Parietal lobe damage (PLD). Despite the significant volume of the parietal lobe (PD), its damage (bruises, crushes, intracerebral hematomas) is much less common than that of the frontal or temporal lobes. This is due to topography: the TD usually experiences only impact trauma, and the anti-impact mechanism of its damage is almost completely lost. However, for the same reason, depressed fractures are common here. The abundance of large veins flowing into the projections of the TD into the superior sagittal sinus creates the prerequisites for the frequent formation - when they rupture due to tension during displacement at the time of injury of the cerebral hemispheres along the falx process - of subdural hematomas with a characteristic parieto-parasagittal-convexital localization.
Gliosis of the brain - what is it?
To understand what gliosis changes in the brain are, you need to understand how the central nervous system (CNS) works.
Neurons are the main cells of the nervous system, a kind of “minicomputers” that receive and process information coming from the environment and issue commands to all internal organs. The functioning of the body as a whole depends on the coordinated work of neurons.
For reference. But besides neurons, the central nervous system contains glial cells. These are auxiliary structures of nervous tissue. They perform supporting, trophic (nourish, regulate metabolic processes of neurons) functions, and participate in the development of nerve cells.
Glial cells are located next to neurocytes and can replace them after death: if neurons die, glial cells grow and fill their place.
Like scars on the skin, glial changes in the brain can be figuratively considered scars on the “body” of nervous tissue.
Such cellular replacement, especially if multiple foci are formed, leads to disruption and changes in the central nervous system.
Single pathological foci of glial growths may be an accidental finding during a diagnostic examination.
If a neurological problem occurs, the manifestations of gliosis may include the following:
- Headache. Painful sensations can be of varying degrees of severity and duration: from moderate constant to unbearable, migraine.
- Dizziness.
- Deterioration of memory and attention.
- Mood lability.
- Unsteadiness of gait, unsteadiness when walking.
- Forgetfulness.
- Noise in the head.
- Instability of blood pressure (typical of gliosis of vascular origin).
- Convulsive attacks.
- Insomnia.
- Paretic disorders, paresthesia (feeling of “crawling goosebumps”).
- Deterioration in the functioning of visual analyzers: hearing or vision.
- Increased fatigue, weakness, manifestations of general asthenia of the body.
- Speech disorders, dysarthria.
Clinical manifestations can be varied and depend on the underlying disease that provoked the formation of gliosis.
Symptoms and complaints may be completely absent if the lesions are few in number and discovered by chance after a long-term TBI without consequences.
For reference. The prognosis for life with cerebral gliosis depends on the disease that caused its appearance.
Single lesions formed as a result of long-term consequences of a TBI, or the onset of senile changes according to the patient’s age, do not pose a danger to life and have a favorable prognosis. The same cannot be said about pathological changes in brain tissue in multiple sclerosis or malignant tumors with glial growths.
To assess the severity of the disease and form ideas about the prognosis of its course, the patient should undergo all the necessary examinations to identify the root cause and stage of the disease that caused gliosis.
For reference. Isolated gliosis of the brain cannot be treated, since it is only a symptom. The disease that caused it should be treated. Therefore, the main methods of treatment and drug therapy will depend on the underlying pathology.
If cellular changes in TBI with developed edema are the basis, the main means of eliminating the consequences of injury and the progression of neuronal replacement with glial cells will be the normalization of blood circulation, respiration, the prescription of diuretics, vascular drugs, and symptomatic therapy (prescription of analgesics, sedatives).
The severity of glial changes in multiple sclerosis can be reduced by taking glucocorticosteroids in an individual dose, cytostatics, beta-interferon, Clonazepam, Amantadine.
Timely treatment of neuroinfections, taking antiviral or antibacterial agents, depending on the nature of the pathogen that caused the inflammation, can reduce the risk of post-infectious transformation of nervous tissue.
When brain tumors are detected, neurosurgeons often recommend surgical treatment aimed at removing all or part of the tumor.
Radical removal reduces tissue compression and prevents the destruction of neurons, slows down the formation of glial scars. If there is inoperability or the presence of multiple metastases, they try to stop the process by treating the tissue with radiation therapy or antitumor agents.
Attention. What a patient should not do is, if there are neurological problems and clinical symptoms, self-medicate on the advice of friends or the Internet, or try therapy with folk remedies. In the presence of gliosis, this may not only be ineffective, but also dangerous!
If the patient has any complaints from the nervous system, you should definitely consult a neurologist or neurosurgeon.
To date, there is no effective treatment to restore neurons. All therapy for gliosis is aimed at slowing down the expansion of these lesions. This is done by treating the underlying disease.
In case of TBI, treatment is carried out in an intensive care unit. Therapy is aimed at preserving the functionality of neurons.
