What is cerebral palsy?
Cerebral palsy (CP) is a separate disease and a spectrum of movement disorders that arise due to brain damage in the perinatal period.
The group of disorders that are united by the term cerebral palsy usually includes:
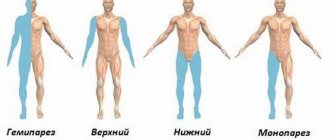
- mono-, hemi-, para-, tetra-paralysis and paresis,
- pathological changes in muscle tone,
- hyperkinesis,
- speech disorders,
- unsteadiness of gait,
- movement coordination disorders,
- frequent falls,
- child's lag in motor and mental development.
Separately, all of these conditions may indicate other neurological or mental problems. That is why it is so important that a doctor gives a conclusion about the presence or absence of cerebral palsy. The material is for informational purposes only.
Differential diagnosis
| Nosology | Onset of the disease | Characteristic symptoms | Biochemical blood tests, instrumental data, diagnostic criteria |
| Congenital myopathy | From birth | Diffuse muscle hypotonia, hyporeflexia. Myopathic symptom complex, delayed motor development, osteoarticular deformities | EMG – primary muscular nature of changes. Increased content of CPK |
| Leukodystrophy | No disturbances during the neonatal period | Movement disorders, muscle hypo-, then hypertension, ataxia. Progressive course, convulsions, spastic paralysis, paresis, increasing decline in intelligence, hyperkinesis | CT scan of the brain: extensive bilateral foci of low density |
| Mucopolysaccharidoses | Absence of disturbances in the neonatal period | The characteristic appearance of the patient: grotesque facial features, depressed bridge of the nose, thick lips, short stature. Delayed development of neuropsychic static functions, speech underdevelopment | Presence of acidic mucopolysaccharides in urine |
| Spinal muscular amyotrophy Werdnig-Hoffmann | From birth or from 5-6 months of age | Generalized hypotonia, hypoareflexia, fasciculations in the muscles of the back and proximal limbs. | Progressive course. EMG from limb muscles – denervation type |
| Congenital hypothyroidism | The first symptoms may appear already in the maternity hospital (attacks of respiratory arrest, jaundice), but more often develop in the first months of life | The specific appearance of the patient: small stature, short limbs, wide hands and feet, sunken bridge of the nose, swollen eyelids, large tongue, dry skin, brittle hair. Delayed psychomotor development, diffuse muscle hypotonia. As a rule, constipation and bradycardia are observed. A very characteristic yellowish-sallow skin color | Aplasia or insufficiency of thyroid function. Delay in the appearance of ossification nuclei |
| Ataxia-telangiectasia Louis-Bar | No disturbances during the neonatal period. Onset of disease 1-2 years | Ataxia, hyperkinesis, decreased intelligence, telangiectasias, pigment spots, often lung pathology | Atrophy of the vermis and cerebellar hemispheres, high levels of serum α-phenoprotein |
| Phenylketouria | Children are born healthy, the disease manifests itself from 3-6 months of age: suspension in psycho-speech and motor development | The disease manifests itself from 3-6 months of age with lightening of the hair, iris, musty specific odor of urine and sweat, cessation or slowdown of motor and mental development; convulsions appear - up to 1 year of age, infantile spasms are more common, later they are replaced by tonic-clonic seizures | Increased phenylalanine in the blood, positive Fehling test |
| Rett syndrome | Up to 1 year of age, psycho-speech development corresponds to age, then there is a gradual loss of previously acquired skills. In the ante- and perinatal period of development, as well as in the first half of life, the development of children is often regarded as normal | The age at which deviations in the development of children are first noted ranges from 4 months to 2.5 years; most often from 6 months to 1.5 years. The first signs of the disease include a slowdown in the child’s psychomotor development and head growth rate, loss of interest in games, and diffuse muscle hypotonia. An important symptom is loss of contact with others, which is often misinterpreted as autism. The diagnosis is considered preliminary until the age of two or five years. | Diagnostic criteria for Rett syndrome (from Trevathan et al., 1998) include the necessary criteria, which include a normal prenatal and perinatal period, normal head circumference at birth followed by slowing of head growth between 5 months and 4 years; loss of acquired goal-directed hand movements between the ages of 6 and 30 months, associated in time with impaired communication; profound damage to expressive and impressive speech and severe delay in psychomotor development; stereotypical hand movements resembling squeezing, squeezing, clapping, “hand washing,” rubbing, appearing after the loss of purposeful hand movements; gait disturbances (apraxia and ataxia) that appear between the ages of 1 and 4 years |
Medical tourism
Get treatment in Korea, Israel, Germany, USA
Get advice on medical tourism ×
