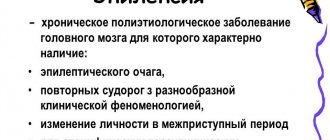
Epilepsy is a chronic disease of a psychoneurological nature. The pathology is characterized by sudden, paroxysmal convulsions, which can sometimes cause death. Epilepsy develops in humans for many reasons, and most of the provoking factors cannot be identified. There are several types of manifestations of epilepsy, each of which is characterized by its own symptoms.
What happens during an epileptic seizure?
To understand what epilepsy is, it is necessary to understand the mechanism of development of an attack. At the initial stage, the disease can be identified based on the results of a comprehensive examination of the patient or when a seizure occurs. Continued progression of the disease contributes to changes in a person’s personality.
A characteristic symptom of epilepsy in adults is a seizure, the causes of which cannot always be determined. The attack comes suddenly. In rare cases, it is preceded by the following symptoms:
- headache;
- problems falling asleep;
- decreased appetite;
- Bad mood.
Over time, patients learn to determine the imminent exacerbation of the disease by the first signs of an epileptic attack.
A seizure begins with irritation of a separate area of the brain, which leads to the appearance of an aura:
- Mental. Occurs against the background of irritation of the temporo-parietal zone. The mental aura is characterized by panic attacks or a state of inexplicable joy.
- Motor. It manifests itself in the form of motor automatism, when the limbs, head, and eyeballs change position against the patient’s wishes.
- Touch. The perception of the surrounding world is disrupted.
- Vegetative. With this aura, there are signs of dysfunction of the cardiovascular (tachycardia) and respiratory (suffocation) systems, paleness or redness of the skin, nausea, and abdominal pain.
- Speech. Expressed in shouting or pronouncing meaningless words and phrases.
- Auditory. During an epileptic attack, a person hears sounds that are not really there, which affects his behavior.
- Olfactory. This aura occurs primarily when the temporal lobe is irritated. At the same time, extremely unpleasant odors are felt that are not characteristic, for example, of food.
- Visual. Occurs when the occipital zone is affected. With visual disorders, the patient sees bright objects, faces of people, animals. Sometimes complete blindness is possible, which is short-term.
- Sensitive. This aura is characterized by a disturbance in the perception of ambient temperature. In particular, the patient may complain of cold in a warm room.
Convulsions in epilepsy, considered the most characteristic sign of pathology, occur after the onset of an aura. However, not all patients develop an exacerbation of the disease according to the described scenario. This pattern is characteristic of a grand mal seizure, which is considered a classic manifestation of epilepsy.
Treatment of epilepsy: medication, surgery, ketogenic diet, physical therapy
Surgical intervention is provided in cases where epilepsy is caused by brain tumors, with focal epilepsy. If the focus is removed correctly, then the attacks stop. However, surgery is a last resort. Basically, operations are performed when drug treatment does not help or the lesion is definitely found.
In most cases, drug treatment is used. There is no point in naming drugs for the treatment of epilepsy, since the dose and drug are determined purely individually and are sold by prescription.
Drug treatment is quite long-term. On average it lasts about 3-5 years. The withdrawal of medications is carried out gradually and under the supervision of a doctor. As a rule, after taking the first drug the patient feels better.
A ketogenic diet is used as an adjuvant treatment. This diet is low in carbohydrates, high in fat, and moderate in protein. Fats should become the main source of energy.
Physical therapy has been successfully used for epilepsy. A set of special breathing and physical exercises is aimed at stabilizing the nervous system and harmonizing a person’s mental state.
Rehabilitation should begin as soon as possible after the discovery of epilepsy. It has been proven that epilepsy with a high frequency of attacks over six months is less responsive to treatment.
Treatment of epilepsy
Forms and types of epilepsy
Depending on the location of the excitation centers, the following types of epilepsy in adults are distinguished:
- frontal;
- parietal;
- temporal;
- occipital
In addition to local epilepsy, there is a generalized form of the disease, which is divided into idiopathic and symptomatic. The first is diagnosed in cases where it is impossible to determine the causative factor. The idiopathic form is detected in 50-75% of patients. Symptomatic epilepsy is caused by organic damage to the brain.
In some cases, it is impossible to determine the type of disease. Then they talk about the flow of the cryptogenic form. Varieties of pathology include Jacksonian epilepsy, which is characterized by somatory and somatosensory disorders.
Depending on the causes of occurrence, the following forms of the disease are diagnosed:
- primary;
- secondary;
- traumatic;
- alcoholic;
- night
Various factors lead to the development of secondary epilepsy. Pregnancy, infectious diseases, nervous strain and other reasons can provoke an exacerbation of the disease. Traumatic epilepsy is caused by organic damage to the structural elements of the brain.
The alcoholic form of the disease develops as a complication of frequent drinking. Alcohol disrupts the conduction of electrical impulses (which is explained by the destruction of brain tissue), resulting in seizures.
In addition to the above forms of epilepsy, the classification of the disease takes into account the so-called absence seizure, characterized by a short-term course.
Depending on the degree of involvement of the body and the form of epilepsy, the types of seizures are of the following nature: focal, polymorphic paroxysms, febrile, tonic and clonic convulsions.