Vascular pathologies are treated with medications aimed at restoring normal blood flow.
Infectious lesions require treatment with antiviral or antibacterial drugs.
Even severe gliosis cannot be treated surgically. Any operation is damage, which is the cause of pathology.
Treatment also requires adherence to a special diet. The most important thing that is required of a person is to completely eliminate foods containing fats. It is believed that the progression of pathological glial proliferation accelerates impaired fat metabolism. Therefore, a person has to switch to a low-fat diet and count the number of calories in food.
Gliosis is an extremely serious disease, during the development of which dead nerve cells are replaced by glial cells, which serve to protect the nervous system and help neurons (transmit impulses and form new connections). When excess glia appear in a specific area, we can talk about a diagnosis such as cerebral gliosis.
The disease itself is incurable; it is the result of functional problems in the central nervous system. Foci in the brain are voids that arise with the presence of pathology in certain areas. Neurons become dead and neuroglia appear, giving rise to the described glial transformation.
Micromovements occur every second in the brain at the neuronal level, affecting the functioning of the entire organism. These are processes invisible to humans, so the violations are invisible for some time. In a smoothly functioning nervous system, some components have main tasks, while others have auxiliary tasks.
The central nervous system consists of the following cell type formations:
- Neurons. Function – generation and distribution of signals;
- Ependymal cells – canal of the spinal cord;
- Neuroglia are responsible for metabolic processes.
If the brain is injured, pathologies are present, neural death begins, and illness occurs. The number of neuroglial cells increases, empty areas are filled, acting as an impetus for neural reorganization. Neuroglia are provocateurs of the formation of a focus of gliosis in the brain. Cells are smaller in size than neural cells, but they significantly exceed them in number, occupying about 40% of the total mass.
Age is not a key factor provoking the formation of lesions. Although, of course, older people are at risk. If no structural changes are visible, no damaged area where neuroglia are located, then there is no obvious effect on brain functions.
It would be wrong to say that the formation of glia in empty zones is a destructive process. Although cells do not have the ability to perform neuroregulatory functions, they:
- Support brain activity;
- Protect healthy tissues;
- Form new nerve fibers;
- Receive and distribute signals.
Brain gliosis cannot be predicted, since the root cause is a mutated type of gene that affects the processes of hexoseamidase A.
The vital activity of brain cells will work as required, provided that the required amount of blood flows to them through the vessels. When arteries stop doing their job and feeding neurons, this leads to diseases of vascular origin.
There are no characteristic symptoms for the disease. All types of disorders are symptoms of many other ailments.
The triggering mechanisms may be different, but the manifestations of all have similarities:
- Regular headaches, with ineffective classical therapy;
- Pressure surges without specifics;
- Weakness, high fatigue;
- Poor coordination;
- Low mnestic functions.
The disease can cause seizures. This is due to the presence of a large lesion. In order for an accurate diagnosis to be made, you need to immediately contact a specialist, because similar problems can also indicate other diseases.
Cerebral gliosis, not being a separate disease, does not have any characteristic symptoms. All disorders associated with disturbances in the functioning of the central nervous system are inherent in many other ailments.
Moreover, unless gliosis is associated with a neurological disease such as multiple sclerosis, there are no symptoms at all. Diagnosed randomly, along with the underlying disease.
The causes of the disease may be different, but the manifestation, if any, is approximately the same:
- constant headaches, treatment with standard anti-spasm drugs has no effect;
- changes in blood pressure are not specific;
- constant dizziness, general weakness or excessive fatigue. The causes of the condition may be different, but against the background of memory deterioration they should cause concern;
- deterioration in coordination of movements. The cause of the symptom is associated with the replacement of damaged nerve tissue by glia and, accordingly, poor signal transmission;
- memory deterioration, noticeable decrease in mnestic functions. The reason is the same - lack of functional nerve tissue. Treatment in this case is useless.
Variants of neuroglial growths
Foci of gliosis can be single or multiple, which are diffusely scattered throughout the tissues of the brain, both in gray and white matter. This is determined by the underlying disease, which provoked the replacement of damaged cells with neuroglia. In this case, glial tissue replaces various cerebral damage heterogeneously. Glionic growth can be:
- Isomorphic (when glia grow in an orderly manner);
- Anisomorphic (neuroglia fibers have a chaotic arrangement);
- Fibrous (the processes of gliocytes are more structured than their bodies).
The types of cerebral gliosis also vary depending on the location of the lesions. In this regard, gliose substitutions are distinguished:
In some cases, it is possible to identify a clear localization of foci of neurogliosis with limited processes (for example, in the right superior parietal lobule or the left middle temporal gyrus).
