Psychiatry
More than 45 million people are affected by the disease. Schizophrenia has its own stages and types, as well as characteristic signs, the occurrence of which should consult a doctor.
The name of the disease “schizophrenia” is translated from Greek as “split thinking.” The disease belongs to the group of mental disorders, and is also characterized as a separate polymorphic mental disorder of an endogenous nature. The term was first used by Eugen Bleuler in 1908.
History of schizophrenia
At the beginning of the 19th century there was a term for a mentally ill person - insane, insane. The rapid growth of industry and the achievements of natural sciences led to an increase in the value of life. The attention of doctors was attracted by the possibility of treating the insane, and attempts arose to classify mental illnesses. Thus, the German psychiatrist Kahlbaum described catatonia in young patients. Mental disorder in the form of incorrect statements and judgments subsequently leads to lethargy, stiffness, and sometimes the impossibility of movement. Sometimes motor agitation develops, with monotonous movements, manifestations of aggressiveness, or ridiculous actions. The catatonic person temporarily freezes in a fixed position, sometimes bizarre and unusual, communication with him is difficult or impossible, he is immersed in his own world.
Hecker described hebephrenia, also characteristic of young people, associated with clownish behavior, antics and grimaces, excitement with elements of clownery. Endless giggles and antics protect the hebephrenic from the real world around him.
Dim identified a simple form of dementia, dementia simplex, which consists of a gradual impoverishment of mental life with a gradual attenuation of interests, motivations and activity.
| Kraepelin Emil (1856-1926) German psychiatrist, student of Wundt, author of the first classification of mental illnesses |
| Kretschmer Ernst (1888–1964) German psychiatrist and psychologist, studied with Kraepelin, interned with Gaupp. The most famous work is “Body Structure and Character” |
At the end of the 19th century, Emil Kraepelin, over the course of long-term, long-term observations, established that disorders with different symptoms develop according to a similar pattern within the framework of dementia precox, dementia praecox, and lead to malignant damage to the psyche, which psychiatrists later called nuclear schizophrenia.
Later it was found that, along with the juvenile, most severe and clearly diagnosable form, there is a disorder, the symptom of which is delusions of persecution, influence, relationships, etc., which develops in adulthood, 25-30 years old, this is the paranoid form of schizophrenia.
Eugen Bleuler in 1911 proposed dividing “dementia precox” into four subgroups: paranoid form, catatonia, hebephrenia and simple schizophrenia. Bleuler also studied the latent form of schizophrenia, which he first described in the relatives of patients. It was he who proposed the name “schizophrenia,” which translated means splitting of the mind.
So, let's come to the definition of schizophrenia. This is a mental illness that manifests itself in the splitting of thinking, feelings, perceptions, relationships with the outside world, leading to the construction of a bizarre picture of the world, connected into a semblance of a whole by unusual logic. Unusual perception gives rise to inadequate emotions. A schizophrenic is characterized by illogical thinking, behavior and absurdity of statements.
You often hear about a strange person: schizo, schizophrenic, schizoid. The frequency of use of a word is not related to correct understanding or interpretation. In everyday understanding, the concept of schizophrenia is distorted and label-like.
When examining a patient, a psychiatrist collects a mosaic from the mass of symptoms, the whole picture is compared with the diagnostic original, the main thing is highlighted and accompanying secondary signs are eliminated.
So, forward to the signs of the disease. I will describe them in harsh psychiatric language. Kurt Schneider, a German psychiatrist, in the 30s of the 20th century, identified symptoms of the first rank, the most important and significant, for schizophrenia:
- openness of thought to others, the feeling that thoughts become known at a distance, without communication, without contact;
- involuntary flow of thoughts, the presence of external control of thoughts, insertion and withdrawal of thoughts, a sense of influence;
- voices inside the patient's head, or auditory pseudohallucinations;
- real perceptions are organized into a false system that does not correspond to reality; there is its own delusional reality, supported by bizarre logic.
