Causes of paresthesia
We found out what paresthesia of the body is. Why does it occur? The mechanism is simple: a failure in the transmission of nerve impulses occurs in the nerve root and irritation occurs. Most often this is observed when there is pressure on the nerve ending. Compressive factors can be:
- benign and malignant tumors;
- osteocondritis of the spine;
- a tourniquet that is placed around a limb to stop bleeding.
Also, paresthesia often occurs with the following diseases and conditions:
- nerve ending injuries;
- exposure to high temperatures (for this reason, paresthesia of the lips and tongue may occur);
- inflammatory processes on the part of the vessels that supply blood to the nerve roots;
- endocrinological disorders (diabetes mellitus);
- poisoning by biological toxins or industrial poisons;
- lack of B vitamins.
The causes of paresthesia of the fingers are generally the same as the causes of a similar disorder in the feet, head or torso. The larger the nerve root that is affected, the larger the area of paresthesia.
Legs
Paresthesia of the legs, and, in medical terms, of the lower extremities, is quite common. In this case, unpleasant sensations can occur in the foot, calf and even thigh. It is worth saying that such paresthesia appears mainly in the morning or evening hours. And all because blood flow deteriorates greatly when a person is in a lying position. As a result, cramps and a feeling of numbness may appear. If this happens infrequently, there is no need to worry. Similar symptoms may occur, for example, due to an uncomfortable sleeping position. However, there are the following reasons why leg paresthesia may occur:
- Migraine attacks.
- Vitamin deficiency, especially B vitamins.
- The causes can also be various diseases: osteochondrosis, brain tumors, intervertebral hernias, diabetes mellitus, Raynaud's disease, etc.
Symptoms of paresthesia of the face and other locations
The classic triad of all paresthesias:
- numbness of varying degrees of severity;
- tingling;
- a feeling of “crawling goosebumps” on the surface of the skin.
Sometimes in the area of the skin that is innervated by the irritated nerve ending, itching of varying intensity and pain may occur.
Most often, paresthesia occurs in the following localization:
- feet (especially on the back surface);
- brushes;
- neck (especially its lateral surface);
- head. It should be borne in mind that symptoms of facial paresthesia are often combined with signs of paresthesia of the scalp. On the other hand, discomfort due to nerve irritation can affect individual locations - the mucous membrane of the mouth and tongue or the mucous membrane of the nose and pharynx, although neighboring organs and tissues will not undergo any sensory changes.
If paresthesia is observed regularly over a period of time, trophic disorders may occur in the area of sensitivity failure (due to impaired tissue nutrition). They signal increasing irritation of the nerve, and can also act as a “red flag” warning of the onset of serious organic disorders on the part of the affected nerve.
Prevention and prognosis
To reduce the likelihood of developing skin paresthesia, it is necessary to adhere to the following general preventive measures:
- complete renunciation of addictions;
- maintaining a moderately active lifestyle;
- constant monitoring of blood glucose levels, as well as blood pressure indicators;
- proper and balanced nutrition;
- use of personal protective equipment when working with chemicals and toxic substances;
- regular complete medical examination - for early detection and elimination of ailments that can lead to paresthesia.
Due to the specific clinical picture, such a pathology has a favorable prognosis - complete recovery and rapid recovery after surgery are observed.
Source: SimptoMer.ru
General description of the disease
This is a term used to describe a burning or tingling sensation that usually occurs in the extremities. However, it can also occur in other parts of the body.
Often this feeling occurs suddenly, and this form is one of the most painless types of paresthesia. Surely, many have experienced it when, for example, they sat on their legs for a long time or crossed them, and then got up. Or if your hand was squeezed.
In such cases, muscles and nerves are compressed, and blood flow is hampered. That is why this tingling feeling comes. When the pressure eases, the unpleasant sensation goes away.
However, chronic paresthesia does not go away as quickly as temporary paresthesia and often causes more severe discomfort[1].
Anyone can experience temporary paresthesia, but the risk of developing this disease increases with age. Also at risk are people whose activities involve repeated compression and release of nerves: office workers who type a lot, musicians, athletes, in particular tennis players. The chances of suffering from paresthesia increase in people with type 1 and 2 diabetes, autoimmune diseases, and neurological disorders [4]..