Treatment abroad
Application for medical tourism
Select the area of medicine you are interested inObstetrics and gynecologyAllergologyPediatric allergologyAngiosurgeryCongenital diseasesGastroenterologyPediatric gastroenterologyHematologyPediatric hematologyDermatovenereologyDermatocosmetologyPediatric dermatologyImmunologyInfectious diseases in childrenInfectious and parasitic diseasesCardiologyPediatric cardiologyCardiosurgery urgyChildren's cardiac surgeryCombustiologyChildren's CombustiologyMammologyMedical rehabilitationNarcologyNeurologyNeurology for childrenNeurosurgeryNeonatologyEmergency medicineNephrologyNephrology for childrenOncohematologyOncohematology for childrenOncologyOncology for childrenOrphan diseases OtorhinolaryngologyOtorhinolaryngology for childrenOphthalmology mologyOphthalmology for childrenPalliative carePediatricsProctologyOccupational pathologyPsychiatryPulmonologyPulmonology for childrenRadiologyRheumatologyRheumatology for childrenDentistologyDentistry for childrenAudiologyToxicologyThoracic surgeryTraumatology and orthopedicsTraumatology and orthopedics for childrenTransplantologyTransplantology for childrenUrology Pediatric UrologyPhthisiologySurgeryPediatric SurgeryNeonatal SurgeryMaxillofacial SurgeryEndocrinologyPediatric EndocrinologyNuclear Medicine
What is the best way to contact you?
Enter your phone number or email addressSubmit an application for medical tourism Medical tourism textarea>
Get treatment in Korea, Turkey, Israel, Germany and other countries
Examination for cerebral palsy
With cerebral palsy, intellectual impairments, mental disorders, epilepsy, hearing and vision impairments can be observed; diagnostics will help clarify. The diagnosis of cerebral palsy is made based on clinical data and examination results. The examination algorithm for a child with cerebral palsy is aimed at identifying additional health problems and excluding other congenital pathologies. The range of studies is recommended by the doctor; they are individual in nature.
Paraplegia and tetraplegia
ICD-10 → G00-G99 → G80-G83 → last changes: January 2006G82.0G82.1G82.2G82.3G82.4G82.5
hide | to uncover
- Some infectious and parasitic diseasesA00-B99
- Diseases of the blood, hematopoietic organs and certain disorders involving the immune mechanism D50-D89
- Diseases of the endocrine system, nutritional disorders and metabolic disorders E00-E90
- Mental and behavioral disorders F00-F99
- Diseases of the nervous systemG00-G99
- Diseases of the eye and its adnexaH00-H59
- Diseases of the ear and mastoid processH60-H95
- Diseases of the circulatory systemI00-I99
- Respiratory diseasesJ00-J99
- Diseases of the digestive systemK00-K93
- Diseases of the skin and subcutaneous tissue L00-L99
- Diseases of the musculoskeletal system and connective tissueM00-M99
- Diseases of the genitourinary systemN00-N99
- Pregnancy, childbirth and the postpartum period O00-O99
- Selected conditions arising in the perinatal period P00-P96
- Congenital anomalies [malformations], deformations and chromosomal disordersQ00-Q99
- Symptoms, signs and abnormalities identified during clinical and laboratory tests, not classified elsewhere R00-R99
- Symptoms and signs related to the circulatory and respiratory systems R00-R09
- Symptoms and signs related to the digestive system and abdominal cavityR10-R19
- Symptoms and signs relating to the skin and subcutaneous tissue R20-R23
- Symptoms and signs related to the nervous and musculoskeletal systems R25-R29
- Symptoms and signs related to the urinary system R30-R39
- Symptoms and signs related to cognition, perception, affect and behavior R40-R46
- Symptoms and signs related to speech and voice R47-R49
- General symptoms and signs R50-R69
- Deviations from the norm identified during blood testing, in the absence of an established diagnosis R70-R79
- Deviations from the norm identified during urine examination, in the absence of an established diagnosis R80-R82
- Deviations from the norm identified during the examination of other fluids, substances and tissues of the body, in the absence of an established diagnosis R83-R89
- Deviations from the norm identified when obtaining diagnostic images and conducting research, in the absence of an established diagnosis R90-R94
- Ill-defined and unknown causes of deathR95-R99
NeoplasmsC00-D48
hide all | reveal everything
xn—10-9cd8bl.com
Risk factors for the development of cerebral palsy
The causes of cerebral palsy are early damage to brain structures. During pregnancy or, as often happens, difficult childbirth, brain cells die for some reason. During pregnancy, the following can cause toxic damage:
- fetoplacental insufficiency,
- premature placental abruption,
- toxicosis (but not any, but very severe forms),
- nephropathy of pregnancy,
- infections (cytomegalovirus, rubella, toxoplasmosis, herpes, syphilis),
- Rhesus conflict,
- threat of miscarriage,
- somatic diseases of the mother (diabetes mellitus, hypothyroidism, congenital and acquired heart defects, arterial hypertension),
- injuries suffered by a woman during pregnancy.
