It’s a good thing to fall asleep sweetly and soundly, and also to have a colorful dream. But after this, it happens that numbness of the toes or the entire leg appears, as well as numbness of the fingers. This happens because the arm or leg is pinched, which causes compression of the nerve trunks and blood vessels. But after a light warm-up and rubbing, the numbness of the fingers or toes goes away within a few minutes. But what to do if it doesn’t go away and bothers you constantly?
Numbness of the toes is a symptom that indicates damage to nerves or blood vessels at different levels, which requires detailed examination in a clinical setting.
Numbness of the toes can be a transient condition or persistent, disturbing for a long time. Numbness in the toes is described as a crawling, tingling, burning sensation. Essentially, this is a sensory disorder. Numbness of the toes is often the first symptom of an emerging disease that causes pinching of the sciatic nerve. Sometimes, at the same time pain occurs in the lower back or throughout the leg, and the function of the limb is impaired.
Causes of numbness in toes
Numbness of the toes often occurs in an uncomfortable position, also in the position of crossing legs, which causes compression of the nerve trunks and blood vessels. And this is a passing condition that goes away on its own and does not require seeking help. But there are multiple spinal diseases in which one of the symptoms is numbness. Therefore, if there is prolonged numbness in the toes that does not go away on its own, you need to contact a specialist.
The most common causes of numbness in the toes:
- osteochondrosis of the lumbar spine, spondylosis;
- displacement of the vertebrae, which causes back pain and numbness in the toes;
- vertebral instability;
- protrusion or intervertebral disc herniation, very rarely - Schmorl's hernia lead to irritation of the nerve roots (radicular syndrome);
- radiculitis, inflammation of the sciatic nerve (sciatica), which are a consequence of the above conditions;
- arthrosis of the knee joint - numbness of the toes occurs when the nerve trunks in the popliteal fossa are compressed;
- bursitis of the knee joint - swelling causes compression of the nerves and numbness of the toes;
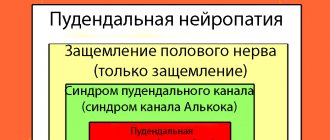
- Tunnel syndromes: irritation of the obturator nerve in the canal of the same name; compression of the sciatic nerve between the piriformis muscle and the sacrospinous ligament (piriformis syndrome); entrapment of the lateral cutaneous nerve of the thigh under the inguinal ligament (Bernhardt-Roth disease); compression of the tibial nerve in the tarsal tunnel (tarsal tunnel syndrome); compression of the plantar digital nerves (metatarsalgia or Morton's syndrome). All of them in one way or another cause numbness in the toes.
- Occlusive vascular diseases: obliterating endarteritis, diabetic angiopathy, atherosclerosis. Impaired sensitivity and numbness of the toes occurs from impaired blood supply to the tissues.
- Damage to the central nervous system: micro-stroke, multiple sclerosis also lead to numbness of the toes.
- Tumors of the spine and tuberculosis also cause numbness and pain in the back.
In order to find out the cause and prescribe appropriate treatment, it is necessary to conduct a thorough examination, taking into account all clinical and physical data. It is also necessary to take into account the data of an X-ray examination, conduct a computed tomography or MRI, and, if necessary, perform ultrasound diagnostics and a thermal imaging examination.
Source: mednean.com.ua
Inflammation of the sciatic nerve: what causes it and how to treat it
Treatment may include both drug and non-drug methods. The treatment method depends on how far the disease has progressed and what its underlying cause is - whether it is caused by pinched nerve fibers or inflammation.
Non-drug therapies include:
- physiotherapy,
- massage,
- physiotherapy,
- exercise classes,
- hydrotherapy.
Non-traditional, but well-proven treatment methods for sciatica:
- manual therapy,
- cupping massage,
- acupressure,
- acupuncture (reflexotherapy),
- ozone therapy,
- hirudotherapy (treatment with leeches),
- mud therapy.
However, medical treatment of sciatica remains the mainstay.
The main groups of drugs used in the medical treatment of sciatica.
| Type | Impact principle | Examples of drugs |
| vitamins and vitamin complexes | improving the functioning of the nervous system | combilipen, milgamma, B vitamins |
| muscle relaxants and antispasmodics | relieving muscle spasms | corisoprodol, mydocalm, drotaverine, papaverine |
| glucocorticosteroids | counteracting inflammatory processes, relieving pain | dexamethasone, prednisolone |
| non-steroidal anti-inflammatory drugs (NSAIDs) | counteracting inflammatory processes, relieving pain | ibuprofen, indomethacin, diclofenac, phenylbutazone, lornoxicam, ortofen, naproxen |
| analgesics | pain relief | ketorolac, paracetamol, morphine, tramadol |
It should be noted that although glucocorticosteroids are used for the same purpose as NSAIDs, the method of their use differs significantly from the method of using the latter. Symptomatic treatment with steroid drugs can only be carried out under the supervision of a physician. The same can be said about narcotic drugs for pain relief (morphine, tramadol).
In some cases, the patient may be prescribed drugs from different categories.
The most commonly used local forms of drugs are in the form of creams and ointments. In the acute form of the disease, with severe pain, some painkillers and anti-inflammatory drugs, as well as vitamin complexes, can be administered parenterally.
If there is a need to use tablet forms of drugs, it is best to consult a doctor before using them. After all, many NSAIDs are known for their side effects. In particular, they can negatively affect the gastrointestinal tract, causing ulcers and bleeding, especially with long-term use.
Folk remedies are often used for sciatica - herbal tinctures (celandine, hot pepper, aloe), honey, beeswax, horse chestnut ointments. They perfectly relieve pain and inflammation.
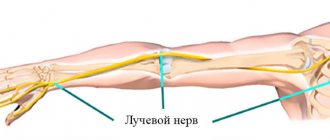
Inflammation of the sciatic nerve or sciatica (sciatic neuralgia) develops unexpectedly even in people who consider themselves absolutely healthy. The sciatic nerve is the longest in the human body: it begins in the lumbar region, passes through the lower end of the spine (coccyx), the posterior thigh muscles and lower limbs, reaching the feet.
Sciatica itself is not considered a pathology, but serves as a manifestation of other diseases.
pharmacological medications, manual therapy, exercise therapy and physiotherapeutic therapy can alleviate and completely eliminate the symptoms of sciatica. Therefore, you should not self-medicate, but put yourself completely in the hands of qualified specialists.
Treatment of this disease is carried out by a set of complex therapeutic measures. As a rule, there is no general treatment for patients with sciatica; the course of treatment is selected strictly individually in each specific case.
However, there are still general treatment methods, which include the following methods:
- treatment regimen;
- drug therapy;
- physiotherapeutic methods;
- massage;
- physiotherapy;
- sanitary resort treatment.
Pronounced symptoms or the first harbingers of the disease are a reason to consult a specialist. It is necessary to make an accurate diagnosis, because the specifics of treatment will depend on the identified causes of inflammation of the sciatic nerve.
At the same time, the neurologist examines the degree of damage to the sciatic nerve, conducting special tests for motor reflexes:
- Achilles tendon,
- knee joint,
- checks for the presence of Lassen symptoms (pain on the back of the thigh and lower leg when lifting a straight leg up and forward independently), Bonnet (the same procedure, only the doctor lifts the leg).
How to treat inflammation of the sciatic nerve? The first aid for a sharp exacerbation of sciatica will be painkillers:
- analgin;
- derivatives with a pronounced direction of action: tempalgin - pain symptoms subside as a result of the action of tempidine - a mild tranquilizer;
- sedalgin - codeine and paracetamol have an invigorating effect on the nervous system, relieving inflammation of the nerve roots;
- baralgin - antispasmodics in the composition remove muscle inflammation, relieving spasm of the sciatic nerve;
- pentalgin.
Non-steroidal anti-inflammatory drugs (NSAIDs) – tablets, injections for severe pain, ointments will be mandatory in the treatment of sciatic nerve entrapment:
- Diclofenac (tablets) – anesthetizes and relieves inflammation, pain, swelling. Injections for inflammation of the sciatic nerve of this drug are more effective, but the degree of influence of side effects on the liver and kidneys increases. Therefore, they are prescribed intramuscularly or intravenously by a doctor with a minimum interval of 12 hours.
- Movalis is a very powerful drug that quickly relieves pain symptoms. Quickly reduces inflammation of the sciatic nerve. The presence of significant side effects requires taking the tablets under medical supervision for no more than 5 days.
- Ibuprofen, Nise, Nurofen are NSAIDs with less pronounced effects. They are good because they affect the peripheral nervous system, relieving inflammation, and muscles, relaxing and removing spasms.
- Corticosteroids are prescribed for long-term, persistent pain symptoms. These are hormonal agents that relieve swelling and inflammation of the sciatic nerve.
For pregnant women, the doctor will recommend a special treatment for inflammation of the sciatic nerve. Taking most medications during this period negatively affects the health of the expectant mother and child, so it is strictly prohibited to use medications without consulting a doctor.
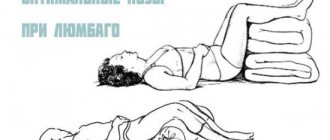
The acute period of inflammation of the sciatic nerve in most cases lasts from 5 to 10 days. During this time, it is necessary to ensure a reduction in physical activity and rest for the lumbosacral region, in other words, it is more in a horizontal position, preferably on a hard orthopedic surface. The subsidence of symptoms is not a reason to increase sports activity.
Symptoms of a pinched nerve in the leg
Signs indicating a pinched nerve in the lower extremities are as follows:
- The appearance of acute and sharp painful sensations in the pinched area. They may also be tingling;
- Swelling of the epidermis, change in shade to red at the pinching point;
- Increased sweating (quite rare);
- Inability to straighten limbs in the morning. As the disease worsens, this symptom becomes permanent.
- The patient appears more constrained; when in an upright position, unbearable pain is noted;
- Painful sensations can also reach the back area.
Most often, symptoms of this kind appear unexpectedly, but disappear just as quickly. In later stages of the disease, the presented sensations continue uninterrupted. In the area in which the pain is felt most strongly, there is precisely the point where the nerve is pinched. This may be due to both physical and psychological influences.
Painful sensations may also occur during sleep. Additional factors that determine pinched nerves in the lower extremities, as mentioned above, may be redness and swelling of the skin. Constant sweating is sometimes added to this. There is a worsening of motor activity in situations where the motor nerve is affected, and sometimes atrophy.
LiveInternetLiveInternet
Quote from Enigmatica
Read in full In your quotation book or community!
What can your feet tell you?
Do you often pay attention to people's feet? Some have fingers lined up in a row, others have one longer than all the others, and clearly do not want to fit into generally accepted norms. Scuffs, calluses, corns - their location often indicates certain deformities of the foot, habits and preferences; nails can actually tell a lot about the owner.
What do your legs , specifically your feet and toes, say? Yellow and white, flat and concave, striated and spotted, thin and thick - they literally scream about diseases and a person’s lifestyle. Feet need our attention, good comfortable shoes, pedicures and massages, and our attentive attitude to our health. Let's try to decipher the signals of our legs and talk about what to do in this or that case.
Foul smelling feet What is it? Smell? Is it really coming from your feet? How inconvenient! Sweaty feet are a fairly common problem among both men and women. Often its causes lie in the fact that the legs have to work too hard. Does the nature of your work force you to be on your feet all day? It’s no wonder that with such “parking” your feet sweat, and in this way they try to somehow cool down.
If you are wearing shoes or boots made of synthetic materials, an unpleasant odor cannot be avoided. Don't want to be embarrassed when taking off your shoes? Remember, your feet need rest and good leather shoes. Another reason for excessive sweating of the feet is their deformities, for example, flat feet. Defects in the structure of the bone structure of the feet lead to increased muscle strain and sweating. Special orthopedic insoles and shoes will solve the problems. However, sweaty feet don't always smell bad. For sweat to acquire an odor, bacteria must work on it. That is why the main method of combating foot odor is to wash them frequently and thoroughly with soap containing antibacterial components and use deodorizing powders.
Calluses on the foot or calluses Calluses are hardening and thickening of the superficial layer of skin on the plantar surface of the foot, opposite the toes, especially the big toe and on the heels. A “fresh” corn looks like an area of redness and swelling on the foot, then as hyperkeratosis develops, it acquires a dirty yellow color, becomes rough to the touch, and is covered with small and deep cracks.
Corns can be flat or convex, sometimes have a central core extending deep into the skin. The sensitivity of the skin in the area of hardening is reduced, but painful sensations occur while walking. Microbes can penetrate into the skin through cracks, which leads to the development of inflammation.
Causes of corns:
uncomfortable, tight high-heeled shoes; flat feet; “bone” in the area of the big toe; excess weight; poor circulation in the feet. To get rid of hardening on the feet, you need to eliminate the causative factor, contact a specialist podiatrist and remove the stratum corneum mechanically using a keratolytic cream or an anti-callus patch.
Calluses Calluses most often form on the skin on the back of the toe joints and on the heels, that is, in those places where the foot is subject to the greatest pressure and friction. Trauma to the skin leads to the growth of its surface layer and roughening. The hardened callus puts pressure on the skin nerve endings located underneath it, which causes pain.
If you have calluses, it means the shoes you are wearing do not match the size and anatomical features of your feet. Perhaps the cause of calluses is a bunion on the big toe, deformed toes, or flat feet. To get rid of calluses, sometimes it is enough to eliminate their cause. In some cases, the help of a podiatrist and a high-quality pedicure are necessary.
Flat feet You should consider it if:
legs get tired quickly when walking; by the end of the working day, your legs feel like they are filled with lead, muscle cramps, swelling of the feet and ankles appear; the heels of your shoes are worn down on the inside; your foot seems to have grown in length or become wider.
Simply put, flat feet is a deformity of the foot in which the plantar surface of the foot touches the ground completely. The disease can be hereditary or acquired as a result of injury, wearing the wrong shoes, or being overweight. Flattening of the arches of the feet causes tension in the plantar fascia, causing discomfort and pain. The problem can be solved with the help of orthopedic insoles and shoes. It is necessary to strengthen the foot muscles with the help of special exercises.
“Bump” on the big toe Scientifically, this is called valgus deformity of the big toe, popularly known as “bunion.” In this case, the thumb deviates towards the other four and can be located under the second finger, which takes on a hammer-like shape.
and forces you to give up dress shoes in favor of “slippers.” In 99% of cases, the “bone” is a female problem. The reasons for its formation are genetic predisposition, congenital weakness of the foot joint, flat feet, excess weight, wearing tight high-heeled shoes, hormonal imbalance associated with menopause. The solution to the problem is surgical. It is necessary to eliminate the traumatic factor. Creams and gels based on analgesics and non-steroidal anti-inflammatory drugs and wearing insoles will help to temporarily reduce pain.
Swollen, red and painful thumb Most often, this disease affects men over 40-45 years of age. The attack develops late in the evening or at night, often after a heavy intake of meat and alcohol. The joint of the big toe begins to hurt very much, swells, becomes red, and hot to the touch. These are symptoms of gouty arthritis.
Gout is a disease associated with impaired metabolism of purine bases and the accumulation of uric acid salts in the human body. Most often, salts are deposited in the area of the big toe joint, sometimes in the knee or elbow joint, and also in the form of nodules (tophi) on the cartilage of the auricles. Treatment for gout involves following a special diet and taking medications that reduce uric acid levels. Attacks are relieved with anti-inflammatory drugs.
Crossed toes Crossed deformity of the toes is characterized by the absence of their orderly row, with one of the toes located on top of the other. Crossed toes are injured by shoes, their joints become inflamed, which causes pain that intensifies when moving the toes and walking. Chronic arthritis causes loss of joint function, making movement very difficult.
The reasons for this condition can be different:
congenital defect in the shape of one of the toes; “bunion” - curvature of the big toe or valgus deformity of the big toe; arthritis; wearing narrow, tight shoes. Medications help relieve pain. It is necessary to eliminate pressure on the toes, wear shoes with wide toes and use special orthopedic devices.
Long second toe Normally, the second toe is somewhat shorter than the big toe, but in some it is significantly larger in size than its fellow. Doctors call the long second toe Morton's finger and consider it an innate constitutional feature of human feet.
Why is Morton's finger dangerous? Its excessive length causes excess pressure on the joint between the first phalanx of the toe and the metatarsus, this pressure increases when walking and standing, which causes injury to the bone joint, the development of arthritis and pain in the foot. Calluses form on the tip of the second finger and on its bones, causing additional inconvenience. The solution to the problem is orthopedic: it is necessary to select the right shoes with a wide and high toe, perhaps a size larger than usual, as well as the use of special instep supports that relieve the load on the second toe.
Hammer fingers Hammer deformity most often affects the second finger, but can also occur on other fingers except the thumb. The protruding bone of a crooked finger is injured by shoes, it hurts, which causes great inconvenience when walking, and sometimes leads to lameness. The formation of a painful callus completes the picture of unpleasant sensations.
The causes of hammertoe deformity can be:
wearing tight shoes and callus on the dorsum of the toes; hallux valgus or “bunion” of the big toe, in which the second toe takes on the appearance of a hammer; chronic arthritis, causing deformation of the finger joint; injuries to the toes, leading to predominant tone of the toe flexor muscles. Orthopedic treatment: selection of shoes and wearing instep supports. Sometimes they resort to surgical methods to eliminate finger deformities.
Hooked toes Hooked toes are the result of a nerve conduction disorder and, as a result, a muscle imbalance in which the force of contraction of the flexor muscles of the toe becomes greater than the counterforce of the extensor muscles. As a result, one or more fingers bend at the last joint and remain in this position all the time.
A bent finger is injured by shoes, its joints become inflamed, the bones become calloused, which causes significant inconvenience and pain. When wearing uncomfortable shoes and heavy load on the feet, the deformity progresses and leads to persistent contracture of the interphalangeal joints and gait disturbance. You can reduce pain and stop the development of the disease if you wear properly selected orthopedic shoes with wide and high toes, use special insoles, liners and instep supports, toe caps with gel, protective bandages, and combs.
Claw-shaped toes Deformation of the toes, in which they bend at the second and third interphalangeal joints and freeze in this position, is called claw-shaped toes. In fact, the toes are shaped like claws, their bones protrude above the main surface of the foot, are compressed, injured by shoes, calluses appear on them, and arthritis often develops
Claw-shaped toes cause significant inconvenience when choosing shoes and make movement difficult. While walking, the main load falls on the pads of the bent fingers and on the bases of the metatarsal bones, so the legs get tired very quickly and begin to hurt. In severe cases, when the deformity is accompanied by contracture or complete immobilization of the joints, lameness occurs. The cause of the formation of claw-shaped fingers is most often neuritis and trauma to the nerve fibers, leading to a predominance of the tone of the finger flexor muscles. Sometimes joint deformation is a consequence of inflammation - arthritis. Treatment consists of selecting shoes with high and wide toes, using special orthopedic combs and splints, and protective caps for the toes. All this will reduce pain and discomfort.
Pain in the “pad” of the thumb This may be a symptom of sesamoiditis. This disease is most often encountered by dancers and athletes, people who are forced to walk a lot for duty. The pain occurs in the ball of the big toe, that is, on the plantar surface of the joint connecting the first phalanx and two small bones of the metatarsus, called sesamoids.
These bones act as a lever that increases the tension of the tendons that flex the thumb; with sudden movements and heavy loads, the tendons can tear and the bones break, which causes pain and inflammation. The pain with sesamoiditis is mild at first, intensifying with every step and attempt to push off the floor. Then, if left untreated, it becomes severe, but is never accompanied by redness and swelling of the thumb joint.
Heel pain Pain that occurs when resting on the heel, especially severe during the first steps after a long rest, not accompanied by swelling and redness of the skin in the heel bone, is characteristic of plantar fasciitis or heel spurs.
Plantar fasciitis is an inflammation of the wide plantar fascia (ligament) that supports the longitudinal arch of the foot, attached on one side to the tubercle of the heel bone, and on the other to the heads of the metatarsal bones. As the load on the legs increases, the fascia can become torn and inflamed, causing pain. The plantar fascia has the ability to quickly heal itself; during the rest period, scars form at the site of its injury, but subsequent stress leads to their rupture and increased pain. The chronic course of plantar fasciitis leads to the hardening of scar tissue, the deposition of calcium salts in it and the formation of a heel spur, which brings a lot of suffering to the patient.
Pain in the “pads” of the 3rd and 4th toes The appearance of swelling and pain in the plantar part of the foot in the area of the pads of the 3rd and 4th toes can be caused by Morton’s neuroma and irritation of the nerve passing in this anatomical region. The pain is burning, shooting in nature, radiating to the fingers, similar to the sensation of a foreign body or a fold of a sock.
Sometimes there is a loss of sensitivity in this area, numbness or tingling, and convulsive muscle twitching. After removing shoes and kneading the foot, the pain often goes away, but appears and intensifies as soon as the patient puts on his shoes again. Morton's neuroma is a benign growth on the nerve trunk that compresses the nerve fibers. The reasons for its formation are not known to science, but its presence leads to inflammation of the nerve and disruption of its conductivity. To relieve pain, painkillers and anti-inflammatory drugs are used, it is recommended to stop wearing shoes with narrow toes, and use orthopedic inserts and insoles. In the absence of effect and persistent pain, hormone injections and various physiotherapeutic techniques are used.
Red, swollen, hot to the touch foot Erythromelalgia is a disease of unknown origin, more common in adults over 40 years of age, occurring in the form of attacks of pain in the foot, accompanied by redness, swelling, increased local temperature and sweating. The occurrence of an attack is usually associated with increased stress on the legs and overheating; relief occurs at rest after rest.
