Classification
All over the world, doctors identify several forms of the disease. For example, primary forms include the following types:
- Huntington's chorea.
- Neuroacancytosis, or choreoacanthocytosis.
- Benign - non-progressive hereditary form.
- Lesch-Nyhan disease.
Secondary forms can be caused by autoimmune diseases, infections, metabolic disorders, brain damage, and intoxication. That is, here the disease begins to manifest itself against the background of some other pathology, which became the trigger. You can see exactly what the disease looks like in a photo on the Internet.
But there is another classification of chorea disease. In this case, the following types are distinguished:
- Hereditary, which includes Huntington's chorea, hereditary non-progressive with early onset and chronic with late onset.
- Occurring in extrapyramidal diseases.
- Secondary forms.
However, no matter what classification it belongs to, almost all types of this disease have the same symptoms.
Causes
This disease cannot appear out of nowhere. It has its own reasons, the most common of which is heredity. The most famous Huntington's chorea belongs to this type, but there are several other types that can also be inherited.
Other reasons include:
- Brain injuries.
- Infectious and viral diseases.
- Vascular pathology.
- Decreased immunity.
- Intoxication.
- Metabolic disorders.
- Rheumatism.
- Chronic tonsillitis.
- Cerebral palsy.
- SCV.
In some cases, pregnancy becomes the trigger. However, a healthy woman will not develop such a pathology during pregnancy. It will begin to manifest itself only if the woman suffered minor chorea in childhood. The first signs begin to appear in the first months of pregnancy, after prolonged and frequent sore throats. Often in this case it is necessary to terminate the pregnancy.
The rheumatic form often occurs, which is most often diagnosed in children. It occurs during exacerbation of rheumatism and in the presence of endocarditis, and significant damage to the heart valves occurs.
Causes of minor chorea
Minor chorea most often progresses at 10-12 years of age, against the background of a previous streptococcal infection (tonsillitis, pharyngitis or tonsillitis), after the appearance of complications of infectious processes. Rheumatism can provoke the development of the disease. Experts note a hereditary or family predisposition to the progression of the disease. Modern neurology has not yet fully studied the nature of this neurological disorder. Research is still underway in this area, which should reveal all the features of chorea minor and many other neurological disorders.
Establishing a diagnosis
The most reliable method for detecting pathology is a molecular genetic study. The most common material for analysis is blood from a vein. The reliability of this technique reaches 99%. To identify a mutated gene, PCR (polymerase chain reaction) is prescribed, during which venous blood is examined. This study will help calculate the number of repetitions of CAG; if there are more than 36, then we are talking about Huntington's disease.
Pathology can be detected during pregnancy or IVF (during the selection of embryos for fertilization). The PCR method is also used for this purpose.
If you suspect Huntington's chorea, you should visit a neurologist. The doctor will take a medical history and perform neurological tests.
To identify pathological changes in the brain, instrumental studies are prescribed:
Parkinson's disease and its causes
- Computed tomography is used to assess the functionality of the brain and can identify abnormalities in it.
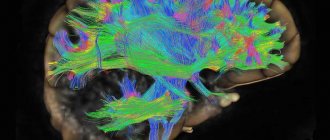
- Magnetic resonance imaging is a more informative method than CT. In addition to assessing the state of the brain, MRI allows you to examine the myelin sheath of the nerves and identify or exclude autoimmune diseases.
- PET (positron emission tomography) is a highly informative method that allows you to assess the intensity of metabolism and transport of substances in the central nervous system. During the procedure, a radiopharmaceutical is injected into the patient's vein, which accumulates in the areas of the most intense metabolism. This technique allows you to identify hereditary chorea in the early stages even before the first symptoms appear.
Electroencephalography will evaluate the electrical activity of the brain.
Main manifestations
Chorea has its characteristic symptoms.
And the first thing you should pay attention to is the sweeping movements of the arms and legs, which are not controlled by consciousness. This condition is called choreic hyperkinesis. Upon examination, a decrease in muscle tone can be detected. Grimacing is often noted, which also does not depend on the person’s consciousness. Increased gesticulation may be observed, and the person cannot help but move his hands during a conversation. Another important diagnostic sign is a lack of coordination of movement. The patient is unable to stand normally, he has disturbances in his gait, and it becomes “dancing.”
When communicating with other people, you can notice many unnecessary movements - sighs, smacking, sniffling and much more. Even in complete rest, a person does not stop twitching his head. All these symptoms can completely disappear during sleep, but after waking up and during emotional stress they all intensify several times.
In addition to the above symptoms, dementia, decreased memory and attention, general anxiety, absent-mindedness, aggressiveness, and handwriting disorders are noted. At the same time, voluntary movements, that is, those controlled by consciousness, are very difficult. Chorea in children has almost the same symptoms, but they are not as severe.
As for the duration of development of pathology, it is always different. For example, rheumatic chorea in children does not appear immediately and proceeds very slowly, and recovery occurs after 1 - 3 months, but the disease can develop in the presence of an unfavorable factor. As for such a genetic disease as Huntington's chorea, it lasts from 5 to 10 years and in any case ends in death.
