n. faciali; 8 - n. auriculotemporalis; 9 - n. alveolaris inferior; 10 - n. mylohyoideus; 11 - n. hypoglossus; 12 - pi. dentalis inferior; 13 - n. mentalis; 14 - n. sublingualis; 15 - rr. linguales; 16 - chorda tympani; 17 - n. lingualis; 18 - n. pterygoideus medialis; 19 - n. massetericus; 20 - n. buccalis; 21 - n. pterygoideus lateralis; 22 - nn. temporales profundi
Meningeal branch (r. meningeus). Its receptors are located in the dura mater of the middle cranial fossa and the mucous membrane of the mastoid cells. Fibers exit the skull through for. spinosum into the infratemporal fossa and enter the nerve near the for. ovale.
The auriculotemporal nerve (n. auriculotemporalis) is formed from the following branches:
a) superficial temporal branches (rr. temporales superficialises) have receptors in the skin of the temporal region. The fibers descend to the temporomandibular joint, passing the premaxillary fossa between the external auditory canal and the temporomandibular joint;
b) anterior auricular nerves (nn. auriculares anteriores) start from the skin receptors of the auricle and temporal region, enter the auriculotemporal nerve in front of the external auditory canal;
c) the nerve of the external auditory canal (n. meatus acustici externi) comes from the receptors of the eardrum and the skin of the external auditory canal;
d) branches of the parotid salivary gland (rr. parotidei) have receptors in the capsule and parenchyma of the gland. Their fibers go upward, entering the auriculotemporal nerve. It contains postganglionic parasympathetic fibers from gangl. oticum for the secretory innervation of the parotid salivary gland (see “Parasympathetic part of the autonomic nervous system”
) (Fig. 527).
527. Diagram of the structure of the ear node. Blue lines are sensory fibers, red lines are parasympathetic; yellow - motor; green - sympathetic (according to Clara)
e) articular branches (rr. articulares) emerge from the joint capsule on its posterior surface and join the auriculotemporal nerve. This nerve, penetrating the infratemporal fossa, covers a. meningea media, entering the mandibular nerve.
The deep temporal nerves (nn. temporales profundi) have motor and sensory fibers. Sensory fibers begin from the receptors of the temporal muscle. They contain afferent-proprioceptive fibers. These nerves receive anterior and posterior deep branches. Their fibers are located between the skull and the temporalis muscle, then pass along the outer base of the skull to the for. ovale, where they join n. mandibularis. Sensory fibers are connected to motor fibers.
The lateral pterygoid nerve (n. pterygoideus lateralis) contains sensory and motor fibers: sensory fibers have receptors in the lateral pterygoid muscle, motor fibers join them and provide the muscle with motor innervation.
The buccal nerve (n. buccalis) starts from the receptors of the cheek, gums and corner of the mouth. The fibers are located on the outer surface of m. buccinator, covered with the fatty body of the cheeks. Then it rises in the direction of the coronoid process of the lower jaw, passes between the temporal and lateral pterygopalatine muscles, penetrating into the infratemporal fossa. It enters, together with the sensory fibers of the lateral pterygopalatine nerve, into the mandibular nerve.
The chewing nerve (n. massetericus) is mixed. Sensory fiber receptors are located in the capsule of the temporomandibular joint and the masticatory muscle. The fibers then gather between the masseter muscle and the ramus of the mandible and pass through the incisura mandibularis above m. pterygoideus lateralis into the infratemporal fossa, where, together with other sensory nerves, they enter the mandibular nerve. The nerve includes motor fibers to innervate the masticatory muscles.
The lateral pterygoid nerve (n. pterygoideus lateralis) consists of sensory and motor fibers. Sensitive fibers contact receptors located in mm. tensor tympani, tensor veli palatini, pterygoideus medialis. The fibers collect near the gangl. oticum into a single nerve that enters the for. ovale. Motor fibers innervate the muscles listed above.