During childbirth, other risk factors for developing cerebral palsy:
- breech presentation of the fetus,
- rapid birth,
- premature birth,
- narrow pelvis,
- large fruit,
- excessively strong labor activity,
- protracted labor,
- discoordinated labor activity,
- long anhydrous period before childbirth,
- birth injury.
In the postpartum period, such factors become:
- asphyxia,
- hemolytic disease of the newborn.
All these are only risk factors, and not mandatory conditions for the development of cerebral palsy.
Causes
Cerebral palsy is caused by a number of different factors that act at different periods of life - during pregnancy, childbirth, and early childhood. In most cases, cerebral palsy occurs after a brain injury received during birth due to asphyxia. However, extensive research in the 1980s showed that only 5-10% of cases of cerebral palsy are associated with birth trauma. Other possible causes include abnormalities of brain development, prenatal factors that directly or indirectly damage neurons in the developing brain, premature birth, and brain injuries that occur in the first few years of life. Prenatal reasons. Brain development is a very delicate process that can be influenced by many factors. External influences can lead to structural abnormalities of the brain, including the conduction system. These lesions can be hereditary, but most often the true causes are unknown. Maternal and fetal infections increase the risk of cerebral palsy. In this regard, rubella, cytomegalovirus (CMV) and toxoplasmosis are important. Most women are immune to all three infections by the time they reach childbearing age, and a woman's immune status can be determined by testing for TORCH infections (toxoplasmosis, rubella, cytomegalovirus, herpes) before or during pregnancy. Any substance that can affect fetal brain development, directly or indirectly, may increase the risk of developing cerebral palsy. In addition, any substance that increases the risk of preterm birth and low birth weight, such as alcohol, tobacco or cocaine, may indirectly increase the risk of cerebral palsy. Because the fetus receives all its nutrients and oxygen from the blood that circulates through the placenta, anything that interferes with the normal function of the placenta can negatively affect the development of the fetus, including its brain, or possibly increase the risk of premature birth. Structural abnormalities of the placenta, premature separation of the placenta from the uterine wall and placental infections pose a certain risk of cerebral palsy. Some diseases in the mother during pregnancy can pose a risk to the development of the fetus. Women with elevated antithyroid or anti-phospholipid antibodies are at increased risk for cerebral palsy in their children. Another important factor that indicates a high risk of this pathology is a high level of cytokines in the blood. Cytokines are proteins associated with inflammation in infectious or autoimmune diseases and can be toxic to fetal brain neurons. Perinatal reasons. Among perinatal causes, asphyxia, entanglement of the umbilical cord around the neck, placental abruption and placental previa are of particular importance. The infection in the mother is sometimes not transmitted to the fetus through the placenta, but is transmitted to the baby during childbirth. Herpetic infection can lead to severe pathology in newborns, which entails neurological damage. Postpartum causes. The remaining 15% of cerebral palsy cases are associated with neurological trauma after birth. Such forms of cerebral palsy are called acquired. Incompatibility of the Rh blood groups of mother and child (if the mother is Rh negative and the child is Rh positive) can lead to severe anemia in the child, which leads to severe jaundice. Serious infections that directly affect the brain, such as meningitis and encephalitis, can lead to permanent brain damage and cerebral palsy. Seizures at an early age can lead to cerebral palsy. Idiopathic cases are not diagnosed as often. As a result of harsh treatment of a child, traumatic brain injuries, drowning, suffocation, physical trauma occurs to the child, often leading to cerebral palsy. In addition, ingestion of toxic substances such as lead, mercury, other poisons, or certain chemicals can cause neurological damage. Accidental overdose of certain medications can also cause similar damage to the central nervous system.
