| This article should be Wikified. Please format it according to the article formatting rules. |
| This article lacks links to sources of information. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on July 18, 2011 . |
This term has other meanings, see PVL (meanings).
| Periventricular leukomalacia | |
| ICD-10 | 91.291.2 |
| ICD-10-CM | P91.2 |
| ICD-9 | 779.7779.7 |
| ICD-9-CM | 779.7[1][2] and 742.8[2] |
| ICD-O | growth- @ m_s raіtpuTmovtabatf |
| OMIM | MTHU037926 |
| DiseasesDB | 9868 |
| MedlinePlus | 007232 |
| eMedicine | ped/1773 |
| MeSH | D007969 |
Periventricular leukomalacia (PVL)
- a form of damage to the white matter of the cerebral hemispheres in children, discovered by morphologists, one of the causes of cerebral palsy. PVL is characterized by the appearance of foci of necrosis, predominantly coagulative, in the periventricular zones of the white matter of the cerebral hemispheres in newborns (rarely in stillborns).[3] It belongs to one of the forms of the so-called “hypoxic-ischemic encephalopathy”.
Description history[ | ]
The first microscopic description of a PVL focus belongs to JM Parrot (1873) [4]. R. Virchow [5] only macroscopically described yellowish foci in the periventricular zones of the lateral ventricles of the brain in deceased newborns born to mothers with syphilis and smallpox, classifying them as congenital encephalitis. There are no sufficient grounds to classify these lesions as PVL. The lesion has been described under various names (“encephalodystrophy”, “ischemic necrosis”, “periventricular infarction”, “coagulative necrosis”, “leukomalacia”, “cerebral softening”, “periventricular white matter infarction”, “white matter necrosis”, “diffuse symmetrical periventricular leukoencephalopathy"), more often by German scientists, but the term “periventricular leukomalacia”, introduced in 1962 by BA Banker and JC Larroche, became widespread worldwide [6]. The term is not clear enough, since with PVL it is not softening that occurs, but foci of coagulation necrosis that are denser than the surrounding areas of the brain. The first article in the USSR and Russia dedicated to PVL was written by V.V. Vlasyuk et al. (1981), who proposed using the term “periventricular leukomalacia.”
The most complete studies of PVL in the world on the largest sectional material were carried out by V.V. Vlasyuk (1981) (frequency, etiopathogenesis, topography, degree of damage to various parts of the brain, stages of development of lesions, neurohistology, role of microglia, electron microscopy, etc.), who for the first time revealed a high incidence of damage to optic radiation and proved that PVL is a persistent process, that old foci of necrosis can be joined by new ones, that PVL foci can be at different stages of development.[7][8]
Brief anatomical information
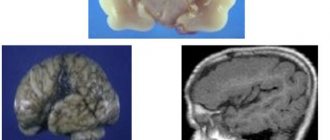
Foci of the disease are about 2-3 millimeters in diameter and can be found in the parietal and frontal lobes. Moreover, their formation is absolutely asymmetrical.
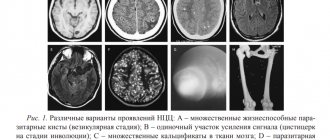
The main outcome of the disease is the formation of a huge number of cysts, all of them of different sizes. It takes about two weeks for necrosis and the formation of cystic compounds to appear, and then the cavities in the baby’s brain collapse—that is, atrophy of the nerve tissue of the brain.
Article on the topic: What are the benefits and harms of walnuts for the body of men and women?
Morphology[ | ]
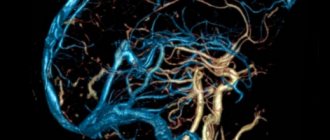
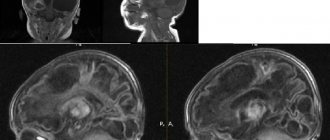
According to the morphological essence of PVL
- These are small-focal, mainly coagulative periventricular infarctions of the white matter of the brain, often bilateral and relatively symmetrical. In PVL, foci of necrosis are located in the periventricular zone, but in the presence of many foci (severe lesions), some of them can spread to the central parts of the white matter of the brain. With the highest frequency, PVL foci occur in the periventricular white matter of the initial sections of the posterior horns of the lateral ventricles of the brain (the optic radiation is affected) and the central sections of the ventricles at the level of the visual thalamus (the corticospinal tract is affected). During the process of morphogenesis, lesions go through three stages: 1) development of necrosis, 2) resorption and 3) formation of a glial scar or cyst. Cysts occur with large and merging foci of PVL, with mixed necrosis (colliquation in the center and a coagulation rim along the periphery). Around the lesions, an area of other lesions of the white matter of the brain is usually determined - death of pro-oligodendrocytes, proliferation of microgliocytes and mast astrocytes, edema, hemorrhages, death of capillaries, etc. (the so-called “diffuse component” of PVL). However, diffuse lesions without necrosis are not PVL. If 15 frontal sections of the brain are made, then the detection of PVL foci in 1-4 sections indicates a mild degree of PVL, in 5-8 sections - a moderate degree of PVL, and in 9-13 sections - a severe degree of PVL (2).
