Epilepsy as a disease occurs in early childhood or during puberty. In modern medical practice there is no reliable data on the causes of episyndrome.
As a result of epilepsy, not only psychoemotional but also cognitive impairment can occur. And in the case of severe convulsive attacks, you can even die. Therefore, you need to know how to act during an exacerbation of the disease, as well as its clinical manifestations, in order to help in time and alleviate the suffering of the patient.
Content
- MRI examination for epilepsy.
- Causes of epilepsy.
- Common symptoms. Major attacks.
- Minor attacks.
- Status epilepticus.
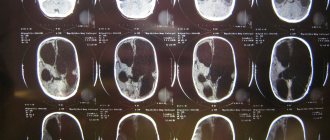
MRI examination for epilepsy
High-resolution MRI is performed after a survey study. Clarifying tomography allows you to visualize those areas of tissue and smallest structures that are inaccessible to the standard procedure. Targeted diagnostics reveals complex pathologies, for example, symptomatic epilepsy.
Targeted resonance imaging is necessary before drawing up a surgical intervention plan and for correcting antiepileptic treatment. Diagnostics are carried out on devices with a power of 3 Tesla. A high-precision study provides an image of the small structures of the brain, its vessels and membranes. Accurate images can be achieved using high-precision devices without the use of contrast agents.
Among the advantages of the technique are the speed of implementation compared to a survey examination and the absence of radiation exposure, unlike X-rays.
Chapter 1
What is epilepsy, episyndrome and epi-reaction.
Prognosis for attacks. WHAT ARE EPI SEIZURES Epi seizures are repeated attacks in the form of various convulsions, motor acts, sensations or states of altered consciousness. Different people experience different types of seizures (for example, the computer program “EPI-CENTRE” that I use allows us to treat 79 types of seizures).
An attack can manifest itself not only as convulsions and shudders, but also in the form of other motor phenomena, various sensations, loss or an altered state of consciousness. Some types of seizures are almost invisible to others.
Therefore, epileptic seizures and epilepsy are not only those dramatic and well-known conditions when a person falls on the street, twitches, and saliva runs out of his mouth. You can read a description of the different types of seizures in the recommendations: “WHAT TYPES OF SEIZURES ARE. HOW THEY DEVELOP AND PROCEED.”
The brain consists of a dense collection of nerve cells connected to each other. These cells convert each irritation perceived by the senses into electrical impulses and transmit them further in this form.
In all cases, the cause of the attack is the same - a change in the chemical state of the entire brain or its individual parts, which is accompanied by a flash of increased electrical activity (a kind of “short circuit” in the brain).
In order for this “short circuit” to occur, a limited group of brain cells with increased electrical activity is needed (epileptic focus) and a decrease in the threshold of convulsive readiness on the part of the remaining brain cells (usually “healthy” cells prevent the spread of the “short circuit” from the focus to the entire brain ).
A sharp increase in the electrical activity of nerve cells is accompanied by their excitation. Excitation of nerve cells leads to various changes in the psyche, including blackout. In addition, from nerve cells with increased electrical activity, along their long processes, excitation spreads to the muscles that are “controlled” by these cells. As a result of this, various involuntary movements or muscle spasms are observed during an attack.
WHY THERE ARE DIFFERENT PICTURES OF ATTACKS
The type of seizure is determined by where in the brain the outbreak originates and how it spreads throughout the brain. If a “flare” can occur in different parts of the brain, one child may experience two or more types of seizures. Different antiepileptic drugs act differently for different attacks.
WHAT IS AN EPI RESPONSE
A flash of electrical activity and a seizure can be caused in any experimental healthy animal in the laboratory by influencing its brain in special ways. And in ordinary life, the brain of any person can give a flash and attack (epi-reaction) when exposed to various environmental factors or various internal reasons.
Adults sometimes unwittingly experiment on themselves to induce an epi-reaction - they may develop convulsions after severe intoxication due to fatigue or skipping meals. In children, an example of epileptic reactions is convulsions against a background of high (febrile) temperature - febrile convulsions (see special recommendations “FEBRILIC CONVESSIONS”).
