Inflammation of the ilioinguinal nerve
We consider the iliohypogastric, ilioinguinal, and femorogenital nerves
in the same group because of their similar origins, sites of innervation, and causes of dysfunction. These nerves begin from the spinal roots of L1 (the L2 root also takes part in the formation of the femoral-genital nerve) and first pass through the psoas muscle, and then in close proximity to it (as they pass in the abdominal cavity). The iliohypogastric nerve appears above the iliac crest and supplies sensory branches to the skin in the upper buttock area, as well as near the pubis. The ilioinguinal nerve enters the inguinal canal from its lateral edge and innervates the area above the inguinal ligament and the base of the genitalia. Both the iliohypogastric and ilioinguinal nerves also innervate the muscles of the lower abdomen. After the genitofemoral nerve emerges from the psoas muscle, it lies retroperitoneally and descends to the inguinal ligament, remaining on the surface of the psoas muscle. It provides sensory innervation to a small area over the proximal genitalia and the anterior proximal thigh.
Etiology
. Due to the location of the nerves, neuropathies usually occur as a result of surgical interventions, especially after repair of an inguinal hernia. The development of neuralgia after damage to these nerves is also common.
Clinical picture of neuropathy of the iliohypogastric, ilioinguinal and genitofemoral nerves
Anamnesis
. Patients present with a variety of sensory complaints, including numbness, paresthesia, or pain in the ipsilateral inguinal and perineal regions. If the cause is surgery, these symptoms may develop immediately after surgery or several weeks later.
Clinical examination of neuropathy of the iliohypogastric, ilioinguinal and genitofemoral nerves
– Neurological
. Neuropathies of the iliohypogastric nerve are uncommon. They cause loss of sensation in the suprapubic and superior gluteal regions. Lesions of the ilioinguinal nerve result in loss of sensation over the groin and base of the genitals, but usually cause minimal impairment of function. In other cases, pain may appear in these areas as well as in the lower abdomen and upper thigh. It may appear or intensify when the position of the leg changes. Neuropathies of the genital femoral nerve usually accompany lesions of the inguinal nerve due to the close anatomical proximity of these nerves. Symptoms and triggers are also similar, but sensory disturbances can extend to the medial and proximal genital areas.
– General
. In neuropathies of the ilioinguinal and genital femoral nerves, areas of tenderness that often coincide with the site of injury may be found in the groin area.
Differential diagnosis
. In cases of these neuropathy, nerve damage causes predominantly sensory disturbances. Therefore, the differential diagnosis should focus on identifying other causes of sensory abnormalities beyond the typical boundaries of these nerves, including abnormalities in the medial thigh (obturator nerve), anterior thigh (femoral nerve), and lateral thigh (lateral femoral cutaneous nerve). as well as dermatomal changes caused by T12 and L1 radiculopathies. Because of the overlap of sensory innervation zones, the presence of motor deficits or altered reflexes is the most important factor in the existence of one of these diseases. Back pain, which may indicate radiculopathy, or lack of previous surgery, which is a common cause of these neuropathy findings, suggests another etiology.
Examination of neuropathy of the iliohypogastric, ilioinguinal and genitofemoral nerves
Electrodiagnostic studies
play a minor role in the diagnosis of these neuropathies. However, EDI becomes necessary when attempting to identify either more proximal lesions (namely, plexuses or roots) or other neuropathies (femoral nerve) that may clinically resemble these neuropathies in terms of sensory innervation.
Ilioinguinal nerve: symptoms and treatment of pinching
Pinched nerves can occur in more than just the neck, lower back, or extremities. In some cases, neurological pain occurs in the groin. This is a fairly rare symptom, but it occurs in some patients. In the groin area there are branches of nerves located in the lumbar and sacrum areas. The endings of the ilioinguinal nerve are located here. It is rarely subject to compression. However, with some pathologies and injuries, infringement of this part of the peripheral nervous system is observed. This is accompanied by chronic pain and sometimes a feeling of numbness.
What causes the disease
The cause of the disease is that the nerves are pinched between the bones, ligaments or tendons of the pelvis. This happens when you stay in an inclined position for a long time, and sometimes even when you sit in one position for a long time. Sometimes, if a nerve is pinched long enough or if there is damage to it, fluid can accumulate inside and begin to put pressure on the pelvic area, leading to increased pain.
The causes of a pinched nerve may include the following:
- the appearance of callus, which causes injury to the joint;
- acquired diseases of joints and ligaments, including various types of arthritis and arthrosis;
- excessive physical activity;
- narrowing of the opening in the spinal cord canal, spinal hernia;
- bone tuberculosis, which affects bone tissue in the pelvic area;
- severe diseases of the circulatory system, including cancer;
- injuries to joint or bone tissue.
