Bulbar syndrome (another name for the disease is bulbar palsy) is a pathology in which several cranial nerves are damaged: the vagus, glossopharyngeal, hypoglossal). The nuclei of these cells are located in the medulla oblongata in the so-called bulbar zone.
These nerves are responsible for the innervation of the lips, tongue, palate, larynx, and vocal cords. Damage to these nerves causes disturbances in speech, chewing and swallowing, and taste sensitivity.
The causes of bulbar syndrome can be different: impaired blood flow in the medulla oblongata, damage to nerve fibers, injuries to the base of the skull, infectious diseases, tumors. Treatment of the syndrome depends on the causes of the disease.
Folk remedies are used in treatment. This therapy normalizes tissue nutrition and improves the overall health of a person.
Why does bulbar syndrome develop? Causes
In bulbar syndrome, the following cranial nerves are affected:
wandering;
When the motor nerves are damaged, the patient develops peripheral paralysis. A number of diseases and pathological processes can lead to the development of such paralysis. The lesion may affect the nuclei of neurons located in the medulla oblongata, or the nerve processes that directly innervate muscle structures. If the nuclei of neurons are affected, then in most cases peripheral paralysis is bilaterally symmetrical.
Thus, the main causes of bulbar syndrome are:
- disturbance of blood circulation and nutrition of the tissues of the medulla oblongata;
- benign and malignant tumors;
- swelling of the medulla oblongata, which develops against the background of damage to other parts of the brain;
- trauma to the base of the skull;
- inflammatory processes in the brain: encephalitis;
- damage to nervous tissue: neuropathy, poliomyelitis;
- various amyotrophies;
- and the effects of botulinum toxin on the brain.
The development of bulbar syndrome may be associated with an autoimmune process. In this case, a person’s immune complexes recognize his own cells as foreign and attack them. In this case, muscle tissue is damaged. As the disease progresses, muscle fibers weaken and, over time, atrophy—the patient develops myasthenic paralysis. In this case, the nerve fibers and centers in the medulla oblongata are not affected, but the symptoms are similar to typical manifestations of bulbar syndrome.
Depending on the nature of the development of bulbar syndrome, acute and progressive forms of the disease are distinguished.
- Acute bulbar syndrome in most cases is a consequence of circulatory disorders in the medulla oblongata (hemorrhagic or ischemic stroke), vascular embolism. This condition also occurs when the medulla oblongata descends and pressure is placed on it by the edges of the foramen magnum.
- Progressive bulbar syndrome is a less critical condition. This disease develops against the background of amyotrophic sclerosis, a degenerative disease in which motor neurons are damaged.
Impaired functioning of nerve fibers leads to malnutrition and atrophy of muscle tissue. The patient gradually develops bulbar palsy. If degenerative processes spread to the nerves innervating the respiratory muscles, this will lead to the death of the patient from suffocation.
Disruption of the normal functioning of the medulla oblongata is manifested not only by bulbar palsy, but also by a number of other disorders. This part of the brain contains important centers that control breathing and heartbeat. If damage affects them, the patient may die.
What is bulbar syndrome and the causes of its occurrence?
If the main parts of the nervous system are damaged, human life is supported by the autonomous functioning of certain elements. Their work is not regulated by the cerebral cortex. These elements are neurons. Their independent activity leads to the fact that complex motor acts (breathing, swallowing, speech) are carried out with disturbances.
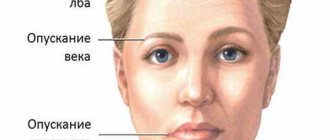
photos of people with bulbar syndromes
Coordinated activity of different muscle groups is possible only with the clearest possible coordination in the work of different parts of the brain. The autonomous functioning of subcortical structures cannot ensure this.
When the higher sections cease to regulate the motor nuclei (a collection of nerve cells) located in the medulla oblongata, a person develops pseudobulbar syndrome.
The absence of a “manager” activates the operation of the cores in autonomous mode.
Such isolated activities have the following consequences:
- complete preservation of the functioning of vital systems of the body (cardiovascular and respiratory);
- paralysis of the soft palate leads to impaired swallowing;
- speech becomes unintelligible;
- inactivity of the vocal cords and impaired phonation.
Spontaneous contraction of the facial muscles leads to the appearance of grimaces that imitate various emotional situations.
Understanding the development process of any disease allows doctors to promptly and promptly select an effective treatment regimen.
This syndrome occurs as a result of damage to the neural pathways through which information from the cerebral cortex enters the nuclei.
In the vast majority of cases, the main causes of this disorder may be the following conditions:
- hypertension (high blood pressure), which favors the development of ischemic and hemorrhagic stroke;
- the presence of atherosclerotic plaques in the arterioles of the brain;
- circulatory disorders caused by unilateral damage to the blood vessels supplying the brain;
- traumatic brain injuries of various types;
- vasculitis arising from diseases such as tuberculosis or syphilis;
- brain injury during childbirth;
- metabolic disorders with long-term use of drugs containing valproic acid;
- malignant neoplasms and benign tumors in the frontal lobes or subcortical structures;
- inflammation of brain tissue caused by diseases of infectious etiology.
Pseudobulbar syndrome mainly develops as a result of many chronic processes that are at the stage of progression. Acute oxygen starvation is a factor that also contributes to the development of this unpleasant condition.
How to understand that it is bulbar syndrome?
Bulbar syndrome is manifested by characteristic signs of damage to the cranial nerves. There are three characteristic symptoms indicating the development of bulbar palsy:
- Dysphagia or impaired swallowing process.
