Porencephaly is a rare congenital disease of the central nervous system, which is accompanied by cystic formations or cavities in the cerebral hemisphere. Cysts or cavities are usually remnants of destructive lesions but are sometimes the result of abnormal development. Pathology can develop before or after birth.
The term is used variably among radiologists in its broadest definition being a cleft or cystic cavity in the brain, and its narrower definition being a focal cystic area of encephalomalacia that associates with the ventricular system and/or subarachnoid space.
Poreencephalic cysts were originally described by R. Heschl in 1859.
Poreencephaly has a number of different, often unknown causes, including lack of brain development and destruction of brain tissue. The presence of porencephalic cysts can sometimes be detected by clearing the baby's skull during infancy. The diagnosis can be confirmed by CT, MRI or ultrasound.
More severely affected children show symptoms of the disorder soon after birth, and diagnosis is usually made before age 1 year. Signs may include poor growth and development, spastic paresis (minor or incomplete paralysis), hypotonia (decreased muscle tone), seizures (often infantile spasms), and macrocephaly or microcephaly.
Individuals with porencephaly may often have poor or absent speech development, epilepsy, hydrocephalus, spastic contractures (shrinkage or contraction of muscles), and cognitive impairment.
Terminology
The need for a cyst communicating with the cerebral ventricles and/or subarachnoid space to receive the designation of porencephaly is a matter of debate among radiologists. Some authors use the term for cysts regardless of whether there is a relationship between them. Others use the term for cysts that communicate with at least one space, in which case they divide poendphalic cysts into internal (communicating with the ventricle) or external (communicating with the subarachnoid space). Still others require communication between both.
For the purposes of this article, the term porencephaly is considered to be: a cystic lesion of the brain due to encephaloclastic disorder (eg, intrauterine infections and ischemia) lined by white matter that communicates with the ventricles and/or subarachnoid space.
Clinical picture
As can be expected from the understanding that porencephalic cysts vary widely in size and location, their clinical presentation is also variable. Patients with periencephalic cysts differ from asymptomatic, pathologies with profound disorders.
Signs and symptoms often become apparent in the first year of life, with spasticity and seizures being common early manifestations. Speech impairment, mental retardation, and movement (motor) disorders are also common.
Head circumference is variable. It may be normal or reduced, or, on the contrary, synechiae can create a one-way valve effect with a gradual enlargement of the cyst and skull or hydrocephalus, which leads to an enlargement of the head.
Pathology
Porancephalic cysts are an unusual congenital pathology. Cysts are usually lined with white matter. They are thought to develop as a result of focal encephalomalacia due to localized cerebral damage, most commonly in early pregnancy. Gliosis develops if the disorder is late enough, usually considered after the start of the third trimester, although it is possible that defects as early as 20 weeks of pregnancy can lead to gliosis.
Causes
In modern medicine, there is an opinion that absolutely any factors that influence the formation of local (local) necrosis of human brain tissue become the cause of a porencephalic cyst in a person. In the process of tissue death, a membrane is formed, in turn, the necrotic tissue that is inside it is later replaced by cerebrospinal fluid. This disease can be caused by a viral infection, for example, cytomegalovirus.
A viral infection suffered by a woman during pregnancy can cause a porencephalic cyst of the brain to develop in the child. There are cases where children fell ill after birth. In this case, we are primarily talking about birth injuries. In quite rare cases, a cyst can form due to accidental damage that can be caused by an amniocentesis needle.
In modern medicine, a rather controversial issue is the question that a disease such as porencephalic cyst can be associated with a hereditary factor; whether it is transmitted by genetic predisposition has not yet been precisely identified. This problem is relevant today.
Specialists are actively interested in the problem of the occurrence of porencephalic cysts of the brain, conducting genetic counseling. Today there are suggestions that this disease can be inherited; A woman who gives birth to a child with this type of disorder has a risk of having subsequent children with exactly the same diagnosis. However, exactly what role genetics plays in the development of such a disorder still remains unclear.
Diagnostics
Ultrasound
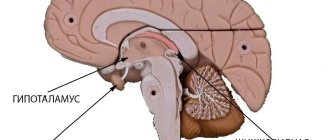
On antenatal ultrasound examination, pathologies may be detected as one or more intracranial cysts that interact with the ventricular system and/or subarachnoid space. Asymmetrical ventricles with a displaced midventricular echo may also be present.