Types of Cerebral Palsy
There are several types of cerebral palsy:
- spastic diplegia
- hemiparetic form
- hyperkinetic form
- double hemiplegia
- atonic-astatic form
- mixed forms.
Spastic diplegia is the most common form of cerebral palsy. This form of cerebral palsy is based on damage to the motor centers, which leads to the development of paresis, more pronounced in the legs. When the motor centers of only one hemisphere are damaged, a hemiparetic form of cerebral palsy occurs, which is manifested by paresis of the arm and leg on the side opposite to the affected hemisphere.
In approximately a quarter of cases, cerebral palsy has a hyperkinetic form associated with damage to subcortical structures. Clinically, this form of cerebral palsy is manifested by involuntary movements - hyperkinesis, which intensify when the child is excited or tired. With disorders in the cerebellum, an atonic-astatic form of cerebral palsy develops. This form of cerebral palsy is manifested by disturbances in statics and coordination, muscle atony. It accounts for about 10% of cases of cerebral palsy.
The most severe form of cerebral palsy is called double hemiplegia. In this variant, cerebral palsy is a consequence of total damage to both hemispheres of the brain, leading to muscle rigidity, due to which children cannot not only stand and sit, but even hold their head up on their own. There are also mixed variants of cerebral palsy, combining different forms.
Classification according to ICD-10
(If movement disorders in the hands are more severe, the clarifying term “bilateral hemiplegia” can be used)
G80.0 One of the most severe forms of cerebral palsy, resulting from abnormalities in brain development, intrauterine infections and perinatal hypoxia with diffuse damage to the cerebral hemispheres. In premature infants, the main cause of perinatal hypoxia is selective neuronal necrosis and periventricular leukomalacia; in full-term infants - selective or diffuse necrosis of neurons and parasagittal brain damage during intrauterine chronic hypoxia. Clinically diagnosed are spastic quadriplegia (quadriparesis; a more appropriate term[3] compared to tetraplegia, since noticeable impairments are detected approximately equally in all four limbs), pseudobulbar syndrome, visual impairment, cognitive and speech impairment. 50% of children experience epileptic seizures. This form is characterized by the early formation of contractures, deformations of the trunk and limbs. In almost half of the cases, movement disorders are accompanied by pathology of the cranial nerves: strabismus, atrophy of the optic nerves, hearing impairment, and pseudobulbar disorders. Quite often, microcephaly is noted in children, which, of course, is secondary. Severe motor defects of the hands and lack of motivation exclude self-care and simple work activities.
(“Tetraparesis with spasticity in the legs”, by Michaelis)
G80.1 The most common type of cerebral palsy (3/4 of all spastic forms), previously also known as “Little’s disease”. The function of the muscles on both sides is impaired, more so in the legs than in the arms and face. Spastic diplegia is characterized by the early formation of contractures, deformities of the spine and joints. It is mainly diagnosed in children born prematurely (consequences of intraventricular hemorrhages, periventricular leukomalacia, and other factors). In this case, in contrast to spastic quadriplegia, the posterior and, less often, middle sections of the white matter are more affected. With this form, tetraplegia (tetraparesis) is usually observed, with muscle spasticity noticeably predominant in the legs. The most common manifestations are delayed mental and speech development, the presence of elements of pseudobulbar syndrome, dysarthria, etc. Pathology of the cranial nerves is common: convergent strabismus, atrophy of the optic nerves, hearing impairment, speech impairment in the form of delayed development, moderate decline in intelligence, including those caused by the influence of the environment on the child (insults, segregation). The prognosis for motor abilities is less favorable than for hemiparesis. This form is the most favorable with regard to the possibilities of social adaptation. The degree of social adaptation can reach the level of healthy people with normal mental development and good hand function. G80.2 Characterized by unilateral spastic hemiparesis. The arm usually suffers more than the leg. The cause in premature infants is periventricular (periventricular) hemorrhagic infarction (usually unilateral), and congenital cerebral anomaly (for example, schizencephaly), ischemic infarction or intracerebral hemorrhage in one of the hemispheres (usually in the basin of the left middle cerebral artery) in full-term infants. Children with hemiparesis master age-related skills later than healthy ones. Therefore, the level of social adaptation, as a rule, is determined not by the degree of motor defect, but by the intellectual capabilities of the child. Clinically characterized by the development of spastic hemiparesis (Wernicke-Mann type gait, but without leg circumduction), delayed mental and speech development. Sometimes it manifests itself as monoparesis. With this form, focal epileptic seizures often occur.