Minor chorea in children: causes, symptoms, forms, diagnosis and treatment
Chorea minor is a neurological rheumatic disease that occurs as a complication of tonsillitis in children and adolescents.
The name of the disease has other names: rheumatic chorea, neurorheumatism, Sydenham's chorea (in honor of the English scientist who first described the symptoms in detail back in the 17th century.
), as well as an even more ancient one - the dance of St. Vitus. By its nature, this is a type of encephalitis of a rheumatic nature.
The ICD-10 code for rheumatic chorea is I02. The disease is extremely rare in medical practice. Diagnosed between the ages of 5 and 15 years, more often in girls than boys. Chorea minor in adults usually develops against the background of systemic lupus erythematosus in the form of vasculitis of the central nervous system.
Lesser chorea: how does the disease manifest?
The main signs of the disorder are excessive uncontrolled motor activity and behavioral disorders.
Signs of Sydenham's chorea:
- grimacing;
- uncontrolled head movements;
- “dancing” movements and gait;
- decreased muscle tone;
- aimless uncontrolled movements of arms and legs;
- difficulties in making targeted movements;
- deterioration of handwriting;
- unclear pronunciation;
- impaired coordination of movements;
- memory impairment;
- possible increase in body temperature.
Prognosis and prevention for chorea minor
In children and young people under the age of 25, cases of secondary chorea are possible. In order to exclude relapses of the disease, you need to carefully monitor the child’s health and strengthen his immunity. The baby needs proper nutrition, hardening, and timely treatment of colds and other diseases.
To prevent the disease, long-acting drugs are used. Usually these are antibiotics from the penicillin series (bicillin-5, benzathine-benzylpenicillin).
Their injections are given once every 3-4 weeks, which makes it possible to neutralize group A β-hemolytic streptococcus. Such prophylaxis can be carried out for several (on average 3-5) years.
Thanks to the use of these drugs in medicine, cases of repeated minor chorea have been significantly reduced.
If preventive measures are not taken, then after a relapse the disease can become chronic. In addition, chorea minor can cause complications associated with heart pathologies:
- heart disease;
- aortic insufficiency;
- mitral stenosis.
Rheumatic chorea is not a fatal disease. But its complications are fraught with serious disturbances in the functioning of the heart, which can lead to death over time.
However, most patients with Sydenham's chorea make a full recovery. With proper treatment, the disease can go away in 5-6 weeks. In some cases, the course of the disease drags on for up to a year or two, but such cases are rare.
Methods for diagnosing chorea
To diagnose Henington's chorea or rheumatic chorea, you need to undergo a series of tests. To prescribe the correct treatment for chorea, a blood test will be required. Based on its results, you can determine whether the level of white blood cells is high or low, as well as whether a streptococcal infection is present. Rheumatoid causes of chorea can also be detected by blood. In the process of diagnosing Henington's chorea, the doctor will definitely study the medical history of the parents of the sick child to determine whether heredity is the cause of its exacerbation.
During the examination, an electroencephalogram and magnetic resonance imaging are used. Chorea in children and adults is also diagnosed using computed tomography.
Complications
As already mentioned, the disease manifests itself as hyperkinesis, so the patient is not able to control his body. This risks injury and asphyxia (suffocation) while eating. There is a possibility of airway obstruction, which can lead to death of the patient.
In the later stages of hereditary chorea, dementia develops
Due to mental disorders, the patient develops obsessive ideas, suicidal tendencies, and inappropriate actions. In later stages, hallucinations occur and dementia develops.
Some time after the first symptoms of Huntington's disease appear, a person loses the ability to care for himself. In addition, during pathology, the risk of pneumonia and heart failure increases, which can lead to death.
Complications and consequences
Fatal outcomes as a result of complications of minor chorea are isolated cases in medical practice.
If the disease is not treated fully and in a timely manner, then the main complications will concern the cardiovascular system, brain and nervous system of the child’s body.
In some cases, a severe degree of pathology can provoke critical physical exhaustion of the child.
The consequences of minor chorea can be the following conditions:
- acquired heart defects;
- dysfunction of the cerebral cortex;
- aortic insufficiency;
- regular muscle tics;
- mitral stenosis;
- violation of social adaptation;
- persistent neurological abnormalities.
Clinical picture of Huntington's chorea and forms of the disease
If Huntington's chorea began at age 30, this is typical, since the first symptoms are observed at this age. The disease can take about 15 years to progress. On average, patients are between 20 and 50 years old. Some people mistakenly define the disease as Huntington's encephalopathy, which causes swelling of the brain. However, such a symptom appears only when this organ is infected.
The ICD 10 code is defined as G10. When describing the clinical picture of typical Huntington's chorea, four main forms are distinguished:
- Hyperkinetic. It develops slowly and leads to emotional disorders: inattention, apathy, irritability, antisocial behavior. The patient often commits illogical actions and cannot concentrate on a specific subject. Involuntary movements of the limbs, tongue, and head are noted. The gait changes: the legs are either wide apart or clenched at the hips. A sharp motor activity appears—hyperkinesis. They are observed during periods of strong mental stress.