Frequency[ | ]
The frequency of PVL, according to different authors, ranges from 4.8% to 88%, but often among a certain group of children or according to neurosonographic studies, which is not entirely objective. On non-selected sectional material, the frequency of PVL is 12.6%, more often in boys, and depending on birth weight: 1001-1500 g - 13.3%, 1501-2000 g - 21.5%, 2001-2500 g - 31.6%, 2501-3000 g - 14.8%, more than 3000 g - 3.5%. It occurs most often in premature infants of the 1st and 2nd degrees. In those who died on the first day after birth, PVL occurs with a frequency of 1.8%, and in those who died on the 6th-8th days - 59.2%. In the group of those born with cephalic presentation, the incidence of PVL is 19.6%, with breech presentation - 17.4%, and with caesarean section - 35.6%.[9]
How to help your baby?
Cerebral leukomalacia is accompanied by changes in nervous tissue and these changes are irreversible, and, unfortunately, there is simply no clear treatment regimen for the disease at the moment. Typically, doctors look at the symptoms and then prescribe treatment depending on the manifestations of the disorder.
To treat the disease, nootropic medications are used, which improve blood flow in the brain and also improve metabolism. The drugs that are most often prescribed are Piracetam, Stugeron.
All other therapy prescribed by the doctor is used to correct motor movements, as well as disorders of psychomotor development.
In order to avoid the onset of the disease, obstetricians try to maintain pregnancy as long as possible. But if the baby was born prematurely, then they need to do everything possible for his safety. Immediately after childbirth, breathing improves, and it must be controlled. It is important that there is the correct ratio of oxygen and carbon dioxide in the blood, and that blood pressure must be normal.
If the baby has grown...
After the baby reaches the age of one year, treatment becomes more symptomatic. The child’s condition during this period requires constant monitoring and if symptoms of leukomalacia are detected, he is prescribed drugs such as: Pantogam, Phenibut. Thanks to their use, an inhibitory effect occurs in the formation of necrosis zones in the cerebral cortex.
If a child has a sleep disorder, he is prescribed sedatives - Valerian and Melissa. Water procedures also have a good effect.
Article on the topic: Chest preparation for bronchitis in children - instructions for use, indications, composition and price
If the baby experiences an increase in blood pressure, then the drugs Diacarb, Furosemide or Glycerin are prescribed. But the last two drugs are not used independently; it is imperative that potassium enters the body.
All convulsive manifestations are removed with the help of the drug Phenobarbital. If its use causes tachycardia and blood pressure, then it can be replaced with beta-blockers - Anaprilin and Obzidan.
Since the disease entails a disruption in the functioning of the musculoskeletal system, massage and exercises are prescribed, as well as physiotherapeutic treatment.
If there is a delay in the development of the speech apparatus, then teachers and speech pathologists come to the rescue and help correct speech.
In particularly difficult cases, respiratory distress syndrome develops. In order to avoid it, surfactant preparations are used. Thanks to its use, the severity of respiratory distress is reduced and the need for a ventilator disappears.
...But here are some rehabilitation methods that can help:
Etiology and pathogenesis[ | ]
Etiologically, PVL is a hypoxic-ischemic lesion of the white matter of the brain associated with arterial hypotension, apnea attacks after birth, resuscitation measures, infections, etc. PVL is promoted by prematurity, and of a small degree (1-2nd). Pathogenetic factors: hypoxia, acidosis, hypocapnia, toxins, etc. Foci of necrosis (infarction) occur in the border zone between the ventriculofugal and ventriculopetal arterial branches[10], localized in the periventricular white matter of the brain.
This nosology is characterized by 2 main signs
:
1. localization in the periventricular zones of the white matter of the cerebral hemispheres 2. lesions have the character of predominantly coagulative necrosis.
Around the PVL foci, other lesions, the so-called “diffuse component,” can be detected.
Time of occurrence of PVL
- mainly in the first days after birth, sometimes ante- and intrapartum.
What diseases have symptoms similar to brain leukomalacia in a baby?
Multicystic encephalomalacia
- occurs in full-term children with severe asphyxia during childbirth;
- diffuse generalized brain damage;
— multiple cystic cavities of various sizes;
- cysts may have septa;
- usually occur in the cortex and nearby white matter;
- often in the frontal and occipital lobes.-
Vasculitis
- very rare;
— multiple lesions of the cortex and subcortical region;
- may be combined with hemorrhages;
— perfusion defects in the acute stage;
— sometimes areas of damage to the blood-brain barrier are identified.