- Dysarthria or impairment of articulate speech.
- Aphonia is a disturbance in the sound of speech.
Characteristic manifestations of bulbar syndrome:
- paresis of half the tongue;
- deviation of the tongue towards the affected side;
- folding of the mucous membrane gradually appears;
- sagging of the velum;
- deviation of the uvula also in the direction of the lesion;
- the patient's palatal and pharyngeal reflexes disappear;
- the swallowing process is disrupted, liquid food may enter the respiratory tract or nose;
- Some patients experience increased salivation and drooling;
- speech disorder.
A patient with bulbar syndrome has difficulty swallowing solid food. Liquid food can enter the respiratory tract because the innervation of the soft palate is impaired. These patients have an increased risk of developing pneumonia.
Due to a violation of the innervation of the tongue, the patient’s speech becomes inarticulate. He speaks nasally, “in the nose.” He has difficulty pronouncing the sounds “l” and “r”. The voice becomes dull and hoarse.
The disease causes paresis of the muscles of the tongue, upper palate, larynx, and pharynx. Often a unilateral lesion develops. The occurrence of bilateral paralysis indicates damage to the neuronal nuclei in the medulla oblongata. Such a lesion is life-threatening for the patient.
Amyotrophic lateral sclerosis - symptoms and diagnosis
A neurologist can diagnose bulbar palsy by carefully studying the patient’s neurological status. The study of the function of the bulbar nerves includes assessment of the speed and intelligibility of speech, timbre of voice, volume of salivation; examination of the tongue for the presence of atrophies and fasciculations, assessment of its mobility; examination of the soft palate and checking the pharyngeal reflex.
It is important to determine the respiratory rate and heart rate, and study the pulse to detect arrhythmia. Laryngoscopy allows you to determine the lack of complete closure of the vocal cords.
How is bulbar syndrome diagnosed?
During diagnosis, it is important to accurately determine the cause of bulbar syndrome. For these purposes, a number of studies are carried out:
- computer or magnetic resonance imaging of the brain;
- electromyographic study of muscle fiber conductivity;
- esophagoscopic examination.
It is necessary to differentiate bulbar and, which manifest themselves with similar symptoms, but have different causes. Pseudobulbar palsy is caused by a disruption of connections between the medulla oblongata and other higher nerve centers. In this case, muscle atrophy and peripheral paralysis do not develop.
Causes of the disease
Brain disorders that cause bulbar syndrome can have a huge number of causes, which can be grouped into several general groups:
- Hereditary abnormalities, mutations and organ changes.
- Brain diseases, both traumatic and infectious.
- Other infectious diseases.
- Toxic poisoning.
- Vascular changes and tumors.
- Degenerative changes in brain and nerve tissue.
- Bone abnormalities.
- Disorders of intrauterine development.
- Autoimmune disorders.
Each group contains a large number of individual diseases, each of which can cause complications on the bulbar group of nuclei of the brain and on its other parts.
How to treat bulbar syndrome?
The development of bulbar syndrome is always associated with some pathological process in the body: dysfunction of the medulla oblongata, damage to nerve fibers, autoimmune damage to muscle tissue. It is necessary to determine the cause of the disease and select appropriate treatment.
Symptomatic treatment is also carried out - therapy aimed at eliminating the manifestations of bulbar syndrome and alleviating the patient’s condition. There are folk remedies that are used to treat paralysis.
- Medicinal collection No. 1. In equal proportions you need to mix the herbs of mistletoe, oregano and yarrow and valerian roots. You need to prepare an infusion from the mixture (1 tbsp per 200 ml of boiling water). Take this remedy half a glass 3 times a day before meals.
- Medicinal collection No. 2. Prepare a mixture of 1 part mint leaves, oregano, mistletoe and motherwort and 2 parts lemon balm and thyme. The mixture should be poured with boiling water (take 1 tablespoon for 1 glass of water), leave in a thermos for 1 hour, then strain. Standard dosage: 100 ml of this drug an hour after meals.
- Peony roots. It is necessary to prepare an alcohol tincture of peony roots. To do this, the roots are rubbed and filled with alcohol in a ratio of 1:10. The roots are infused in a warm place for a week, after which the tincture is filtered. Standard dosage for an adult: 35 drops three times a day before meals. The child should take 15–20 drops of the drug 3 times a day before meals. You can also prepare an infusion of peony roots. The crushed roots are poured with boiling water (in the ratio of 1 tablespoon per half liter of boiling water), left for 1 hour and filtered. This infusion should be drunk 1 tbsp. l. adults and 1 tsp. children also three times a day before meals.
- Tanning or dyeing sumac. Fresh leaves of this plant are used to treat paralysis. You can steam 1 tbsp in a glass of boiling water. l. leaves, leave in a warm place for an hour, then filter. Standard dosage: 1 tbsp. l. this infusion 3-4 times a day.
- Sage. Prepare a saturated sage solution. 100 g of dried herb is poured with half a liter of boiling water and left warm overnight, filtered the next morning. The standard dosage of this infusion: 1 tablespoon 3-4 times a day, an hour after meals. You can also take healing baths with a decoction of sage herb or rosehip roots and fruits. For one bath you need to take 200–300 g of plant material, boil it in 1.5 liters of water for 5–10 minutes, then let it sit for another hour, filter it and pour it into the bath. The procedure lasts half an hour. Take a bath several times a week.