In women during pregnancy, the greatly enlarged uterus puts pressure on the sacral plexus, from which the nerve emerges. This leads to pinching and severe pain. Sometimes symptoms of pinching appear after childbirth. This happens when the baby is malpresented or during a difficult birth.
The causes of neuralgia can be diabetes, excess weight, and sometimes even shingles if it is localized in the lumbar region. In children, entrapment is more often caused by trauma.
Establishing the cause is very important, since this allows you to develop the correct approach to treatment and elimination of pain caused by a pinched nerve
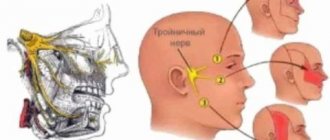
Anatomical structure
The ilioinguinal nerve begins in the lumbar region. In the groin area it branches into 2 parts. One of them innervates the thigh. The second is called the inguinal branch. The further continuation of this nerve ending depends on the gender of the person:
- In men, the inguinal branch passes through the spermatic cord and ends in the scrotum.
- In women, the inguinal branch exits in the area of the uterine ligament and ends in the area of the labia majora.
The inguinal branch is responsible for the innervation of the following organs:
- muscles and skin of the anus;
- anal sphincter;
- external genitalia;
- perineal muscles;
- bladder sphincter.
The ilioinguinal nerve affects sensations during sexual intercourse, the process of defecation and urination. Its work is regulated by the autonomic nervous system.
In some pathologies, compression of the nerve occurs, which is accompanied by chronic aching pain.
Why do men experience pain in the groin area?
In representatives of the stronger sex, the groin area is limited above by the lower part of the abdominal wall, and below by the pubic symphysis. The rectum, bladder, prostate gland and urethra are projected onto this area. Any pathology of these organs causes discomfort in the groin in men and boys.
Anatomy of the groin in men
In the groin area there is a canal through which the vas deferens, nerves, blood vessels and the muscle that lifts the testicle pass. Here are the male external genitalia, including the penis and scrotum. Structures that become inflamed cause pain in the groin:
- bladder;
- kidneys;
- ureter;
- seminal vesicles;
- urethra;
- prostate;
- testicles;
- colon;
- inguinal ligaments, muscles and lymph nodes;
- nerves of the lumbar plexus.
Causes of a pinched nerve
What causes a pinched nerve? Most often, the inguinal branch is compressed after operations for a hernia. During surgery, the doctor closes the hernial opening. In this case, the nerve branches are often damaged. In addition, after surgery, scar tissue forms, which can put pressure on the nerve.
There are other factors that can cause neuropathy (pinched nerve):
- pelvic fractures;
- difficult childbirth;
- tumors of the groin area;
- anal sphincter spasms;
- pathology of the round ligament of the uterus;
- varicocele;
- hypertonicity of the pelvic muscles;
- herpes zoster;
- horseback riding;
- long bike rides.
Symptoms
It is often difficult to diagnose ilioinguinal nerve neuropathy. Symptoms of pathology are usually mild. Patients show the following signs of the disease:
- chronic aching pain in the pelvic area;
- discomfort in the anus;
- urinary incontinence;
- sensation of a foreign body in the groin, as well as burning and tingling;
- numbness of the genital skin;
- pain during sexual intercourse and urination;
- constipation
Women experience the following symptoms of a pinched ilioinguinal nerve:
- itching in the genital area;
- burning when urinating.
For this reason, patients often mistake neuropathy for an inflammatory gynecological disease.
Nature of pain
The cause of the symptoms can be determined by the severity of the discomfort. Drawing, aching pain in the groin in men occurs with chronic diseases, tumors or tissue swelling. Severe colic indicates urolithiasis. Acute pain in the pubic area in men is a consequence of sexually transmitted diseases, acute cystitis, neuropathy of the pudendal nerve or arthrosis of the hip joint.
How does the groin hurt when the digestive system is damaged?
Many pathologies of the gastrointestinal tract cause pain in the pubic area. An inguinal hernia when strangulated is manifested by protrusion of the abdominal wall and pain with a sharp onset. The pathological process is accompanied by stool retention, nausea, and vomiting.
Chronic groin discomfort in men is observed with irritable bowel syndrome. In addition, the patient changes the frequency and consistency of stool (diarrhea or constipation), and bloating occurs. With intestinal obstruction, a sharp lumbago appears in the left iliac region, which radiates to the groin. Associated symptoms of the disease are abdominal asymmetry, vomiting, nausea, stool retention, flatulence.