- Akinetic-rigid. This is the last stage of the disease, which is characterized by vegetative exhaustion of the body. By this time, hyperkinesis disappears, and unusual reflexes appear. An unstable mental state is noted, the person experiences hallucinations.
- Juvenile form. It affects children and young people, who make up 10% of the total number of cases. Most often this occurs in families where Huntington's disease can be traced for several generations in a row. Hyperkinesis in this form is mild, but involuntary movements are present.
- Mental. Identified very rarely, the patient experiences emotional disturbances, paranoid ideas, and delusions of grandeur for several years. Hyperkinesis is almost completely absent. A person behaves aggressively towards others and suffers from irritability.
REFERENCE! The mental form of chorea is often confused with schizophrenia; the patient is placed in a special institution, where he receives the wrong treatment.
Causes of chorea in children. Symptoms of the disease, diagnosis and treatment methods
Chorea is involuntary obsessive movements of the face, head and limbs. Movements are sudden, shaking or swinging, unrelated. Strictly speaking, chorea is not an independent disease. It is a symptom of many diseases of various kinds and intoxications, including those of a medicinal nature.
Symptoms
Chorea of any origin is manifested by obsessive movements that are not controlled by the patient. It is very typical for her symptoms to disappear during sleep.
There are many diseases, one of the manifestations of which is chorea. Its symptoms differ depending on the etiological factor:
- Chorea in cerebral palsy appears from an early age and is characterized by obsessive movements of the limbs of small amplitude and facial muscles.
- Konovalov-Wilson disease (hereditary pathology of copper metabolism with its excessive accumulation in the liver, cornea and nervous tissue). Accompanied by characteristic sweeping choreic hyperkinesis.
- Sydenham's chorea is especially common in children. This is a disease of the rheumatoid type, developing after a bacterial sore throat (caused by streptococcus) or a streptococcal infection of another localization (streptoderma, erysipelas). It is characterized by a selective effect on the facial muscles, manifested by sticking out the tongue and grimacing.
- Huntington's chorea is a genetically determined disease that manifests itself in wide sweeping movements that are compared to dancing. Huntington's chorea occurs at older ages, usually between 20 and 25 years of age. In rare cases, an earlier onset in adolescence is possible.
Classification of chorea in children
Chorea is divided into types depending on the speed of development of the process:
- Acute - caused by acute damaging effects - intoxication, strokes. Symptoms of chorea can be caused by an overdose of antihistamines, anticonvulsants, various stimulants, lithium preparations, and antiemetics. In adults, intoxication with oral contraceptives is also possible. In rare cases, chorea in children can be caused by hemorrhage in the basal ganglia area of the brain.
- Subacute chorea develops over several weeks to a month. In children, the most common form of this group is Sindeham's chorea. As the disease develops, chorea progresses, emotional instability joins it and muscle tone decreases. Also, chorea with gradual development may be the result of a brain tumor, an early manifestation of lupus in a child, or a symptom of endocrine diseases, in particular Addison's disease.
- Chronic chorea in children in most cases is one of the early manifestations of Huntington's disease. It also serves as a characteristic sign of ataxia-telangiectasia. Thanks to the progress of medicine, chronic chorea due to kernicterus suffered in the first month of life practically does not occur.
Treatment of chorea
It is extremely important to identify the disease of which chorea is a symptom. Its treatment is entirely determined by the cause:
- For Huntington's chorea, antipsychotics and tranquilizers are indicated to reduce the severity of obsessive movements. However, due to the hereditary nature of the disease, complete recovery in this case is impossible. Systematic therapy will help reduce the severity of hyperkinesis and significantly slow down its progression.
- Urgent withdrawal of drugs, an overdose of which caused chorea, if it is impossible to cancel them, reduce the dose.
- Prescription of corticosteroids for vasculitis.
- Copper-binding drugs for Konovalov-Wilson disease.
- If other methods are ineffective, surgical treatment is possible - separation of the basal ganglia. Currently, this method is rarely used.
Additionally, for chorea of any etiology, nootropics, neurotrophic drugs and B vitamins are prescribed.
In most cases, the prognosis for chorea is favorable. Long-term treatment is likely to be required and must be strictly monitored. In the absence of hereditary or organic pathology, a complete cure is possible.
Other symptoms of chorea minor
- Decreased muscle tone. Most often, a decrease in tone corresponds to the localization of hyperkinesis. But there are forms of minor chorea when there are almost no signs of hyperkinesis, and muscle tone is so low that the child becomes practically immobilized.
- Psycho-emotional disorders. Often this symptom is the first alarming sign of this disease, but such manifestations are associated with minor chorea only after the manifestation of hyperkinesis. The child behaves inappropriately, often cries and is capricious, there is frequent forgetfulness and lack of concentration. In some cases, on the contrary, the child shows apathy towards the world around him and becomes lethargic.