Bulbar palsy (BP) is characterized by damage to groups of nerve fibers and their nuclei. The main symptom of the disease is a decrease in the motor activity of muscle groups. Bulbar syndrome leads to unilateral and bilateral damage to areas of the brain.
Symptoms of the disease
This pathology causes partial or complete paralysis of the muscles of the face, tongue, palate, and larynx, for which the glossopharyngeal, vagus, and sublingual nerve fibers are responsible.
The main symptoms of bulbar palsy:
- Swallowing problems. With bulbar syndrome, disturbances occur in the functioning of the muscles that carry out the swallowing process. This leads to the development of dysphagia. With dysphagia, the muscles of the tongue, soft palate, epiglottis, pharynx and larynx lose their functionality. In addition to dysphagia, aphagia develops - the absence of a swallowing reflex. Water and other liquids enter the nasal cavity, solid food enters the larynx. There is profuse drooling from the corners of the mouth. It is not uncommon for food to enter the trachea or lung cavity. This leads to the development of aspiration pneumonia, which, in turn, can be fatal.
- Speech impairment and complete or partial loss of the ability to speak. The sounds produced by the patient become muffled, often incomprehensible to perception - this indicates the development of dysphonia. Complete loss of voice – progressive aphonia.
- During the development of bulbar palsy, the voice becomes weak and muffled, and nasal sound occurs—speech “in the nose.” Vowel sounds become almost indistinguishable from each other, and consonants become indistinct. Speech is perceived as incomprehensible and barely audible; when trying to pronounce words, a person gets very and quickly tired.
Paralysis of the tongue leads to problematic articulation or its complete disruption, and dysarthria appears. Complete paralysis of the tongue muscles may develop - anarthria.
With these symptoms, the patient is able to hear and understand the speech of the interlocutor, but he cannot answer.
Bulbar palsy can lead to the development of problems in the functioning of other organs. First of all, the respiratory system and cardiovascular system suffer. The reason for this is the close proximity of the affected areas of nerve fibers to these organs.
Factors of occurrence
The occurrence of bulbar palsy is associated with many diseases of various origins and is their consequence. These include:
- Oncological diseases. With the development of neoplasms in the posterior cranial fossa. For example, brainstem glioma.
- Ischemic stroke of cerebral vessels, infarction of the medulla oblongata.
- Amyotrophic sclerosis.
- Genetic diseases, such as Kennedy's disease.
- Diseases of an inflammatory-infectious nature (Lyme disease, Guyon-Barré syndrome).
- This disorder is a manifestation of other complex pathologies occurring in the body.
Therapeutic measures
Treatment of bulbar palsy directly depends on the primary (main) disease.
The more effort is put into eliminating it, the greater the chance of improving the clinical picture of the pathology.
Treatment of paralysis consists of resuscitating lost functions and maintaining the vitality of the body as a whole. For this, vitamins are prescribed to restore swallowing function; in addition, ATP and Prozerin are recommended.
To restore normal breathing, artificial ventilation is prescribed. Atropine is used to reduce saliva volume. The prescription of Atropine is caused by the need to reduce the volume of secreted secretions - in a sick person its amount can reach 1 liter. But even the measures taken do not guarantee recovery - only an improvement in overall well-being.
Characteristics of pseudobulbar palsy
Pseudobulbar palsy (PBP) is a centralized paresis of muscles, the activity of which directly depends on the full functioning of the bulbar nerve fibers. Unlike bulbar palsy, which is characterized by both unilateral and bilateral lesions, pseudobulbar syndrome occurs only with complete destruction of the nuclear pathways, which include the entire length from the cortical centers to the nuclei of the nerve fibers of the bulbar group.
With PBP, the functioning of the muscles of the pharynx, vocal cords, and speech articulation are disrupted. As with the development of PD, pseudobulbar syndrome may be accompanied by dysphagia, dysphonia or aphonia, and dysarthria. But the main difference is that with PBP there is no atrophy of the lingual muscles and defibrillary reflexes.
A sign of PBS is considered to be uniform paresis of the facial muscles; it is rather centralized in nature - spastic, when muscle tone is increased. This is most expressed in a disorder of differentiated and voluntary movements. At the same time, the reflexes of the lower jaw and chin increase sharply.
Unlike PD, atrophy of the muscles of the lips, pharynx and soft palate is not diagnosed during the development of PBP.
With PBP, there are no changes in the functioning of the respiratory and cardiovascular systems. This is due to the fact that destructive processes occur higher than the medulla oblongata. From which it follows that PPS does not have the consequences characteristic of bulbar palsy; vital functions are not impaired during the development of the disease.
Bulbar disorder
Bulbar syndrome occurs due to damage to the nuclei located in the medulla oblongata.
These nuclei are clusters of cells of the nervous system and take an active part in regulating the coordination of movements, the formation of emotions and other vital functions.
Violations can develop for the following reasons:
- Mechanical compression and injury to the nuclei as a result of a benign or malignant brain tumor.
- Circulatory failure due to stroke.
- Viral diseases affecting the nervous system.
- Botulism
Damage to the nuclei leads to the development of a pathological condition, the characteristic feature of which is severe peripheral paralysis. Degenerative changes in the muscles of the pharynx or soft palate make it difficult for a person to swallow and speak. The nature of the clinical picture is largely determined by the degree of damage to nerve cells.
The main symptoms are:
- Increased salivation.
- There is no facial expression.
- Half-open mouth.
- The soft palate droops.
- The presence of the tongue outside the oral cavity with a characteristic deviation to the side and short-term twitching.
- Speech is difficult to understand.
- Weakening or complete loss of voice during a conversation.
Bulbar syndrome is accompanied by disruption of the cardiovascular system and respiratory organs. As a result, the patient experiences a weak or rapid pulse, as well as deviations in the heartbeat rhythm. There is a disruption in breathing movements with the appearance of pauses in the breathing process.
- If pseudobulbar syndrome is detected, the doctor determines a treatment regimen that will focus on the treatment of the underlying disease. If the disease has developed as a result of hypertension, therapy is prescribed aimed at reducing blood pressure and normalizing the functioning of the cardiovascular system.
- Antibacterial drugs are effective for vasculitis due to syphilis or pulmonary tuberculosis. An important element of an integrated approach are medications that improve microcirculation in the brain and normalize the activity of the central and peripheral nervous system.
- There is currently no classical treatment regimen for pseudobulbar syndrome. The therapeutic course is drawn up based on the disorders present in the patient. The use of special exercises and physiotherapeutic procedures have proven themselves to be effective. This approach is an important part of complex therapy.
It is not possible to completely overcome this problem. However, adequate drug therapy and special classes aimed at speedy rehabilitation favor the fact that a person gradually adapts to the problems that have arisen. Strict adherence to the doctor’s recommendations will not only slow down the development of the underlying pathology, but also preserve nerve cells.
Bulbar and pseudobulbar syndromes have many similarities with each other. They are rightfully serious pathologies of the nervous system. When structural elements of the brain are damaged, the risk of disruption of the functioning of vital systems and organs increases significantly.
Observable reflexes when disrupted
The main sign of the development of this disease is considered to be involuntary crying or laughter when a person exposes his teeth, and if something is passed over them, for example, a feather or a small sheet of paper.
PBS is characterized by reflexes of oral automatism:
- Bekhterev's reflex. The presence of this reflex is determined by lightly tapping the chin or using a spatula or ruler that lies on the lower row of teeth. A positive result is considered to be the case if there is a sharp contraction of the chewing muscles or clenching of the jaws.
- Proboscis reflex. In specialized literature you can find other names, for example, kissing. To trigger it, lightly tap on the upper lip or near the mouth, but it is necessary to touch the orbicularis muscle.
- Korchikyan's distance-oral reflex. When testing this reflex, the patient’s lips do not touch; a positive result occurs only if the lips are automatically extended with a tube without touching them, only when any object is presented.
- Naso-labial reflex Astvatsaturov. The presence of contractions of the facial muscles occurs when lightly tapping the back of the nose.
- Marinescu-Radovic palmomental reflex. It is caused by irritation of the skin in the area under the thumb. If the facial muscles on the side of the irritated hand contract involuntarily, then the reflex test is positive.
- Janyshevsky's syndrome is characterized by convulsive clenching of the jaws. To test for the presence of this reflex, a stimulus is applied to the lips, gums, or hard palate.
Although even without the presence of reflexes, the symptoms of PBP are quite extensive. This is primarily due to damage to many areas of the brain. In addition to positive reactions to the presence of reflexes, a sign of PBS is a noticeable decrease in motor activity. The development of PBS is also indicated by memory deterioration, lack of concentration, decrease or complete loss of intelligence. This is caused by the presence of many softened brain foci.
A manifestation of PBS is an almost motionless face that resembles a mask. This is due to paresis of the facial muscles.
When diagnosing pseudobulbar palsy, in some cases a clinical picture similar to the symptoms of central tetraparesis may be observed.
Concomitant diseases and treatment
PBS appears in combination with such disorders as:
- Acute cerebrovascular accidents in both hemispheres.
- Encephalopathy.
- Amyotrophic lateral sclerosis.
- Atherosclerosis of cerebral vessels.
- Multiple sclerosis.
- Motor neuron disease.
- Tumors of some parts of the brain.
- Traumatic brain injuries.
In order to alleviate the symptoms of the disease as much as possible, the drug Proserin is most often prescribed. The treatment process for PBS is aimed at treating the underlying disease. Drugs that improve blood clotting and accelerate metabolic processes must be prescribed. To enhance oxygen supply to the brain, the drug Cerebrolysin and others are prescribed.
Modern techniques offer treatment for paralysis with stem cell injections.
And to alleviate the suffering of the patient, careful oral care is necessary. When eating, be as careful as possible to prevent pieces of food from entering the trachea. It is advisable that nutrition be provided through a tube passed through the nose into the esophagus.
Bulbar and pseudobulbar palsy are secondary diseases, the cure of which depends on improving the overall clinical picture.
One of the most dangerous neurological disorders is bulbar syndrome. This symptom complex occurs with combined peripheral damage to several pairs of cranial nerves of the caudal group. Bulbar syndrome that quickly appears and increases in severity is potentially life-threatening. In this case, emergency hospitalization of the patient is necessary to monitor his condition and provide intensive care.
Differential diagnosis
It is necessary to correctly differentiate bulbar syndrome from pseudobulbar palsy. Their manifestations are very similar, however, there is a significant difference. Pseudobulbar palsy is characterized by reflexes of oral automatism (proboscis reflex, distance-oral and palmar-plantar reflex), the occurrence of which is associated with damage to the pyramidal tracts.
The proboscis reflex is detected by carefully tapping the upper and lower lips with a neurological hammer - the patient pulls them out. The same reaction can be observed when the hammer approaches the lips - the distance-oral reflex. Streak irritation of the skin of the palm above the eminence of the thumb will be accompanied by contraction of the mentalis muscle, causing the skin to be pulled up on the chin - the palmomental reflex.
Pathogenesis
Depending on the etiology of the underlying disease, there is a disruption of synaptic transmission with relative structural preservation of the main formations, destruction of nuclei or pronounced compression of nerve structures. In this case, there is no disruption of the conduction of impulses along the cortical-nuclear pathways and damage to central motor neurons in the frontal region of the brain, which distinguishes bulbar syndrome from. This is important not only for diagnosing the level of damage in the central nervous system and determining the cause of the formation of the main symptoms, but also for assessing the prognosis of the disease.
Bulbar syndrome develops with simultaneous damage to the IX, X and XII pairs of cranial nerves. The pathological process can involve their motor nuclei in the medulla oblongata (previously called the bulb), roots extending to the base of the brain, or already formed nerves. Damage to the nuclei is usually bilateral or bilateral; mosaicism is not typical for this syndrome.
Paralysis of the muscles of the tongue, soft palate, pharynx, epiglottis and larynx that develops with bulbar syndrome is classified as peripheral. Therefore, they are accompanied by a decrease or loss of the palatine and pharyngeal reflex, hypotonicity and subsequent atrophy of paralyzed muscles. It is also possible that fasciculations may appear when examining the tongue. And the subsequent involvement of neurons of the respiratory and vasomotor centers in the medulla oblongata in the pathological process, and a violation of parasympathetic regulation become the cause of the development of life-threatening conditions.
What causes the symptoms
Symptoms of the pathology are caused by damage to an entire group of brain organs, specifically the nuclei of several nerves located in the medulla oblongata, their intracranial or external roots. With bulbar syndrome, damage to any one nucleus almost never occurs with the loss of only one function, since these organs are located very close to each other and also have a very small size, which is why they are affected simultaneously.
Due to the lesion, the nervous system loses connection with the organs of the pharynx and can no longer control them either consciously or unconsciously at the level of reflexes (when a person automatically swallows saliva).
A person has 12 pairs of cranial nerves, which appear in the second month of prenatal life, which consist of brain matter and are located in the very center of the brain between its hemispheres. They are responsible for the human senses and the functioning of the face as a whole. At the same time, they have motor, sensory function, or both at once.
The nerve nuclei are unique command posts: ternary, facial, glossopharyngeal, hypoglossal, etc. Each nerve is paired, so their nuclei, which are located symmetrically relative to the medulla oblongata, are also paired. In bulbar syndrome, the nuclei responsible for the glossopharyngeal, hypoglossal or vagus nerve are affected, which has mixed functions in innervating the pharynx, soft palate, larynx, esophagus, and has a parasympathetic effect (exciting and contracting) on the stomach, lungs, heart, intestines, pancreas, responsible for the sensitivity of the mucous membrane of the lower jaw, pharynx, larynx, part of the auditory canal, eardrum and other less important parts of the body. Since the nuclei are paired, they can be damaged either completely or only half of them, located on one side of the medulla oblongata.
Impairment or damage to the vagus nerve in bulbar palsy can cause a sudden stop in the contractions of the heart, respiratory system, or disruption of the gastrointestinal tract.
Main reasons
The cause of bulbar syndrome can be:
- vascular accidents in the vertebrobasilar region, leading to ischemic or hemorrhagic damage to the craniospinal region;
- primary and metastatic tumors of the brainstem and medulla oblongata, sarcomatosis, granulomatosis of various etiologies;
- conditions that give a positive mass effect without a clearly defined formation in the posterior cranial fossa and threaten wedging of the brain into the foramen magnum (hemorrhages, swelling of the nervous tissue in neighboring areas or acute diffuse brain damage);
- leading to compression of the medulla oblongata;
- fracture of the base of the skull;
- and various etiologies;
- polyneuropathy (paraneoplastic, diphtheria, Guillain-Barre, post-vaccination, endocrine), ;
- , as well as genetically determined spinal-bulbar amyotrophy Kennedy, and bulbospinal amyotrophy of childhood (Fazio-Londe disease);
- suppression of brain motor neuron activity by botulinum toxin.
Many authors also classify changes in the muscles of the soft palate, pharynx and larynx as bulbar syndrome. In this case, their cause is a violation of neuromuscular transmission or primary damage to muscle tissue in myopathies, or dystrophic myotonia. The medulla oblongata (bulb) remains intact in myopathic diseases, so they speak of a special form of bulbar palsy.
Forecast
The prognosis is determined by the nature of the pathological process that caused the disease and the severity of clinical symptoms. Mostly unfavorable.
Treatment consists of treating the underlying disease. To improve swallowing function, proserin, glutamic acid, vitamins, ATP are prescribed; in case of breathing problems, artificial respiration is prescribed; in case of salivation, atropine is prescribed. Tube feeding. When indicated, dehydration therapy is carried out (see), vasodilators and drugs that normalize blood clotting are prescribed.