The lingual nerve (n. lingualis) is formed from three sensory nerves: a) lingual branches (rr. linguales) have general sensitivity receptors in the mucous membrane and muscles of the tongue and specialized taste sensory receptors of the tongue go linea terminalis. The branches accompany a. and vv. profundae linguae to the root of the tongue, between m. hyoglossus and m. genioglossus enter the lingual nerve. Taste sensory fibers leave n. lingualis at the upper edge of the medial pterygoid muscle, entering the chorda tympani. The chorda tympani fibers reach the intercalary nucleus nucl. tr. solitarii; b) the hypoglossal nerve (n. sublingualis) contacts receptors in the mucous membrane of the floor of the mouth, gums and sublingual salivary gland. This nerve connects to n. lingualis near the posterior edge of the submandibular gland; c) branches of the isthmus of the pharynx (rr. isthmi faucium) begin from the receptors of the mucous membrane of the pharynx and the floor of the mouth. All three branches contain parasympathetic fibers, attached from the chorda tympani to innervate the mucous glands (see Parasympathetic part of the autonomic nervous system
).
From the fusion of the lingual branches, the hypoglossal nerve and the branches of the isthmus of the pharynx, n is formed. lingualis. The lingual nerve exits the tongue on the lateral surface at the level of the circumvallate papillae. It passes above the submandibular gland between the inner surface of the lower jaw and the medial pterygoid muscle, then is located on the outer surface of the hyoglossus muscle in the fold of the oral mucosa. Above the tongue, the nerve is initially located in the tissue between the medial pterygoid muscle and the branch of the mandible, passing between the pterygoid muscles in front of the mandibular nerve near the for. ovale, then enters the mandibular nerve.
The inferior alveolar nerve (n. alveolaris inferior) contains sensory and motor fibers. Formed from the following branches.
The mental nerve (n. mentalis) is formed from the connection of several branches: a) mental branches (rr. mentales) begin from the skin receptors of the chin; b) branches of the lower lip (rr. labiales inferiores) extend from the receptors of the skin and mucous membrane of the lower lip; c) the incisive branch (r. incisivus) has receptors in the pulp of the incisors, the canine, and the gum. Fibers from the receptors penetrate the lower jaw and enter n. mentalis in the area of the mental foramen.
The lower dental and gingival branches (rr. dentales et gingivales inferiores) are represented by receptors in the pulp of small and large molars, periodontium, periodontal tissue and gums. The branches of the nerve enter the inferior alveolar nerve along the entire passage of the nerve along the canalis mandibularis.
The maxillohyoid nerve (n. mylohyoideus) starts from sensory receptors in the m. mylohyoideus and m. digastricus (venter anterior). The fibers gather towards the inner surface of the lower jaw and go in the for direction. mandibulare. Above this foramen the nerve enters the inferior alveolar nerve. The mylohyoid nerve contains motor fibers to innervate the muscles. The inferior alveolar nerve emerges from the canalis mandibularis and lies between the lig. sphenomandibula and the branch of the lower jaw, penetrating between the pterygoid muscles. Enters the mandibular nerve next to n. lingualis.
Embryogenesis. The trigeminal nerve has sensory and motor fibers. Sensitive fibers grow from the neuroblasts of the semilunar ganglion at the beginning of the 4th week of embryonic development into the formation of the visceral skull to innervate the derivatives of the first branchial arch. Proprioceptive afferent neurons originate outside the trigeminal ganglion, in the basal lamina of the hindbrain, forming the nucl. mesencephalicus. Motor fibers grow from the cells of the basal plate of the bridge into the muscles of the branchial apparatus, which represent the anlage of the masticatory muscles.
Phylogenesis. As data from comparative anatomy show, the trigeminal nerve was formed as a result of the connection of the deep orbital nerve with its ganglion (gangl. profundum) and the trigeminal nerve itself. It is preserved as an independent nerve in Polypterus (many-feathered ganoids), Urodela and some fish. In other animals, the deep ophthalmic nerve joins the trigeminal nerve itself, turning into n. ophthalmicus (I branch). Some fish have two orbital branches - superficial and deep. In Tetrapoda, only the deep branch of the ophthalmic nerve is preserved, and the superficial branch is reduced. The second branch (r. maxillaris superior) in all animals innervates the teeth, upper jaw and the area from the eye to the mouth. The third branch is best developed - r. mandibularis, which contains sensory and motor fibers. In cartilaginous fish, the third branch runs along the outer surface of the cartilaginous lower jaw. In animals with a bony skeleton, r. mandibularis enters the bone canal. Only in Sauropsidae are motor fibers separated into an independent bundle. In mammals, as a result of division, only the axons forming the portio minor remained independent. In reptiles and mammals, the sensory branches innervating the tongue and the mucous membrane of the floor of the mouth are concentrated into a single n. lingualis. In animals of other species, the sensory nerves of the oral cavity have a scattered shape and n. lingualis does not exist in the form of a single trunk.
Symptom complex of lesion
The pain associated with damage or inflammation of this nervous structure is extremely intense, which causes significant discomfort for the patient. Often the ternary nerve can cause intense pain in the upper or lower jaw.
Such pain practically does not go away without treatment, so it is important to find a specialist who will prescribe quality treatment. In addition, there are points on the face that allow you to determine the level of damage - a separate root or the entire nerve as a whole.
Often, pathology occurs due to organic changes at the exit sites of the trigeminal nerve, since the nerve located there is most susceptible to compression and further inflammation. This may be indicated by pain around the eyes or nose.
The neuralgic condition is accompanied by a feeling of pain, which is similar to electric shocks. The pain may also spread to the cheek, forehead, or jaw areas. It is important to determine the source of trigeminal nerve damage in order to alleviate and eliminate discomfort.
Classification of neuralgic diseases
Before proceeding to structuring the identified pathologies, it should be noted that neuralgia is understood as a pathological process that occurs as a result of damage to the nerves of the peripheral system.
In practice, the following types of damage are distinguished:
- Damage to the trigeminal nerve, which is characterized by pain in the gums, in the upper part of the jaw, as well as in the lower eyelids and along the side of the nose.
- Intercostal neuralgia, manifested by sharp pain in the chest area.
- Damage to the external cutaneous nerve.
- Neuralgia of the glossopharyngeal nerve, which is quite rare.
- Occipital lesion, which is characterized by pain in the back of the head, in the temporal and ocular areas.
- Neuralgia of the pterygopalatine ganglion usually affects the affected half of the face.
Causes of pain
Pain can occur for various reasons, which may not go away on its own without treatment. For example, neuralgia can occur due to close contact between a nerve and a vessel (vein or artery), which will lead to inflammatory reactions. In addition, tumors can compress nerve structures, which will certainly lead to excessive irritation of the receptors. Remember that the trigeminal nerve is extremely sensitive to various pathological influences.
The symptom complex of neuralgia that affects the tertiary nerve is as follows:
- The appearance of “shooting” pain in the facial area;
- Changes in the sensitivity of the skin of the facial area;
- The pain intensifies with chewing, touching, and activity of the facial apparatus;
- The occurrence of paresis (an extremely unlikely situation);
- Painful sensations appear only on one side;
Another cause of pain may be pinched nerve structures. In such situations, the duration of pain can vary from a few seconds to hours. Such neuropathies are caused by unsuccessful plastic or dental operations, during which a pathological change in the surrounding structures occurred.
In this case, the patient is in an anxious state, which significantly affects the course of treatment. The patient is worried about not only his physical condition, but also his aesthetic one. Such worries can only intensify the pain experienced. It is important to ensure that the branches of the trigeminal nerve do not spread infectious agents between each other.
In addition to the mechanical nature of the cause, the trigeminal facial nerve can be affected by viral agents.
For example, a special herpes virus, which causes shingles, is capable of destroying the skin down to the nerve roots.
You can suspect herpes zoster (zoster disease) by:
- Herpetic rash on the skin;
- Changes in skin color and the appearance of edematous manifestations;
- Formation of bubbles with liquid of varying turbidity;
As you can see, there are a number of reasons that can cause neuralgia of the corresponding nerve. It is important not only to relieve pain, but also to get rid of the cause, and only a competent medical specialist can cope with this task.
Remember that the maxillary nerve and the infraorbital nerve lie extremely close, so if only one part is inflamed, the process can spread lower. It is extremely important that the pathology does not damage other cranial nerves, as this can lead to disruption of other vital functions of the human body.