The nature of groin pain in pathologies of the urinary system
Diseases of the organs that accumulate and secrete urine also cause pain in the groin area in men. With cystitis, there is a piercing pain that intensifies when urinating. The man has a feeling of incomplete emptying of the bladder, the temperature rises, and there is blood in the urine.
Complications and prognosis
In most cases, doctors are able to relieve compression of the ilioinguinal nerve. Treatment leads to the disappearance of pain and discomfort. However, a favorable prognosis is possible only if the patient consults a doctor in a timely manner. A complication of an advanced form of neuropathy is the chronicity of the process. In this case, persistent disorders of sexual function and frequent urinary incontinence occur. Patients suffer from chronic constipation. In such cases, surgical treatment of neuropathy is indicated, which requires long-term recovery after surgery.
Diagnostics
To detect neuropathy of the ilioinguinal nerve, doctors prescribe an ultrasound examination. In the presence of pathology, a deterioration in blood flow in the pudendal artery is determined. This vessel is usually compressed along with the inguinal branch.
A reliable diagnostic method is nerve block. The patient is injected into the affected area with a solution of analgesics and corticosteroids. If after this the discomfort goes away, it means that the cause of the pain was compression of the inguinal nerve. In this case, the patient is prescribed a course of treatment.
Conservative treatment
When treating a pinched ilioinguinal nerve, the patient is prescribed the following medications:
- To relieve pain, use the anticonvulsant drug Gabapentin.
- To eliminate spasms, the muscle relaxant Mydocalm is prescribed.
- It is recommended to take the Neuromultivit multivitamin complex.
For severe pain, nerve blocks are performed using analgesics and steroid hormones. For discomfort in the genital or anal area, the use of vaginal and rectal suppositories based on diazepam is indicated.
Drug treatment is supplemented with physiotherapy. When a nerve is pinched, procedures such as phonophoresis and electrophoresis are useful.
Physical therapy is also recommended. It is useful to do exercises to open and close the muscles of the perineum. However, the exercise therapy complex should be performed only after pain relief.
Therapeutic techniques
Therapy for neuropathy of the ilioinguinal nerve is divided into conservative and surgical. The first, in turn, involves the use of medications and physiotherapeutic procedures. The course of drug treatment includes:
- Analgesics – Analgin. Baralgin, Pentalgin. With their help, a nerve pathway is blocked, which helps relieve pain.
- Anticonvulsants and muscle relaxants - Hebapentin, Mydocalm - relieve muscle spasms.
- Rectal and vaginal suppositories - Diazepam.
- Vitamins – Neuromultivit.
Physiotherapeutic procedures include massage, physical therapy, electrophoresis, and phonophoresis. They improve blood circulation in muscle and nerve tissues, relieve swelling, and restore normal dynamics.
If conservative treatment is ineffective or does not produce results at all, surgical intervention is used to unblock the pinched nerve and relieve compression. The operation gives good positive results, but the recovery period after it is quite long - several months.
With timely and competent treatment, it is quite possible to correct the situation. In its absence and the pathology becomes chronic, the development of serious complications cannot be ruled out: impotence, involuntary urination and defecation. At the same time, some patients live with this disease for years, its negative impact is limited to an average level of discomfort.
Surgical intervention
If there is no effect from conservative therapy, surgical treatment is indicated. The doctor performs decompression surgery under general anesthesia. This eliminates pinching of the nerve by nearby tissues.
This operation effectively eliminates all unpleasant symptoms. However, the rehabilitation period can last several months. During this period, it is necessary to follow a gentle regimen: avoid physical activity and prolonged sitting.
It is important to remember that even after surgery, relapses of the disease are possible. When exposed to unfavorable factors, re-pinching of the inguinal nerve is possible. Therefore, preventive measures and recommendations of the attending physician should be followed.
Since there is no limit to indignation, or about neuropathy
In addition to neuralgia, the pudendal nerve can also become the scene of an inflammatory process, then they talk about neuropathy (neuropathy), or neuritis of the pudendal nerve (a term rarely used today).
Neuropathy differs from neuralgia in the presence of structural changes in the pudendal nerve, as well as movement disorders and the possibility of loss of sensitivity, which serves as a reason for indignation and upset of the patient, because we are talking about neither more nor less than the genitals.
What could be the reason?
The cause of the pathology (also called pudendoneuropathy) is the implementation of two mechanisms:
- compression-squeezing of the nerve trunk in the “scissors” of the sacrospinous ligament-piriformis muscle;
- traction due to overstretching of the nerve in the zone of its transfer over the ischial spine.