Causes that provoke the occurrence of paresthesia
The main cause of paresthesia is pressure on the nerve. When it weakens, the unpleasant feeling goes away. But in some cases this does not help, the tingling feeling is constantly present. This is chronic paresthesia and may be a sign of nerve damage or disease. Chronic paresthesia is caused by the following factors:
- 1 Trauma or accident causing nerve damage.
- 2 Stroke or mini-stroke - when blood flow to the brain is restricted and causes damage.
- 3 Multiple sclerosis is a disease of the central nervous system.
- 4 Diabetes is a blood sugar disorder that can damage nerves over time.
- 5 A pinched nerve (often in the neck, shoulder or arm) from injury or overuse.
- 6 Sciatica – pressure on the sciatic nerve (which runs from the lower pelvis to the buttocks and legs), is a common problem during pregnancy and usually causes numbness and pain in the back or legs.
- 7 Lack of certain vitamins, especially low levels of vitamin B12, which is essential for maintaining nerves in good condition.
- 8 Alcohol abuse.
- 9 Taking medications – for example, some types of chemotherapy that cause nerve irritation or damage, some antibiotics, birth control pills[3].
Among other common causes of paresthesia, doctors name the following:
- migraine;
- neuropathy;
- malnutrition;
- menopause;
- dehydration;
- fibromyalgia;
- herpes zoster;
- hypoglycemia;
- Fabry disease;
- nervous irritation;
- atherosclerosis;
- immune deficiency;
- metabolic disease;
- lidocaine poisoning;
- taking anticonvulsants;
- lupus erythematosus;
- neurological disorders;
- motor neuron diseases;
- Lyme disease;
- autoimmune disorders;
- heavy metal poisoning;
- Guillain-Barré syndrome[2].
Symptoms of paresthesia
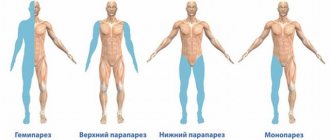
Paresthesia can affect any part of the body, but it usually appears in the arms, hands, legs, and feet.
The most common symptoms are numbness of a limb or other affected area, a feeling of weakness in it, tingling, burning, or vice versa - a feeling of coldness, muscle atrophy, restless legs syndrome, a crawling sensation on the skin.
Chronic paresthesia may cause stabbing pain. This may cause the affected limb to become clumsy. When paresthesia occurs in the legs and feet, it makes walking significantly more difficult.
If you experience symptoms of paresthesia that do not go away within a short time and impair the quality of life, you should definitely consult a doctor. This may be a sign that the person has an underlying medical condition that requires treatment[4].
Types of paresthesia
There are two types of paresthesia. Transient and chronic . The first occurs briefly as a consequence of migraines, injuries, taking certain medications, as well as mechanical compression of nerves and muscles, which occurs when sitting on your feet or squeezing your hand.
Chronic paresthesia can result from disorders that affect the central nervous system. For example, such as transient ischemic attacks or strokes, multiple sclerosis or encephalitis.
Vascular lesions or tumor-like growths can put pressure on a person's spinal cord or brain and cause the development of paresthesia. However, the occurrence of the disease for these reasons is a fairly rare case.
More often, paresthesia develops after nerve damage from infections, injuries, inflammation or other conditions [1].
Complications of paresthesia
Paresthesia in most cases is a symptom that can cause complications of the primary or underlying disease that provoked its appearance.
For example, people with paresthesia may have difficulty walking or difficulty grasping objects with their hands, depending on which limb is affected.
People with decreased sensation may be unable to detect an injury (eg, burn, puncture wound), which can lead to infection of the extremities.
Loss of sensation in the legs can lead to an increased risk of falling[5].
Prevention of paresthesia
Paresthesia cannot always be prevented. After all, even temporary paresthesia can happen because you compress a nerve in your arm in your sleep. We have no control over this. But in order to avoid the unpleasant sensations of passing paresthesia, you can, for example, give up the habit of sitting on your feet. This way you won't feel any tingling sensations in them.
To prevent chronic paresthesia, follow the simple tips below.
- Avoid repetitive movements if possible.
- Rest often if you need to perform repetitive movements.