The great Russian psychiatrist Viktor Kandinsky first used the concept of pseudohallucinations, and identified the difference from true hallucinations, similar to real sensations. This is difficult to understand. I'll try to explain. Imagine that you are dreaming. Now imagine that in a dream you know that you are dreaming. That's the difference. The schizophrenic feels the foreignness, imposition and external origin of the voices. Kandinsky noted that voices are perceived directly by the brain, as if coming from the patient’s head. The doctor himself suffered several attacks of paranoid schizophrenia and committed suicide at the age of 40.
Along with these symptoms, consciousness in malignant forms of the disease formally remains clear, there is often no amnesia, but thinking changes most of all, for example, one’s own unconventional logic is present, the concepts of main and secondary, similar and different change, and clear boundaries of definitions are blurred. The speed of flow and sequence of thoughts changes, and control over one’s own thoughts may be completely lost.
Emotions become dull or paradoxical. An event that is sad for an ordinary person causes revival and joy. A joyful event causes sadness. Dullness or poverty of emotions is expressed in indifference, in this case the reaction to an event that is important for an ordinary person is equal to the reaction to a minor, secondary one. Spit in your eyes - God's dew. Literally.
The great Russian physiologist Ivan.P. Pavlov , studying patients with schizophrenia, noted the distortion of the simplest sensations and reflexes. The schizophrenic tried a quinine solution and showed pleasure; the sugar solution caused a grimace of disgust.
Historical era, social status, occupation, religious practice are reflected in the content of delirium.
In the modern picture of symptoms of the paranoid form of schizophrenia, one encounters, first of all, delusions of persecution from the CIA, the Ministry of Internal Affairs, the FSB, from scientific organizations or alien entities in order to establish surveillance or conduct an experiment on the patient. The stereotype of a powerful organization, a powerful and authoritative subject turns into an influencing image that exists in the mind of the patient. Let's call this image an operator. The patient expects the operator’s actions to cause damage and is confident of his danger to himself. There is also an expectation of a positive result from the operator’s influence, but such experiences are described less frequently.
| Kandinsky Viktor Khrisanfovich (1849–1889) Russian psychiatrist. Famous work: “On pseudohallucinations” |
| Eugen Bleuler (1857–1939) Swiss psychiatrist and pathopsychologist. Author of the term "schizophrenia" |
So, the patient strives to close the windows and lock all the doors. He may believe that listening devices are installed everywhere, that the TV announcer is transmitting his thoughts directly to him. The neighbor somehow doesn’t look at it that way; he probably already knows everything.
What about psychotronic weapons and generators? The desire to hide from influence leads to withdrawal or isolation. However, the work inside the patient's head does not stop for a minute. There is a constant game or struggle with the operator. He needs to be outsmarted, deceived; he is a competent opponent. On the one hand, his intentions are known, and one can guess about his upcoming actions. On the other hand, constant struggle and competition lead to exhaustion of strength.
Of course, the intellectual qualities of the operator depend on the personality of the patient before the illness. From his level of education, from the problems that the patient faced in his previous “healthy” life. If the patient worked as a dishwasher and had an intelligence corresponding to the activity, then the operator will most likely seem unattractive and uninteresting, just boring.
Imagine, what if the patient’s education and field of activity before illness were related to science, art, and the latest technologies? Then the patient’s operator will be extraordinary. Colored. Multimedia. It turns out to be simply a fascinating competition, a single combat with an active and vibrant opponent. It is truly captivating and completely absorbing.
The patient often tries to hide his hallucinations from others, and the doctor sometimes can only guess about their existence based on indirect signs. This could be facial expressions, a conversation without an interlocutor.
When there are several operators, they can perform theater or a large-format picture in front of the patient. They compete with each other for the right to exercise external control over the patient's thoughts and actions. This is exactly what happened to Barbara. Along with the formidable schizo operators, there were also less dangerous subjects with whom she talked, consulted and listened to their conversations with each other. Some threatened her, while others gave her very useful recommendations.