When contacting a neurologist, the doctor may identify several more symptoms during examination and testing of the child:
- The Gordon phenomenon. When testing the knee reflex, the leg freezes for several seconds in an extended position (hyperkinesis of the femoral muscle).
- “Symptom of flabby shoulders” - when a sick child is lifted by the armpits, his head sinks heavily into his shoulders.
- “Chameleon tongue” - a child cannot keep his tongue out if his eyes are closed.
- “Charic hand” - with outstretched arms, a special arrangement of the hands appears.
Chorea: how to treat?
Patients with chorea are subject to hospitalization, as they require the most careful care.
Medical nutrition
The subject of special care is their feeding. Food should be easily digestible and high in calories. It is necessary to exclude chocolate, cocoa, coffee, spices, and strong meat broths, as they excite the nervous system.
Drug treatment
Since involuntary muscle contractions stop during sleep, patients should be prescribed sedatives and hypnotics (bromides, luminal). Children under 12 years of age are prescribed Luminal - 0.01-0.02 two times during the day, and at night - at a dose of 0.05. In cases of severe anxiety, intravenous administration of a 10% sodium bromide solution in an amount of 5-10 ml is indicated.
Arsenic has a good effect on chorea, which is prescribed either in the form of a Fowler solution (6-12 drops per dose) or in combination with antipyrine according to the following recipe:
Rp. Natrii arsenici 0.06
Antipyrini 5.0
Syr. Corticio Aurantii 50.0
Aq. destill. 100.0
M.D.S. 1 tablespoon 3 times a day for older children
In the acute period of the disease, taking into account its infectious-toxic nature, intravenous administration of methenamine (2-3 ml of 40% solution), as well as salicylates, pyramidon (0.25-0.4 several times a day) are prescribed. Salicylic sodium in combination with methenamine and adonylene can be prescribed according to the following prescription:
Rp. Adonileni 4.0
Sodium salicylici 8.0
Urotropini 4.0
Aq. Menthae 200.0
M.D.S. Children from 5 to 8 years old: 1 teaspoon 3-4 times a day, from 8 to 12 years old - a dessert spoon, over 12 years old - a tablespoon
Good results are obtained by intramuscular injections of a 20% solution of magnesium sulfate, starting with 1 ml and increasing to 3-10 ml once every 2-3 days.
Features of the disease in children
The hormonal factor that plays a role in the development of rheumatic chorea explains the reason for its more frequent occurrence in childhood and adolescence. It is during this period of life that the body most often undergoes hormonal changes. Girls get sick more often than boys for the same reason. It is the female body that experiences major hormonal surges up to the age of 15, and if this is accompanied by weak immunity, the risk of getting chorea increases.
A peculiarity of the disease in children of preschool and school age is frequent errors in the interpretation of symptoms. Behavioral manifestations of the disease are extremely difficult to distinguish from ordinary children's pranks, disobedience, and self-indulgence. Often children are punished for grimaces, ridiculous movements, whims, etc., not knowing that there is an illness behind all this. This is difficult for adults to deal with. On the one hand, not every naughty child has chorea, but on the other hand, an ill child often cannot control the abnormalities of his behavior.
Forecast and prevention of Huntington's chorea
Without proper medical care, the disease often has complications, including pneumonia and upper respiratory tract diseases, heart failure, and serious mental disorders. In addition, a person can injure himself due to careless movement of his limbs. The listed complications in most cases become the causes of death.
If you see a doctor early, life expectancy is about 50 years. This is provided that the disease manifested itself at the age of 30 years. If a person has suffered from Huntington's chorea since childhood, then the prognosis is not so comforting: he can live only 10-15 years from the moment the first symptoms appear.
There is no specific prevention. In general, you should adhere to the following basic rules to reduce the risk of complications:
- Healthy food;
- eliminate bad habits;
- undergo regular examination by a neurologist;
- reduce stress;
- get enough rest.
What is the disease?
Chorea is involuntary, obsessive movements of the trunk and limbs. The movements are characterized by a sudden swinging nature, they are uncontrollable and look jerky. The twitching may be slightly noticeable, but may also be overly aggressive. The disease is also called St. Vitus's dance, because when the muscles of the body twitch, the hands and fingers tremble, the child becomes like a dancing man.
As a rule, children aged 5-12 years are more susceptible to chorea. It is noteworthy that girls are noticeably more common among sick people than boys.
Today it has been proven that the disease affects not only the nervous system - it leads to pathological changes in the functioning of the heart. As a result, rheumatism may well develop. In general, some doctors tend to classify chorea as a type of rheumatism.
It is important to note that sometimes chorea is just a symptom of a more complex disease, and can also be an indicator of intoxication of the child’s body (food poisoning or drug overdose).
Don't let the disease recur!
As a rule, chorea can reoccur in a child due to a number of reasons. It is especially important to ensure that the body is not weakened. Overwork, infectious diseases and excessive worry may well lead to a surge in recurrent illness. Sometimes it seems to parents that the recovered child is in no hurry to delve into their adult affairs. This is not entirely true. The slightest quarrel between mom and dad can return the child to a state in which signs of chorea begin to appear.
What is chorea
The term “chorea” defines a pathological condition in which a person experiences involuntary, rapid, sudden movements in one muscle or in an entire muscle group. They can be either one- or two-sided, but they are still not consistent with each other. Such movements are called hyperkinesis. Most often, non-stereotypical, erratic movements occur in the muscle groups of the upper or lower extremities.
Chorea is manifested by sudden involuntary movements in different muscle groups
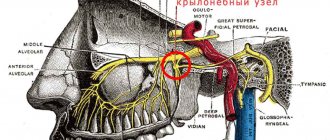
Hyperkinesis with chorea occurs due to damage to the neurons of the basal ganglia (nuclei) of the brain. This anatomical structure includes the striatum, substantia nigra, globus pallidus, and some nuclei of the diencephalon and midbrain. It is these areas that are responsible for neuromuscular regulation and voluntary human movements.
Chorea develops due to damage to basal ganglia neurons
The causes of damage to neurons can be various factors - heredity, various diseases, injuries, etc.
In neurology, primary and secondary forms of the disease are distinguished.
Chorea disease: treatment
Unfortunately, scientists have not yet been able to find a cure that completely cures this insidious disease. The course of treatment is symptomatic and supportive. As a rule, sedative and antipsychotic drugs are prescribed. In severe forms of the disease, tranquilizers may be prescribed to relieve depression and make the person more manageable. With rheumatic chorea, it is better to register the patient at the dispensary.
Treatment
A child who has shown signs of chorea must be admitted to a hospital to be under the constant supervision of specialists. Mental and physical peace is a must! In addition, such children must certainly receive affectionate treatment from others, including doctors and clinic staff.
Treatment recommended by a professional must be followed exactly as chorea, especially Genington's chorea, is prone to recurrence. By adhering to all prescriptions, parents can protect their child from developing a severe form of the disease.
The therapy needed to treat a child with chorea includes medication. As a rule, sedative, antiviral, antipsychotic and anti-inflammatory drugs are prescribed. Medications to improve brain function and those that promote vasodilation may be indicated.
The therapy also includes physiotherapeutic procedures and pine baths.
The success of treatment depends on the speed of action and the correctness of the prescribed treatment. If the form of the disease appears to be advanced, surgical intervention may be applicable. However, today, when there are many truly high-quality medications, and diagnostic methods make it possible to promptly detect the slightest signs of the development of the disease, surgery is extremely rarely resorted to.
An important factor for the speedy recovery of a child diagnosed with chorea is a review of nutrition. It should be complete, but you shouldn’t overfeed either.
Hardening and all kinds of health promotion methods also play a big role in recovery.
Modern methods of treating chorea
If there is an underlying disease that has led to the development of hyperkinetic syndrome, efforts are directed towards eliminating it. Treatment of chorea takes place, depending on the patient’s condition, in an inpatient or outpatient setting. In case of drug or toxic pathology, the first step is to stop taking the drug and eliminate the influence of the external factor that adversely affected the body.
For autoimmune pathology, long-term therapy with immunosuppressants is used, which inhibit the production of antibodies to brain cells. Metabolic diseases require dietary adjustments and specific medications. For neoplasms, chemotherapy or radiotherapy is used. Sometimes radical surgery to remove the tumor is indicated. For vascular diseases and strokes, long-term rehabilitation is carried out with the prevention of new exacerbations.
Specific treatment for chorea includes the newer drug Tetrabenazine. It is an inhibitor of the vesicular monoamine transporter and can suppress movement disorders. Take the drug in long courses. Significant disadvantages of the drug are the inability to use it for depression, which often accompanies chorea, and the high market price, which makes it inaccessible to a large number of patients.
In combination, neuroleptics (antipsychotic drugs) are used, which can somewhat reduce the manifestations of the disease, as well as emotional and mental symptoms. In practice, the following are most often prescribed:
- Risperidone;
- Olanzapine;
- Amisulpride;
- Clozapine;
- Aripiprazole.
Another group of drugs that are often prescribed are benzodiazepines. They can reduce symptoms of insomnia, emotional disorders and panic attacks. However, with prolonged use, patients become dependent on the drugs, which limits the timing of their use. One of the following medications is prescribed:
- Alprazolam;
- Flunitrazepam;
- Conazepam;
- Lorezepam;
- Nitrazepam;
- Temazepam.
Antiparkinsonian drugs are also used for long-term treatment of movement disorders. They increase the concentration of dopamine in the basal ganglia of the brain, one of the most important neurotransmitters in the human body, which has an inhibitory function and helps reduce the severity of involuntary movements. Patients are prescribed:
- Madopar;
- On whom;
- Sindopa;
- Sinemet;
- Tremonorm;
- Levocarbidopa;
- Tidomet.
What is the prognosis for the lives of patients with Pick's disease?
Learn about treatment methods. Read how extrapyramidal hyperkinesis manifests itself. Features of the treatment of pathology.Purposes of brain tomography. What are CT and MRI?
Chorea disease in childrenTreatment of a child - childhood diseases, consultations, experience
The cause of the primary forms of pathology lies in genetic disorders. Certain chromosomal defects cause damage to various neurons of the basal ganglia and, ultimately, the development of one of the variants of primary chorea.
The following factors can lead to the development of secondary forms of the disease:
- infections: whooping cough;
- meningitis;
- borreliosis;
- viral encephalitis;
- neurosyphilis;
- HIV;
- autoimmune pathologies:
- rheumatism;
- lupus erythematosus;
- antiphospholipid syndrome;
- inadequate response of the body to immunization;
- exchange (metabolic) disorders: hypo- or hyperglycemia due to diabetes;
- atherosclerosis of cerebral vessels;
How does the pathology manifest itself?
The symptoms of chorea minor are quite specific and the disease can be diagnosed already at the dawn of its development.
Lesser chorea, being a “juvenile” anomaly, develops extremely rarely after puberty. Girls are again at risk. Minor chorea almost never occurs in adult young ladies. The exception is individuals who are prone to relapses during pregnancy.
Main signs
The main symptoms of minor chorea include uncontrolled motor passages. They are expressed in nervous twitching of the upper and lower extremities, which is called choreic hyperkinesis in medicine.
According to some researchers of this pathology, rheumatic cardiac anomalies can develop against the background of minor chorea.
The fact that girls are more susceptible to this disease is explained by the influence of female hormones.
Clinical signs
Subsequently, the symptoms of minor chorea manifest themselves in:
- Muscle weakness.
- Impaired motor coordination.
- The presence of choreic hyperkinesis.
A sick child moves quickly, but not rhythmically. Motor passages are characterized by roughness, awkwardness and random distribution. From the outside it seems that the movements are very “ragged”.
Hyperkinesis can be either symmetrical or unilateral. They are expressed in facial expressions, feet, and hands. Laryngeal hyperkinesis is very common. Against this background, a person suffers from slurred speech and swallowing is impaired.
The muscles of the trunk are rarely involved in hyperkinesis. In this case, rapid, almost interrupted breathing is observed. The severity of abnormal manifestations may vary. In some cases, there is a slight grimacing. Sometimes the patient suffers from violent pathological motor passages.
Symptoms
Manifestations of choreic hyperkinesis differ somewhat depending on the form of the disease.
But they also have common signs: involuntary chaotic movements of the limbs, having a twisting nature, forced squats, crossings, intertwining of arms and legs, facial hyperkinesis, gait disturbances. Movements can occur only on one side, in which case we are talking about hemichorea, for example, with a stroke.
Choreic hyperkinesis has similar manifestations in any form of pathology
Hyperkinesis can be:
- focal (isolated disorders of any function), for example, oral hyperkinesis in the case of senile chorea or the initial stage of neuroacanthocytosis;
- generalized (spread throughout the body) - with minor or benign hereditary chorea.
The patient does not experience hyperkinesis during sleep.
A distinctive feature of chorea is hyperkinesis of the facial muscles
Chorea can develop acutely or gradually. Rapid onset suggests an autoimmune, vascular, or metabolic disease. The gradual and slow addition of symptoms indicates the neurodegenerative, often hereditary, nature of the pathology.
Table: symptoms of the main types of chorea
| Name | Characteristic signs |
| Huntington's chorea |
|
| Chorea |
|
| Chorea of pregnancy | Clinical manifestations resemble those of rheumatic chorea |
| Benign chorea |
|
| Chorea in vascular pathology |
|
| Drug chorea | The disorder develops several months or years after starting to take the drug (usually antipsychotics, dopamine receptor antagonists). Accompanied by dystonia (muscle spasms) or other dyskinesias, including internal organs. Most often, symptoms reverse when the drug is discontinued. |
| Chorea due to autoimmune pathologies |
|
With progressive forms of chorea, mental and intellectual impairments are irreversible. A person completely loses control over his body and becomes dependent on others.
Story
An engraving by Hendrik Hondius depicts three women stricken by the dancing plague
The term “trochea” comes from ancient Greek. χορός - dance, dance.
At first, the meaning of this term differed from the modern one: since the 13th century, “chorea” (“choreomania”) was a psychogenic movement disorder - dissociative convulsions, sometimes widespread among the medieval population in the form of “”.
Groups of people afflicted with dance mania performed dance-like movements amidst a narrowed consciousness, probably venting the nervous shock caused by the plague epidemics.
St. Vitus became associated with chorea for several reasons. In the 9th century, after miracles that occurred during the transfer of his relics from Saint-Denis to Saxony, the cult of this saint arose as the patron saint of patients suffering from epilepsy and chorea.