Cerebral gliosis can be with a predominant increase in the number of astrocytes (astrogliosis) or oligodendrocytes (oligodendrogliosis).
Cerebral gliosis is not considered as an independent disease. It is a morphological manifestation of a number of pathological conditions of various origins. Its occurrence is provoked by both congenital and acquired causes:
Systemic primary non-cerebral processes (for example, diabetes mellitus, hypertension, chronic renal failure) can also trigger the development of cerebral gliosis.
In all cases, the formation of gliosis foci can be considered as a consequence of the main mechanisms of neuronal death (hypoxic in nature, as a result of autoimmune damage, programmed cell death).
The main purpose of gliocytes is to provide the neuron with an optimal environment for its functioning. However, shifts in the neuroglial balance can lead to the development of a number of pathological conditions.
Clinical manifestations
Neurogliosis is not a disease, so specific symptoms characteristic of it cannot be identified. The main neurological deficit depends on the cause of glial growths and the localization of pathological foci. In addition, the clinical picture is influenced by the size of neurogliosis.
Signs of neurogliosis are caused by a primary disease that provokes the death of neurons.
Often gliosis occurs latently (the clinical picture is hidden) or asymptomatically (there are no signs) . In this case, its detection is a diagnostic finding during neuroimaging (MRI), and the prognosis for such a condition is favorable.
Most often, small foci of gliosis of unknown origin manifest themselves:
- Headaches;
- Instability of blood pressure;
- General weakness;
- Fatigue;
- Decreased attention and memory;
- Dizziness and unsteadiness of gait.
In severe cases, a massive focus of gliosis can act as an epileptic neural system that can discharge with the manifestation of partial or generalized paroxysms. In this regard, glial areas are often considered as a morphological substrate of locally caused epilepsy. However, studies of the latter explain somewhat differently what gliosis is. It turned out that the more intense the proliferation of gliocytes in the epiactive zone, the milder the disease progresses. Thus, the judgment is confirmed that the zone of proliferation of gliocytes is not a pathological focus, but is an adaptive protective reaction.
Diagnostics
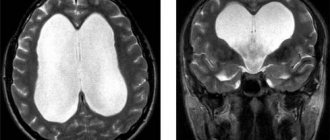
The method for detecting gliosis of the brain is magnetic resonance imaging and pathological examination of the brain. These types of diagnostics make it possible to reliably study foci of gliosis - to obtain a complete picture of their size and location, and also to indicate the supposed causes of the development of the process (for example, gliosis of the right parietal lobe of vascular origin).
MRI most often reveals accumulations of glial cells near the ventricles (periventricular neurogliosis) and above the tentorium of the cerebellum (supratentorial neurogliosis).
Histological analysis of macro- and microspecimens of the brain obtained as a result of a pathoanatomical autopsy will make it possible to identify in detail the variant of the glial reaction and calculate the neuroglial index. However, scientists often note a clear dissociation between these methods. The identified foci of gliosis on MRI do not have a morphological equivalent. Conversely, transformation of the MR signal, indicating the presence of gliosis, is absent in those areas where it is detected histologically.
In a child of the first year of life, diagnosis of areas of neurogliosis is possible using neurosonography.
Hereditary gliosis of the brain (formed as a result of a genetically determined pathology) in the fetus can be assumed starting from the 18-20th week of gestation based on the results of puncture amniocentesis.
Gliotic changes in the brain cannot be reversed, since they represent a compensatory recovery mechanism by which the brain responds to the death of its own neurons. However, this does not mean that it is not necessary to treat a patient with clinical manifestations of glial tissue proliferation. Treatment of gliosis should be aimed at the root cause that led to the occurrence of proliferation of gliosis cells.
It is not gliosis itself that needs to be treated, but the causes of its occurrence.
Prevention of the proliferation of glial tissue comes down to preventing the development of diseases that provoke it, proper lifestyle, and planning pregnancies.
Gliotic changes are a normal reaction of the brain to the influence of damaging factors and are compensatory and protective in nature, aimed at restoring lost functions. However, large-scale proliferation of gliocytes can cause nonspecific neurological symptoms that significantly worsen the quality of life of patients. Such conditions must be treated comprehensively and in a timely manner.
Causes of gliosis
The causes of gliosis, or rather, the initial disease that led to changes in the substance of the brain, are as follows:
- multiple sclerosis;
- tuberculosis;
- encephalitis;
- ischemic diseases of the brain;
- hereditary disorders of fat metabolism;
- infectious diseases characterized by the creation of an inflammatory focus;
- traumatic brain injuries.
It is important to distinguish between treating a disease and preventing it. Of course, it is impossible to restore dead nerve tissue, but it is important to prevent further growth of the formation, and thus treat the disease.
Single foci of gliosis may be a consequence of the natural aging of the body, the physiological death of nerve cells, or their moderate replacement by glial cells. The result of this condition is decreased memory, slowness, decreased ability to concentrate, and insomnia. The changes develop gradually and are not a disease.
Reasons for the formation of foci of gliosis in the white matter of the brain:
- TBI. Concussion, bruise, diffuse axonal damage, intracranial hematoma are conditions that provoke the activation and growth of glial cells due to the massive death of neurocytes as a result of traumatic brain injury.
- Multiple sclerosis. A severe, disabling disease that often occurs at a young age. It is believed that the basis of the disease is an autoimmune disorder, leading to the destruction of myelin and the formation of multiple pathological changes in the central nervous system.
- Neuroinfections. Infectious agents (viruses, bacteria), entering the body, can overcome the blood-brain barrier and penetrate the central nervous system. Released toxins and breakdown products lead to the death of nerve cells. The consequences of meningitis and encephalitis can manifest as glial changes on MRI.
- Hypoxia. Acute or chronic oxygen deficiency, especially in the prenatal period, leads to a slowdown in the maturation and development of brain cells, and excessive proliferation of astrocytes and oligodendrocytes. Cystic-gliotic changes in the brain can be observed even in newborns whose mothers abused alcohol or smoked during pregnancy, causing hypoxia.
- Pathology of blood vessels. Long-term arterial hypertension leads to sclerotic lesions, increased intracranial pressure, and negatively affects metabolic processes: supratentorial multiple foci of gliosis of vascular origin are formed.
- Encephalopathy. A chronic progressive disorder of brain function caused by insufficiency of cerebral circulation can provoke the appearance of proliferation of glial foci that replace neurons.
- Epilepsy. Seizures and other symptoms of epilepsy are caused by degenerative lesions of the central nervous system tissues. Instrumental diagnostics reveals focal changes in the white matter, glial supratentorial areas, changes in signal intensity from the temporal and frontal lobes.
- Tumors. Organic formations in the brain have a destructive effect on neurons, contribute to the occurrence of intracranial hypertension, and provoke increased division of glial cells.
Gliosis is a physiological process during brain aging. When brain neurons die off with age, their place is deservedly taken by neuroglial cells. This is what is associated with the deterioration of fine movements, deterioration of coordination, memory and mnestic functions.
Systemic dilation of normal brain pumps results in cortical vein return and cerebrospinal fluid flow from the ventricular and subarachnoid spaces. As brain atrophy and loss of elasticity in the aged brain reduce their pumping function, the result will be stagnation of fluid near the ventricles and the formation of these images. These fluids have proven myelinotenogenic effects in experimental studies, and the consequences are myelin destruction and the development of spongiosis.
Leukobiosis is also considered an incomplete cerebral infarction based on the vascular risk factors of the elderly, low anatomical vascularization of the centrum ovale, few incidental arterioles, and the histologic changes themselves. It is also noted that in leukoaraesis there is vascular spongiosis in the white matter, characterized by chronic hypoxia and primary myelin degeneration in aging, which is not an exception at this age, as seen in young people with vasculopathies.
The development of gliosis can be triggered by any factors that cause damage and death of neuronal cells. In this way, the body limits the pathological area from healthy tissue, thereby protecting functioning neurons.
The main reason for the formation of gliotic changes is the death of neurons and their processes. In this case, the compensatory mechanism is activated and the voids that appear in the brain tissue are filled with internal neuroglial cells.
Neuronal death can occur as a result of various processes:
- Genetically determined diseases or chromosomal damage are a common cause of gliosis in children;
- A neurological disease such as multiple sclerosis belongs to the group of demyelinating pathologies;
- Alcoholic gliosis can occur in people who drink alcohol and its substitutes for a long time;
- Inflammatory process in the substance of the brain (encephalitis) - most often it is of infectious origin;
- Poor blood supply to the brain is the cause of gliosis of vascular origin;
- The consequence of hypertension is encephalopathy;
- Intrauterine and perinatal hypoxia - oxygen starvation of the fetal brain during pregnancy and childbirth;
- TBI of open and closed type;
- Parasitic brain damage.
There are many reasons for the occurrence of cerebral gliosis. It can appear at any age. Also, gliosis of the brain can form as a result of the physiological death of neurons - during the aging process of the body.
The causes of vascular gliosis in adults, or rather the initial disease, are:
- Multiple sclerosis;
- Tuberculosis;
- Ischemic cerebral disorders;
- Poor fat metabolism of hereditary type;
- Infectious diseases in which inflammation is present;
- Injury, tumor.
Accumulations of the glial type are found in athletes who have suffered head injuries, as well as in those who lead an unhealthy lifestyle and have bad habits that lead to neural destruction.
Is there an age limit for the disease?
It should be noted that single focal changes in the brain substance of a dystrophic nature occur not only in older people, but also in people under fifty years of age.
Stress, injuries, stressful situations, hypertension and other provoking factors can trigger the development of focal changes. The constant overstrain that many able-bodied citizens experience also plays its unseemly role.
As a hereditary condition, leukodystrophies are a group of diseases considered rare, although they usually appear in childhood, they can have an adult onset. These metabolic diseases typically affect white matter in a fairly symmetrical and widespread manner and typically damage the brain stem and cerebellum, with the exception of mitochondrial diseases, which exhibit more asymmetrical damage and typically affect gray matter. The most common in adults are metachromatic leukodystrophy, balloon cell leukodystrophy, adrenomyeloneuropathy, mitochondrial diseases, vanishing white matter, and cerebrogendinous xanthomatosis.
Increased brain function against the background of what is present in youth, as well as ischemia in old age, can equally lead to the emergence of foci of dystrophic changes with all the ensuing consequences. And it follows from this that timely and properly organized rest is a very important part of the prevention of the described pathology.
Types of disease
Foci of neuronal damage lead to deterioration in the functionality of the central nervous system. There is no way to treat them, as already mentioned, since it is impossible to restore dead neural tissue. It is also unacceptable to remove the focus of glia accumulation, since it performs replacement functions.
As a rule, the lesion has a specific area of localization - a focus, although not always.
Based on the location of concentration and form of change, cerebral gliosis can be classified into the following groups:
- Anisomorphic form - the cellular structure of glia predominates over the fibrous one. The growth is chaotic.
- Fibrous form – the fibrous structure predominates, the signs of dominance are clearly expressed.
- Diffuse - there are no lesions, tissue changes are observed not only in the brain, but also in the spinal cord. This picture is typical for diffuse pathological diseases, for example, cerebral ischemia. Treatment, obviously, must begin with eliminating the underlying disease.
- Focal - has a clearly defined area - the focus. Usually, it turns out to be the result of an inflammatory process that leads to the death of neurons. Here treatment is useless.
- Regional - lesions are located mainly on the surface of the brain, under the membrane
- Perivascular – glia surround sclerotic blood vessels. Such changes are often observed in systemic vasculitis. To prevent the development of the disease, it is necessary to treat sclerosis first of all.
- Subependymal - the lesion is localized in the subependymium - the ventricle of the brain.
The size of gliosis is a physical value and can be calculated. It is equal to the increase in neuroglial cells in relation to the number of normal functioning neurons per unit volume. The larger the lesion and the less localized it is, the more difficult the work of the central nervous system is.
Otherwise, the disease manifests itself in young children. The reason for the replacement of nervous tissue with glia is associated with any congenital pathologies. That is, first, as a result of the disease, nerve cells die, and then the affected area is filled with glia.
For example, Tay-Sachs disease, which results in the development of gliosis, appears at 4–5 months of a child’s life. Symptoms indicate disturbances in the functioning of the central nervous system: regression of physical and mental development, loss of hearing and vision, difficulty swallowing, convulsions. The prognosis in this case is extremely pessimistic, and treatment does not produce results.
Based on the signs, features and location, the following types of disease are distinguished:
- If the lesions are fibrous (glial fibers), they speak of the fibrous form of the disease;
- When single (for example, on the left frontal lobe) formations form on the inner zone of the ventricular membrane, they speak of a subependymal type of disease;
- If the lesion is localized in a clear area (under the membrane), the type of disease is called marginal;
- In contrast to the previous type of disease, with a chaotic arrangement of elements, anisomorphic gliosis appears;
- If the distribution is uniform, they speak of an isomorphic form of the disease;
- The perivascular type is not uncommon. In this case, there is a spread around vessels affected by atherosclerosis. This variety has its own special variant - supratentorial. Supratentorial foci of gliosis of vascular origin are structures lying above the process of the tough membrane of the brain.
- The focal type is distinguished by the presence of areas that usually arise in connection with infectious and inflammatory processes;
- When areas are located directly in the brain, they speak of marginal gliosis;
- When the lesion is located near the cerebral stomachs, it is periventricular (paraventricular) gliosis;
- The diffuse form means a pathology when there are many lesions affecting the spinal cord and brain.
- Subcortical changes are oculomotor disorders and subcortical dementia disorders.
The islands that appear at the site of neuronal death may be sporadic and few in number. And they can exist as multiple pathological spread.
Individual lesions are discovered as a result of birth trauma or as a natural process that is typical at a certain stage of life. Such areas may remain isolated and difficult to detect without medical equipment.
Classification
Since gliosis changes in the brain can occur in any part of the brain, different forms of this pathological process are distinguished.
- The predominance of cellular elements in glial proliferation indicates an anisomorphic type.
- If, on the contrary, glia fibers predominate, a fibrous type of gliosis is formed.
- They speak of the marginal type if pathological changes are found only under the membranes of the brain.
- The focal type is observed if the pathological zone occupies a small delimited area of the brain substance and has a capsule;
- The opposite diffuse process covers the entire brain - the white matter is cystic;
- The perivascular type is characterized by pathological changes around the vessels.
- Periventricular type - gliosis is located around the ventricles of the brain.
Gliotic foci
Focal islands vary in size, and their number can also vary. Tissue spread occurs due to the destruction of neuron functions. Gliotic foci are divided into two main types. Let's look at each of them.
Single outbreaks
Single occurrences are common. The picture of single foci of gliosis is such that it is most often found in hypertensive patients with unstable blood pressure. After some time, hypertensive encephalopathy appears. Foci of gliosis in the frontal lobe are quite common.
Gliotic changes in the brain, once they have begun, are an irreversible process. The goal is to prevent further destruction.
Multiple foci of gliosis in the brain are characteristic of a diffuse course of the disease. There are impressive growths. Symptoms in several foci are pronounced, the course of the disease is severe.
It is worth adding that the perifocal type can also develop during the aging process. This situation is natural and medication treatment can help.
Spinal tumors
The same tumors as in other bones occur in the spine; they can be benign or malignant.
At the age of up to 30 years, tumors are more often benign in nature, and at older ages they are malignant. Benign tumors and tumor-like diseases of the spine (Fig. 301). Osteochondroma (Fig. 301, L) is a cartilaginous tumor of a growing organism. Clinically it is asymptomatic. Radiographs reveal a pedunculated mass arising from the cancellous bone (1). Pa MRI (Fig. 301, B) - osteochondroma of the posterior vertebral arch.
Aneurysmal bone cyst (Fig. 301, 4). A formation emanating from the bone marrow (usually venous) spaces, surrounded by newly formed bone tissue and growing outward. The vertebral bodies and their posterior sections, the arches, are affected. Occurs in children and young adults. Clinic: symptoms of compression of surrounding structures, radicular pain. Radiographs show a large focus of destruction with clear contours.
Eosinophilic granuloma (Fig. 301, 5). A type of histiocytosis, abnormal proliferation of histiocytes that replace bone. It occurs at any age, but most often in children 5-10 years old. X-ray examination reveals round-shaped foci of destruction in the vertebral body with clear contours and compression fractures.
Diagnosis and treatment
This condition is most often discovered accidentally - during examination for other neurological diseases.
For this purpose, computed tomography and magnetic resonance imaging are used. In this case, darkening will be observed in areas of the white matter.
Using puncture of the amniotic sac and subsequent examination of the resulting fluid, the presence of congenital gliosis can be assumed.
The method allows you to clearly determine the volume of changes and its localization, and, therefore, clarify or establish the real causes of the lesion, since the localization of lesions, unlike symptoms, is specific.
It is necessary to treat the primary ailment. Treatment of gliosis is only to prevent pathological spread.
- To do this, you need to follow some recommendations.
- Refusal of fatty foods. The pathological distribution of glia is associated with disorders of fat metabolism. Even if there is no such hereditary disease, but a focus of gliosis has already arisen, excessive fat consumption will contribute to the proliferation of non-functional cells. A complete rejection of fats is unacceptable, but their amount should be minimal.
- A healthy lifestyle - following simple nutritional rules and a regimen of physical activity allows you to prevent most central nervous system disorders and changes in metabolic processes.
- Regular examination reduces the risk of diseases that cause gliosis.
Replacing dead nerve cells with glia is a completely natural process, ensuring further brain function in the event of non-fatal damage. However, the very appearance of foci of gliosis indicates other diseases that threaten the state of the central nervous system.
It is impossible to diagnose cellular changes in brain tissue solely based on complaints and symptoms. Instrumental diagnostic methods help in identifying neurological problems, including glial pathologies.
Mandatory research methods are:
- MRI.
- CT.
- X-ray of the skull.
- Fundus examination.
- Electroencephalogram.
For reference. Foci of gliosis are best visualized on MRI or CT machines.
These modern devices make it possible to accurately identify vascular changes, tumor processes, pathological areas in the white matter of the frontal lobes, areas of hemorrhage, and ischemic lesions.
Other diagnostic methods are complementary and necessary to determine the cause of gliosis. After all, this condition is not an independent disease, but only a symptom of it.
If gliosis is detected after a CT or MRI, and there are complaints from the nervous system, the patient should visit a neurologist or neurosurgeon to continue an in-depth examination and subsequent treatment.