Diagnostics
Diagnosis is carried out under the supervision of a neurologist. If necessary, a cardiologist and neurosurgeon are involved. The list of studies varies from case to case.
Oral questioning makes it possible to objectify symptoms. Systematize them and create a clear clinical picture. Next, hypotheses are put forward.
A medical history is used to determine the likely underlying cause of the disorder. Plays one of the key roles in diagnosis. Facts such as lifestyle, previous diseases, current pathological processes, family history, injuries and others are established.
Routine assessment of neurological status. Testing basic reflexes. With severe symptomatic epilepsy, especially against the background of primary pathologies, deviations are present in more than half of the cases.
Electroencephalography. To assess the electrical activity of individual areas of the brain and all cerebral structures in general.
MRI of the brain. For greater information content and accuracy, it is performed with contrast enhancement using gadolinium-based drugs. They enhance the image, make it possible to identify areas of gliosis (scarring), recognize tumors and give them primary characteristics. Histological examination puts an end to the issue (a sample for evaluation is taken during the operation, since in terms of risk levels it is no more dangerous than a stereotactic brain biopsy).
As necessary, additional studies are carried out under the supervision of other specialists: cerebrospinal puncture, daily Holter monitoring (assessment of cardiac activity and blood pressure within 24 hours), electrocardiography, echocardiography, general blood tests, biochemical tests, and hormone tests.
Differential diagnosis as such is not required, because symptomatic epilepsy manifests itself quite specifically. Moreover, you can find a clear culprit for the disorder. What can not be said about the cryptogenic form. A differential diagnosis should be made when the etiology of the disorder is identified.
How does symptomatic temporal lobe epilepsy differ from structural epilepsy?
There is terminological confusion. Symptomatic structural epilepsy includes temporal and other forms. A structural disorder is spoken of if there is an organic disorder in the structure of nerve tissue. Including the already mentioned gliosis. At the same time, the temporal variety may not have a structural character, as, for example, with spontaneous excitation. Therefore, we are talking about the generic and specific relationship of concepts, and even then not always.
Causes of epilepsy
On average, in 70% of patients it is impossible to determine what can cause an attack of epilepsy (idiopathic form of the disease). This type of pathology is typical for children and adolescents. In this category of patients, impulses propagate abnormally along the nerve cells, however, when examining the brain, abnormalities in the structure of the organ are not detected.
According to research results, 40% of patients with epilepsy had cases of epilepsy among their relatives. However, the relationship between heredity and the likelihood of developing pathology has not been established.
It is important to distinguish between epileptic attacks and the causes of seizures. The latter are characteristic of infectious diseases affecting the central nervous system. Convulsions due to such pathologies occur mainly in children. In adolescents who suffered severe infectious diseases in childhood, such attacks cause severe stress and brain injury.
People at risk for developing the disease include those who:
- cases of enuresis, alcohol addiction, and migraines were diagnosed among close relatives;
- a disturbance in the conductivity of electrical impulses in the brain was detected.
Traumatic epilepsy, which occurs against the background of an injury, is one of the forms of the disease (with the exception of the above). The following factors can provoke pathology:
- encephalitis, meningitis and other brain diseases;
- organic brain damage (tumors, cysts);
- long-term use of certain medications;
- circulatory disorders caused by stroke;
- multiple sclerosis;
- toxic damage to the body;
- atherosclerosis;
- alcoholism;
- metabolic disorder in the brain.
There are also psychosomatic causes of the disease caused by internal conflicts. Such disorders, under the influence of external factors, cause excitation of certain structures of the brain, which provokes seizures. Mental reasons influence the patient’s body in a similar way. Suspicious people “invent” problems for themselves, which leads to an abnormal reaction of the brain to the surrounding reality. As a result of such exposure, an epileptic seizure occurs.
atherosclerosis
meningitis
In addition to congenital and acquired forms of the disease, epileptiform syndrome is distinguished. It occurs against the background of a strong external influence on the body, which leads to another attack of seizures. Due to the similarity in the development of these forms of the disease, neurologists have not yet been able to determine the mechanism of development of the pathology.
Risk factors
Doctors identify several factors that can increase the risk of developing the disease. These include:
- Floor. According to statistics, men suffer from the disease much more often than women.
- Age. Epilepsy can occur in a person of any age. However, the disease is more common in children and older people over 65 years of age.
- Heredity. People who have relatives suffering from epilepsy have a good chance of encountering this disease.
- Stroke, other vascular diseases. These ailments can trigger the onset of epilepsy, so it is important to prevent their development. To do this, it is important to limit alcohol consumption, stop smoking, pay due attention to physical activity, and adhere to a healthy diet.
- Inflammation of the brain. Diseases of the spinal cord and brain, such as meningitis, can increase the risk of developing epilepsy.
- Seizures in childhood. Prolonged attacks suffered in childhood (including fever caused by high temperature) can recur many years later.
- Head injuries. Take safety precautions: wear a helmet when riding a bicycle/motorcycle, buckle up when driving.
In order not to “miss” the onset of the disease, it is important to familiarize yourself with the main symptoms of the disease.