CT
Porencephalic cysts appear as an intracranial cyst that has a well-defined border and central attenuation. There is usually no mass effect on adjacent parenchyma, although sometimes enlarging cysts lead to local mass effect. There is no improvement with contrast and without the solid component.
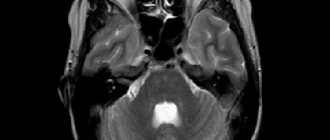
MRI
As with CT, the cyst appears well defined and often corresponds to vascular territory. The cyst is lined with white matter, which may or may not indicate gliosis (depending on the age at which the disorder occurred). It is important to note that the cyst is not covered by gray matter to distinguish them from arachnoid cysts and schizencephaly. Typically the cyst is visible for communication with the ventricles and/or subarachnoid space.
The cyst content follows the CSF signal in all sequences:
T1: low signal intensity
T2: high signal intensity
FLAIR: Signal Intensity Reduction
DWI: no restricted diffusion
Types of pathology
The manifestations and prognosis of cerebral schizencephaly largely depend on the degree of defect in the cerebral cortex. Neurologists distinguish two types of anomalies:
- Closed cleft. The walls of the gap are connected to each other by epithelium. The communication between the ventricles and the meninges is not disrupted, and there is no cerebrospinal fluid in the cleft. This type of pathology cannot be detected during prenatal diagnosis.
- Open (open) cleft. The walls of the defect do not communicate with each other. The anomaly appears as a deep groove in the cortex. It passes from the ventricles of the brain to its membranes. The cavity of the gap is filled with cerebrospinal fluid, which often causes hydrocephalus. With this form of brain schizencephaly, MRI shows ventricular hypertrophy.
On the subject: Cosmetic suture after cesarean section: what it looks like, how to treat it, how long it takes to heal
In approximately half of the cases, a closed cleft is diagnosed. In a third of patients, the pathology is complicated by hydrocephalus.
Clefts can occur on one or both sides. Bilateral defects are usually accompanied by more severe symptoms and have a less favorable prognosis.
General symptoms
Typically, the first signs of the disease appear in children 4 to 5 years old. But sometimes manifestations of pathology are noticeable in infants at 3–4 weeks. Symptoms depend on the type of defect. But we can also identify general signs of an anomaly:
- frequent seizures;
- hydrocephalus (fluid accumulation in the brain);
- microcephaly (small head size);
- low muscle tone.
In almost all patients, schizencephaly of the brain leads to deterioration of vision, hearing and smell. The severity of the disorders depends on the degree of the brain defect. In 100% of cases, the disease is accompanied by motor dysfunction. Patients have impaired coordination of movement, and muscle paralysis often occurs.
This is how schizencephaly manifests itself in children. As for adults, they may continue to have movement disorders and seizures. The severity of symptoms in adulthood largely depends on the location of the cleft.
Therapy methods
Treatment of cerebral schizencephaly can only be symptomatic. This defect cannot be corrected surgically.
For epileptic seizures, anticonvulsant medications are prescribed:
- "Finlepsin".
- "Depakine."
- "Convulex".
In mild cases, taking antiepileptic drugs leads to complete disappearance of seizures.
In more severe forms of the pathology, the administration of drugs based on botulinum toxin helps stop seizures. They slow down the transmission of signals from nerves to muscles and reduce the frequency of attacks.
If the patient has cognitive impairment, then sessions of electrical stimulation of the brain are prescribed. The procedures help increase the activity of the cerebral cortex.
For hydrocephalus, diuretics are indicated:
- "Veroshpirona".
- "Diakarba".
- "Furosemide".
However, diuretics help only temporarily reduce cerebral pressure and alleviate the patient’s condition. A more radical and effective treatment method is bypass surgery. A special tube is inserted into the brain. Through it, the cerebrospinal fluid flows to another part of the body, where it is absorbed.
On topic: 8 dental care mistakes you make most often
Be sure to prescribe therapeutic exercises to improve coordination and increase muscle tone. Exercises also help restore movement in case of paralysis and paresis. Sick children need developmental classes with a speech therapist. An occupational therapist may need to help teach the child self-care skills.
Pathomorphology of the anomaly
In the process of filling the cavities with cystic fluid, the brain matter is displaced, which often causes secondary damage to brain tissue. There is also a violation of the orientation of the cell layer.
With this disease, the total mass of the brain decreases by 20-25%, insufficient development of the frontal lobes and cerebral hemispheres is detected, nerve cells are not differentiated and are practically absent on the surface of its cortex.
There is insufficient development of the vascular system, and the process of maturation of the sheath of nerve fibers is also disrupted.
In young children, epilepsy attacks occur, asymmetry of the skull is observed, in which the affected side bulges somewhat in the temporal region, a significant lag in mental development, disorders of nerve cells in the cranial region, and paralysis of the limbs is also observed.
Often a violation of the development of the corpus callosum, microcephaly, as well as other defects in the development of organs are detected.
Autosomal dominant porencephaly type I. Similar disorders
- Disorders associated with mutations in the COL4A1 gene are a group of rare disorders characterized by damage to small blood vessels, including those in the brain. The age at onset of these disorders, disease progression, specific symptoms/manifestations and their severity vary significantly from one person to another.
- Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy is a rare genetic disorder. It is characterized by damage to small and medium-sized blood vessels, especially in the brain. CADASIL potentially causes a wide range of symptoms and manifestations, including migraines, strokes, cognitive impairment, speech problems, vision problems and changes in personality and behavior. CADASIL eventually progresses to dementia. Individuals with this disorder are at higher risk of developing a heart attack.
- Sporadic porencephaly is a rare disorder affecting the central nervous system. This disorder is characterized by the development of the same cysts or cavities.
Treatment
The treatment prescribed by specialists will depend on many factors, such as the degree of damage to brain tissue, the area in which the cystic cavity is located, and its size.
Often in patients the disease manifests itself in a weak form for the nervous system - therefore the symptoms do not affect mental development.
If there is a weak form, specialists prescribe medication therapy, for example, the drug encephabol, physiotherapy, and can also be treated with orthopedic exercises.
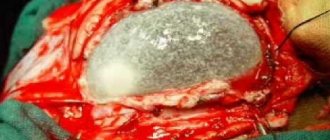
If the patient’s condition worsens, epileptic seizures become more frequent, or other consequences of the disease progress appear, a surgical operation is required. The purpose of the operation is the dissection of porencephalic cystic cavities and excision of defective brain tissue, dotted with vascular connections and located deep in the porencephaly. However, with a large area of damage, the prognosis of the disease is unfavorable, including the death of the patient.
Congenital porencephaly also has a low chance of a good prognosis for life after the disease. In the presence of small cystic cavities, patients experience developmental delay, in addition to epilepsy and paresis of the arms and legs. In the case of a false form of the disease, when the disease occurs as a result of infectious, inflammatory processes or trauma, until porencephaly progresses, the newborn or older child develops normally.
If treatment does not produce a positive effect after surgery, then in the postoperative period the ventricles are drained through the application of a ventriculoatreal or ventriculoperitoneal shunt.
Etiology of the disorder
This disease can be a consequence of brain injury, early microsis of brain tissue, or an intrauterine disorder of the development of the nervous system.
Such defects in brain development as cystic cavities are most often an intrauterine pathology, and are not only a consequence of impaired uterine circulation, but also a defect in the process of morphogenesis.
Sometimes cystic formations can appear at any age and are a consequence of brain injury, hemorrhage, infectious and inflammatory processes, various types of tumors that have a destructive effect on the white and gray matter of the brain.
Signs of bilateral schizencephaly
This form of pathology is much more severe. In patients, the connection between the brain and spinal cord is disrupted. As a result, severe motor impairment and bilateral paralysis are observed. Many patients cannot move independently.
On the subject: What not to eat if you have a diseased liver: contraindications and dietary recommendations, list of healthy foods, menu
In addition, children with bilateral schizencephaly of the brain experience severe mental retardation. They have great difficulty studying in a regular school. It is very difficult for them to master new knowledge and subjects.
Cognitive impairment and paralysis may persist into adults. Adaptation and rehabilitation of such patients is extremely difficult. They often need outside help.
The severity of symptoms in this case does not depend on the size of the cleft. Even small bilateral gaps in the hemispheres can significantly worsen the patient’s quality of life.
Unilateral cleft: symptoms
If the defect affects only one side of the cerebral hemispheres, then the pathology proceeds more favorably. During childhood, patients experience the following symptoms:
- unilateral paralysis and paresis;
- impaired coordination of movements (on one side of the body);
- apathy;
- retardation in mental and physical development;
- difficulties with speech perception.
In adulthood, the mental and physical development of patients is normalized. Most mature people with closed unilateral schizencephaly of the brain have average intelligence and adapt well to life in society. However, they may continue to have movement disorders and high intracranial pressure, especially if they did not receive the necessary treatment in childhood.