The operators lived their own lives, lurking and intriguing. They were engaged in “hooking”, plotting each other, stepping over defeated rivals, almost the same as employees of the company where Barbara worked before her illness. Having found such a connection with the events of her past life, she decided that it was the imperfection of human relationships, the experience of this feeling of competition that became the cause of her illness.
Diversity of the schizophrenia spectrum
Despite the fact that several main and most typical types of disease are usually distinguished, about 50 different diagnoses can be found in ICD-10. Their diversity is explained by the fact that the concept of schizophrenia has very wide boundaries. And almost every individual case of the disorder has individual manifestations or an atypical course. If undifferentiated schizophrenia is characterized by polymorphism of symptoms (a combination of criteria for different forms), then an atypical disease is diagnosed when the general picture of schizophrenia is evident, but the symptoms do not meet the criteria of any of the identified types of disorder.
The nature of the disease manifestation also depends on the age of onset of manifestation. Pediatric forms often have an atypical clinical picture, so in ICD-10 they are classified as a separate category. If schizophrenia begins in childhood or adolescence, its features are manifestations of hebephrenia and a malignant type of course. First psychosis in late life is often confused with senile dementia caused by neurodegenerative diseases. In general, the onset of the disease in old age is very rare. Its peculiarity is a paranoid or hypochondriacal clinical picture. More often, the senile form of schizophrenia is a relapse after many years of remission, and the onset of the disease was simply not noticed.
Separately, it is worth paying attention to such a type of disorder as senestopathic schizophrenia. Its development occurs very slowly and usually in adulthood. Symptoms are limited to painful sensations in various parts and organs of the body, the schizophrenic defect is weakly expressed.
What actually causes schizophrenia?
Statistics on identical twins indicate that when schizophrenia develops in one, the disease occurs in the other with a probability of 50-70%. If the twins are fraternal, then the probability decreases to 15-20%. It is known that the coincidence of the gene set of identical twins is complete. So, there is a hereditary predisposition. If one of the parents is sick, the probability of the child getting sick is 15-17%; if both parents are sick, the risk increases to 40%.
Other studies aimed at considering the psychogenic factor, namely upbringing, lead to data that children from a sick parent, raised in other, mentally normal families, still subsequently get sick in 17% of cases. On the contrary, children from healthy parents who found themselves in a family where one of the parents was sick grew up healthy. The results of these studies speak in favor of the genetic nature of schizophrenia, without excluding the influence of internal and external psychogenic factors on the development of the disease.
There is a term “schizophrenogenic mother”, who is overly protective, protective, but at the same time cold towards her child. Just like the mother from “The Wall” by Pink Floyd. Such a mother will not cause the child’s illness if she herself is not a carrier of the gene.
So, there are genes associated with schizophrenia, they are inherited. However, there is extensive evidence that children of sick parents remain healthy throughout their lives. This indicates the presence of a mechanism for triggering the function of these genes, initiation. There are three known reasons that can activate the gene.
1. Exposure to a chemical. For example, a single dose of LSD can cause schizophrenia. 2. It is believed that various factors of psychogenic origin: stress, strong negative experiences, can push the carrier of the genes towards the ladder of the disease. 3. In genetics, the trigger mechanism is also known as a result of interaction with other genes.
In this regard, let us note what productive and negative symptoms are.
Productive symptoms are usually those that are associated with the appearance in the psyche of something that should not normally be present in it. Productive symptoms are the so-called plus symptoms, that is, symptoms associated with the appearance in the psyche of something that should not be there. Here you can highlight a variety of symptoms, but the main, most important ones are various neurotic symptoms, various symptoms of personality disorders, as well as such productive symptoms as delusions, hallucinations, affective disorders (depression or mania). This is pathological production.
Negative symptoms or minus symptoms are symptoms associated, first of all, with the loss of what should be normal. That is, if something that should normally be present in the psyche disappears, these are negative symptoms (negative symptoms). What are the negative symptoms? Negative symptoms are: autism - that is, withdrawal or building a barrier between oneself and the world, withdrawal into the inner world, if there is one (although it may turn out that there is nothing inside autism either), refusal to contact reality; emotional impoverishment (impoverishment of the emotional sphere); apathy (loss of mood); abulia (lack of will). Also negative are some thinking disorders, namely those disorders that are associated with a weakening of motive, impaired motivation, and a tendency to fragmented thinking.