Bibliography:
Bogolepov N.K. Impaired motor functions in vascular lesions of the brain, M., 1953, bibliogr.; aka, Neuropathology, Emergency Conditions, M., 1967; Zakharchenko M. A. Vascular diseases of the brain stem, blockage of art. cerebelli inferior posterior, M., 1911; Mankovsky B. N. Progressive bulbar palsy, Multivolume, manual on neurol., ed. N. I. Grashchenkova, t. 7, p. 109, D., 1960; Duchenne GB A. Paralysie musculaire progressive de la langue, du voile, du palais et des livres, affection non encore decrite comme espfece morbide distincte, Arch. gin. M6d., t. 16, p. 283, 1860; Erb WH Zur Gasuistik der bulbaren Lahmungen, Arch. Psychiat. Nervenkr., Bd 9, S. 325, 1878-1879; Goldflam S. Uber einen scheinbar heilbaren bulbarparalytischen Symptomen Komplex mit Beteiligung der Extremitaten, Dtsch. Z. Nervenheilk., Bd 4, S. 312, 1893; Wallenberg A. Verschluss der Arteria cerebelli inferior posterior dextra (mit Sektionsbefund), ibid., Bd 73, S. 189, 1922.
HK Bogolepov.
Clinical picture
A characteristic sign of bulbar syndrome is deviation of the tongue towards the affected side.
Combined peripheral damage to the glossopharyngeal, vagus and hypoglossal nerves leads to paresis of the muscles of the palate, pharynx, larynx, and tongue. Characteristic is the combination of the triad “dysphonia-dysarthria-dysphagia” with paresis of half the tongue, sagging of the palatal curtain and the disappearance of the pharyngeal and palatal reflexes. Changes visible in the oropharynx are most often asymmetrical; the appearance of bilateral bulbar symptoms is a prognostically unfavorable sign.
Upon examination, deviation (deviation) of the tongue towards the lesion is revealed. Its paralyzed half becomes hypotonic and inactive, and fasciculations may appear in it. With bilateral bulbar palsy, there is almost complete immobility of the entire tongue, or glossoplegia. Due to the increasing atrophy of the paretic muscles, the affected half of the tongue gradually becomes thinner and becomes pathologically folded.
Paresis of the muscles of the soft palate leads to immobility of the palatine arches, sagging and hypotension of the palatine curtain with deviation of the uvula to the healthy side. Together with the loss of the pharyngeal reflex, disruption of the functioning of the muscles of the pharynx and epiglottis, this becomes the cause of dysphagia. There are difficulties when swallowing, choking, reflux of food and liquids into the nasal cavity and respiratory tract. Therefore, patients with bulbar syndrome have a high risk of developing aspiration pneumonia and bronchitis.
When the parasympathetic portion of the hypoglossal nerve is damaged, the autonomic innervation of the salivary glands is disrupted. The resulting increase in saliva production, together with impaired swallowing, causes drooling. Sometimes it is so pronounced that patients are forced to constantly use a scarf.
Dysphonia in bulbar syndrome is manifested by nasality, deafness and hoarseness of the voice due to paralysis of the vocal cords and paresis of the soft palate. The nasal tone of speech is called nasolalia; such nasalization of sound pronunciation can appear in the absence of obvious disorders of swallowing and choking. Dysphonia is combined with dysarthria, when slurred speech occurs due to impaired mobility of the tongue and other muscles involved in articulation. Damage to the medulla oblongata often leads to a combination of bulbar syndrome with facial nerve paresis, which also affects speech intelligibility.
With severe paralysis of the muscles of the palate, pharynx and larynx, asphyxia may occur due to mechanical blocking of the lumen of the respiratory tract. With bilateral damage to the vagus nerve (or its nuclei in the medulla oblongata), the work of the heart and respiratory system is inhibited, which is due to a violation of their parasympathetic regulation.
Symptoms
Against the background of formed bulbar palsy, people most often experience an aphagia syndrome complex, in which it is difficult for a person to swallow a bolus of food. At the same time, impaired articulation of words and changes in voice modulation are diagnosed - nasality, hoarseness.
Dysfunction in this syndrome affects the autonomic nervous system - in the form of a malfunction in the cardiovascular structures. The main signs of bulbar palsy:
- facial expressions are suppressed, up to complete absence,
- chewing – impossible to do on your own,
- closing the mouth is difficult,
- penetration of liquids into the nasopharynx due to sagging of the soft palate,
- suppression of the palatine and pharyngeal reflex,
- speech is unclear, choppy,
- constant drooling,
- phonation is impaired.
Damage to the respiratory and vascular centers at the same time will have a serious impact on a person’s well-being, often leading to death. In addition to dysphagia, dysarthria, and dysphonia, examination reveals weakness in the muscles of the pharynx and tongue, as well as groups of masticatory/facial muscles.
Symptoms with manifestations of bulbar palsy can be mild at the initial stage of the onset of the disorder or so severe that the person requires emergency resuscitation measures.
Treatment
It is not the bulbar syndrome itself that requires treatment, but the underlying disease and the resulting life-threatening conditions. If the severity of symptoms increases and signs of cardiac and respiratory failure appear, the patient requires transfer to the intensive care unit. According to indications, mechanical ventilation is performed and a nasogastric tube is installed.
To correct disorders, in addition to etiotropic therapy, drugs of various groups with neurotrophic, neuroprotective, metabolic, and vascular effects are prescribed. Hypersalivation can be reduced with atropine. During the recovery period or for chronic diseases, massage, classes with a speech therapist, and kinesiotherapy are prescribed to improve speech and swallowing.
Bulbar syndrome is a serious sign of damage to the medulla oblongata. Its appearance requires a mandatory visit to a doctor to clarify the etiology and decide on the need for hospitalization.
Petrov K. B., MD, professor, brings to your attention a slide show about clinical variants of bulbar syndrome and non-drug methods of treating this condition:
Damage to the IX, X and XII nerves of the skull or their nuclei causes bulbar syndrome.
At the same time, it is observed
paralysis of the palatine and lingual muscles, vocal cords, epiglottis, impaired sensitivity of the mucous membrane of the nasopharynx, larynx, trachea with certain manifestations: problems with swallowing, food getting into the respiratory system, speech abnormalities, taste disturbances on the back of the tongue, autonomic disorders.
Pseudobulbar syndrome occurs as a result of bilateral damage to cortical fibers. With unilateral dysfunction of the nerves, except for the XII pair, are not impaired, because their nuclei have bilateral innervation.
Treatment methods
Bulbar palsy and pseudobulbar syndromes are diagnosed using the following methods:
- General urine and blood tests.
- Electromyogram is a study of nerve conduction in the muscles of the face and neck.
- Tomography of the brain.
- Examination by an ophthalmologist.
- Esophagoscopy is an examination of the esophagus with a probe and a video camera.
- Analysis of cerebrospinal fluid - brain fluid.
- Tests for myasthenia gravis is an autoimmune disease characterized by extreme fatigue of striated muscles. Autoimmune diseases are disorders in which one’s own enraged immune system begins to kill.
Treatment methods and the possibility of complete recovery from bulbar or pseudobulbar palsy depend on the exact cause of their occurrence, since it is a consequence of other diseases. Sometimes it is possible to restore completely all functions, for example, if the disease was not caused by complete damage, but only by irritation of the brain due to infection, but more often during treatment the main goal is to restore vital functions: breathing, heartbeat and the ability to digest food, and it is also possible smooth out the symptoms somewhat.
When some areas of the brain are damaged, serious pathological processes can appear that reduce a person’s standard of living, and in some cases, threaten death.
Bulbar and pseudobulbar syndrome are disorders of the central nervous system, the symptoms of which are similar to each other, but their etiology is different.
Bulbar occurs due to damage to the medulla oblongata - the nuclei of the glossopharyngeal, vagus and hypoglossal nerves that are located in it.
Pseudobulbar syndrome (paralysis) manifests itself due to disruption of the conductivity of the corticonuclear pathways.
Causes of syndromes
The main causes of bulbar syndrome include various diseases.
At the onset of the disorder, there is difficulty swallowing liquid food. However, as the disorder develops, along with weakness of the tongue, weakness of the facial and masticatory muscles appears, and the tongue becomes immobile.
Dystrophic myotonia most often affects men. The disease begins at 16 years of age.
Bulbar syndrome causes
dysphagia, nasal tone of voice, choking, and in some cases, breathing problems; attacks of muscle weakness.
The development of the disorder is provoked by increased salt consumption, carbohydrate-rich foods, stress and negative emotions, debilitating physical activity. Pseudobulbar syndrome involves two parts of the medulla oblongata.
Psychogenic disorders can be combined with psychotic disorders and conversion disorders.
This disorder manifests itself with central swallowing paralysis, changes in speech phonation and articulation.
Disorders manifest themselves in the following diseases:
- Alzheimer's disease;
- amaurotic idiocy;
- amyotrophy;
- Kennedy's disease;
- damage to the arteries of the brain;
- botulism;
- bulbar palsy;
- thrombosis of the venous sinuses;
- glycogenosis;
- Gaucher disease;
- diffuse sclerosis;
- myasthenia gravis;
- olivopontocerebellar degeneration;
- brain formation;
- polyradiculoneuropathy;
- polyneuropathy;
- myelinolysis;
- syringobulbia;
- myopathy;
- encephalomyelitis;
- Binswanger encephalopathy.
Clinical picture
Bulbar and pseudobulbar syndromes have many similar symptoms and signs, since the common feature of these disorders is the effect on one muscle.
But if pseudobulbar deviation occurs due to a disorder of the central motor neuron
, then bulbar -
when a peripheral neuron is damaged
. That is, pseudobulbar palsy is central, and bulbar palsy is peripheral.
Accordingly, in the clinic of pseudobulbar disorder, the main thing is an increase in muscle tone, the occurrence of unhealthy reflexes and the absence of muscle atrophy.
In the bulbar clinic, the main factors are muscle weakness, the appearance of muscle twitching, the death of muscle tissue, and the absence of reflexes.
Manifestations of both types of lesions simultaneously occur when.
Bulbar and pseudobulbar syndrome in children
For pediatric practice, the pseudobulbar form is most significant.
Pseudobulbar form
Children with pseudobulbar disorder often stay in auxiliary schools
, because its external manifestations are so severe that they force doctors and teachers to send children without intellectual problems only because of speech to special schools, and sometimes even to social security institutions.
From the neurological side, this form has a complex picture:
Together with central paralysis of the muscles of the speech apparatus, the baby experiences changes in muscle tone, hyperkinesis, and other movement disorders.
The complexity of the disease also determines the characteristics of its manifestations.
This form of deviation in children is usually a manifestation of cerebral palsy, which often appears before 2 years of age due to brain diseases. Cerebral palsy is often a consequence of trauma during childbirth.
Motor impairments in these children are widespread.
Often affected
the upper part of the face, which is why it is motionless, there is general awkwardness and clumsiness. Parents notice that the baby cannot take care of himself and does not actively move.
All non-speech functions involving the tongue, lips and other parts of the speech apparatus are also impaired: the child has difficulty chewing food, swallowing, and cannot swallow or retain saliva.
Bulbar syndrome
Bulbar dysarthria occurs when there is inflammation or formation of the medulla oblongata.