- Get up and stretch as often as possible.
- If you suffer from diabetes or any other chronic disease, get timely and regular checkups. Diagnosis and treatment of diseases will help reduce the risk of paresthesia[4].
Diagnosis of paresthesia
In most cases, paresthesia of the lips and tongue, hands, feet and other parts of the body is easy to diagnose. The doctor asks the patient about the following nuances:
- the nature of unusual sensations;
- their frequency;
- what the patient associates with numbness, tingling and other atypical sensations;
- whether similar sensations have appeared before;
- whether the patient works with harmful substances (salts of heavy metals, nitrates and organic solvents are especially important);
- whether there is any consumption of alcoholic beverages.
You should also find out if there are any medical procedures in your medical history (this is how paresthesia may occur after the removal of a wisdom tooth).
In addition, the doctor should check skin sensitivity not only in those areas of the body that are subject to paresthesia, but also in neighboring ones. An examination of the skin will be informative, during which the following will be noted:
- pale skin;
- hair loss;
- a decrease in local temperature, which can be diagnosed even by touch.
In a number of cases, it was thanks to paresthesia that complex diseases were diagnosed. Therefore, you should carefully determine the causes of paresthesia of the fingers, toes and torso, since behind harmless sensations that may not cause any particular inconvenience to the patient, the same diabetes mellitus can be hidden. For any, even minor, sensitivity disorders, a comprehensive examination is necessary.
Treatment
Paresthesia of the face, limbs, lower jaw or any other localization is often eliminated using conservative techniques, which is based on the following:
- detoxification medications;
- hypoglycemic substances;
- vitamin complexes;
- antiplatelet agents, vasoactive drugs and other tablets aimed at improving blood rheology.
In addition, drug therapy also involves the use of warming ointments applied to the area of the injured nerve.
Treatment of paresthesia of the lower extremities or other types of illness using physiotherapeutic procedures includes:
- vacuum and underwater massage;
- darsonvalization;
- medicinal electrophoresis;
- galvanic mud applications;
- acupuncture.
Conservative therapy can also be aimed at:
- the patient undergoing a course of therapeutic massage;
- the use of folk remedies at home is indicated only after consulting with your doctor. The most effective are decoctions based on sweet clover and birch leaves, horse chestnut and willow bark.
If the above methods of treatment are ineffective, it is recommended to implement low-traumatic neurosurgical techniques. In addition, surgery is necessary in cases where the cause of paresthesia is tumors or hematomas.
How can you help a patient?
Treatment of paresthesia can be successful. The treatment strategy depends on where exactly the disease developed.
Physiotherapy
Physiotherapy is used when sensitivity is lost in any area of the lower extremities. Treatment of paresthesia is:
- Massage procedures (performed manually).
- Using the Darsonval apparatus.
- The use of electrophoresis (the participation of nicotinic acid is assumed).
- Applications (galvanic mud).
- Physical therapy exercises.
- Acupuncture.
Physiotherapy + tablet therapy
The effect of treating paresthesia will be much better if you follow a combined approach. In most cases, the doctor prescribes an appointment for the patient:
- Piracetam.
- Cavinton.
- Trentala.
- Nootropil.
These drugs help reduce blood viscosity and improve cerebral and peripheral circulation.
Methods of neurosurgery
In some cases, the doctor makes the decision regarding surgery. Neurosurgical methods are performed with little tissue trauma. Against this background, an excellent result is ensured in eliminating the hernial tumor.
Alarming symptoms may disappear immediately after the patient has been operated on and completed a rehabilitation course.
Grandma's advice
Treatment of paresthesia using traditional methods allows you to quickly achieve a complete recovery. In most cases, the doctor prescribes internal use of herbs and infusions to the patient. Infusions can achieve a good effect:
- birch leaves;
- willow bark;
- horse chestnut;
- sweet clover
Thanks to these plants, blood vessels dilate and blood circulation becomes much better. A person can recover only if he is consistent and does not exceed the dosage.
Preventive measures are of great importance. Many patients are prescribed medications to improve blood circulation for the rest of their lives.
Rate this article:
(votes: 1 , average: 5.00 out of 5)
Loading...
Related posts: