Etiology
Paresis of the facial nerve can act in two qualities - an independent nosological unit, and a symptom of a pathology already progressing in the human body. The reasons for the progression of the disease are different, therefore, based on them, it is classified into:
- idiopathic lesion;
- secondary damage (progressing due to trauma or inflammation).
Facial nerve paresis
The most common cause of nerve fiber paresis in the facial area is severe hypothermia of the head and parotid area. But the following reasons can also provoke the disease:
- polio;
- pathogenic activity of the herpes virus;
- mumps;
- respiratory pathologies of the upper airways;
- head injuries of varying severity;
- damage to the nerve fiber due to otitis media;
- damage to the nerve fiber during surgery in the facial area;
- syphilis;
- tuberculosis.
The trigeminal nerve is often damaged during various dental procedures. For example, tooth extraction, root apex resection, opening of abscesses, root canal treatment.
Reasons for the development of the condition
A very common cause is neuritis or inflammation of the nerve. It can be compressed when passing through the birth canal or when obstetric forceps are applied incorrectly or when the head is in the pelvic plane for a long time. The cause may be infectious pathologies suffered during pregnancy, or hypothermia, which can cause not only inflammation, but also infections.
The cause may be surgery for another pathology. A very serious condition is otitis media or ear inflammation. The middle location of otitis is dangerous, in which inflammation of the facial nerve can occur. Infection in the tissue surrounding the nerve leads to its inflammation and swelling in the canal of the temporal bone in which it passes.
Another reason worth paying attention to is congenital syphilis. Also, paresis can be the result of mumps, because the nerve passes through the tissue of the parotid salivary gland and is divided into five branches. The cause may be polio immediately after birth. The cause of a central type lesion will only be a traumatic brain injury received during childbirth.
Symptoms of pathology
Damage to the facial nerve causes disruption of the passage of nerve impulses. This results in a violation of the main function of the facial nerve - ensuring the motor activity of facial muscles. Since facial paralysis often affects only one side of the face, the characteristic symptoms are difficulty moving the muscles in the affected area.
Paralysis is characterized by the following symptoms:
- drooping of the corners of the mouth and smoothing of the nasolabial fold on the affected part of the face;
- the patient cannot completely close the eye;
- disturbances in the natural hydration of the eye develop - the tear fluid is either insufficient or too much;
- difficulty chewing food develops due to weakening of the muscles around the mouth;
- loud sounds cause discomfort;
- the patient cannot frown.
Depending on the severity of facial asymmetry, mild, moderate and severe degrees of paralysis are distinguished. In mild forms of the disease, there is slight distortion of the corners of the mouth, and the motor activity of the facial muscles is difficult, but not completely paralyzed.
Moderate disease is characterized by worsening symptoms. The lower part of the face is motionless, but motor activity in the eyebrow area is still present.
The severe form is characterized by a visible violation of the symmetry of the face, and there is a significant distortion of the diseased side in relation to the healthy one. Motor activity of the muscles is completely absent, the patient cannot control facial expressions.
Paresis of the branches of the facial nerve occurs under the negative influence of a wide variety of causes.
- In first place is idiopathic, that is, primary paresis; it develops after severe hypothermia of one part of the head or parotid region.
The cause of this form of neuritis is also past respiratory diseases of the upper respiratory tract. Hypothermia of the head can occur while sitting under air conditioning or when traveling in a vehicle with an open window. - In second place among the causes of paresis is otogenic neuropathy - the nerve is affected during otitis media and during operations.
- The rarest cause is considered to be the negative impact of the herpes virus; the development of paresis due to tuberculosis, syphilis, mumps and polio is possible.
For all of the above reasons, an inflammatory process occurs, and paresis can also develop under the influence of a disturbance in the blood supply to the face. This occurs with ischemic strokes, a sharp increase in blood pressure, diabetes mellitus, and multiple sclerosis.
The motor and sensory function of the facial nerve can be impaired during dental procedures and injuries.
Neuritis of the facial nerve in children
- Weakness of facial muscles: a unilateral process leads to weakness of the facial muscles of one half of the face.
In this case, one half of the face remains motionless, or muscle movements are slowed down: - lag in the corner of the mouth when talking or smiling; smile asymmetry;
- lagophthalmos: when the eye is closed voluntarily, there is always a strip of the eye not covered by the eyelid.
With prolonged existence of lagophthalmos, the development of ulcers and erosions (defects) of the cornea of the eye is possible; - cheek swelling during sleep: this is due to decreased tone and weakness of the cheek muscles, which passively swell when exhaling during sleep.
- Impaired lacrimation: lacrimation: in this case, the edge of the lower eyelid may be slightly turned outward. The occurrence of lacrimation is associated both with a decrease in the tone of the orbicularis oculi muscle and with damage to the nerve pathways responsible for the innervation of the lacrimal glands;
- dry eyes, lack of tear production.
- Hearing impairment: hearing loss;
- hyperacusis: in this case, every audible sound is perceived with a special metallic tint. The occurrence of this symptom is associated with a violation of the innervation of the stapedius muscle, which fixes the auditory ossicles from excessive vibrations when the eardrum perceives a sound wave.
- Decreased taste sensitivity of the posterior 2/3 of the mucous membrane of the tongue.
Depending on the cause of occurrence, the following forms of facial nerve neuropathy are distinguished:
- traumatic: caused by trauma (most often in the extracranial area, although it is also possible with bone fractures inside the skull). In particular, neuropathy of the facial nerve can often be associated with injury during childbirth, as well as a consequence of oxygen starvation experienced during childbirth (fetal hypoxia);
- infectious: often associated with hypothermia, viral infection (usually herpetic, manifested by blistering painful rashes on the skin of the face), as well as respiratory infections (for example, with influenza, a viral disease that primarily affects the respiratory system, with the development of intoxication (manifested by chills, headache , weakness));
- ischemic: when the blood supply to the facial nerve trunk is disrupted;
- compression: develops when compression is caused by tumor processes inside the skull.
Depending on the reasons that caused the damage to the facial nerve, the following forms of neuritis (or neuropathy) of the facial nerve are distinguished:
- infectious neuropathy: caused by infections (for example, the herpes virus, which affects the nerve ganglia and manifests itself in the form of the formation of small blisters on the skin);
- ischemic neuropathy: a consequence of circulatory disorders in the facial nerve (for example, with inflammation of the stylomastoid artery, which supplies the facial nerve);
- compression neuropathy: a consequence of compression of a nerve in the bony canal of the facial nerve or as it exits the substance of the brain (in the cerebellopontine angle).
LookMedBook reminds you that this material is posted for informational purposes only and does not replace medical advice!
- A neurologist will help in treating the disease
Make an appointment with a neurologist
- Analysis of complaints and medical history: how long ago weakness of the facial muscles, dry eyes or lacrimation, impaired taste sensitivity of the tongue began;
- whether any injuries to the face or head were received in the period preceding the development of these complaints;
- whether there have been previous episodes of a similar disorder;
- did the patient suffer from any ENT pathology before the occurrence of these complaints (especially inflammation of the inner and middle ear, salivary gland);
- Before these complaints appeared, were there any blistering, painful rashes on the skin of the face and torso?
- Neurological examination: assessment of the strength of facial muscles, the presence of lacrimation disorders (dry eye or, on the contrary, lacrimation).
- Consultation with a pediatric otolaryngologist: hearing assessment, examination and palpation of the parotid salivary gland.