In this case, the nuclei of the motor cranial nerves located there die.
Characterized by paresis
muscles of the pharynx, tongue, soft palate.
A child with this disorder has difficulty swallowing food and has difficulty chewing.
In children with this form of deviation, the muscles of the tongue and pharynx die. Speech is unclear and slow. The face of a baby with bulbar dysarthria is motionless.
Treatment of the disease
In some cases, urgent assistance is necessary to save life with bulbar syndrome.
The main goal of this assistance is to neutralize the threat to the patient’s life
, before being taken to a medical facility, where treatment will then be determined and prescribed.
The doctor, in accordance with the symptoms and nature of the disorder, can predict the outcome of the disease, as well as the effectiveness of the prescribed treatment for bulbar syndrome, which is carried out in stages, namely :
- resuscitation, support of body functions that were impaired due to the disorder - restoration of breathing, activation of the swallowing reflex, reduction of salivation;
- This is followed by treatment of manifestations aimed at alleviating the patient;
- treatment of the disease that caused the syndrome;
- Patients are fed using a feeding tube.
The photo shows special gymnastics for bulbar syndrome
Good results are achieved in the treatment of pseudobulbar syndrome using stem cells.
Their administration to a patient with pseudobulbar disorder leads to the fact that they replace functionally affected cells. As a result, the person begins to live normally.
to carefully monitor the oral cavity in case of pseudobulbar and bulbar syndromes
, and also, if necessary, monitor the patient while eating so that he does not suffocate.
Diagnosis of the disease
After consulting a therapist, to diagnose bulbar syndrome it is usually necessary to undergo a series of studies:
Depending on the clinical symptoms and the nature of the pathology, the doctor can predict the outcome and effectiveness of the proposed treatment for bulbar syndrome. As a rule, therapy is aimed at eliminating the causes of the underlying disease. At the same time, measures are taken to support and resuscitate impaired important body functions, namely:
- Breathing – artificial ventilation;
- Swallowing – drug therapy with proserine, vitamins, ATP;
- Drooling - prescription of atropine.
It is quite important against the background of pseudobulbar and bulbar syndrome to carry out careful care of the oral cavity, and also, if necessary, monitor patients while eating to prevent aspiration.
ALS is a serious disease with inevitable death. Therefore, to make such a diagnosis, it is necessary to conduct a lot of research.
What is taken into account when making a diagnosis:
- The presence of an affected peripheral motor neuron, confirmed by clinical data and instrumental research methods;
- The presence of an affected central motor neuron, confirmed by clinical data;
- Progressive spread of these lesions throughout all parts of the spinal cord;
- Elimination of all other diseases that can cause such symptoms.
- This is a fairly rare disease.
- The disease affects each person differently. In this case, there are not so many common symptoms.
- Early symptoms of amyotrophic lateral sclerosis may be mild, such as slightly slurred speech, awkwardness in the hands, and clumsiness. However, these symptoms may be the result of other diseases.
However, when diagnosing amyotrophic lateral sclerosis, it should be remembered that many diseases occur with selective damage to motor structures. With ALS syndrome, the patient may experience pain in the neck, as well as protein-cell dissociation of the cerebrospinal fluid, a block on the myelogram and loss of sensitivity.
If the doctor has suspicions, he should refer the patient to a neurologist. And only after this may it be necessary to undergo a series of diagnostic studies.
A neurologist prescribes diagnosis and treatment of bulbar palsy. First of all, the specialist conducts a neurological examination and electromyography. Based on the diagnostic results, the doctor identifies the cause of bulbar syndrome and prescribes treatment. The specialist must determine the breathing rate and heartbeat.
The following studies are carried out for bulbar palsy:
- Radiography makes it possible to detect fractures and bruises of the head, and tumor processes.
- Electromyography helps check the performance of the muscles of the tongue, neck, arms, and legs. This type of diagnosis reveals muscle activity in a calm state and during contraction.
- Esophagoscopy. This research method helps to examine the esophagus. The performance of the pharynx muscles and vocal cords is assessed.
- Magnetic resonance imaging. A fast and high-quality diagnostic method that detects various diseases in 90% of cases. MRI makes it possible to evaluate the condition of all organs. Tomography helps identify brain pathologies. The study is most often carried out using a contrast agent.
- Electrocardiogram. Makes it possible to find different heart diseases and study heart rhythm.
- Laboratory tests are carried out to identify inflammatory processes, infections, and hemorrhage. A general analysis of urine, blood and cerebrospinal fluid examination is prescribed.
Prognosis and complications
Depending on the nature of the disorder, the clinical signs that provoked the syndrome, the doctor assumes the outcome and effectiveness of treatment, which is usually aimed at eliminating the causes of the main deviation.
It is also necessary to support and restore impaired body functions: breathing, swallowing, salivation, etc.
Thanks to the use of proven medications, it is often possible to achieve an improvement in the patient’s condition, but it is very rare to achieve a complete cure.
Prevention
Prevention of this disorder consists of preventing serious illnesses that can cause paralysis.
Prevention of pseudobulbar syndrome includes identification and treatment
cerebral atherosclerosis, stroke prevention.
Must be adhered to
work and rest schedule, limit calorie intake, reduce consumption of animal proteins and foods with cholesterol. There is no specific prevention.
It is very important to immediately contact a specialist who will not only select the correct treatment, but also help reduce the manifestations of the disorder in order to improve the patient’s quality of life.