Mechanism of occurrence
Peripheral paralysis occurs when the peripheral motor neuron is damaged at any level - from the anterior horn of the spinal cord and the motor nuclei of the cranial nerves to the axon terminals. Since no efferent impulse can reach the muscle without passing the peripheral motor neuron, peripheral paralysis is characterized by loss of all movements - voluntary and involuntary. The muscle is deprived of both impulse and non-impulse (trophic) influence from the peripheral motor neuron.
Treatment
Symptoms of spastic lower paresis can only be treated comprehensively. In therapy, thermal procedures should be used along with massage. This helps to normalize the conduction of active impulses to the muscles, and also improves their trophism. When the patient can actively move his leg, massage should be combined with exercise therapy and the use of a load, which should be gradually increased. In this case, all exercises must be strictly dosed, and massage should be performed only by a professional.
In addition, treatment includes activities such as:
- Taking medications.
- Use of orthoses.
- Drug blockades.
- Surgical intervention.
The choice of treatment method is strictly individual and depends on the location and degree of spastic paralysis.
Signs of peripheral paralysis (symptoms)
The occurrence of peripheral paralysis leads to the impossibility of muscle tone (muscle atony), reflexes (areflexia) and to disruption of trophic processes (degenerative muscle atrophy). Regressive biochemical, structural and physical processes occur in the muscles, as a result of which their function is disrupted. Thus, when irritated by electric current, the muscle responds with a slow worm-like contraction, like smooth muscle. The damaged peripheral motor cell shows signs of increased excitability, which leads to sporadic contractions of the motor units, which are called fascicular twitches. They are very characteristic of such peripheral motor neuron diseases as amyotrophic lateral sclerosis, cervical myelopathy, and syringomyelia.
Denervated muscles also become hypersensitive (denervation hypersensitivity), which is manifested by spontaneous contractions of individual muscle fibers, sometimes difficult to detect visually. However, fasciculations and fibrillations are well identified using EMG.
Diagnostics
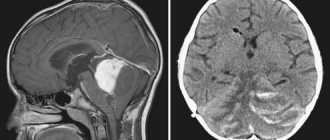
A neurologist diagnoses and treats spastic paralysis. At the appointment, the doctor examines the patient and conducts special tests (assessing motor functions, muscle tone, reflexes). But since symptoms characteristic of SP also occur with other diseases (brain tumors, muscular dystrophy, etc.), to clarify the diagnosis, an additional examination is prescribed, including:
- laboratory blood tests (CBC, biochemical analysis);
- X-ray examination of the skull;
- CT scan of the head and spine;
- MRI;
- neurosonography.
Damage levels
Spinal cord lesion
In the anterior horns of the spinal cord along the vertical spinal axis there are motor neurons that innervate different regions. From the level CI-CIV and partially CV, the muscles of the neck and the diaphragmatic muscle (CIV), CV-CVIII (there are 8 spinal segments in the cervical spinal cord) and partially thoracic ThI - the belt of the upper limbs and themselves, ThI-ThXII - the muscles of the trunk are innervated , lumbar LI-LV, partially ThXII and sacral SI-II - the girdle of the lower extremities and the lower extremities themselves, SIII-IV - the sphincters of the bladder and anus. According to the level of damage to the segments of the spinal cord or the peripheral structures emanating from them, peripheral paralysis will be noted. In a clinical setting, the doctor has to solve the opposite problem, namely: by the localization of peripheral paralysis, determine the topic of damage to the nervous system.
Lesions of the spinal cord are usually characterized by bilaterality: upper or lower paraplegia, tetraplegia (paresis).
Cranial nerve damage
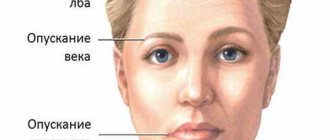
When the motor structures of the cranial nerves are damaged at any level - from the nucleus to the terminal and axon - peripheral paralysis occurs in the muscles of the tongue, pharynx, larynx and soft palate (caudal group of cranial nerves, bulbar syndrome), masticatory muscles (trigeminal nerve), facial muscles (facial ) and external muscles of the eye (oculomotor group of cranial nerves).
Central (spastic) paralysis
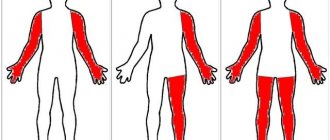
Central paralysis occurs as a result of damage to the central motor neuron in any part of it. Since the arrangement of cells and fibers of the pyramidal bundles is quite close, central paralysis is usually diffuse, spreading to an entire limb or half of the body.
Peripheral paralysis may be limited to damage to certain muscle groups or even individual muscles. There may, however, be exceptions to this rule. Thus, a small lesion in the cerebral cortex can cause the occurrence of isolated central paralysis of the foot, face, etc.; conversely, multiple diffuse lesions of the nerves or anterior horns of the spinal cord sometimes cause widespread paralysis of the peripheral type.
As mentioned above, the symptomatology of central paralysis differs sharply from that of peripheral paralysis: pronounced muscle atrophy is not characteristic here and there is no degeneration reaction, neither muscle atony nor loss of reflexes is observed.
Minor diffuse muscle atrophy can sometimes be observed with central paralysis, but it never reaches such a significant degree as with peripheral paralysis, and is not accompanied by the degeneration reaction typical of the latter. This atrophy may result from lack of muscle activity, but sometimes it develops early after the lesion; in this case, it can be explained as a trophic disorder resulting from damage to the cortex (according to some data, more often than the parietal lobe). In cases of acute central paralysis (trauma, hemorrhage), muscle hypotonia and loss of reflexes are initially possible. At I.P. Pavlov we find an indication that with thrombosis and hemorrhages in the cerebral hemispheres, accompanied by paralysis, and not “catalepsy” (i.e., not hypertension. - Author),
There is even an absence of spinal reflexes.
“It is clear that the retarding (inhibitory) effect of the destruction that has occurred has descended even on the spinal cord...” This phase is usually short-lived and in most cases is soon replaced by a typical picture of central paralysis (with muscle hypertonia and increased reflexes).
The absence of disorders characteristic of flaccid paralysis is understandable, since the peripheral motor neuron (and segmental reflex arc) remains intact in central paralysis; therefore, there are no symptoms depending on its defeat. The segmental apparatus of the spinal cord that remains intact not only retains its reflex activity, but also increases it, freed during central paralysis (damage to the pyramidal system) from the inhibitory (subordinate) influences of the cerebral cortex.
The main features of central paralysis are muscle hypertonia, increased tendon reflexes, so-called accompanying movements, or synkinesis, and pathological reflexes.
Hypertension,
or
spasticity of the muscles, determines another name for central paralysis - spastic.
The muscles are tense, dense to the touch; During passive movements, a clear resistance is felt, which is sometimes difficult to overcome. This spasticity is the result of increased reflex tone and is usually unevenly distributed, leading to typical contractures. With central paralysis, the upper limb is usually brought to the body and bent at the elbow joint: the hand and fingers are also in a flexed position. The lower limb is extended at the hip and knee joints, the foot is bent and the sole is turned inward (the leg is straightened and “elongated”). This position of the limbs with central hemiplegia creates a unique Wernicke-Mann position, the interpretation of the patterns of its occurrence from the point of view of the history of the development of the nervous system was given by M.I. Astvatsaturov. The gait in these cases is of a “circumducing” nature: due to the “lengthening” of the leg, the patient has to “circle” the affected leg (in order not to touch the floor with the toe).
Increased tendon reflexes
(hyperreflexia)
is also a manifestation of increased, disinhibited, automatic activity of the spinal cord.
Reflexes from the tendons and periosteum are extremely intense and are easily evoked as a result of even minor irritations: the reflexogenic zone expands significantly, i.e. the reflex can be evoked not only from the optimal area, but also from neighboring areas. An extreme degree of increase in reflexes leads to the appearance of clonus (see above). In contrast to tendon reflexes, skin reflexes (abdominal, plantar, cremasteric) do not increase with central paralysis, but disappear or decrease.
Associated movements
or
synkinesis
observed with central paralysis may occur in the affected limbs reflexively, in particular when healthy muscles are tense. Their occurrence is based on the tendency to irradiate excitation in the spinal cord to a number of neighboring segments of its own and opposite sides, which is normally moderated and limited by cortical influences. When the segmental apparatus is disinhibited, this tendency to spread excitation is revealed with particular force and causes the appearance of “additional” reflex contractions in the paralyzed muscles.
There are a number of synkinesis characteristic of central paralysis. Here are some of them:
1) if the patient, according to the instructions, resists with his healthy hand the extension in the elbow joint produced by the examiner, or strongly shakes his hand with his healthy hand, then a concomitant reflex flexion occurs in the paralyzed arm;
2) the same flexion of the affected arm occurs when coughing, sneezing, or yawning;
3) under the mentioned conditions, involuntary extension is observed in the paralyzed leg (if the patient sits with his legs hanging over the edge of the couch or table);
4) The patient lying on his back with his legs extended is asked to adduct and abduct his healthy leg, in which he is resisted. In this case, an involuntary corresponding adduction or abduction is observed in the paralyzed leg;
5) the most constant of the accompanying movements with central paralysis is the symptom of combined flexion of the hip and trunk.
When
the patient tries to move from a horizontal position to a sitting position (the patient lies on his back with his arms crossed on his chest and straightened legs apart), the paralyzed or paretic leg is raised (sometimes adducted).
Pathological reflexes
These
are a group of very important and persistent symptoms of central paralysis.
Of particular importance are pathological reflexes on the foot, which are observed, of course, in cases where the lower limb is affected. The most sensitive symptoms are Babinski (perverted plantar reflex), Rossolimo and Bekhterev. The remaining pathological reflexes on the foot (see above) are less constant. Pathological reflexes in the hands are usually weakly expressed and have not acquired much significance in the practice of clinical research. Pathological reflexes on the face (mainly a group of “oral” reflexes) are characteristic of central paralysis or paresis of muscles innervated by cranial nerves, and indicate bilateral supranuclear lesions of the tractus cortico-bulbaris in the cortical, subcortical or brainstem regions. Symptoms such as increased tendon reflexes of the limbs, weakened abdominal reflexes and Babinski's symptom are very subtle and early signs of a violation of the integrity of the pyramidal system and can be observed when the lesion is not yet sufficient to cause paralysis or even paresis. Therefore, their diagnostic value is very great. E.L. Venderovich described a symptom of “ulnar motor defect”, indicating a very mild degree of pyramidal lesion: on the affected side, the patient’s resistance to forced abduction of the little finger as far as possible towards the fourth finger is weaker.
The table is given. 1 (according to M.I. Astvatsaturov) symptoms of peripheral and central paralysis.
The methodology for studying movements consists of
- studying the general appearance, facial expressions, speech, posture and gait of the patient,
- determining the volume and strength of active movements,
- studies of passive movements and muscle tone,
- motor coordination studies
- checking the electrical excitability of nerves and muscles.
Already one external inspection
the patient can give a lot of significant information and direct the investigator’s attention to one or another defect in the state of muscles and motor function.
Table 1
| Type of paralysis | Central or spastic | Peripheral, flaccid, or atrophic |
| Localization of lesions | Motor projection area of the cortex or pyramidal fasciculi | Anterior horns of the spinal cord, anterior roots and motor fibers of peripheral nerves |
| Spread of paralysis | More often diffuse | Mostly limited |
| Muscle tone | Hypertension, spasticity | Hypotension, lethargy |
| Reflexes | Tendons are increased, abdominal and plantar tendons are lost or decreased | Tendon and skin are lost or reduced |
| Pathological reflexes | Babinsky's symptom, etc. | None |
| Related movements | Available | » |
| Amyotrophy | Absent | Available |
| Reaction of rebirth | » | » |
Thus, muscle atrophy and limb contractures can be immediately detected. Sometimes the patient’s posture, low or, conversely, excessive mobility attracts attention. In a conversation with a patient, paresis of facial muscles, speech disorders, and phonation disorders may be noticed. Trembling, convulsive twitching, etc. are noticeable. Be sure to examine the patient's gait, which may be disordered. In particular, with hemiparesis of the central type, the gait, Wernicke-Mann posture, as mentioned above. With spastic lower paraparesis, a “spastic” or “spastic-paretic” gait is observed, when the patient walks with straightened legs, without lifting the soles from the floor; When you move your legs, the tension in them is noticeable. With flaccid paraparesis, the feet usually hang down, and the patient, in order not to touch the floor with his toe, is forced to raise his leg high (the so-called “cock” or peroneal gait).
Active movements
are examined in order from top to bottom; usually the volume of only some basic movements is determined.
On the face, we examine the wrinkling of the forehead upward, the closing of the eyelids, the movements of the eyeballs, the opening of the mouth and the pulling of the corners of the mouth outward, and the protrusion of the tongue.
The volume of head rotation to the sides is determined. The subject is asked to make a shoulder-raising movement (“shrug”). The arms are raised to the horizontal and higher; flexion and extension in the elbow, wrist and finger joints; pronation and supination of the hands; bringing and spreading fingers; To determine a mild degree of paresis and disorder of fine movements, it is advisable to ask the subject to make quick flexion and extension movements with his fingers, moving them in the air with his arms extended forward.
This is followed by flexion and extension of the body, tilting to the right and left.
Flexion and extension are performed in the joints of the hip, knee, ankle, and toes, walking on the heels and on the toes.
In necessary cases, it is necessary to check more subtle and isolated movements relating to individual muscles during the study.
The presence of a full range of active movements does not always exclude the possibility of mild paresis, which in such cases may be limited by a weakening of muscle strength. Therefore, the study of the range of active movements of the limbs is usually accompanied by a simultaneous study of muscle strength, for which the subject provides a certain counteraction to the movement being performed. The grip force of the hand is determined, which can be measured with a dynamometer.
Passive movements
It is clear that they will not be limited if there is a full range of active movements. Their study is necessary when establishing the absence or limitation of active movements in a particular muscle group. It may turn out that movements are limited not because of paresis, but because of damage to the joints, due to pain, etc. The study of passive movements is also carried out to determine muscle tone.
Tone
determined primarily by palpation of the muscle at rest. With atony or hypotension, the muscles feel flabby and sluggish; with hypertension - dense, tense. With passive movements in the case of atony, excursions in the joints are completely free, even excessive; joints are “loose.” As tone increases, passive movements encounter significant resistance, to overcome which a certain amount of tension is necessary. With spasticity of the muscles that accompanies central paralysis, a phenomenon is observed that is called the “jackknife symptom”: if we make a fast passive movement, then the resistance provided by the rigid muscles is not the same throughout the entire movement; it is especially felt at the beginning and decreases later.
Coordination of movements
is disrupted as a result of damage to the cerebellar system and the loss of the “sense of position and movement” (articular-muscular sense).
A. V. Triumfov,
“Topical diagnosis of diseases of the nervous system”
All articles Addresses and telephone numbers of clinics
Consequences of paralysis
Breathing disorders
Patients with signs of damage to the spinal cord and other parts of the nervous system often experience breathing disorders. They can be caused by: Material from the site https://wiki-med.com
- decompensation of previous pulmonary and cardiac pathology (chronic obstructive processes in the lungs, etc.);
- secondary respiratory disorders due to bulbar lesions and impaired pharyngeal reflex, retraction of the tongue, flow of saliva, mucus and food entering the upper respiratory tract with the development of atelectasis and pneumonia;
- somatic complications in the form of hypostatic pneumonia on the side of hemiplegia;
- central respiratory disorders with damage to the medulla oblongata (tachypnea, periodic types of respiratory distress, apnea);
- damage to the fibers of the corticonuclear pathway ending on the peripheral motor neurons of the respiratory muscles (diaphragm, intercostal muscles), with loss of voluntary control of breathing and the risk of sudden death during sleep;
- damage to peripheral motor neurons at the level of the IV and thoracic spinal cord.
Categories: Symptoms in alphabetical order Symptoms of diseases of the nervous system
On this page there is material on the following topics:
peripheral paresis motor system
paralysis of the distal upper limb Dejerine-Klumpke
typical for peripheral paralysis
impairment in flaccid peripheral paralysis
Left-sided and right-sided hemiparesis: causes, types, degrees
Hemiparesis is not a specific disease, but a syndrome, that is, a clinical sign. Its etiology is varied, as are its symptoms, which depend on the level of damage to nerve fibers. In the region of the medulla oblongata, these fibers intersect, therefore, with lesions of the right hemisphere, left-sided hemiparesis develops, and with lesions of the left, right hemiparesis develops.
Causes of hemiparesis
Right-sided and left-sided hemiparesis in children is possible for a number of reasons associated with the prenatal period:
- incorrect position of the fetus, in which nerve fibers are pinched, most often at the level of the lumbosacral region;
- fetal hypoxia;
- penetration of neurogenic pathogens through the placenta;
- traumatic birth;
- asphyxia at birth;
- congenital anomalies of the brain or brain;
- meningoencephalitis;
- cerebral palsy (CP);
- injuries;
- congenital aneurysm of the arteries of the brain and other diseases.
In adults, the etiology is slightly different, more related to acquired diseases:
- neurogenic infections;
- strokes, thrombosis of the head vessels;
- epilepsy;
- tumors and traumatic damage to the brain and brain tissue.
Classification and types of hemiparesis
According to the level of damage to the central nervous system, hemiparesis is:
- central (cortical nuclei or motor roots are affected, which start from the nuclei and connect to the anterior horns of the SC);
- peripheral (damage at the level of motor neurons of the anterior horns of the SC or peripheral nerves;
- mixed (both central and peripheral lesions);
- psychogenic (hemiparesis occurs due to mental illness).
Degrees of paralysis
The degree of paresis is determined on two scales that are inverse to each other:
- on a five-point scale (from complete paralysis to normal);
- according to four degrees of severity (from the mildest to paralysis).
Five-point scale:
- 0 - complete absence of voluntary movements;
- 1 - muscle contractions are slightly noticeable, but there is no movement in the joints;
- 2 - significant decrease in motor amplitude, passive movements are possible, it is impossible to hold the limb suspended or tear it off the floor;
- 3 - with significant motor restrictions, active movements overcoming natural resistance forces become possible;
- 4 - movements are available in full, but slight weakness is observed in the muscles;
- 5 – muscle volume and strength are completely preserved.
Degrees of severity: mild (1), moderate (2), deep (3), paralysis (4).
Symptoms and manifestations
Symptoms of central paralysis:
- Muscular hypertension is pathological muscle tension. They have increased resistance to movement.
- Expansion of the zone of distribution of reflexes - manifested in involuntary movements of individual parts of the body.
- Synkinesis - involuntary movements against the background of active actions. Manifests itself in swinging arms when walking.
These disturbances appear when you want to take a certain pose or perform body movements. People with spastic paralysis tend to be in an unnatural position and experience convulsive twitching of a muscle group.
Gait is difficult due to the inward bending of the feet. You may notice involuntary twitching of the shoulders, arms and facial muscles. Speech disturbances, eyelid twitching, or facial muscle disturbances are observed.
These symptoms will help not only to distinguish SP from PP, but also to identify areas of damage to the nervous system.
Features of the violation
In a healthy person, when the skin comes into contact with irritants, impulses are transmitted through the spinal cord to the brain using nerve fibers.
With spastic paralysis, the muscles are in constant tone. Tendon reflexes do not occur. The pain impulse does not reach the brain, creating muscle spasms and uncontrolled movements. With spastic paralysis, the patient cannot take certain positions. Paralysis of the facial muscles causes mental suffering.
A temporary decrease in tone is possible through warming up, special massage and physical therapy.
Impulses that increase tone are internal and external in nature. Over time, the patient will learn to independently determine their character. Thus, for people with spastic paralysis, the only way to feel pain and discomfort is through the degree of spasticity.
People with moderate levels of spasticity may be able to walk at slow paces or transfer from one place to another.
Since central paralysis is a consequence of damage to a specific focus of the neurological system, it may not be the only manifestation of this condition.
Characteristic consequences are impaired coordination of movement and difficulty in eating. Difficulty in the respiratory system and digestive problems may also occur.
Tactile sensitivity may become worse or, conversely, dull. Possible vision impairment. Caring for such patients requires careful handling. Changing your body posture can be quite difficult.
DIF diagnostics
When diagnosing central paralysis in adults, the differentiated diagnosis method (DIF) is used. It is carried out by excluding diseases that are not related to a specific case. Ultimately, DIF remains the only disease that causes spastic paralysis.
This diagnosis consists of three stages:
- at the first stage, all diseases suffered by the patient are clarified;
- the second stage includes examination of the patient and clarification of symptoms;
- at the third stage, all laboratory and computer tests are studied, on their basis the doctor must make a conclusion and announce the diagnosis.
When conducting a study, the doctor can rely on his experience or use special computer programs. The latest software applications allow you to most accurately identify the entire picture of the disease and make a diagnosis in the shortest possible time.
Impairment in children is determined by tracking the development of various abilities. The most common signs of paralysis are:
- inability to keep food in the mouth;
- when trying to make a voluntary movement, trembling of the limbs is observed;
- the legs are constantly in a tightly compressed state;
- has poor use of hands or only one hand is active.
Also, a test for spastic paralysis is included in the examination procedure for newborns up to 6 months.