“INFANTRY” IS NOT A DIAGNOSIS
The word “infantile” is sometimes used to describe seizures in infants. It is believed that these attacks occur only in young children, and will not recur at an older age. There is some truth in this, since the smaller the child, the easier his brain reacts with an epi-discharge (epi-reaction) to any harm - high temperature, transmitted disease, rickets, etc.
With age, the tendency to react to these factors with seizures decreases and in many children the seizures no longer recur. However, epilepsy can also begin from the first months of life. Seizures in the first year of life can also be a manifestation of a wide variety of brain diseases.
EPIC SYNDROME WHAT IS IT AND HOW DOES IT MANIFEST (SYMPTOMATIC EPILEPSY)
Changes in the electrical activity of brain cells can be caused by any brain disease (tumor, encephalitis, hydrocephalus, etc.), and can also be a consequence of any brain damage (head injury, oxygen starvation, brain hypoxia).
Such damage can occur before the baby is born, during childbirth, and then throughout the life of the child or adult. Therefore, when attacks occur, it is necessary to check a child or adult for all these and many other diseases, since, if they are present, these diseases must be treated first as a cause, and only then their consequence in the form of attacks.
If the patient is diagnosed with such brain diseases, then an additional diagnosis is made regarding the attacks: “episyndrome”. According to the modern international classification of seizures and epilepsy, episyndrome is now called “symptomatic epilepsy” - meaning that the seizures themselves are only a symptom of some other brain disease.
WHAT IS EPILEPSY
However, for most people with seizures, careful examination reveals no disease or significant brain damage that can be treated to eliminate the cause of the seizures and thus the seizures themselves. In this case, repeated, regularly recurring seizures are simply a congenital or acquired feature of a given brain - idiopathic epilepsy (according to the modern international classification).
The word “idiopathy” translated from Greek means “a painful disorder that occurs for no apparent reason.” This tendency of the brain to have seizures does not always appear in the first years of life - the first seizures in epilepsy (its debut) may appear for the first time after the age of majority.
Modern science has accumulated a lot of data on why some people have repeated attacks for no apparent reason. This feature of the brain is a consequence of various combinations of various factors in the prenatal period of brain development, during childbirth and in the process of further brain development after childbirth.
With the help of some modern, very expensive devices, it is possible to detect subtle changes in certain layers of neurons that have occurred due to the influence of these factors. However, despite the high cost of this type of research, the information obtained with their help does not change anything in the tactics of the treatment and does little to predict attacks.
Some hereditary predisposition to the development of seizures is also possible, although only a few rare forms of epilepsy are purely hereditary (the issue of heredity is described in more detail in the Recommendations “PROBLEMS OF FAMILY LIFE AND MARRIAGE IN EPILEPSY.”
REFLECTOR EPILEPSY
Most often, seizures in epilepsy occur on their own – from “internal” reasons. With the so-called REFLECTOR, quite rare, epilepsy, seizures can be provoked by various external factors, which, by themselves, never cause seizures in other people.
Such a triggering factor can be a light (“photo” in Latin) stimulus: flickering (flashing) light, black and white contrasts (see details in the recommendations “PHOTOGENIC EPILEPSY”). Less commonly, attacks are provoked by sound stimuli (unexpected sounds), sharp touch, etc.
Some other “external” causes and influences can also contribute to the occurrence of a particular seizure (provoke it). You should carefully look for these provoking factors and suspicious circumstances that preceded the next attack and record them in the diary of attacks (for this, read and follow another Recommendation “WHAT TYPES OF ATTACKS ARE AND HOW THEY DEVELOP” and “LIFESTYLE DURING EPI-ATTACKS”).
DO YOU OR YOUR CHILD HAVE EPILEPSY? WHAT DIAGNOSIS SHOULD BE MADE – CORRECT OR “CONVENIENT”?
People who are illiterate in matters of epilepsy, including many doctors, in all cases of epilepsy consider it, firstly, to be an incurable disease for life, and secondly, necessarily leading to mental and mental degradation. This is wrong. Firstly, in the modern international classification there is, for example, a diagnosis such as “Benign infantile myoclonic epilepsy,” which goes away on its own without any treatment.