People with these disorders went on a pilgrimage to one church or another on the Feast of St. Vitus and danced there to overcome their fears and pain. In the 16th century, a belief spread in the Holy Roman Empire that whoever danced in front of a statue of a saint on his name day (June 15) would receive a charge of vigor for the whole year.
Therefore, on this day, many people danced emotionally near such statues. Residents of Strasbourg, gripped by the dancing plague in 1518, were directed by the magistrate to the chapel of St. Vitus in Zabern (now Saverne
), where their “healing” took place.
For the first time, separately from psychogenic types of chorea, minor chorea under the name chorea naturalis (from Latin - ““real” chorea”) was described in the 16th century. Paracelsus. Children suffering from rheumatic chorea were first described by Gregor Horst (German) in 1625.
One of the names of chorea comes from St. Vitus, a Roman martyr of the early Christian period.
Thomas Sydenham in 1686 first identified rheumatic chorea as a separate childhood disease and a special form of hyperkinesis, and also very accurately and in detail described its main symptoms.
As a synonym, he used the term “St. Vitus’s dance,” which from that time began to have a new meaning.
This caused some confusion, since the same term also meant organic disease ( minor
, or English chorea
), and psychogenic disorder (
big
, or
German chorea
). Despite the fact that Sydenham also described rheumatic fever and its joint symptoms, he did not find a connection between it and chorea.
The English physician Bright first identified chorea minor as a manifestation of rheumatism in 1831. However, chorea minor finally became a delineated nosological entity only in the second half of the 19th century. In the late 1860s, J. Jackson and W. Broadbent (eng.
) determined that the cause of Sydenham's chorea is dysfunction of the striatum.
In 1887, William Osler presented 410 clinical cases of rheumatic chorea, and in 1894 he published the monograph “On Chorea and Choreiform Affections” - one of the most widely cited North American studies of the 19th century, which showed its connection with rheumatoid arthritis and endocarditis.
Based on the results of studies conducted in the 1920s, scientists suggested that chorea minor was a bacterial meningoencephalitis. In 1976, research by G. Husby and his colleagues demonstrated that Sydenham's chorea is not caused by infection per se, but is the result of a violation of immune mechanisms.
Diagnostic methods
Before making a diagnosis, the neurologist conducts a comprehensive examination of the patient:
- collecting anamnesis and analyzing complaints: were there any cases of the disease in relatives;
- timing of the appearance of involuntary movements;
- whether certain drugs were used for a long time;
- what the patient was sick with before the onset of symptoms (sore throat, rheumatism, childhood infections, viral diseases);
- assessment of movements (amplitude, direction, symmetry) and reflexes;
Before diagnosing chorea, the neurologist carefully examines the patient
Source: https://rptp-rd.ru/rasstrojstva/revmaticheskaya-horeya-u-detej-proyavlyaetsya.html
Diagnostic algorithm for chorea
At the slightest suspicion of the development of hyperkinetic syndrome in a patient, he is referred for an appointment or consultation with a neurologist. The hospital conducts comprehensive neurological testing, identifies pathological symptoms and prescribes the following tests to the patient:
- general blood and urine analysis;
- blood chemistry;
- computed tomography (CT) of the brain;
- magnetic resonance imaging (MRI);
- positron emission tomography (PET);
- genetic examination (if a hereditary pathology is suspected).
Symptoms of rheumatic chorea
At the very beginning of the disease, symptoms are almost invisible. Parents regard the child's grimaces as pranks. Then involuntary movements of the arms and legs appear. There are main manifestations of the disease:
- rapid and sweeping twitching of the limbs;
- sudden change of mood;
- gait disturbance;
- twitching of the muscles of the face and neck;
- nodding head;
- sleep disturbance;
- seizures;
- change in handwriting;
- increased fatigue;
- disturbance of emotions (unreasonable laughter or crying);
- deterioration of memory and attention;
- Gordon's symptom (when the knee reflex is evoked, the patient's leg remains extended for some time).
The disease occurs in the form of hyperkinesis attacks. One of the more common is hyperkinesis of the larynx and tongue. Because of this, correct speech is impaired and swallowing becomes difficult. Rarely there is hyperkinesis of the diaphragm, which entails intermittent and irregular breathing. Typically, hyperkinesis lasts from 3-6 months, rarely the disease can progress for 1-2 years. Muscle hypotonia also occurs.
General information
Chorea minor is a disease that manifests itself in the form of hyperkinesis, developing as a result of damage to the structures responsible for muscle tone and coordination of movements. Treatment of the pathological process is within the competence of the neurologist. The disease is most often detected in childhood against the background of rheumatic changes. Girls get sick more often - this is due to the hormonal characteristics of the body and the production of female sex hormones. Of greatest importance during the course of the disease is the involvement of the cerebellum and striatal structures of the brain in the pathological process. The duration of a choreic attack is approximately 12 weeks, and can last up to 5-6 months, less often for years (1-2). Relapses of the disease are possible.