(the term “hyperkinetic form” is also used)
G80.3 One of the most common causes of this form is previous hemolytic disease of the newborn, which was accompanied by the development of nuclear jaundice. Also the cause is status marmoratus of the basal ganglia in full-term children. With this form, as a rule, the structures of the extrapyramidal system and the auditory analyzer are damaged. The clinical picture is characterized by the presence of hyperkinesis: athetosis, choreoathetosis, torsion dystonia (in children in the first months of life - dystonic attacks), dysarthria, oculomotor disorders, hearing loss. It is characterized by involuntary movements (hyperkinesis), increased muscle tone, simultaneously with which there may be paralysis and paresis. Speech disorders are observed more often in the form of hyperkinetic dysarthria. Intelligence develops generally satisfactorily. There is no correct alignment of the torso and limbs. Most children experience preservation of intellectual functions, which has a favorable prognosis for social adaptation and learning. Children with good intelligence graduate from school, secondary specialized and higher educational institutions, and adapt to certain work activities. There are athetoid and dystonic (with the development of chorea and torsion spasms) variants of this form of cerebral palsy.
(earlier the term “atonic-astatic form” was also used)
G80.4 Characterized by low muscle tone, ataxia and high tendon and periosteal reflexes. Speech disorders in the form of cerebellar or pseudobulbar dysarthria are common. It is observed with predominant damage to the cerebellum, fronto-pontine-cerebellar tract and, probably, the frontal lobes due to birth trauma, hypoxic-ischemic factor or congenital malformation. Clinically characterized by a classic symptom complex (muscle hypotonia, ataxia) and various symptoms of cerebellar asynergia (dysmetria, intention tremor, dysarthria). With this form of cerebral palsy, a moderate delay in the development of intelligence is emphasized, and in some cases mental retardation occurs in the degree of deep debility or imbecility. More than half of the cases diagnosed with this form are unrecognized early hereditary ataxias.
G80.8 Despite the possibility of diffuse damage to all motor systems of the brain (pyramidal, extrapyramidal and cerebellar), the above-mentioned clinical symptom complexes allow in the vast majority of cases to diagnose a specific form of cerebral palsy.
The last point is important in drawing up a patient’s rehabilitation chart.
Often a combination of spastic and dyskinetic (with combined severe damage to the extrapyramidal system) forms is also noted, the presence of hemiplegia against the background of spastic diplegia (with asymmetric cystic foci in the white matter of the brain, as a consequence of periventricular leukomalacia in premature infants).
“,”author”:”Рвтор: Якимчук Т.Ð .”,”date_published”:”2020-04-24T07:03:00.000Z”,”lead_image_url”:NULL, ”dek”:NULL,”next_page_url”:NULL,”url”:”https://o-dcp.blogspot.com/2014/07/10.html”,”domain”:”o-dcp.blogspot.com ”,”excerpt”:”Ð”ÐµÑ‚Ñ ÐºÐ¸Ð¹ церебраДьный параДич – ДЦП – What about you? What is the difference?,”word_count”:746,”direction”:”ltr”,”total_pages”:1,”rendered_pages”:1}
Source: https://o-dcp.blogspot.com/2014/07/10.html
Symptoms of cerebral palsy
How can you suspect cerebral palsy? The first signs, if the form of cerebral palsy is not so severe that it can be recognized immediately, are often noticed by the child’s mother or father or another relative. The child must develop at a certain pace and, if there is a delay in psycho-motor development:
- a child at a certain age cannot hold his head up,
- doesn't look after the toy
- doesn't turn
- doesn't try to crawl,
- does not hum, etc.