- CT (computed tomography) and MRI (magnetic resonance imaging) of the head: allows you to study the structure of the brain layer by layer and identify pathological processes in any part of the facial nerve (especially the intracanalicular part).
- It is also possible to consult a pediatrician or pediatric neurosurgeon.
- Painkillers.
- Decongestants (diuretics).
- Vitamins of group B, as well as A, C.
- Hormonal drugs (steroids).
- Drugs that improve blood supply to tissues and improve blood flow (antiplatelet agents that improve blood rheology).
- Physiotherapy: ultra-high-frequency currents, magnetic therapy, ultrasound with hormonal drugs.
- Neurotrophics: drugs that improve the restoration of nervous tissue.
- Contractures of facial muscles: with prolonged inactivity of the muscles, they tighten and harden, which leads to the complete impossibility of their movements.
- Synkinesia: when the nerve is restored, the nerve fibers grow incorrectly, which leads to unusual combinations of movements of the facial muscles (for example, when the eyes are closed, the corners of the mouth rise).
- Persistent neurological defect: permanent weakness in the facial muscles.
- A balanced and rational diet (eating foods high in fiber (vegetables, fruits, herbs), avoiding canned, fried, spicy, hot foods).
- Frequent split meals (5-6 times a day in small portions).
- Hardening.
- Daily walks in the fresh air.
- Wearing warm clothes in the cold season, wrapping your neck with a scarf.
Source: https://lookmedbook.ru/disease/nevrit-licevogo-nerva/children
| Poliomyelitis-like diseases - a polyetiological group of acute infectious diseases, clinically similar to mild paralytic forms of polio. They are associated with Coxsackie enteroviruses A and B, ECHO, mumps viruses, herpes simplex viruses, and adenoviruses. In approximately half of patients, the etiological factor remains unclear. Diseases are often sporadic. However, group B Coxsackie viruses can cause epidemic outbreaks. Before mass vaccinations against polio and continuous virological and serological examinations of patients, these forms of pathology were registered as poliomyelitis. Based on clinical manifestations, polio-like diseases are difficult to distinguish from mild forms of polio observed in vaccinated children. The clinical picture is characterized by paresis of single muscle groups, reversibility of pathological changes, and the absence of inflammatory changes in the cerebrospinal fluid. Patients with transient paresis account for about 90%. Infection caused by the Coxsackie B-5 virus is characterized by pronounced general infectious symptoms, as well as myalgia and herpetic sore throat. For viral infections ECHO-2, ECHO-11, ECHO-6 and Coxsackie A-4 describe spinal and bulbar-spinal forms with a fatal outcome. Virological and serological studies make it possible to distinguish between individual forms of diseases within this group. As with the mild spinal form of poliomyelitis, poliomyelitis-like diseases should be distinguished from focal myelitis, mononeuritis, diseases of the musculoskeletal system, and rickets. |
Varieties
Clinicians distinguish three types of trigeminal nerve paresis:
- peripheral. This is the type that is diagnosed most often. It can manifest itself in both an adult and a child. The first symptom of peripheral paresis is severe pain behind the ears. As a rule, it appears on one side of the head. If you palpate the muscle structures at this time, you can identify their weakness. The peripheral form of the disease is usually a consequence of the progression of inflammatory processes that provoke swelling of the nerve fiber. As a result, nerve impulses sent by the brain cannot fully pass through the face. In the medical literature, peripheral paralysis is also called Bell's palsy;
- central. This form of the disease is diagnosed somewhat less frequently than the peripheral one. It is very severe and difficult to treat. It can develop in both adults and children. With central paresis, atrophy of the muscle structures on the face is observed, as a result of which everything that is localized below the nose sags. The pathological process does not affect the forehead and visual apparatus. It is noteworthy that as a result of this the patient does not lose his ability to distinguish taste. During palpation, it can be noted that the muscles are under strong tension. Central paresis does not always manifest itself unilaterally. Bilateral damage is also possible. The main reason for the progression of the disease is damage to neurons located in the brain;
- congenital. Trigeminal nerve palsy in newborns is rarely diagnosed. If the pathology is mild or moderate in severity, then doctors prescribe massage and gymnastics for the child. Massage of the facial area will help normalize the functioning of the affected nerve fiber, and also normalize blood circulation in this area. In severe cases, massage is not an effective treatment method, so doctors resort to surgical intervention. Only this method of treatment will restore innervation to the facial area.
Causes and treatment methods for facial nerve paresis
Neurological diseases often receive little attention: sometimes because the symptoms are not pronounced, and sometimes because they seem insignificant. Facial nerve palsy is a disorder in which the facial muscles function incorrectly or not at all and there is significant limitation of movement.
About the disease
Facial nerve paresis is a disease of the nervous system characterized by a decrease in the ability of facial muscles to move.
It is most often a complication of ARVI; it arises and develops unexpectedly and rapidly - in just a few days. In ICD-10 it has the code G51.
With this diagnosis, external manifestations are significant: asymmetry of the facial muscles, mouth during conversation, difficulty opening and closing the eyes, inability to frown.
There is only one cause of paresis - disruption of the trigeminal nerve , but the disease has enough triggers.
As far as statistics are concerned, the disease does not have a “target audience”. It appears in both men and women, and even occurs in newborn children, being congenital. The prevalence of the disease is 20 people out of 100 thousand. More often, patients over 40 years old come to see a neurologist with this disease.
The facial nerve is responsible for the motor and sensory functions of the face, the innervation of the lacrimal and salivary glands, the sensitivity of taste buds on the tongue, and the sensory fibers of the upper layer of the face. When it is damaged, nerve impulses may arrive in a smaller volume - then they speak of a mild degree of paresis. In severe cases, the face looks like a mask, and nerve impulses do not pass through at all.
Symptoms
The disease has characteristic symptoms:
- Smoothing the forehead and nasolabial folds;
- Unilateral flaccid paresis of facial muscles with facial asymmetry;
- Inability to smile;
- Drooping of the corner of the mouth with limitation of its function;
- Variable movements of the lower lip;
- Drooping of the eyebrow on the side of paralysis;
- Widened palpebral fissure with drooping lower eyelid and incomplete closure of the eye.
Peripheral paresis
The most common type of disease that occurs in both children and adults. The first symptom of peripheral paresis is severe, sudden pain behind the ears , usually on one side. When diagnosing, the doctor feels the muscle structures and records their weakness.
Reference! This type of paresis most often occurs after suffering inflammatory processes, due to which the nerve fiber swells and the impulse cannot fully move across the face. In medicine, it is also called Bell's palsy.
Central paresis
This variety is less common, but is very difficult and painful, and difficult to treat.
Central paresis is characterized by atrophy of the facial , due to which the entire lower part (everything below the nose) sags, but the ability to distinguish taste is preserved.
The forehead and visual analyzer remain unchanged. Diagnostics shows excessive tension in the muscular system .
The disease occurs at any age and can affect one or both sides of the face. The cause of this pathology is damage to brain neurons (trauma, consequences of unsuccessful surgery, tumors).
Congenital and acquired paresis
Facial paresis also occurs in children. Despite the danger of the disease, it is easier and faster to restore its functionality in early childhood than in adulthood .
Paresis of the facial nerve in a child can be congenital or acquired. More often it develops as a result of trigeminal neuritis, or its inflammation.
In newborns, the incidence of congenital paresis does not exceed 0.1-0.2%, and in most cases this is associated with birth trauma (use of forceps during childbirth, fetal weight above 3.5 kg, etc.).
If we are talking about a congenital pathology, it is very difficult to get rid of it - almost impossible. Emergency surgery is used to determine whether the nerve responds to stimulation at all.
If there is a reaction, then the cause of the paresis is a birth injury, and then the chances of recovery increase markedly. Otherwise, a conclusion is made about a congenital anomaly of the facial nerve, and its restoration becomes impossible.
Photo
Read more about the photo of facial nerve paresis:
Causes
Paresis of the facial nerve can develop as a primary disease and as a secondary disease - a symptom of an inflammatory process.
The most common cause is neuritis, or inflammation of the nerve. It can be non-infectious and infectious (herpes, for example) in nature. As a rule, severe hypothermia becomes the trigger.
Paresis in some cases occurs from a violation of the blood supply to the facial nerve or centers of the cerebral cortex, as well as a tumor or injury to the nerve.
Paresis and paralysis of the facial muscles is observed with:
- diabetes mellitus and other endocrine disorders;
- stroke;
- poor quality therapy for atherosclerosis;
- multiple sclerosis;
- otorhinolaryngological diseases;
- dental injuries;
- head injuries;
- complication of acute respiratory infections;
- otitis;
- herpes;
- syphilis;
- tuberculosis;
- polio;
- mumps.
Paresis of the facial nerve appears against the background of upper respiratory tract infections and their complications, after operations of the ear or nasal cavities, with tumors near the trigeminal nerve, and toxic poisoning. Paresis is completely treatable if the patient seeks help in time.
Treatment
The effectiveness of therapy for facial paresis largely depends on the stage of the disease. The sooner the patient seeks help, the higher the likelihood of quick and high-quality treatment.
When the disease becomes chronic, it is almost impossible to treat and restore normal functioning of the nerve.
In acute cases, an integrated approach is used, which includes drug therapy, physiotherapy, massage and recreational exercises. Treatment of the disease in children and newborns follows the same scheme as in adults.
You cannot treat facial paresis at home. This is possible only after the doctor has carried out all the necessary procedures.
Medicines
In the acute period, it is necessary to get rid of the signs and symptoms of the disease and begin to restore nerve cells. The following methods are used:
- Pain relief by taking tablets or injections (analgesics and antispasmodics);
- Taking anti-edema medications;
- For moderate and severe cases, corticosteroids are prescribed;
- Taking vasodilator drugs;
- In some cases, it is recommended to take light sedatives, which also relieve muscle spasms;
- Taking B vitamins;
- If the visual apparatus is damaged, drops of artificial tears are prescribed, which moisturize the mucous membrane and prevent the penetration of infection;
- If secondary symptoms are detected, individual medications are prescribed.
If the facial nerve is completely torn, surgery is required . Operations are carried out in case of injury or congenital anomaly with the only condition that they must be carried out no later than a year after the onset of the disease. Otherwise, the facial muscles will completely atrophy.
Important! If a nerve ruptures, it is sutured. For congenital pathology, the autotransplantation . The graft is removed from the patient's leg, placed in the damaged part of the face, attached to a healthy nerve on the opposite side of the face.
Massage
For paresis, it is recommended to combine massage with recreational exercises. It is performed by the patient independently at home and does not require special preparation other than hand washing.
All manipulations should be carried out slowly, gently, superficially , so that no hand marks remain on the skin. Therapeutic facial massage is done from top to bottom, i.e. you need to move from the forehead to the chin area:
- Light movements on the forehead;
- Massage the eye socket area with eyes closed and down. The eyes are closed with the palm (the area of 2.3 fingers), and movement begins from the inner corner of the eye to the ear;
- Nose massage: move from the wings of the nose towards the ears;
- Massage of the mouth and perioral area: hand movements should begin in the middle of the mouth and end in the corner of the jaw (under the ears);
- Massage of the chin, neck;
- Circular movements of the head and tilts;
- A massage should always end with gymnastics.
Exercise therapy
Exercises for facial paresis help improve blood circulation in the neck and head, relax the muscles on the healthy side of the face and stimulate the muscles on the affected side.
When performing gymnastics, it is important to follow the rules:
- Use only the necessary muscle groups, the rest should be at rest;
- Strive for the quality of exercises, not their quantity;
- After each exercise, take a short break;
- Before performing the exercise, you should do it mentally: this additionally stimulates the nervous system;
- You can try to make the patient laugh so that at this time he holds the healthy side of his face with his hand. This helps restore your smile;
- Exercise therapy can be supplemented with DENAS therapy and Sujok therapy.
We invite you to watch a useful video on how to do facial gymnastics:
Forecast
It is difficult to assess the prognosis for facial nerve paresis, because... the effectiveness of therapy depends on many factors: the stage and cause of the disease, the duration, the timeliness of treatment, the competence of the doctor and the conscientiousness of the patient.
If the disease is no more than 3 months old, the probability of a favorable outcome is 75%. With a longer course of the disease, the chances of successful recovery decrease.
There is also a relationship between the success of treatment and the location of the damage: the prognosis is more optimistic if the damage to the facial nerve occurs at its exit from the skull.
Conclusion
When, after suffering from a cold, the ear suddenly begins to “give” pain, pain or discomfort in the parotid area, you should not self-medicate. If you notice the first signs of paresis (difficulty opening your eyes, drooping corner of your mouth), you should contact a neurologist. Effective treatment is only possible with rapid response and diagnosis.
Paresis in infants
Paresis of the facial nerve in a newborn may be a congenital pathology in the infant. In this case, the disease is caused either by birth trauma or infectious diseases suffered by the mother during the period of bearing the child.
Often, paralysis of the facial muscles is observed during complicated childbirth, when forceps were applied to the child’s head, or vacuum extraction was performed.
A characteristic external manifestation of paresis in newborns is weakening of one side of the mouth. The baby's lips are lowered and feeding is difficult.
As a rule, the situation in infants can be corrected with the help of massage. With timely treatment, paralysis is completely cured, the motor functions of the facial muscles are restored, and the risk of developing any complications is minimal.
Congenital paresis of the facial nerve in newborns, not caused by birth trauma, is treated depending on the degree of nerve damage. For mild to moderate illness, recovery is achieved through massage and drug therapy, but for severe paresis, surgical intervention may be necessary.
Neuritis in children: causes, symptoms, treatment and prevention methods
Neuritis implies an inflammatory process of the nerve ending. In children, damage to the facial or auditory nerve is more often diagnosed. The causes and symptoms of the disease differ depending on the age of the child. For any form of neuritis, consultation with a doctor is required to begin treatment in a timely manner and avoid complications.
Causes
In newborns, inflammation of the nerve endings develops after birth trauma. It can occur during uterine formation of the fetus or during the passage of the birth canal.
During the process of bearing a child, the baby's facial part comes into close contact with the mother's bone tissue, which causes compression of the nerve ending and inflammation. Unilateral facial neuritis is more often diagnosed.
In older children, the disease progresses under the influence of various factors:
- frequent hypothermia, accompanied by muscle spasms;
- physical damage;
- excessive concentration of sugar in the blood;
- neoplasms of a malignant or benign nature;
- complications during oral cavity treatment;
- intoxication of the body;
- damage by adenoviral infection;
- frequent stressful situations;
- systemic lupus;
- diseases of the ear canal.
Types of neuritis in children
Neuritis of the auditory nerve ending in children is accompanied by the following symptoms:
- discomfort in the ear area;
- nausea;
- attacks of dizziness;
- otitis of the auditory nerve ending;
- purulent discharge;
- deterioration of the hearing aid;
- impaired coordination;
- tinnitus.
When the facial nerve is damaged in a newborn, half of the child’s face is wrinkled and motionless. It's easier to notice the difference when the baby cries.
With the development of neuritis, the sick child is not fully applied to the mother's breast, and some of the milk flows out of the mouth.
On the affected area of the face, the baby cannot close his eyes completely, causing lacrimation. Symptoms in school-aged patients are more pronounced:
- asymmetrical position of facial muscle tissues;
- lower lip lowered;
- when laughing, the face contorts, a grimace of grinning appears;
- in the affected area the eyes do not close completely;
- while eating, some of the food remains in the oral cavity;
- the functioning of taste buds deteriorates.
When the first signs of neuritis occur in a child, you need to contact a neurologist. The doctor will collect anamnesis and identify the cause of the disease.
To obtain accurate information about the location of inflammation, the patient is prescribed electroneuromyography. The child is sent for stool and blood tests to identify microbes and infectious diseases.
Based on the data obtained, the doctor draws up a course of treatment.
When diagnosing inflammation of the nerve endings in a child, treatment involves the use of drug therapy, massage procedures, and physical education courses to restore the symmetry of the facial area and eliminate the symptoms of the disease. Before using any traditional therapy methods, it is recommended to consult a doctor.
Drug treatment
Treatment is aimed at eliminating the cause of the disease. To strengthen the immune system and stimulate blood circulation, multivitamins are prescribed.
If neuritis develops as a result of a cold, the patient is prescribed an anti-inflammatory drug. When the body is affected by a bacterial infection, antibacterial agents are used.
To eliminate swelling and discomfort, the baby is prescribed corticosteroids.
Massage treatments
If there is a large degree of asymmetry of the facial part, massage is prescribed. The course of treatment begins 7 days after the first signs of neuritis appear. This is explained by the risk of irreversible changes with earlier massage procedures. Touching the affected area yourself is contraindicated; this increases the risk of complications.
Healing Fitness
To speed up recovery, the patient is prescribed gymnastics 2 times a day. The duration of physical exercise should not exceed 15 minutes. The training regimen is drawn up by the doctor on an individual basis, depending on the severity of the disease and the characteristics of the patient’s body.
Complications
Failure to follow the doctor’s recommendations or ignore symptoms increases the risk of limited mobility of muscle tissue and complete atrophy. The asymmetry becomes irreversible. With neuritis, a child may develop conjunctivitis.
Prevention of neuritis in children
To reduce the risk of inflammation of the nerve ending in a child, a number of rules must be followed:
- protect children from stressful situations;
- control your diet;
- carry out hardening to strengthen the immune system;
- protect children from hypothermia, dress them according to the weather;
- periodically go out into nature.
Sources
- Clinic and diagnosis of optic neuritis in children with multiple sclerosis, Guseva M.R., 2001
- Clinical and epidemiological features of uveitis in children, Guseva M.R., 2004
Diagnostic accuracy and quality service are the main priorities of our work. We value every review our patients leave us.
Panina Valentina Viktorovna
Actress, Honored Artist of the RSFSR
I found out about you on the Internet - I urgently need an MRI.
And after the performance I’m with you. I really liked your staff. Thank you for your attention, kindness and accuracy.
May everything be as good in your soul as I am now, despite all the problems...
Be!!! We're happy! Your Panina V.V.
Open review scan
Array( [ID] => 107 [~ID] => 107 [CODE] => [~CODE] => [XML_ID] => 107 [~XML_ID] => 107 [NAME] => Panina Valentina Viktorovna [~NAME ] => Panina Valentina Viktorovna [TAGS] => [~TAGS] => [SORT] => 100 [~SORT] => 100 [PREVIEW_TEXT] =>
I found out about you on the Internet - I urgently need an MRI.
And after the performance I’m with you. I really liked your staff. Thank you for your attention, kindness and accuracy.
May everything be as good in your soul as I am now, despite all the problems...
Be!!! We're happy! Your Panina V.V.
[~PREVIEW_TEXT] =>
I found out about you on the Internet - I urgently need an MRI.
And after the performance I’m with you. I really liked your staff. Thank you for your attention, kindness and accuracy.
May everything be as good in your soul as I am now, despite all the problems...
Be!!! We're happy! Your Panina V.V.
Source: https://cmrt.ru/zabolevaniya/nervnoy-sistemy/nevrit-u-detey/
Degrees
Doctors divide the severity of trigeminal nerve paresis into three degrees:
- light. In this case, the symptoms are mild. A slight distortion of the mouth may occur on the side where the lesion is localized. A sick person must make an effort to frown or close his eyes;
- average. A characteristic symptom is lagophthalmos. A person can practically not move the muscles in the upper part of the face. If you ask him to move his lips or puff out his cheeks, he will not be able to do this;
- heavy. The asymmetry of the face is very pronounced. Characteristic symptoms are that the mouth is severely distorted, the eye on the affected side practically cannot close.
Signs and symptoms
Symptoms of facial neuritis are clearly visible - facial asymmetry is difficult to confuse or overlook. Not only the forehead and cheek suffer, but also the palpebral fissure - it widens. The nasolabial fold drops and the lower lip droops.
The effect of baring teeth is observed, and during laughter the mouth is pulled to the healthy side. If a person closes his eyes, the eyelids will not close completely. The patient loses the ability to kiss and whistle. While eating, food particles get stuck in the teeth. The tongue may also be affected, affecting the sense of taste.
Types of nerve damage
There are two types of pathology - central paresis and peripheral.
Central paresis is characterized by damage to the lower facial muscles. External asymmetry may be absent. The patient does not experience difficulty moving his eyes, he can frown or relax his forehead, but the muscles around the jaw and cheeks are tense, and there is no facial expression in this area.
Central paresis is rare and is caused by damage to the neural network of the brain.
In 85% of cases, doctors diagnose peripheral paresis. The onset of the disease is characterized by pain behind the ear. When palpated, it feels lethargic and lacks muscle tone. As a rule, the disease affects only one side of the face, which causes visible asymmetry.
The cause of peripheral paresis is an infectious disease and inflammatory process. As a result, swelling of the nerve fibers is formed and their further compression, which causes paralysis of the facial muscles.
Diagnostics
When the first signs of neuritis occur in a child, you need to contact a neurologist. The doctor will collect anamnesis and identify the cause of the disease. To obtain accurate information about the location of inflammation, the patient is prescribed electroneuromyography. The child is sent for stool and blood tests to identify microbes and infectious diseases. Based on the data obtained, the doctor draws up a course of treatment.
Symptoms
Symptoms of facial nerve paresis
The severity of symptoms directly depends on the type of lesion, as well as on the severity of the pathological process:
- smoothing the nasolabial fold;
- drooping corner of the mouth;
- the eye on the affected side may be unnaturally wide open. Lagophthalmos is also observed;
- water and food flows out of the slightly open half of the mouth;
- a sick person cannot wrinkle his forehead much;
- a characteristic symptom is deterioration or complete loss of taste;
- auditory function may become somewhat worse in the first few days of pathology progression. This causes great discomfort to the patient;
- lacrimation. This symptom manifests itself especially clearly during meals;
- the patient cannot pull the lip into a “tube”;
- pain syndrome localized behind the ear.
What types of disease are there?
According to the nature of the flow
According to the nature of the course, there are 3 types of trigeminal neuralgia:
- Spicy. Characterized by frequent attacks of unbearable pain. The number of attacks per day in rare cases can reach 300. The intensity of pain in acute trigeminal neuralgia intensifies when touching trigger points (nose, chin, temple).
- Subacute. Attacks of pain are present, but their intensity and frequency are reduced.
- Chronic. The disease occurs cyclically: periods of exacerbation are followed by periods of remission. During remission, the patient does not experience acute attacks of pain - the sensations have a less pronounced aching character. A new exacerbation usually occurs unexpectedly without obvious reasons.
A separate point is made about the atypical nature of the course of the disease. In the atypical form of trigeminal neuralgia, pain does not occur in attacks, but is constant.
Severe aching or throbbing pain, burning, itching are signs of atypical trigeminal neuralgia.
Due to the occurrence
Because of their occurrence, doctors distinguish between primary and secondary neuralgia:
- Primary or true neuralgia is caused by a direct effect on the trigeminal nerve - compression, irritation or disruption of blood flow.
Primary neuralgia occurs regardless of any other diseases. - Secondary neuralgia (symptomatic) is a pathology that develops against the background of other diseases (tumors, infections, inflammations).
By localization
Types of trigeminal neuralgia according to localization:
- 1st branch – the areas of the eyeballs and eyelids, forehead and upper part of the back of the nose are affected;
- 2nd branch – pain syndrome affects the lower eyelids, cheekbones, tip of the nose, upper jaw;
- 3rd branch – the lower jaw and oral cavity are vulnerable.
Most often, pathology of the 2nd and 3rd branches is diagnosed.
Bell's palsy
You can identify violations at home (note the presence or absence of facial expression disorders and movements of facial muscles), you just need to take a test - see if the movements are performed equally on both sides (close your eyes; close alternately first one and then the other eye; close your eyes;
In diagnosis, the main importance is to conduct research to determine the level and depth of nerve damage - the development of indications for surgical intervention, and therefore the success of the operation, depends on this. The set of diagnostic procedures includes a mandatory visual inspection, determination of the level and threshold of sensitivity.
instrumental studies in the form of myography, ultrasound of blood vessels and, if necessary, tomography. Only after receiving complete information about the location and extent of damage to the nerves and muscles of the face, a treatment plan (reconstructive operations) is drawn up, the essence of which is the reinnervation of the affected muscle fibers or the transposition of muscle fibers.
Surgical treatment of facial nerve paralysis is carried out by Mikhail Leonidovich Novikov, a reconstructive microsurgeon, a leading specialist in Russia in the treatment of congenital pathologies of the peripheral nervous system.
Bell's palsy is a disorder of facial expression due to damage to the facial nerve. Paresis (prosoparesis) and Bell's palsy have similar symptoms: the disease affects one side and is characterized by visible asymmetry of facial features.
The disease is accompanied by the formation of nerve edema. The causes of Bell's palsy are hypothermia, impaired immunity and infectious lesions of the body.
This form of paresis is characteristic of older people and is often a secondary disease that develops against the background of progressive atherosclerosis, but children are also susceptible to paralysis.
Therapy includes taking antiviral drugs. Unlike facial paresis, Bell's palsy can be successfully treated in nine out of ten cases.
Many people are interested in whether facial nerve paresis can go away without treatment? It should be remembered that this serious disease is fraught with loss of facial function and hearing impairment, so it must be treated in a timely manner.
Facial nerve paresis, its symptoms and treatment require attention from the patient. The disease cannot be started.
Causes
The causes of a damaged nerve are associated with the following factors:
- Injuries are common causes. Moreover, injury can occur both at home and during dental procedures. If there is a fracture or crack in the bones of the skull on the right or left side of the head, this threatens the onset of the disease. Bruises cause less harm.
- Impact from external factors. The causes of neuritis lie in hypothermia, inflammatory processes on the face (otitis media).
- Infections and tumors. Facial nerve neuropathy is a complication of mumps. Herpetic pathologies also influence the onset of neuritis. Tumors in the area of the nerve put pressure, causing the nerve to also become inflamed.
The causes of the disease may be associated with pathological changes and processes in the brain; polio has a negative effect, as well as sclerosis and other diseases. Polyneuropathy affecting other parts of the body can cause damage to the facial nerve. Neuropathic syndrome in rare cases is related to hereditary predisposition.
Pathogenesis and causes are associated with physical damage to the nerve. To understand pathogenesis, it is necessary to understand that on the human head all organs are closely interconnected and close to each other. So, swelling due to inflammation in the ear or herpes leads to pressure on the nerve. Infectious processes also have a destructive effect on the structure of the nerve. Consequently, the pathogenesis is based on pathological changes in the shape, size, dysfunction and integrity of the facial nerve.
Therapeutic measures
This disease must be treated as soon as the diagnosis has been made. Timely and complete treatment is the key to restoring the functioning of the nerve fibers of the facial area. If the disease is neglected, the consequences can be disastrous.
Treatment of paresis should only be comprehensive and include:
- eliminating the factor that provoked the disease;
- drug treatment;
- physiotherapeutic procedures;
- massage;
- surgical intervention (in severe cases).
Drug treatment of paresis involves the use of the following pharmaceuticals:
- analgesics;
- decongestants;
- vitamin and mineral complexes;
- corticosteroids. Prescribe with caution if the pathology progresses in the child;
- vasodilators;
- artificial tears;
- sedatives.
Physiotherapeutic treatment:
- Sollux lamp;
- UHF;
- paraffin therapy;
- phonophoresis.
Massage for paresis is prescribed to everyone - from newborns to adults. This method of treatment produces the most positive results in cases of mild to moderate damage. Massage helps restore the functioning of muscle structures. Sessions are carried out a week after the onset of paresis progression. It is worth considering that massage has specific features, so it should be entrusted only to a highly qualified specialist.
Massage technique:
- warming up the neck muscles - you should tilt your head;
- massage begins with the neck and back of the head;
- You should massage not only the sore side, but also the healthy one;
- an important condition for a quality massage is that all movements should be carried out along the lines of lymph outflow;
- if the muscle structures are very painful, then the massage should be superficial and light;
- It is not recommended to massage the localization of lymph nodes.
Pathology should be treated only in a hospital setting. Only in this way will doctors have the opportunity to monitor the patient’s condition and observe if there are positive dynamics from the chosen treatment tactics. If necessary, the treatment plan can be adjusted.
Some people prefer traditional medicine, but it is not recommended to treat paresis in this way alone. They can be used as an adjunct to primary therapy, but not as individual therapy. Otherwise, the consequences of such treatment can be disastrous.
Neuralgia in a child: causes, signs, treatment methods
Neuralgia in a child causes severe pain that occurs against the background of damage to the peripheral part of the nervous system. In children, intercostal and trigeminal neuralgia is detected. Delayed therapy or failure to seek medical help leads to attention deficit, delayed development of the speech apparatus and hyperactivity. Children diagnosed with neuralgia are apathetic, nervous, and tearful.
Provocative factors
The following factors contribute to the development of neuralgia:
- lack of oxygen during fetal formation;
- insufficient hemoglobin concentration in a pregnant woman;
- smoking by the expectant mother;
- trauma during childbirth;
- depression and stress while waiting for the baby;
- premature birth;
- infectious pathologies;
- diseases of the spine;
- increased physical activity;
- constant drafts, dampness;
- long stay of the baby in a kangaroo pouch;
- abnormalities of the musculoskeletal system.
Diagnosis of neuralgia
In order to diagnose neuralgia in a child, the following activities are carried out:
- the child’s medical history is studied;
- inspection is carried out;
- a small patient is examined by a neurologist, during the consultation the sensitivity of the area where the pain is concentrated is identified, the nature of the pain is determined, and the causes of the pathology are clarified;
- do electroneuromyography - assess the speed of impulse transmission along nerve fibers, as well as the degree of their damage;
- material taken from nerves is subject to microscopic examination;
- examine the condition of blood vessels;
- If necessary, the child is examined by a neurosurgeon.
Treatment. Complications
After making an accurate diagnosis, the doctor prescribes complex therapy. It is selected individually depending on the severity of the clinical picture, the age of the small patient and taking into account the characteristics of the body, as well as the nature of the pain syndrome. Conservative treatment of neuralgia in children (symptoms influence the choice of methods) consists of:
- taking analgesic medications;
- herbal medicine;
- homeopathic treatment;
- physical therapy;
- massage;
- physiotherapy;
- acupuncture;
- manual therapy;
- reflexology.
Surgical treatment is indicated only in very severe cases.
All children with this diagnosis are monitored by a neurologist at the clinic at their place of residence.
The danger of neuralgia in a child is due to the occurrence of pain shock and neuritis, as well as muscle atrophy and sensitivity disorders. To minimize negative consequences, it is recommended to consult a doctor at the first signs of pathology to establish a diagnosis and select complex therapy.
Clinical picture of neuralgia in an infant
The main symptoms on the basis of which neuralgia is assumed are the following:
- constant shaking of the lower and upper extremities, as well as the chin;
- during strong crying, the baby pulls his hands towards his face, the muscles of which twitch;
- poor quality sleep;
- when changing body position, the baby screams loudly;
- When crying, due to a clenched jaw spasm, the baby is unable to open his mouth.
If the above symptoms are detected, you must seek help from doctors to receive timely qualified assistance. To confirm the diagnosis, an examination of the fundus of the eye is performed and an ultrasound is performed.
If necessary, other examination methods are also prescribed. To treat neuralgia in infants, courses of massage, physical therapy and physiotherapy are used. Pharmacotherapy is rarely used.
Neuralgia in infants is treatable.
Intercostal neuralgia
The intercostal nerves depart from the spinal cord and are located in the intercostal spaces. When they are irritated, neuralgia occurs. This disease is not common in children. The main symptom of the disease is a sharp pain in the area of the ribs, which radiates to the back. Additional symptoms of intercostal neuralgia in children include:
- the appearance of pain when changing body position, coughing, sneezing, sudden movements;
- pain on palpation of the chest and spine;
- discomfort when inhaling and exhaling;
- involuntary muscle contraction;
- loss of sensation in some areas of the body;
- increased sweating;
- redness of the skin in the area where the irritated nerve is located;
- possible convulsions of the upper extremities;
- palpitations and rapid pulse.
After some time, the pain goes away because the nerve root dies. The condition improves, but then the pain reappears, preventing you from breathing deeply. If the disease becomes advanced, it will become more difficult to treat. Therefore, if the above symptoms occur, the child should be shown to a neurologist.
Therapy for intercostal neuralgia
If a child experiences pain in the chest area, contact a pediatrician. The doctor will conduct an examination and, first of all, do an ECG to determine the functioning of the heart muscle.
Most likely, a chest X-ray will also be prescribed to rule out pulmonary pathology. Then the sick child is sent to a neurologist, who treats intercostal neuralgia in children.
He conducts additional examination using computer diagnostics, myelography and electrospondylography. And only after an accurate diagnosis is made, the necessary therapy is prescribed.
Depending on the child’s condition, treatment is carried out in a hospital or on an outpatient basis. Bed rest is required in the first days. It is advisable to lie on a hard surface. To do this, place a wooden shield under the mattress.
Non-steroidal anti-inflammatory drugs are prescribed to reduce pain. A major role in treatment is given to:
- physical therapy;
- physiotherapeutic procedures;
- massage;
- acupuncture;
- manual therapy;
- homeopathy.
In addition, gels and creams are used for local anesthesia.
Topographic anatomy of the trigeminal nerve
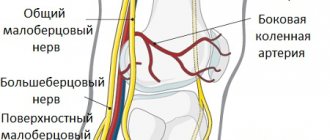
The trigeminal is one of the largest cranial nerves. It consists of a sensory and motor nucleus and fibers. Coming from the trigeminal ganglion, the sensitive part is divided into three branches:
- orbital;
- maxillary;
- mandibular
These branches provide sensitivity to the soft tissues of the skull and face, mucous membranes and tissues of the mouth, nose, and teeth. The motor part controls the tissues of the lower lip, jaw, gums and chewing muscles.
Inflammation of the trigeminal nerve disrupts the functioning of the corresponding motor and sensory systems.
Most often, pain occurs on one side of the face, but there is also bilateral inflammation of the trigeminal nerve.
Causes of trigeminal neuralgia in children
The disease is caused by the following reasons:
- Severe hypothermia - constant exposure to drafts or under running air conditioning.
- Features of the anatomical location of the nerve - close superficial location causes increased sensitivity.
- Infections of the nose and throat - sinusitis, sinusitis, tonsillitis.
- Chronic dental problems – caries.
- Tumors that contribute to pinching and cause neuralgia in the child.
- Complications after traumatic brain injuries.
- Herpes virus infection, chickenpox.
- Consequences after surgery on the face.
Before treatment, it is important to establish the cause of inflammation of the trigeminal nerve. The success of the chosen therapy largely depends on this.
Symptoms associated with inflammation of the facial nerve
When the trigeminal nerve becomes inflamed, pain immediately occurs in the facial area, and it may resemble symptoms of disease in other organs. In a child, signs of trigeminal neuralgia are of two types:
- Typical - attacks of burning, severe pain occur cyclically, gradually reaching a peak and gradually subsiding. Their frequency is strictly individual, from once a day to every hour. The sensation is similar to an electric shock.
- Atypical - rare. Painful sensations are observed constantly. They are distributed over half the face.
Other symptoms include:
- decreased or increased sensitivity of the skin in the area of the face with an inflamed nerve;
- nervous tics - involuntary muscle twitching;
- increased salivation and lacrimation;
- redness of the skin;
- sleep disturbance;
- constant fatigue and bad mood.
Often pain attacks due to inflammation of the trigeminal nerve in a child are provoked by touching the skin of the face, blowing wind, talking, smiling, brushing teeth.
Therapy for facial nerve inflammation
To treat neuralgia in a child, the doctor prescribes the following therapy:
- Procedures to eliminate foci of dental and otolaryngeal infections.
- NSAID drugs that relieve pain and inflammation.
- B vitamins and drugs to improve peripheral blood supply.
- Anticonvulsants are used individually.
- Dry heat on the affected part of the face is recommended.
There is no need to self-medicate a serious illness; early consultation with a doctor gives positive results.
Any pathology of the nervous system, including neuralgia, can affect the development of the child’s vital organs.
Prognosis with conservative treatment
A favorable outcome of the disease is observed in those patients who completed the course of treatment on time. The prognosis also depends on the cause of the paresis; if it is an injury or an oncogenic tumor, then muscle atrophy may develop.
Muscle contracture is observed in cases where the patient sought help after 2-3 months from the onset of the disease. When a contracture occurs, the face looks like a mask, and asymmetry is noted in the healthy half.
Surgical operations to restore muscle innervation are successful if such treatment is carried out on time. With muscle atrophy, it is not possible to completely restore facial movements. If the defect is noticeable, cosmetic surgery is performed.
The best treatment for facial paresis depends on the severity of the disease. Conservative treatment is based on drug therapy. Treatment includes therapy with the following groups of drugs:
- non-steroidal anti-inflammatory drugs for pain relief;
- drugs to quickly get rid of swelling;
- taking antispasmodics to relieve spasm of nerve fibers;
- in severe cases of the disease, injections of corticosteroids are indicated to relieve swelling and relieve pain;
- to improve local nutrition, vasodilating drugs are used;
- moisturizing drops to normalize tear production.
Paresis is often accompanied by feelings of anxiety and sleep disturbances. In this case, taking mild sedatives before bed is indicated. As a rule, such therapy helps to quickly relieve spasms by normalizing sleep and the activity of the nervous system.
A course of vitamins to strengthen the nervous system (group B drugs) is mandatory.
The success of a patient’s cure depends on timely consultation with a doctor.
Typically, paresis is characterized by acute and subacute forms. The acute form of the disease develops quickly, and from the appearance of the first symptoms (ear pain) to impaired facial expressions, it takes from one to two weeks. The subacute form develops within a month.
If treatment is not started at this stage, the subacute form may become chronic. In this case, surgical intervention will be required to correct the facial expression disorder.
Treatment of paresis is a long process. From the start of therapy to the restoration of facial expressions, at least six months of intensive treatment take place.
However, timely treatment guarantees the patient’s full recovery without the development of possible complications.
The chronic form of the disease is dangerous with the risk of hearing loss and decreased visual acuity due to lack of blood circulation in the affected area.
Along with drug treatment, physiotherapeutic methods are used. As a rule, electrophoresis or phototherapy is indicated for paresis. Low-frequency magnetic therapy methods are also used.
Physiotherapeutic methods are aimed at restoring normal blood flow. They help improve metabolic processes in the affected area and relieve spasm of nerve fibers.
In addition to physiotherapy, some massage techniques and acupuncture are used. All this allows you to improve local blood circulation and gradually helps restore the ability to control your own facial expressions.
Patients are shown facial gymnastics, which helps restore motor activity. It includes the following exercises:
- “frowning eyebrows” - the patient needs to frown and relax the brow ridges several times a day;
- “full cheeks” - you should puff out your cheeks as much as possible and then relax them;
- “whistle” - you need to stretch your lips folded forward as much as possible, imitating a whistle.
Exercises for developing the facial muscles responsible for the movement of the eyelid also help: the eyes should be opened as wide as possible, making a surprised face, and then relax. Gymnastics is performed up to 10 times a day, in any free minute.
However, gymnastics or massage alone cannot cure paresis, so it is necessary to combine these methods with conservative drug treatment.
Treatment of the disease
Before starting treatment, both the patient and the doctor must set specific goals for themselves.
The goals of treatment of facial nerve paresis:
- Firstly , it is necessary to get rid of the concomitant disease (this could be otitis media, neuritis, etc.) in order to proceed directly to the treatment of the disease itself.
- Secondly , it is necessary to cure swelling and inflammatory processes that have spread in the nerve tissues.
- Thirdly , it is necessary to maintain blood flow in the nerve tissues so that the nerves can be “nourished” and get rid of inflammation.
- Fourthly , it is necessary to increase immunity so that the disease does not return a second time with even greater force.
- And fifthly , it is necessary to stimulate the processes of nerve regeneration in every way.
Techniques
Treatment methods for peripheral and central facial nerve paresis are practically the same.
integral therapy methods as treatment
This course has a lot of advantages, but it will only be effective if completed in a timely manner. If treatment occurs immediately, the paresis will recede in eighty percent of cases.
The first method is gymnastics for facial nerve paresis, and the second is the use of reflexes.
Acupuncture, massages, mud poultices and laser treatment are also widely used . All these techniques are very effective if you follow all the advice and recommendations of the doctor.
First, significant improvements in general condition will follow, followed by the possibility of complete recovery.
At the end of the entire course, doctors can make the face more vibrant and mobile. The shape of the face will also change – it will no longer appear asymmetrical. The facial nerve will be able to perform all its functions again, and the symptoms that were observed from the influence of the concomitant disease will disappear.
Also, after the course of treatment, the risk of recurrent disease is significantly reduced.
Drug treatment of facial nerve paresis
Naturally, treatment of facial nerve paresis cannot be done without medications.
They can only be prescribed by the attending physician, since there is no universal remedy that would suit all patients.
Such drugs usually increase immunity and the general condition of the patient’s body, which is why a general therapeutic course is prescribed: physical activity will help improve blood flow, and the drugs will increase the susceptibility of nerve fibers and relieve inflammation.
Complications
In case of untimely or incomplete therapy, the consequences may be as follows:
- irreversible damage to the nerve fiber;
- improper nerve restoration;
- complete or partial blindness.
If the pathology is recognized in a timely manner, there are no health consequences; almost all children recover without complications. With advanced paresis, atrophy of facial muscles, impaired taste perception, speech disorders, facial asymmetry and cosmetic defects can form.
Complications of the disease
The most important danger that neuritis of the facial nerve poses is contracture of the facial muscles. This is a strong reduction of the diseased half of the face, which is a consequence of improper or untimely treatment.
The following complications of facial nerve neuritis may also occur:
- Facial hemispasm or blepharospasm is involuntary twitching of the facial muscles that occurs due to compression of a nerve.
- Amyotrophy. If no noticeable improvements are observed within a year from the onset of the disease, muscle atrophy may develop, which is an irreversible process. To avoid this condition, you should constantly massage your face using baby cream and fir oil.
- Facial synkinesis. This condition resembles a short circuit: irritation in one area provokes an impulse in another. For example, when chewing, tears may flow from the affected side, and when closing the eyes, the corner of the mouth may rise.
- . Inflammation of the inner lining of the eyes and cornea occurs due to incomplete closure of the eyelids.
Symptoms and manifestations
The most basic function of the branches of the facial nerve is considered to be motor, that is, the nerve ensures the mobility of the muscles responsible for facial expressions.
In the absence of the necessary nerve impulse, symptoms primarily manifest themselves in the inability to perform facial movements.
Facial nerve paresis is divided into an acute stage, lasting up to 2 weeks, and a subacute phase lasting up to one month.
If the disease is not cured within a month, then they speak of the chronic stage of the disease.
The following manifestations are noticeable on the affected side:
- Smoothing of the nasolabial fold.
- The corner of the mouth is downturned.
- The eyelids are wide open, and when they close, lagophthalmos is observed - a light, visible strip of sclera remains.
- Taste sensations on the first third of the surface of the tongue are reduced or completely stopped.
- The function of the eyes is impaired - dryness or, on the contrary, watery eyes appears. A noticeable secretion of tears occurs when eating and chewing food.
- The patient cannot extend his lips, and food may leak out of the half-open half of the mouth.
- In the first days of the disease, there is an exacerbation of hearing - pain appears with loud sounds.
- Before the development of all symptoms, there is a sharp pain behind the ear.
- An attempt to wrinkle the forehead ends in failure - the skin of this area remains completely smooth.
In addition, facial nerve paresis is usually divided into several degrees.
- Mild degree. The asymmetry of the face is not very pronounced - there may be a slight distortion of the mouth on the affected side, the patient can, with difficulty, frown the muscles of the eyebrows, and completely close the eye.
- Paresis of moderate severity is already manifested by lagophthalmos, minor movements are noted in the upper half of the face. When asked to perform lip movements or puff out a cheek, their incomplete execution is noted.
- A severe degree of paresis is manifested by pronounced asymmetry - the mouth is noticeably distorted, the eye on the affected side almost does not close. Simple movements in which facial muscles should participate are not performed.
Diagnostic methods
Damage to the maxillofacial nerve has specific signs that are clearly expressed. If inflammation is suspected, the doctor conducts neurological tests - the patient performs certain exercises with facial muscles:
- frowns, raises eyebrows;
- blinks, closes his eyes;
- smiles, showing teeth;
- puffs out his cheeks, tries to whistle;
- wrinkles his nose.
Special neurological tests will help determine the presence of the disease
Such movements help the specialist analyze the symmetry of the facial muscles on both sides of the face and identify paralysis or weakening of tissues.
If the development of concomitant diseases (inflammation of the brain, neoplasms, infections and viruses) is suspected, additional diagnostic methods are prescribed:
- electroneuromyography;
- MRI (magnetic resonance imaging);
- CT scan;
- electroencephalogram.
Important! The diagnosis is made based on examination, the results of a neurological test and instrumental studies. Comprehensive diagnostics allows not only to identify the disease, but also to understand what to do in a particular case
The need for surgical intervention
The operation is indicated in the following cases:
- nerve rupture;
- paresis caused by trauma;
- congenital facial paralysis;
- ineffectiveness of conservative treatment for chronic disease.
In case of rupture, surgery involves suturing the damaged area of the facial nerve. This intervention is quick and rehabilitation does not require a long time.
For congenital paralysis or other anomalies, nerve transplantation from other parts of the patient’s body is used.
The operation leaves no visible scars, except for a small strip behind the ear. As a result of surgical intervention, the asymmetry is successfully corrected, and difficulties with facial expressions do not arise in the future.
Types of disease
There are two types of neuritis of the facial nerve, which differ in their origin:
- Primary. The disease develops independently against the background of hypothermia.
- Secondary. The condition is a consequence of other diseases (for example, otitis media, Melkerson-Rosenthal syndrome, herpetic infection).
Manifestations of secondary neuritis of the facial nerve are combined with symptoms of the underlying disease. Also, nerve inflammation can be a consequence of a hypertensive crisis, impaired blood supply to the brain, neuroinfections, tumors or various injuries.
Treatment of newborns and children
Prosoparesis of the facial nerve in newborns is treated in the maternity hospital immediately after birth. The baby is exposed to thermal physiotherapy, which helps relieve swelling and spasm of nerve fibers.
Treatment of infants continues after discharge, at home. It involves applying heat to a soft cloth that is applied to the affected area on the child. Loud and sudden noises should be avoided at home as they may cause discomfort to the sick child.
In order for the baby to recover faster, a massage is needed that will help quickly restore facial activity. Massage should only be performed by a specialist!
Treatment of children of primary school age is also based on physiotherapeutic methods, gymnastics and massage. Along with these methods, drug therapy is carried out, including taking antispasmodics. Young patients are required to take a course of vitamins.
Treatment
Treatment for neuritis should begin immediately as soon as the first symptoms of the disease appear. The most effective in this regard are corticosteroids (Prednisone). The drug is taken in the dosage recommended by the doctor for at least 10 days. This remedy allows you to reduce swelling of the nerve and reduce the degree of its infringement.
Symptomatic therapy is also indicated - drops similar to artificial tears are used to moisturize the eyeball. In addition, a massage of the face, neck and collar area is prescribed. At first it should be light, and then the intensity should gradually increase.
From the third week of treatment, physiotherapeutic procedures are prescribed. Sedatives may be prescribed to reduce anxiety, eliminate muscle spasms and other symptoms of neuritis.
Full recovery occurs no earlier than 3 weeks from the moment of active full treatment. But final functions may take several months to recover.
In three quarters of cases, complete recovery occurs and normal functions of the facial muscles are restored. However, if the disease lasts more than 3 months, it is much more difficult to establish normal facial expressions. The disease can recur, and subsequent cases of the disease are much less responsive to treatment.
Treatment methods
A neurologist may prescribe the following procedures for the treatment of facial neuritis:
- Magnetic therapy (to eliminate nerve swelling).
- Phonophoresis of drugs.
- Carboxypuncture (activation of blood circulation).
- Electrophoresis (anti-inflammatory effect).
- Laser therapy (infrared radiation).
Surgical treatment may also be prescribed. It is justified when there is no result of conservative therapy within 8-10 months. The essence of the operation is autotransplantation of the facial nerve. Material for transplantation is taken from the lower extremities. In the affected part of the face, 2 new branches of the facial nerve are grafted onto the muscles, connecting them to the healthy side. The result is an extension of the facial nerve, which ensures symmetrical movement of facial expressions.
Massage and exercise therapy
The self-massage technique is quite simple. It is recommended to perform it at least twice a day. Use stretching movements to massage healthy muscles towards the sick ones, and lift paralyzed ones from the chin to the forehead.
You also need to massage your eyelids, pressing them with your middle fingers and making circular movements. You can also massage the tip of your nose, stroking the healthy side down and the diseased side up. Massage for neuritis of the facial nerve will prevent muscle atrophy, improve blood supply to nerve cells and, in general, recover faster from the disease.
Exercise therapy for neuritis of the facial nerve is no less effective. It should be done twice a day for twenty minutes. The essence of the exercises is to ensure muscle mobility - you need to close your eyes, raise your eyelids, frown your eyebrows, puff out the wings of your nose, and then lift them, smile, opening your teeth, close your lips, and so on. During exercise, you need to monitor the uniformity of breathing.
Treatment with folk remedies
In addition to traditional therapy for facial neuritis, you can also use traditional medicine recipes:
- To revive the affected nerve, a medicine is prepared from several varieties of herbs. You should take one glass bottle of pharmaceutical tincture of calendula, hawthorn, motherwort and marina root (peony) and mix. Add half a bottle of Corvalol there, as well as 3 tsp. honey (pre-dissolved in a water bath). Drink a teaspoon of the mixture at bedtime. The course of treatment is two months, and after that you need to take the same break. After this, you can repeat the tincture.
- After brewing rose petals in a teapot (you should choose red and burgundy flowers), take them instead of regular tea during the day. This remedy is very effective for neurasthenia and has a calming effect on the body. The course of treatment with rose tea is 3 weeks.
- Goat's milk will also help with facial neuritis. Add mumiyo (the size of beads) and a tablespoon of honey (it’s better to take acacia honey) to the hot milk. The duration of treatment is 21 days, then a break of at least 2 weeks is required. After this, the course should be repeated.
Prevention
Since paresis of nerves in the face often develops due to hypothermia, the only preventative measure is to prevent the effects of cold and drafts. They will help prevent the development of paresis and timely treatment of otitis media and respiratory diseases.
The basis for the prevention of paresis in newborns is the careful management of labor using gentle techniques for pushing. In older children, this is the prevention of infections, injuries to the face and ear area, exacerbations of herpes infections, and severe hypothermia. Parents need to strictly monitor the condition of the facial muscles and consult a doctor at the slightest deviation from the norm.