Lesions in the lungs on CT - what focal formations can mean - Your online doctor
Focal formations in the lungs are tissue compactions, which can be caused by various ailments. Moreover, to establish an accurate diagnosis, a doctor’s examination and radiography are not enough. The final conclusion can be made only on the basis of specific examination methods, including blood tests, sputum tests, and tissue puncture.
Important: the opinion that only tuberculosis can be the cause of multiple focal lung lesions is erroneous.
We can talk about:
- malignant neoplasms;
- pneumonia;
- disorders of fluid exchange in the respiratory system.
Therefore, diagnosis must be preceded by a thorough examination of the patient. Even if the doctor is sure that a person has focal pneumonia, it is necessary to perform a sputum analysis. This will identify the pathogen that caused the development of the disease.
Now some patients refuse to undergo certain specific tests. The reason for this may be reluctance or inability to visit the clinic due to its distance from the place of residence, or lack of funds. If this is not done, then there is a high probability that focal pneumonia will become chronic.
How to prevent brain gliosis
There is no specific prevention that can protect neurons from destruction and brain tissue from glial growths.
But doctors can give advice that will help support the blood vessels of the brain and preserve the activity of neurons for as long as possible.
Patients must adhere to the following rules:
- Lead a healthy lifestyle.
- Stay physically active. Avoid gaining excess weight.
- “Train” the brain: learn languages, poetry, solve crosswords.
- Monitor cholesterol and glucose levels.
- Monitor blood pressure, and if you have hypertension, take antihypertensive medications regularly.
For reference. It is important to eliminate risk factors that may cause neurological problems. Limit your intake of “junk” food, do not drink alcohol and do not smoke. Monitor the course of chronic diseases (hypertension, arrhythmia, diabetes mellitus).
What to do and how to treat
There are no specific medical recommendations for eliminating the tumors in question. The treatment for brain gliosis prescribed by a specialist will be aimed at combating the disease that became the “trigger” mechanism for the appearance of gliosis. Medicines must be prescribed strictly by a doctor. Drug therapy will consist of taking medications that can maintain the condition of the blood vessels.
Diagnostics
To diagnose the disease, CT, MRI and EEG are performed. Let's consider in what cases one or another method is used.
Magnetic resonance imaging is the most preferred method. With its help, the doctor will see foci of gliosis in the frontal lobe and understand how advanced the situation is.
Computed tomography is also sometimes used by specialists to diagnose white matter gliosis in the brain. However, this method will not provide such a necessary clinical picture as MRI. A significant disadvantage for the patient will also be the presence of radiation during the procedure.
Electroencephalography - finding out how active the brain is. Electrodes and computer processing are used. This method is often used to clarify problems when epilepsy or seizures are present.
Often, in order to get a detailed picture, it makes sense to conduct additional examinations, namely, take tests or perform other manipulations.
Among drug therapy, commonly prescribed drugs are:
- Aimed at improving brain function;
- Improving cerebral circulation;
- Vitamins.
Surgeries are also considered if treatment with medications does not bring the desired result and any other treatment has been tried without a positive effect, but the focus of gliosis remains and the disease progresses.
Traditional treatment
In addition to the usual, traditional methods of treatment, there are also so-called traditional methods of combating gliosis, or rather the source disease.
Dandelion root. Helps strengthen blood vessels and lowers cholesterol. Used as a decoction.
Melissa. Positive effect on the cerebral cortex, strengthens vascular walls, acts as a sedative, restoring nerve cells.
Dill seeds. They can restore blood circulation and help normalize blood pressure.
St. John's wort. Positive effect on vascular lesions, tissue restoration.
Dioscorea. Indicated for vascular and cardiac problems, relieves headaches. The root is crushed and brewed, after which it is taken several times a day, a tablespoon after meals.
Prevention
To exclude gliosis of a vascular nature, as well as slow down the process of cell death, you should:
- Provide physical activity. It is worth trying to perform a simple set of exercises on a daily basis, it will increase your strength and endurance.
- Rest, adjust your routine. Only then will the nervous system work as it should.
- Take care of proper nutrition.
Hemangioma
An asymptomatic tumor of a vascular nature, occurs at any age. An X-ray examination (Fig. 302) reveals the vertical striation of the vertebral bodies. Often the vertebra is swollen, a defect with finely festooned contours and a fine-mesh pattern (thickened trabscules) is determined, sometimes a vessel approaches the defect.
The transition of the process to the arches and the intact state of the disc are characteristic. Involvement of the arch is a poor prognostic sign, just as the symptom of swelling and the soft tissue component are signs of active tumor growth.
Is gliosis dangerous?
Disturbances in the brain lead to failure of the entire body system. With a large number of lesions, the functions of all departments suffer, the person becomes helpless.
What are the consequences of the disease?
- Pressure changes;
- Encephalitis;
- Multiple sclerosis;
- Impaired blood circulation;
- Irreversible damage to the nervous system.
If the first symptoms are present, you should not hesitate and consult a neurologist. For newborns, diagnosis is often a death sentence. Children rarely survive even to kindergarten age, despite the fact that at the initial stage the disease does not make itself felt.
Cardiovascular diseases can not only cause gliosis, but also become the result of the disease itself for other primary reasons. The chances of overcoming the disease at any age are almost the same for everyone.
Speaking about the life prognosis, it is worth understanding that only a doctor can assess the degree of danger that glial changes pose.
A timely visit to a specialist will greatly improve the condition and stop the appearance of additional lesions in the brain.
The disease has different life prognoses, which are influenced by the catalyst that led to tissue changes. The prognosis also depends on the intensity of the changes and how many foci there are already. As with many diseases, a favorable outcome can be expected if early diagnosis is made and adequate therapy is started on time. With this option, people with gliosis live for quite a long time.
By adhering to the doctor's instructions, the course of the disease can be slowed down. Of course, only a specialist can predict how dangerous neoplasms are, so it is important to seek help as early as possible.
How to make a diagnosis?
It is impossible to make a diagnosis based on clinical symptoms. As a rule, gliosis is diagnosed quite accidentally during an examination for another reason. A method that allows you to visualize gliosis foci is magnetic resonance imaging. With its help, you can accurately calculate the amount of gliosis.
Magnetic resonance imaging is a diagnostic imaging modality of great value, superior to computed axial tomography, and is considered more sensitive in detecting early cerebral infarcts, brainstem and posterior fossa lesions, and in diagnosing lacunar infarcts; it is not only able to identify smaller lesions, but also provides information about its chronology.
It is an important imaging medium because it allows early diagnosis and monitoring of cerebrovascular diseases, allows timely treatment in the ischemic penumbral phase, reduces the infarct area, and guarantees a better quality of life for patients.
In addition to identifying the pathological process itself, it is necessary to find out its cause. For this purpose, all possible additional techniques are used, which include a detailed neurological examination.
Primary malignant tumors
An early clinical sign of a malignant tumor of the spine is pain that worsens at rest, at night, and does not subside with massage and thermal procedures.
X-ray examination in standard projections can detect a tumor, but not at an early stage. The method of choice is CT, MRI, radioactive scanning. In case of mislom, X-ray examination provides comprehensive information.
X-ray signs of a malignant tumor.
1. Destruction in the spongy substance of the vertebra is often not visible until compression occurs. With a negative X-ray picture, up to 1/3 of the vertebral body may be destroyed. Diagnosis of early destruction is possible with CT and MRI (Fig. 303).
2. Osteosclerosis - often detected with osteoblastic metastases. Differential diagnosis with compact islands. Diagnosed by X-ray and radioisotope examination.
4. Enlargement of soft tissues - observed more often with a primary tumor, less often with metastatic ones. The soft tissues are usually more enlarged than seen on x-ray, especially in the lumbar region where the shadow of the muscles overlaps. The diagnosis is established radiologically and using CT, MRI.
5. Calcification and ossification of soft tissues. The x-ray shows flaky, chaotic, rounded shadows at the level of the affected vertebra - a sign of exophytic tumor growth.
Consequences and complications
Ischemic cerebrovascular disease. Cerebrovascular diseases. Development of magnetic resonance. Magnetic resonance imaging. Factors determining prognosis in ischemic stroke. New risk factors for ischemic stroke. Morphology and immunocytology of atherosclerotic plaque of the internal carotid artery in the pathogenesis of ischemic stroke.
Cerebrovascular diseases: In: Issues of internal medicine. Concept and classification of cerebrovascular diseases. Guide to vascular diseases of the brain. 2nd ed. Acute ischemia of cerebrovascular disease. Neuroradiological assessment of cerebrovascular diseases.
- intellectual disabilities;
- mnestic disorders;
- blood pressure surges;
- constant headaches and dizziness;
- asthenic manifestations;
- coordination problems;
- speech pathology;
- paralysis and paresis;
- hearing and vision impairment;
- mental change;
- development of dementia.
Metastases in the spine symptoms
The first and most important symptom of the development of metastases in the spine is a feeling of dull local pain in the projection of the affected vertebral segment; it is often confused with osteochondrosis.
A characteristic difference between pain is that it appears at night, and it also tends to irradiate and increase along the radicular plexuses. An alarming symptom is also the presence of a primary tumor at the time of spinal pain. Increasing pain is an extremely unpleasant trend, since it reflects the increasing degree of destruction of the vertebra.