Kraepelin named the new nosological unit dementia praecox because the main pattern in the course of these diseases generalized into one unit was that the increase in negative symptoms occurs gradually and as a result leads to a personality defect, literally to the early, premature death of the individual. With this condition, literally several years pass, and we see the defective personality of a schizophrenic - a person without emotions, without motivation, with reduced energy potential and broken thinking.
A personality defect is a set of negative symptoms, the result of a certain process of impoverishment, impoverishment of the psyche and personality.
The term dementia praecox allowed us to distinguish schizophrenic dementia from dementia that occurs in older patients with age. This dementia was called early, only on the basis that it can occur at the beginning of adolescence, long before old age, and this, according to Kraepelin, constitutes the essence of dementiae præcox.
However, this term did not catch on and in 1911 another psychiatrist, Eugen Bleuler, published a monograph called “Dementia praecox or group of schizophrenia.” It was Eugen Bleuler who introduced the concept of “schizophrenia” (“schizophrenia” literally translates as “splitting of the soul”). Bleuler was significantly influenced by Freud through Jung, while he worked in Zurich as Jung's assistant and accepted a great deal of psychoanalytic teaching. He paid attention not so much to the prognosis and clinic, like Kraepelin, but to the psychological mechanisms that underlie this condition.
The main psychological mechanism of schizophrenia according to Bleuler is splitting, or “schisis” (the term translates as splitting or divergence in different directions). The point is that Bleuler considered schisis to be the central negative symptom of schizophrenia.
With schisis, individual mental functions work on their own, the possibility of connection in communication is lost. Bleuler considered ambivalence (both love and hate at the same time) and ambitendence as a manifestation of schisis.
A schizophrenic often loves and hates his relatives at the same time . For example, hatred of his father or mother (I love and hate at the same time) is a very suspicious symptom that makes one think about the person’s mental state. An example of the manifestation of schizis can be disgust brought to the point of absurdity (if once a cat ate from this plate, then the woman will not eat from it for the rest of her life, although the plate can be washed), which can be combined with sloppiness and total cluttering of the apartment.
Example. The patient worked as a cleaner and performed her duties perfectly, but at the same time there was a dump at home. In addition, cats lived in the house and relieved themselves wherever necessary. Neighbors periodically complained about yellow stains appearing on the ceilings and the stench from this apartment.
To designate this kind of combination of incompatible things, there is a term - a combination of incompatible things, and this condition is very characteristic of schizophrenia. The combination of the incongruous can manifest itself in the fact that a person is absolutely weak-willed.
For example, he has completely cluttered his apartment and does nothing to fix it; it is difficult for him to force himself to do anything at all, but at the same time, due to some delusional motives, he can be very, very strong-willed in one area: “I I believe that they are persecuting me and want to take away my apartment, and therefore I spend a lot of energy on actions that are related to protecting myself from these persecutors.”
Such a person may move from city to city, change or sell an apartment and buy another, because he thinks that he is being hunted. These rather complex actions require a colossal mental load for a normal person, but patients with schizophrenia do this persistently and repeatedly. This so-called parabulia - a distortion of the will - is a vivid example of schism, an example of a combination of incompatible things. Apathy and abulia are also characteristic of schizophrenics. For example, if a woman has never used cosmetics in her entire life, or has stopped using it, stopped taking care of herself, or cleaning the house, then such signs may be associated with a disease.
How to treat and cure
The first reaction to encountering madness is usually a feeling of anxiety and danger. Based on this, the first attempts at treatment made by ancient doctors consisted of the use of extreme influences, which were supposed to push the madman to adequacy. They used blows with a stick or snake bites. Remember the expression “snake pit”? Various herbs with natural calming properties and magical effects were widely used.
During the period of growth and development of capitalism in Europe and America, uselessness and maladaptation, and especially the aggressive actions of the insane led to their imprisonment and detention in inhuman conditions.