Causes of the disease
For students of neurology, it is important to know the causes of the disease ganglionitis, what it is. In women, the disease occurs as often as in men. It is less common in children.
The causes of the disease are different, but most often these are the following infections: influenza, rheumatism, malaria, diabetes, sore throat, tumors. It can also be otitis, sinusitis, pharyngitis, rhinitis. Injuries, general poisoning of the body, overexertion, stress can cause illness. Statistically, the most common cause is herpes.
Ganglionitis that occurs in the area of the pterygopalatine node most often appears due to sinusitis, rhinitis, tonsillitis, pharyngitis, and purulent otitis.
Thus, inflammation starting in the nerve ganglia leads to rashes and acute pain. The virus can stay there for quite a long time, and stress, infection, or some kind of damage can trigger the rash.
The virus can persist in the spinal ganglia after chickenpox in childhood. Against this background, ganglionitis occurs in adulthood. This happens if the body is weakened or gets infected.
Principles of pathology treatment
The main goal of treatment procedures is to relieve pain in the patient. Basically, doctors give preference to drug treatment, but physiotherapeutic procedures – treatment with dynamic currents, ultraphoresis, etc. – have an important positive effect.
Taking pharmacological agents helps relieve pain attacks. Initially, the doses of drugs are quite large, but subsequently they are reduced to reduce hepatotoxic and nephrotoxic effects.
Main classes of medications for treatment:
- Antiepileptic drugs;
- Antispasmodic and anticonvulsant drugs;
- B vitamins and antidepressants;
Medical specialists give preference to Finlepsin, Baclofen and Lamotrigine, since these drugs have shown the greatest effectiveness in the treatment of such pathology.
When the pain intensity is high, blocks of the corresponding nerve are often performed. This procedure is performed by injecting an anesthetic in close proximity to a nerve or ganglion to relieve pain.
The procedure is carried out in two stages, with two injections: intradermal and periosteal injection. The drugs of choice are Ledocaine and Diprosan, however, performing this procedure on your own is strictly prohibited, as there is a high probability of damage to important structures.
Preventive actions
Only the patient is able to delay the exacerbation of attacks as much as possible, and for this he needs to follow a number of recommendations that will definitely help him:
- Avoid draft winds and hypothermia of the scalp, as long-term compensatory inflammatory reactions can intensify the pathological process;
- Do everything possible to activate the immune response - hardening, walks in nature, physical exercise;
- Avoid stressful situations;
- Watch your diet and the balance of food intake. These actions will help optimize metabolic processes in your body, which will significantly improve the quality of your life;
- Carry out routine examination and treatment of the mouth and nasopharyngeal space, since these are the regions that can cause pathological infectious and inflammatory processes;
As you can see, nothing is impossible. In addition to the fact that these tips will ease and delay the appearance of neuralgia, you will feel a surge of vital energy and a desire to live, since a healthy lifestyle predisposes to such a desire
Remember that it is much easier to prevent and prevent a disease than to carry out lengthy and expensive treatment in the future, which may not help the first time. The treatment is extremely long and unpleasant, and also requires an extremely competent neurologist to help you. Unfortunately, today it is quite difficult to find a specialist who has the necessary knowledge, and it is important to start competent treatment as early as possible.
Disease prognosis
Neuralgia of the fifth pair of cranial nerves is not capable of causing death, but the patient’s quality of life is significantly reduced. Positive results can only be achieved by the patient’s perseverance and the high qualifications of the attending physician.
The patient is obliged not only to follow all the doctor’s recommendations and prescriptions, but also to monitor his lifestyle. It is necessary to exclude exposure to damaging environmental factors.
By carrying out a course of drug treatment, the patient has a chance to maximize life expectancy without exacerbation of the condition, as well as significantly reduce its intensity. Sometimes the desired effect can only be achieved through surgical manipulation. It is unacceptable to refuse to undergo them, since further development of the pain syndrome can significantly worsen your life.
Remember that despite the presence of many traditional methods of relieving pain and treating neuralgia, it is unacceptable to use them without specialized medical treatment. People's advice can only alleviate the condition in the first stages, but in no way cure it.
Take care of your health in order to live a long and happy life, since the quality of your life depends only on you!