The first is illustrated by the consequences of long-term or unsuccessful horse riding or cycling (compression by a hard saddle), and the second by the consequences of surgical intervention - for example, when traction of the hip with the use of a perineal fixator, tension occurs on the nerve pressed to the pubic region.
Features of symptoms
The clinic may consist of lesions of the main nerve trunk or signs of involvement of various branches of the pudendal nerve.
When a surgical fixation is used in the perineal area, isolated damage to the dorsal nerve of the penis occurs with anesthesia of the penis and complete disruption of the previously normal erection.
Full restoration of sensitivity can occur within 6 to 18 months after surgery, but restoration of erection can be only partial.
When compressed by a hard saddle, the disorder is felt as transient numbness or the appearance of paresthesia in the genital area.
Both unilateral and bilateral loss of sensitivity may be observed, not limited to the penile area, but continuing to manifest itself also in the scrotum area.
Neuropathies of the pudendal nerve can signal themselves by pain in the lower buttock and in the anus, short-term urinary retention or a disorder of the imperatives to urinate, accompanied by sharp pain when palpated in the projection of the ischium.
In men, an inflamed pudendal nerve manifests itself with characteristic symptoms - paresthesia or hypoesthesia and pain in the peri-anal area, in the area of the penis and scrotum.
Diagnosis and treatment methods
The main diagnostic criterion is that the pull of the knee towards the opposite shoulder causes pain in the buttock (due to stretching of the sacrospinous ligament).
A simple diagnostic method is to pull the knee towards the shoulder
The clinic is confirmed by electromyography, noting the lengthening of the anal reflex, which closes on the pudendal nerve trunk, as well as a test blockade with the introduction of a novocaine solution into the area of the ischial spine.
The choice of treatment method depends on whether the process is advanced or in an acute stage.
Thus, all the symptoms disappeared in a group of cyclists on their own, after they agreed to refrain from cycling for a month. In case of chronic neuropathy, long-term restorative therapy is necessary.
In chronic cases, methods of drug therapy in combination with rational exercise therapy and physiotherapy are applicable.
Drug therapy includes the use of anti-inflammatory drugs (glucocorticoids Prednisolone, Triamcinolone, Hydrocortisone) in combination with anesthetics (Novocaine 0.5 or 1%) in the form of blockades. A case of relief of pain that had been observed for 14 years after a course of perineural administration of Triamcinolone is described.
Blockade is an effective method, the injection point is indicated with a finger
Pure novocaine blockades are usually less effective.
In order to relieve pain, suppositories of a combined formulation with anesthetics, sedatives and antispastic compounds, both rectal and vaginal, are used.
Vitamin therapy (administration of vitamin C and group B in adequate doses) is especially effective in combination with physiotherapy techniques (various methods of heat therapy), while exercise therapy allows you to increase the capabilities of muscles spasmed by pain and helps to increase the overall tone of the body.
Surgical intervention is applicable if there is no effect from treatment with therapeutic methods.
You should be extremely careful in the case of neuropathy of oncogenic etiology.
Prevention
How to prevent inguinal branch neuropathy? First of all, it is necessary to promptly cure such pathologies as hernia, pelvic fractures, herpes zoster, and gynecological diseases. If even minor aching pain persists for a long time after surgery in the pelvic area or difficult childbirth, you should consult a doctor.
A comfortable riding seat should be used. This will reduce stress on the inguinal nerve. When cycling for long periods, you need to take breaks periodically. This will reduce the risk of nerve damage.
Lumbosacral plexitis
Diseases of the pelvic organs (ovaries, tubes, appendix) can involve the lumbosacral plexus in the inflammatory process. The cause of inflammation of the lumbosacral plexus can be infections, intoxications and autointoxications. In addition, certain occupational exposures can cause diseases of various parts of the plexus.
More often we see unilateral plexus disease, but in infectious diseases they can be bilateral. Inflammation of the plexus is called plexitis.
Clinical manifestations of plexitis can be in two forms:
Paralytic form of lumbosacral plexitis
The paralytic form of plexitis is manifested by paralysis of the muscles that innervate the branches of this plexus (these are the muscles of the pelvic girdle and lower limb). Typically, atrophy, flabbiness, absence of tendon reflexes, and sensitivity disorders on the skin of the pelvic girdle and lower extremities are observed in paralyzed muscles. Patients may experience pain, which may be spontaneous or appear when pressure is applied to the plexus.
Sometimes patients experience trophic disorders. They can manifest as swelling of the skin, increased sweating, abnormal nail growth, and impaired mobility in the joints. If the process involves the pudendal part of the plexus, then disorders of the pelvic organs may occur.