Types and forms of pathology
There are 2 types of hereditary chorea:
- Classic. Clinical manifestations are observed after 35 years. The pathology is transmitted from one of the parents and progresses slowly. Sometimes it happens that characteristic symptoms appear too late, so the patient is not even aware of his condition. In this case, he may die from another disease.
- Westphalian option. This type of pathology occurs in 7–10% of all cases. The mutated gene is passed on through the paternal line. Most often, the disease manifests itself after 20 years. This type of Huntington's chorea is characterized by rapid development.
Reference. With Westphal variant disease, characteristic symptoms are observed in the first or second decade of life. The youngest patient who suffered from this type of pathology was 3 years old.
In addition, the following forms of pathology are distinguished:
- Classic. The main clinical manifestations are hyperkinesis (involuntary, chaotic movements).
- Akinetic-rigid. This variant of the disease is characterized by increased muscle tone, and hyperkinesis is practically invisible.
- Mental. The disease is manifested by mental disorders, for example, weakening of memory, slowing of thought processes, and increased irritability.
As you can see, each form of Huntington's disease has different clinical manifestations.
Symptoms
Chorea may be manifested by the child's grimacing and awkward movements.
Clinical manifestations usually occur several weeks after a sore throat or tonsillitis. Less commonly, the disease manifests itself without preliminary signs of upper respiratory tract infections, which happens when β-hemolytic streptococcus has settled in the body unnoticed.
The duration of minor chorea is on average about 3 months, sometimes dragging on for 1-2 years. In 1/3 of people who have had the disease, relapses of minor chorea are possible after puberty and up to 25 years.
In its morphological essence, chorea minor is rheumatic encephalitis with damage to the basal ganglia of the brain.
The main manifestations of minor chorea include chorea hyperkinesis : involuntary movements. These are fast, non-rhythmic, randomly distributed, chaotic muscle contractions that occur against the will of a person and, accordingly, cannot be controlled by him. Choreic hyperkinesis can involve various parts of the body: hands, face, entire limbs, larynx and tongue, diaphragm, entire torso. Usually, at the beginning of the disease, hyperkinesis is barely noticeable (clumsiness of the fingers, slight grimacing, which is perceived as a child’s prank), and intensifies with excitement. Gradually, their prevalence increases, they become more pronounced in amplitude, up to the so-called “choreic storm”, when uncontrolled movements occur in paroxysms throughout the body.
Causes of chorea minor
Rheumatic chorea is caused by a pathogen from the streptococcus family - group A hemological streptococcus. Children and adolescents with tonsillitis and upper respiratory tract infections are automatically included in the risk group for this disease.
However, angina is complicated by the development of chorea not in all patients. Most of those who have suffered tonsillitis, sore throat, and upper respiratory tract infections soon recover safely. Why do some people suffer from further complications? There are a number of factors that can provoke minor chorea. These include:
- hereditary predisposition;
- weak immune system;
- dental problems (untreated caries);
- the presence of rheumatic pathologies in the body;
- cerebral palsy;
- disruption of the endocrine system;
- taking certain medications;
- insufficient blood supply to the brain;
- hormonal changes in the body.
Chorea develops due to damage to the basal ganglia of the brain and the dentate nuclei of the cerebellum. The reason for this is the body's production of additional antibodies. In most patients with sore throat, the production of antibodies is designed to overcome the sore throat. But in some patients, a so-called cross-immune response occurs: antibodies are produced against the ganglia of their own brain. The further mechanism of development of chorea is based on a violation of the transmission of the neurotransmitter dopamine.
Diagnostics
If there are symptoms of chorea, a mandatory diagnosis is carried out. Firstly, this is a blood test, which reveals an increased or decreased level of white blood cells. Secondly, this is an analysis for the presence of streptococcal infection, which will help identify C-reactive protein, cyclic citrullinated peptide, and antistreptolysin-O.
An electroencephalogram is required, which shows changes in brain activity. To accurately understand the cause of involuntary movements of the arms and legs, a study such as electromyography is also carried out. If necessary, these tests can be supplemented with computed tomography, MRI and positron emission tomography (PET study).
Sources
- https://vashaspina.ru/xoreya-prichiny-razvitiya-simptomy/
- https://spina.guru/bolezni/bolezn-gentingtona
- https://www.neboleem.net/horeia.php
- https://onevrologii.ru/nasledstvennye-zabolevaniya/horeya-gentingtona
- https://www.mosmedportal.ru/illness/malaya-khoreya/
- https://NewVrach.ru/xoreya.html
- https://onevrologii.ru/drugie-zabolevaniya/malaya-horeya-u-detej-prichiny-simptomy-formy-diagnostika-i-lechenie
- https://lechenierebenka.ru/horeya-bolezn-u-detej/
- https://fb.ru/article/130841/bolezn-horeya-simptomyi-i-lechenie-neduga
- https://golmozg.ru/zabolevanie/zabolevanie-horeya.html
- https://artrozmed.ru/xoreya/malaya-xoreya-u-detej.html
- https://doctor-neurologist.ru/malaya-xoreya-prichiny-simptomy-lechenie
[collapse]