Differences from other lesions[ | ]
In very premature infants, other lesions of the white matter of the brain other than PVL are more likely to occur - diffuse leukomalacia and multicystic encephalomalacia. Due to insufficient knowledge of the latter lesions, they are often mistakenly classified as PVL.
PVL must be differentiated
with the following main lesions of the white matter of the cerebral hemispheres:
- edematous hemorrhagic leukoencephalopathy (OHL)
- telencephalic gliosis (TG)
- diffuse leukomalacia (DFL)
- subcortical leukomalacia (SL)
- periventricular hemorrhagic infarction (PVI)
- intracerebral hemorrhage (ICH)
- multicystic encephalomalacia[11]
- subependymal pseudocyst.
In LS, foci of necrosis are located in the subcortical region and in some severe cases can spread to the central parts of the cerebral hemispheres. In DFL, foci of necrosis are located diffusely in all parts of the white matter of the brain, involving the periventricular, subcortical and central regions of the cerebral hemispheres; colliquation necrosis leads to cyst formation and occurs most often in very premature infants. With TG there is no complete necrosis of the brain and cysts do not form. PGI occurs due to thrombosis in the system of internal cerebral veins or is a complication of intraventricular hemorrhage. Pseudocysts have nothing to do with brain necrosis and are most likely developmental defects. The pathogenesis of all these lesions is different.
Currently, there is an overdiagnosis of PVL due to the overestimation of neuroimaging studies and underestimation of other lesions of the white matter of the brain.
Preventive measures
To reduce the risk of developing leukomalacia you need to:
- extend the pregnancy period, since the shorter the period, the greater the likelihood of developing this disease;
- If possible, it is necessary to prevent premature birth in a woman in labor.
But not only the doctor can influence the development of pregnancy, but the pregnant woman herself can change the situation in a positive direction. What do we have to do:
- first of all, a pregnant woman is a future mother and she should lead a healthy lifestyle;
- Pregnancy cannot occur spontaneously; it must be carefully planned;
- nutrition should be harmonious and balanced;
- every pregnant woman must register and strictly follow doctors’ recommendations;
During pregnancy, you should try not to get sick from various diseases, especially viral and infectious ones. Due to the illness, the unborn baby may suffer.
Notes[ | ]
- Disease Ontology release 2019-05-13 — 2019-05-13 — 2020.
- ↑ 12
Monarch Disease Ontology release 2018-06-29sonu - 2018-06-29 - 2018. - 1. Vlasyuk V.V. Periventricular leukomalacia in children. - St. Petersburg: Glikon Plus, 2009. - 218 p. ISBN 978-5-93682-540-8.
- Parrot JM Etude sur le ramollissement de l'encephale chez le nouveaune. —Arch. Physiol. Norm. Path., 1873, v. 5, p. 59-79.
- Virchow R. Zur pathologischen Anatomie des Gehirns: I. Congenitale Encephalitis und Myelitis. - Virchows Arch., 1867, Bd 38, S. 129-138.
- Banker BA, Larroche JC Periventricular leukomalacia of infancy. A form of neonatal anoxic encephalopathy. —Arch. Neurol., 1962, v. 7, p. 386-410.
- Vlasyuk V.V., Tumanov V.P. Pathomorphology of periventricular leukomalacia. Novosibirsk, “Science”, 1985.- 96 p.
- Vlasyuk V.V., Mayer I.O., Okhtyrskaya L.A., Babutsidze T.Ya. Periventricular leukomalacia in newborns and its thanatogenetic significance. Pediatrics, 1981, No. 11, p. 32-36.
- V. V. Vlasyuk Birth trauma and perinatal cerebrovascular accidents. St. Petersburg, “Nestor History”, 2009. - 252 pp. ISBN 978-5-98187-373-7.
- De Reuck J., Chattha AS, Richardson EP Pathogenesis and evolution of periventricular leukomalacia in infancy. —Arch. Neurol., 1972, v. 27, p. 229-236.
- V. V. Vlasyuk, Yu. P. Vasilyeva, A. A. Vilnits, V. E. Karev. Multicystic encephalomalacia in children, the role of infections. Journal of Infectology, 2010, No. 2, p. 45-53. ISSN 2072-6732.
What are the signs of periventricular leukomalacia?
Periventricular leukomalacia can be difficult to detect in newborns, as very young children generally do not show signs of impairment. Periventricular leukomalacia can resemble other conditions, and each case is different. Intellectual impairment, developmental disorders, visual, hearing, and coordination impairments are common with periventricular leukomalacia.
Spastic diplegia (tight muscles and limbs that do not bend easily) is the most common type of cerebral palsy caused by periventricular leukomalacia; quadriplegia is the most severe.