New methods used in the treatment of schizophrenia in the mid-20th century included electric shock and brain surgery.
Nowadays, when a diagnosis of schizophrenia is made, antipsychotics, chemical compounds that alter the transmission of nerve impulses, are prescribed. Antipsychotics unfortunately cause a number of side effects, such as anxiety, weakness, muscle spasms and tics. Activity and volitional qualities are temporarily suppressed. Despite the side effects of these medications, their use is the main means of relief. For depressed mood, antidepressants are also prescribed. The psychiatrist monitors the dosage of medications, and if the condition improves, the dose is reduced.
In order to reduce the risk of suicide or accident, ensure timely administration of medications and the possibility of constant monitoring, the patient is placed in a hospital. The aggressive behavior of some patients may also be a reason. The voice can order the patient to deal with someone or himself. And the schizophrenic will obey the order of the imperative operator.
Treatment may result in remission and return to normal activities. However, after remission, an exacerbation of schizophrenia may begin.
Spontaneous remissions, like Barbara’s, also occur without taking medications. Recovery with a residual defect of varying severity also happens. A defect is considered to be a persistent impairment of thinking, speech, emotions and manifestations of autism and isolation.
Note that with modern methods it is impossible to exclude a gene from the body. The predisposition to schizophrenia remains. It’s like a herpes retrovirus, written into the genome for the rest of its life after invasion. The only difference is that schizophrenia cannot be contracted.
When I asked Professor Polishchuk about the schizoid character, I received the answer that here it is, a sleeping gene, and this is how it manifests itself. Half-heartedly. Quarter strength.
Freud believed that the connections between the libido and external objects in a schizophrenic person are disrupted. Therefore, a psychoanalyst and a schizophrenic cannot get along, and treatment with psychoanalytic methods during an exacerbation does not produce results.
A psychotherapist can help a patient who has already emerged from a crisis state. Restoring relationships with others, treating depression, helping with feelings of loneliness and helplessness, social adaptation - this is where psychologists and classes in a special rehabilitation group are needed. There are various approaches, for example, creative expression psychotherapy, but this is the subject of another article. You can teach how to live and talk with voices - set aside visiting hours for them, from 9-00 to 10-00. The approach of family psychotherapy is also useful. First of all, loved ones need to realize that the reality of a schizophrenic really exists, it must be respected. There is also hope for restoration of relationships if relatives know more about the disease, apply the right communication tactics, and show patience, attention and understanding of the experiences of their loved one.
The most current recommendations suggest an integrated approach: a combination of medications, psychotherapy and social support programs. But the state program is one thing, the attitude of society, manifestations of intolerance and xenophobia are another matter. How can we eliminate the stigma of a schizophrenic and his rejection by society?
There was one interesting and instructive fact in the writer’s medical history. As soon as she discovered voices inside her head, one of the operators advised her to leave her permanent place and travel. Barbara followed his advice. Therefore, none of the neighbors, colleagues and relatives ever found out what exactly happened to her. The doctor Barbara consulted was in one of the towns of her schizophrenic trip, far from her home. Fortunately, the attack-like schizophrenia resulted in a gradual recovery, she was able to start working and successfully advanced her career. If anyone around him knew the truth, they would have to forget about the service and new positions.
One of Barbara’s main thoughts is that it was humor, optimism and an ironic perception of reality and oneself that were significant helpers, both during illness and in recovery.
Now about prevention. A competent geneticist approach to family counseling identifies risk. Parents decide whether to take risks or not. When raising children with hereditary conditions, the harmonious development and assistance of parents and psychologists in resolving traumatic situations is of particular importance.
Cost of treatment in our clinic
| Service | Price | |
| Ambulatory treatment | ||
| Psychiatrist consultation | 4 000 ₽ | |
| Consultation with a psychotherapist | 4 000 ₽ | |
| Psychodiagnostics extended | 6 000 ₽ | |
| Consultation with a psychiatrist at home | 3 800 ₽ | |
| Treatment in hospital | ||
| Delivery to hospital | For free | |
| Standard room | 6 900 ₽ | |
| 3-bed superior room | 9 400 ₽ | |
| 2-bed superior room | 12 000 ₽ | |
| 1 local VIP chamber | 16 000 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Myths about schizophrenia
- There is a gene that determines predisposition to schizophrenia.
In fact, one gene has not been identified. It is assumed that there must be a set of genes, a polygenic predisposition, but this is just an assumption.
- Schizophrenia is forever.
If the symptoms manifest themselves clearly, then the likelihood of going into remission is high. In addition, there is no reason to say that no one was cured.
- Schizophrenia is a split personality.
Split personality – this manifestation corresponds to another mental disorder, dissociative disorder, and it itself does not always manifest itself the way it does in Hollywood films. Schizophrenia manifests itself in a splitting of connections with reality.
There are other myths about schizophrenia. For example, the assumption of a schizophrenogenic mother. Rather, raising a child by such a mother will lead to schizoid accentuation, to schizoid manifestations in character, but not to a psychiatric diagnosis.
Mosaic psychopathy and schizophrenia
With mosaic psychopathy, a person experiences a number of symptoms that make it difficult for him to be in society. Periodically, one or another psychopathic disorder predominates, which makes it difficult to make an accurate diagnosis.
Mosaic psychopathy may have the following symptoms:
- various forms of addiction (alcohol, drugs, gaming);
- increased temper and initiative - a person feels that his rights and interests are constantly being infringed. A striking example would be individuals who constantly write complaints to all authorities with or without reason;
- the emergence of extremely valuable ideas.
If there is a combination of several criteria that are opposite in terms of psychopathic types, then the doctor has every reason to believe that the patient may be developing schizophrenia. The main goal is to prevent the development of a disease that makes it impossible for a person to be in society.
Schizophrenia leads to disability
It is impossible to predict at what age the disease will begin. Head injuries, stress, death of loved ones, and drug use can contribute to the occurrence. Any of these factors, superimposed on genetically altered soil, causes neurotransmitter disorders, which leads to the onset of the disease. The prognosis directly depends on the type of schizophrenia.
The childhood type of schizophrenia is very difficult. The course of the disease is continuous and symptoms increase. The child gets “stuck” in development and hobbies at the age of onset of the disease. Hebephrenic behavior appears and there is no sense of distance. Motor disturbances are typical - the child may continuously bang his head against the wall, walk around the room in circles, ignore requests, or scream. From a very early age, children with schizophrenia are helpless and require constant supervision and care from adults. They are unteachable, have little contact, and become disabled early and for life.
When the disease begins in middle age, the disease is often paroxysmal. Moreover, this can be either a single case in a lifetime or periodically recurring attacks of the same type. A mild episode of the disease can occur in adolescence and is called “lightning”. More often, its presence is assessed retrospectively. The symptom complex in most cases is represented by hallucinatory and affective-delusional symptoms. After the cessation of psychosis and the onset of remission, with well-chosen treatment, such people can work successfully, even occupy leadership positions. A different picture is observed with frequent attacks. With each new phase, the symptoms deepen and change the personality more strongly. A person quickly loses socialization, due to thinking disorders and hallucinations, from an able-bodied member of society, unfortunately, he turns into a disabled person. People with severe personality disorder and the absence of caring relatives end up in boarding schools for the mentally ill, where they live for a long time and receive treatment.
Classification of the disease: main types, stages of schizophrenia
There are 3 types of schizophrenia, classified according to the course of the disease: continuous, periodic and paroxysmal-progressive:
- Continuous schizophrenia includes cases of the disease with a smooth development of the disease process, a clear delineation of its clinical varieties according to the degree of progression from mildly expressed personality changes to gross progression (both positive and negative symptoms are expressed). This type of course is prognostically the most unfavorable;
- Periodic (recurrent) schizophrenia is characterized by the presence of phases in the development of the disease with the appearance of time-limited attacks. Personality changes are not pronounced. In the foreground of the clinical picture are affective symptoms: irritability, anxiety, depression, hypomania, mania. During a lifetime, one or several attacks are possible;
- An intermediate place between these types of course is occupied by paroxysmal-progressive schizophrenia, when, against the background of a continuous process, attacks appear, the clinical picture of which is determined by syndromes similar to attacks of recurrent schizophrenia. With each new attack, the personality defect becomes larger, as if a “split” of the psyche actually occurs.
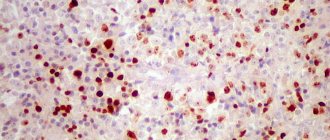
Hallucinations are one of the most striking productive symptoms of schizophrenia.
Hallucinations are an individual’s distorted perception of the surrounding reality, when a person hears, sees, or touches something that is not really there. This distinguishes hallucinations from illusions. A hallucinating patient can simultaneously perceive reality adequately along with false images. The patient, for example, during a conversation with the doctor Fr. In this case, attention is distributed unevenly, often shifting towards deceptions of perception. Sometimes a person is so absorbed in non-existent images that he completely ignores reality. In such cases they speak of detachment or hallucinatory overload.
Most often, auditory hallucinations occur with schizophrenia; a person may think that voices are sounding in his head or coming from external objects. Voices may be threatening, commanding, or commentary. There can be one or several voices, male or female. Conversations or individual phrases can take place at any time of the day. The content of hallucinatory statements may be absurd, devoid of any meaning, but for the most part they express various ideas that are not always indifferent to patients. A dangerous type of auditory deception for others and the patients themselves are imperative hallucinations containing orders to do something or prohibitions on actions. Patients often take the orders of their voices personally. Voices may prohibit eating, and a person may refuse food for days and resist feeding. There are often cases when voices order to hit and even kill themselves or strangers. In addition to voices, non-verbal auditory hallucinations (acoasms) in the form of noise, crackling, clicking, knocking are also possible. During hallucinations of musical content, the patient hears the playing of musical instruments, singing, and choirs.
Signs of auditory hallucinations:
- a person during a conversation suddenly becomes silent, listens to something, covers his ears, looks around;
- a person talks to an imaginary interlocutor;
- sudden, causeless laughter;
- inability to concentrate on the conversation, inappropriate answers, isolation.
Tactile hallucinations are possible, usually of an elaborate, unpleasant, painful nature, called senestopathies (for example, “worms are eating the heart; the brain is rubbing against the skull; the stomach seems to be turned out; the feeling that the organs are rotten”). The body may seem alien, this is how depersonalization manifests itself. Algic senestopathies are pain sensations characterized by an extraordinary richness of all possible shades: drilling, burning, sharp, dull, bursting, squeezing, tearing, breaking, piercing, aching, itching, twisting, pulling, gnawing, breaking, cutting, shooting, etc. One and the same patient can have very different types of algic sensations. Sometimes patients group unpleasant sensations in a certain way in order to understand them themselves, inform the doctor more fully about their well-being, and even record their manifestations, location and time of occurrence in a special notebook. The pain can be constant or occur in the form of attacks, short-term paroxysms, be localized in one part of the body for several years or appear in different places.
Olfactory and gustatory hallucinations are not similar to the perceived ordinary reality, are unusual and also extremely unpleasant, intrusive (“the taste of burnt paper in the mouth; the smell of kerosene”). By their behavior, patients can detect these hallucinations: closing windows, spitting saliva, etc.
Visual hallucinations in schizophrenia appear less frequently than auditory hallucinations. Visual hallucinations vary in color, size, clarity of contours and details, degree of similarity to real objects, mobility, and localization in space. As a rule, these are visions of long-dead relatives, strangers, aliens, animals, wires, cobwebs.
Hallucinations are dangerous; a patient in psychosis can harm himself or the people around him, commit illegal and socially dangerous actions. In this case, according to the Law on Psychiatric Care of the Russian Federation, involuntary hospitalization in the inpatient department of a psychiatric hospital is necessary in order to relieve acute psychotic symptoms.