This may not be a symptom of cerebral palsy, but it is definitely a reason to visit a specialist to correct possible deficiencies.
Another alarming symptom is that the child has difficulty swallowing and has problems with speech. Paresis in cerebral palsy can be in only one limb, be unilateral (arm and leg on the side opposite to the affected area of the brain), and affect all limbs. Insufficient innervation of the speech apparatus causes a violation of the pronunciation aspect of speech (dysarthria) in a child with cerebral palsy. If cerebral palsy is accompanied by paresis of the muscles of the pharynx and larynx, then problems with swallowing arise.
A child with cerebral palsy usually has decreased muscle tone. Skeletal deformations typical of cerebral palsy (scoliosis, chest deformities) develop. In addition, cerebral palsy occurs with the development of joint contractures in paretic limbs, which aggravates motor disorders. Motor skills disorders and skeletal deformities in children with cerebral palsy lead to the appearance of chronic pain syndrome with pain localized in the shoulders, neck, back and feet.
Hyperkinetic cerebral palsy is manifested by sudden involuntary movements: turning or nodding the head, twitching, grimacing on the face, pretentious poses or movements. The atonic-astatic form of cerebral palsy is characterized by discoordinated movements, instability when walking and standing, frequent falls, muscle weakness and tremor.
Cerebral palsy may be accompanied by such manifestations as strabismus, functional disorders of the gastrointestinal tract, respiratory disorders, urinary incontinence, epilepsy, hearing loss, mental retardation and mental retardation.
Clinical picture
Based on the clinical manifestations of the disease, it is possible to determine the localization of the pathological process and the severity of damage to the nervous tissue. The central nature of the disease confirms spasticity of the muscles of the limbs on one side of the body. In this case, the arm or leg is in a tense position, patients feel muscle stiffness and lose the ability to move. On the contrary, the peripheral form of pathology, which develops when nerve fibers are damaged after leaving the spinal cord, is characterized by a decrease in muscle tone.
Depending on the damage to the right or left hemisphere of the brain, right-sided and left-sided hemiparesis are distinguished. In older patients, right-sided hemiparesis is more common, and in children, left-sided development of muscle weakness is typical. Characteristic motor disorders due to muscle spasticity develop 2-3 weeks after the onset of the disease and can increase over the course of a year. Insufficient conservative treatment and refusal of rehabilitation measures causes progression of the pathology, which leads to the formation of hemiplegia. The disease causes serious consequences in the form of persistent contracture of muscles and joints - the person becomes disabled.
With a pathological process in the left hemisphere of the brain, paralysis occurs in the right half of the body
General clinical symptoms of the disease include:
- constant headaches of varying intensity for several weeks;
- general malaise, decreased ability to work, weakness;
- loss of appetite, weight loss;
- periodic increase in body temperature;
- pain in the joints and muscles.
Most often, right-sided and left-sided hemiparesis in adults develops after a stroke or traumatic brain injury. With focal damage to brain tissue, disturbances in motor function and a decrease in the sensitive sphere on one half of the body appear. Patients develop a Wernicke-Mann gait - the leg on the affected side does not bend and, when walking, makes a semicircle across the side. This variant of the disease usually has a mild course and a favorable outcome for the restoration of lost functions. With a large area of hemorrhage or damage to nervous tissue, in addition to motor disorders, the following neurological disorders are observed:
- change in speech (more often accompanies right-sided hemiparesis);
- episodic epileptic seizures;
- impairment of intelligence and learning ability;
- change in perception (agnosia);
- decreased ability for purposeful activity (apraxia);
- emotional instability and personality disorders.
In the congenital form of the disease, left-sided hemiparesis develops, which becomes noticeable 3 months after the birth of the child. In the initial stages of the disease, moderate changes in the motor ability of the limbs are observed:
- asymmetrical movements of arms and legs;
- weak passive and active movements of the affected limbs;
- when lying on your back, your hips are spread out;
- the hand is clenched into a fist;
- poor supporting function of the leg on the side of the pathology.
The final diagnosis is made around 12-18 months of age, when children begin to walk independently and motor impairments become more noticeable. In severe cases, the disease occurs with impaired development of speech and intellectual abilities. The congenital form of the pathology refers to one of the forms of cerebral palsy.
Sometimes childhood spastic hemiparesis develops, which affects the limbs, with the arms being affected more often than the legs. Cerebral palsy right-sided hemiparesis in newborns develops less frequently than left-sided hemiparesis.
How to cure cerebral palsy?
Since cerebral palsy is not a separate disease, but a whole group of conditions acquired at the earliest stages of a child’s development, it cannot be cured like cerebral palsy. But thanks to rehabilitation and the ability of the child’s brain to recover, many manifestations of cerebral palsy go away over time, and the child’s condition improves. As the child grows and his central nervous system develops, previously hidden pathological manifestations may be revealed, which create a feeling of so-called “false progression” of the disease. In reality, cerebral palsy does not progress throughout life. Only under the influence of additional somatic diseases can deterioration occur. But constant rehabilitation, on the contrary, will improve the condition and give a chance for a significant increase in the quality of life. The children's brain is flexible and plastic; healthy tissues can take over the functions of damaged structures.
Signs of cerebral palsy in children
The child learns to hold his head up, sit independently and walk later than necessary. Reflexes that should disappear by 6-8 months persist longer. Sometimes by the age of 1.5 years one arm works better because the other half of the body is weaker. Muscles can be both relaxed and overly tense, which is why the limbs have an unnatural state. Movements are too sudden or slow, often uncontrollable.
The following signs of the development of cerebral palsy in a child are also identified:
- skeletal deformity;
- asymmetry of the limbs;
- mental retardation - 30-50%;
- hearing impairment;
- speech problems;
- impaired swallowing;
- uncontrollable drooling;
- seizures - in 30% of cases;
- myopia or strabismus - 70%;
- uncontrolled urination and bowel movements.
Factors in the development of cerebral palsy
The causes of the disease include:
- premature or difficult labor
- hypoxia or asphyxia;
- infections during pregnancy;
- having a twin;
- congenital anomalies of the spinal cord or brain;
- impaired cerebral circulation;
- chronic diseases, hypo- and vitamin deficiency in the mother;
- smoking and drinking alcohol by the mother;
- Rhesus conflict.
There are often multiple risk factors present. It is not possible to name a specific reason in all cases.
Forms of the disease
Types of cerebral palsy in children are classified according to ICD-10. The syndrome belongs to class VI - diseases of the nervous system. Section - Cerebral palsy and other paralytic syndromes.
- Code G80.0 - spastic tetraplegia, prevalence - 2%
- G80.1 - spastic diplegia, 40%
- G80.2 - hemiplegic form, 32%
- G80.3 - dyskinetic, 10%
- G80.4 - ataxic, 15%
- G80.8 - mixed
- G80.9 - unspecified form.
Child development with cerebral palsy
Psycho-emotional characteristics manifest themselves in different ways: some children are irritable, excitable, and suffer from sudden changes in mood. Others are shy, fearful, and have difficulty communicating with people.
Restriction of physical activity causes curvature of the spine, contracture and internal pathologies. Due to speech impairments, meaningful communication is limited or absent. Parents should not show excessive pity and impressionability in their upbringing. It is necessary to praise the child more often, encourage him to take active actions, and form normal self-esteem; all this is very important for the normal development of the child. Parents should help the patient adapt socially.
Diagnostics
You should contact a neurologist if you suspect the development of cerebral palsy in a child if:
- at 1 month he does not blink his eyes at loud noises;
- at 4 months does not reach for toys and does not turn towards sounds;
- at 7 months does not sit independently;
- at 1 year of age does not speak words and acts with one hand;
- does not walk or moves incorrectly;
- experiences convulsions;
- makes sudden or excessively smooth movements.
To make a diagnosis, a neurologist studies the medical history, pregnancy and childbirth, and conducts an examination. Blood tests, urine tests, and MRI are prescribed. As well as a number of studies to exclude genetic diseases.
Clinics for treatment with the best prices
Price
Total: 384in 31 cities
| Selected clinics | Phones | City (metro) | Rating | Price of services |
| Road Clinical Hospital of JSC Russian Railways | +7(812) 679..show+7(812) 679-70-03 | St. Petersburg (metro station Ploshchad Muzhestva) | — | 10215ք (90%*) |
| State Clinical Hospital named after. V.M. Buyanova | +7(495) 321..show+7(495) 321-57-40+7(495) 321-54-92+7(495) 321-10-06+7(495) 321-13-06 | Moscow (metro station Tsaritsyno) | — | 12850ք (90%*) |
| Military Medical Academy named after. S.M.Kirova | +7(812) 292..show+7(812) 292-34-35+7(812) 292-32-86 | St. Petersburg (metro station Lenin Square) | — | 14930ք (90%*) |
| MEDSI in Khoroshevsky Proezd | +7(495) 152..show+7(495) 152-58-90+7(495) 780-40-64+7(495) 152-55-46 | Moscow (metro station Begovaya) | — | 19510ք (90%*) |
| MEDSI on Polyanka | +7(495) 730..show+7(495) 730-57-23+7(495) 152-55-46 | Moscow (m. Polyanka) | — | 19510ք (90%*) |
| MEDSI on Solyanka | +7(495) 023..show+7(495) 023-60-84+7(495) 730-14-34+7(985) 239-51-02 | Moscow (m. Kitay-Gorod) | — | 19510ք (90%*) |
| MEDSI on Leninskaya Sloboda | +7(499) 519..show+7(499) 519-37-04+7(495) 023-60-84 | Moscow (m. Avtozavodskaya) | — | 19510ք (90%*) |
| MEDSI on Leninsky Prospekt | +7(499) 519..show+7(499) 519-39-17+7(495) 023-60-84 | Moscow (metro station Shabolovskaya) | — | 19510ք (90%*) |
| MEDSI on Rublevskoe highway | +7(495) 023..show+7(495) 023-60-84 | Moscow (metro station Kuntsevskaya) | — | 19510ք (90%*) |
| MEDSI in Blagoveshchensky Lane | +7(495) 023..show+7(495) 023-60-84+7(915) 047-23-65 | Moscow (m. Mayakovskaya) | — | 19510ք (90%*) |
| * — the clinic does not provide 100% of the selected services. More details by clicking on the price. | ||||
Source
Treatment
Cerebral palsy cannot be cured completely, since damaged areas of the brain and nervous tissue cannot be restored. But treatment is needed to simplify the child’s life and adapt socially. A set of procedures is required, which includes:
- taking medications;
- massage and exercise therapy;
- physiotherapy;
- electroreflexotherapy;
- hippotherapy and canistherapy;
- classes with a speech therapist;
- motor development;
- training on simulators.
Rehabilitation
We specialize in the treatment of cerebral palsy in children. We use traditional methods and advanced techniques. Our goals are to renew lost skills, develop new ones, and adapt the child to living conditions.
Our statistics show the following successes after the rehabilitation course:
- new motor skills - in 70% of children;
- improvement of existing skills - 90%;
- development of speech, chewing skills and swallowing reflex - in 90%;
- improvement in psycho-emotional state - in 90%.
Registration for a rehabilitation course is carried out 2 months before the start. child’s medical history to our email [email protected] After studying, we will send an invoice with an approximate list of procedures. On average, the course is 3 weeks.
We accept patients from all regions of the country: Moscow, St. Petersburg, Yekaterinburg, Chelyabinsk, Novosibirsk, Ufa, Kazan and others.
Any form of cerebral palsy requires comprehensive and timely treatment. Don't delay, contact a rehabilitation center!
Qualified treatment and therapy methods
To prevent complete paralysis, treatment for hemiparesis must begin as early as possible. Treatment in children should begin in the first year of life. After a year, results are more difficult to achieve, because the main functions have already been formed. Often, after hemiparesis is detected in a child, the baby is hospitalized and then sent to a rehabilitation center for a long period.
The therapeutic technique depends on the severity of the pathology, the structural features of the body, and the age of the patient. As a rule, the general treatment regimen for hemiparesis includes:
- prescription of muscle relaxants - Mydocalm - reduction of muscle tone provoked by pain;
- taking drugs that improve blood supply to the brain - Cerebrolysin;
- taking anticonvulsants - Carbamazepine.
Reasons for the development of salt deposits on the neck and principles of treatment