Neurotic form of lumbosacral plexitis
As for the individual branches of the lumbosacral plexus, they usually manifest themselves as less intense isolated symptoms.
Anatomical location and functionality
The ilioinguinal nerve originates in the anterior lumbar vertebrae and descends to the groin area through the sacroiliac joint. Coming from under the lateral (side) edge of the psoas major muscle, it passes over the quadratus lumborum muscle through the transverse abdominal muscle, crosses the opening of the inguinal canal and is adjacent to the surface of the spermatic cord of the man or the round uterine ligament of the woman.
In men, the anterior scrotal nerves depart from it, approaching the root of the penis and innervating the scrotum and pubic skin. In women, these branches are called the anterior labial nerves because they approach the skin of the labia majora.
The scrotal and labial nerves are responsible for sensation, respectively, of the scrotum and penis in men or the upper part of the labia in women. In addition, the innervation of the following zones depends on them:
- anus - the outlet of the rectum;
- anal sphincter - a round muscle that closes the opening;
- bladder sphincter;
- perineal skin.
Causes of PPN pinching
Damage to the ilioinguinal nerve is quite rare. This can be explained by its location: the risk of somehow damaging the PPN, located deep in the groin, is quite low. And yet this happens sometimes. The most common cause of strangulation is surgery to reposition a prolapsed intestinal loop back into the abdominal cavity.
PPN neuritis can also occur as a result of surgical treatment of appendicitis and nephrectomy - removal of the kidney. The scar tissue formed after the intervention can compress and damage the nerve body - compression or compression-ischemic syndrome occurs - associated with disruption of the normal blood supply to the nervous tissue - syndrome.
Also, the cause of PPN neuropathy can be:
- Trauma (fracture) of the pelvic bones.
- Complications during labor in women.
- Defects in the structure of the round uterine ligament.
- Tumor pathologies localized in the groin area.
- Varicocele is a varicose vein surrounding the spermatic cord of the testicle in men.
- Increased tone of the pelvic muscles, including the piriformis.
- Exacerbation of herpes zoster (one of the forms of herpes).
- Displacement of the abdominal muscles when lifting heavy weights.
Pudendal neuralgia – Oberig Clinic
The main etiological factor that can provoke genital neuropathy is pinching of the pudendal nerve, which occurs in the Alcock canal. It is in this regard that experts refer to the disease as “Alcock canal syndrome.”
The disease can progress due to the formation of a hernia or injury to the groin area. Damage to the inguinoiliac nerve is the result of muscle scars beginning to form. As a rule, this occurs after injury or surgery.
Neuropathy can also develop as a result of the following factors:
- prolonged labor;
- presence of pelvic bone fractures;
- hypertonicity of the piriformis gland;
- herpes;
- tension in the obturator internus muscle;
- the presence of malignant neoplasms in the pelvic area;
- spasm of the muscles located in the anus;
- Nerve damage due to cycling or horseback riding.
Symptomatic picture
The main symptom of inflammation of the ilioinguinal nerve is causalgia - burning pain in the groin area. However, at the initial stage of the pathology, the causalgic syndrome can be episodic or weakly expressed. Therefore, it is not always possible to quickly diagnose PPN neuropathy.
Among the most common symptoms of a pinched ilioinguinal nerve are:
- Chronic aching pain in the pelvic area - according to patients, it feels as if there is a “pulling” there.
- Difficulty urinating.
- Constipation.
- Discomfort in the anal area.
- Numbness, burning and tingling in the groin area.
- Numbness of the skin of the external genitalia.
- Pain during sexual intercourse.
Patients do not immediately identify the source of the symptoms, confusing them with hemorrhoids, cystitis and other inflammatory diseases of the genitourinary area, or a sprained inguinal ligament. Women sometimes experience a burning sensation when urinating and itching in the intimate area, so they may mistake these sensations for symptoms of gynecological diseases.
Causes of groin pain in women
Groin pain in women can be caused by:
- diseases of the urinary system;
- diseases of the reproductive system;
- diseases of the digestive system;
- diseases of the musculoskeletal system;
- diseases of the lymphatic system;
- diseases of the nervous system.
The urinary system includes a complex of organs that are responsible for the formation, accumulation and removal of urine from the human body.
When consuming foods
nutrition
and liquids in
stomachTo diagnose the causes of groin pain in women, the following are used:
- interviewing the patient;
- objective examination;
- laboratory research;
- instrumental studies.
Questioning the patient
In the groin area on the right there are vital organs, tissues, and nerve endings, so there are many causes of pain radiating to the *leg*.