Secondly, Alexander the Great, Socrates, Julius Caesar, Peter I, Dostoevsky, Napoleon, and the founder of the Nobel Prize, Alfred Nobel, had epilepsy. Therefore, the contemporaries of these greats believed that people with epilepsy, on the contrary, have special mental abilities.
For example, in ancient times epilepsy was called “Hercules disease.” Epilepsy is more common than diabetes, tuberculosis or other well-known diseases. There are more than 500 thousand people with epilepsy in Ukraine. Due to the illiteracy of people, the diagnosis of “epilepsy” puts a certain stamp on a person, which can subsequently cause the wrong attitude of others towards him.
Therefore, in the presence of even obvious epilepsy, when making a diagnosis, I usually limit myself to an accurate and detailed diagnosis of the type of seizure, which is necessary for proper treatment, and if it is necessary to issue any official certificates, I try to make do with the term “epi-syndrome” even in the presence of a valid diagnosis of epilepsy.
FORECAST OF SEIZURES AND CHANCES OF RECOVERY
Both the patients with seizures themselves and their loved ones are interested in the main thing - whether the threat of repeated seizures remains for the rest of their lives and whether they can be completely cured (prognosis of seizures). According to average statistical data, for one person who actually suffers from epilepsy, there are 10 such people who within There was only one seizure in my life.
Only 30 percent of those who have had one seizure will have a second one in the next 3 years. After the second seizure, the risk of their recurrence increases to 75 percent. These are statistics, and each individual case is individual. Therefore, even with one single attack, I can sometimes predict a completely different percentage of probability for a particular patient.
Most patients and their loved ones associate a patient’s poor prognosis with a diagnosis of epilepsy, as opposed to a diagnosis of epi-syndrome. However, most often epilepsy is “better” than epi-syndrome, which must also include some serious brain disease.
In general, both good and not very good prognosis of seizures can occur in both epilepsy and epi-syndrome. There are benign forms of epilepsy itself, which are cured in 90-95% of cases. The prognosis depends on the type of attacks and many other characteristics that I determine in the patient.
Determining the prognosis requires special knowledge and a lot of time - and therefore cannot be carried out by a doctor at a regular appointment in a clinic. In the process of selecting treatment and monitoring its effectiveness, the accuracy of the prognosis can be significantly increased.
If the nature of the attacks is such that the tendency to recur may remain for life, this is a significant inconvenience, but not a tragedy: according to foreign scientists, the correct selection of antiepileptic drugs allows epilepsy to be controlled in 70-80 percent of cases.
Causes of epilepsy
The development of epilepsy is influenced by numerous causes. Predisposition to epilepsy can be hereditary or acquired.
In the first case, the disease develops due to genetic dysfunction of brain neurons. This feature is passed on from generation to generation.
Acquired predisposition is associated with pathologies and brain injuries.
Diseases that cause epilepsy include:
- cerebral hemorrhages;
- meningitis;
- encephalitis;
- toxic damage to the organ structure;
- cysts;
- malignant formations;
- brain aneurysms.
Each of these diseases develops as a result of biochemical and metabolic disorders in brain cells, which cause low excitability of neurons. A group of affected neurons unites into an epileptic focus. Over time, new structures are involved in the pathological process.
Clinically, the condition manifests itself as motor, mental or autonomic seizures. The symptoms of the disease depend on the area of the brain that has been damaged.
Treatment options
The doctor selects the treatment method individually, based on various data: causes and age.
- Adults are prescribed:
- Tranquilizers to relax muscles.
- Anticonvulsants to reduce the frequency of seizures.
- Sometimes surgery.
- Herbal medicine. Medicinal herbs and plants: linden, violet, celandine, wild rosemary, oregano.
- Diet: less liquid, smoked and salty foods.
- For children:
- A special diet high in fat and low in protein. This forces the body to consider fat as its only source of energy, converting it into ketone bodies, which in turn leads to a decrease in the regularity of seizures.
- Normalization of potassium-calcium balance in the body.
- Mandatory use of antipyretics at high temperatures.
- Phytotherapy.
For a complete cure, it is necessary to eliminate the underlying causes, only then will a truly effective result be obtained.
Common symptoms
3.1. Major attacks
Seizures begin with an involuntary contraction or loss of sensation in the hands and feet and spread to other parts of the body, developing into a seizure. The condition is characterized by successive phases:
- Harbingers . A few minutes before the seizure, the patient develops anxiety syndrome. Abnormal neuronal activity increases and covers new sections.
- Toxic seizures . Characterized by sharp tension in all muscle groups. The patient lies down on the floor and arches his back. There is a bluish discoloration of the face due to oxygen deficiency. The duration of the phase is from 30 seconds to 1 minute.
- Clinical seizures . Muscles contract involuntarily and quickly. A characteristic sign of the phase is foam at the mouth. Within 5 minutes the patient’s breathing is restored and the bluishness of the face disappears.
- Stupor . After abnormal brain activity, brain inhibition occurs. The phase is characterized by relaxation of all muscle groups. The patient loses control of consciousness. The duration of stupor is 30 minutes.
- Dream . After an attack, a person may suffer from headaches and movement disorders for 2-3 days.
3.2. Minor attacks
The condition is characterized by a vague clinical picture. The patient's muscles in the face and other parts of the body involuntarily contract. During an attack, the person is conscious, but may temporarily experience stupor. He does not notice the neurological changes occurring.
3.3. Status epilepticus
The disease is associated with a series of seizures and requires professional help, since epileptic seizures provoke swelling and hypoxia of the brain. Symptoms come on suddenly and end spontaneously.
From history and statistics
In ancient times, epilepsy was treated very warily, considering it a mental illness. Such people were avoided and humiliated in every possible way, believing that this disease was “from the devil.”
Many countries with a low level of civilization have not changed their attitude towards this disease to this day, although the achievements of modern medicine have refuted the groundlessness of such stereotypical thinking.
New therapeutic approaches to treatment have radically changed public views in developed countries and contributed to positive social adaptation and alleviation of somatic suffering in patients with epilepsy.
According to doctors, epilepsy is a chronic disorder of brain activity with specific clinical changes in the form of seizures. According to WHO statistics, about 50 million people worldwide suffer from this disease.
Approximately their number ranges from 4 to 9 cases per 1000 people. More than half of patients live in countries with low living standards. Epilepsy cannot be diagnosed with just one seizure. As a rule, they occur more often with a certain gap in time.
Convulsive seizures manifest themselves involuntarily and briefly in the form of involuntary spasms of any part of the body, or the whole body.
Often such convulsive states are accompanied by loss of consciousness, vomiting, and convulsions of the limbs. Seizures can occur at any time of the day. Depending on the clinical course of the disease (main or concomitant), their number ranges from one per year to several paroxysmal seizures per day.
The number of epileptics has increased significantly in the last decade, so research in this area continues. Especially in countries with low living standards (from 7-14 per 1000 people).
Every year, 2.3 million people around the world are diagnosed with epilepsy.
Outbreaks of the disease are typical for countries with a high risk of endogenous organic diseases, low level of medical care (birth injuries, lack of emergency assistance in road accidents, financial difficulties in obtaining quality medical care). In 65% of cases, epilepsy can be treated with medication.
4. Features of the study for epilepsy
Diagnosis of chronic forms of epilepsy is difficult. The cause of pathology in childhood is severe infectious diseases and defects of the organ cortex. Microstructural abnormalities are detected only with the help of contrast agents and special scanning modes, which are not used for survey MRI. For targeted research, thinner sections are needed - 2-3 mm and a device with a power of at least 3 Tesla.
To increase the effectiveness of the study, the patient undergoes electroencephalography before MRI. The procedure identifies the area of the brain in which the pathological focus is located.
What does an MRI show for epilepsy?
Most often, resonance imaging for epilepsy reveals sclerosis of the hippocampus.
The disease is characterized by several MR signs: high-intensity signals from the area of gliosis on T2 images and hippocampal atrophy on T1 images. These signs of the disease can be combined with each other or appear separately.
Another cause of epilepsy is benign tumors. Formations are detected by MRI with contrast. Pathological areas actively accumulate contrast (which is clearly visible in the images) and have a cystic component in their structure.
Perifocal edema is not typical for benign tumors, but sometimes there are calcifications that can only be diagnosed using CT. The figure shows an image of a small ganglioma with a cystic component.
MRI image of a gangliomas with a cystic component
MRI diagnoses degenerative changes in the brain that form in children during fetal development in the form of encephalomalacia. Epilepsy in adults often develops against the background of post-traumatic scars, which is also detected by resonance imaging.
Indications for MRI in epilepsy
Epilepsy can be congenital or acquired. MRI is performed for the following symptoms:
- temporary loss of consciousness and orientation in space;
- impairment of visual and auditory functions;
- involuntary muscle contractions;
- spontaneous head nodding.
It is a mistake to believe that epilepsy is always accompanied by seizures. This disease can manifest itself in different ways. In some patients, epilepsy is expressed by asymptomatic seizures, which are difficult to diagnose without a set of specialized measures. Mild forms of the disease are expressed by nervous tics and head twitching. The duration of such attacks ranges from 5-20 seconds, which makes them invisible to surrounding people.
MRI diagnostics to detect epilepsy are also prescribed for people who suffer from severe headaches, speech disorders and sleep disorders. Signs indicate the development of a common neurological pathology. The procedure is indicated for children who often wake up from nightmares.
How does epilepsy differ from episyndrome?
Epilepsy in various forms is diagnosed in 10% of the population, including children. The main symptom of the pathology is seizures. There is another neurological disease similar to epilepsy - episyndrome. How do pathologies differ from each other, and what danger do they pose to humans?
Epilepsy is a chronic disorder characterized by sudden attacks. The problem is characterized by increased excitation of neurons to the highest degree. Episyndrome manifests itself as a result of any brain disease and does not have a chronic course. The attacks are sporadic. In most patients, after an exacerbation of the episyndrome, a phase of long-term remission is observed.
Symptomatic epilepsy develops due to:
- tumors and head injuries;
- purulent processes in the membranes of the brain;
- degenerative processes in brain vessels associated with age-related characteristics.
Differences
When considering diseases such as episyndrome and epilepsy, what is the difference between these problems is what is important to talk about. After all, although these are diseases that are similar in symptoms, they still differ significantly. To put it briefly and as simply as possible, episyndrome is a problem that is easier and simpler than epilepsy.
The symptoms may be similar, but all signs manifest themselves to varying degrees. We also must not forget that episyndrome is a consequence of a previously diagnosed disease, and epilepsy is an independent disease, which, moreover, affects the neuropsychic system. But that's not all.
We further consider diseases such as episyndrome and epilepsy. What else is the difference between these problems? So, doctors say that in the first case the problem is acquired after a previous illness. In the second case, epilepsy is often a congenital problem, although it can also be acquired.
MRI for episyndrome
An MRI of the brain is prescribed if the cause of the episyndrome cannot be determined by other methods. An alternative diagnostic method is CT, but unlike MRI, it exposes the body to radiation.
The magnetic field of the tomograph interacts with hydrogen atoms located in the soft and bone structures of the human body. Arranging in a certain sequence, molecules and atoms produce a certain signal in response to magnetic interaction. These signals enter the tomograph coil and are converted into a black and white image. Signals from different structures and organs differ in intensity. Clear images of the area under study are obtained in 3 projections. MRI is considered the most effective technique for identifying episyndrome caused by traumatic, degenerative and dystrophic changes in the structures of the brain.
Diagnosis of the disease
Diagnosing a patient with “epileptic syndrome” is only an intermediate stage of diagnosis. Next, you should identify the root cause of the development of this condition. At the moment, the following methods are used to search for the underlying disease:
- MRI. The effectiveness of the procedure is based on the creation of a strong magnetic field. The technology allows us to identify pathologies of bone and muscle structures.
- CT. Involves the use of x-rays. The technique differs from traditional radiography in higher quality images.
- Electroencephalogram. The technique allows you to record seizures and determine their location.