It has been noted that erythromelalgia accompanies scleroderma, varicose veins of the lower extremities, neuromas of the legs and feet, hypertension, blood cancer, and drug intolerance. The disease is incurable, chronic, and over the years the attacks become more severe and longer lasting.
Ingrown nail It is impossible to make a mistake; when a nail becomes ingrown, it seems to sink into the skin, injuring it, and the addition of an infection leads to the development of paronychia or felon. The big toes are most often affected. Wearing tight shoes and improperly cutting nails leads to a chronic course of the process. The nail grows over and over again, changes its shape, the skin thickens and creeps onto the free part of the nail, which causes pain.
In the absence of panaritium, you can cope with the situation yourself. It is enough to steam your foot, release the ingrown edge of the nail and place a small thick cotton ball under it. Treat your finger with an antiseptic solution until the nail changes shape and stops growing. In case of a chronic process, when the nail is deformed and it is impossible to correct its shape, competent pedicure and self-medication will not help solve the problem, the help of a podiatrist is needed. Sometimes an ingrown nail has to be removed so that it can be replaced by a new, smooth one.
Yellow, crumbling, peeling nails Most often, these are signs of a fungal infection. Penetrating through cracks in the nail into the nail bed, the fungus multiplies, grows deep into the tissue, loosens it, which leads to thickening and detachment of the nail plate. The nail becomes grayish-white or yellowish in color, becomes brittle, and becomes covered with cracks.
Usually the disease begins with the big toe, then the infection spreads to the remaining toes. The diagnosis is made on the basis of microscopy of scraping tissue of the nail bed, treatment is prescribed by a mycologist. It involves long-term oral administration of antifungal drugs; no traditional methods help. If the disease persists for a long time, the fungus dies, but changes in the nail bed reach such a degree of destruction that the nail can no longer grow healthy. By the way, nails can peel off not only due to a fungal infection; deep circulatory problems in the feet due to heart disease, diabetes mellitus, obliterating endarteritis are often accompanied by dystrophic changes in the nails.
Spoon-shaped nails A change in the shape of the nails, in which their edges rise upward and the nail plate takes on a concave shape, is called a spoon-shaped deformity and is a type of nail dystrophy, scientifically known as koilonychia. To some extent, the tendency to deformation is inherited, but for the most part, spoon-shaped nails are the result of injuries or occur as a result of common diseases.
Among the reasons:
illiterate pedicure; using low-quality nail polish containing acetone; long-term wearing of false nails and frequent extensions; thyroid diseases; Iron-deficiency anemia; infectious diseases. In fact, spoon-shaped nails do not cause physical suffering to a person, but psychological discomfort is obvious; deformation of nails is especially painful for women. Treatment consists of eliminating the traumatic factor, treating the underlying disease, taking vitamin and mineral supplements and medications that improve trophism in the nail bed.
Swelling of the legs is not always a sign of disease. In a completely healthy person, the legs may swell in hot weather, when overworked, walking or standing, but especially often people complain of swelling of the legs after prolonged sitting. If the situation requires constant sitting, for example, during work, car travel, air travel, swelling of the feet and ankles cannot be avoided.
When the legs are bent at a right angle and the thighs lie on the seat of the chair, the veins running along their back surface are compressed and the outflow of blood from the feet to the heart is disrupted. An increase in venous pressure leads to increased filtration of fluid outside the bloodstream into the surrounding tissues - swelling develops, a feeling of fullness and heaviness in the legs appears. As soon as venous blood flow is restored, pressure returns to normal, fluid returns from the tissues back into the blood vessels, swelling and discomfort disappear. Pathological swelling of the feet occurs with the following diseases:
heart failure; hypothyroidism; Varicose veins; pregnancy with gestosis; diseases of the urinary tract and kidneys (acute nephritis, glomerulonephritis, pyelonephritis)
Cold feet A feeling of cold and chilliness in the feet most often accompanies patients with vegetative-vascular dystonia. Violation of the tone of the autonomic nervous system towards the predominance of its sympathetic part leads to spasm of small blood vessels, paleness, coldness and sweating of the feet. In addition to the feet, most patients also have cold hands, the palms become damp and cold, the fingertips become numb, and the nails become bluish.
Cold legs are the result of poor blood circulation, which can be associated with obliterating endarteritis, varicose veins of the lower extremities, and heart disease. Often the cause is damage to small blood vessels in diabetes mellitus or diabetic angiopathy. Hypothyroidism or decreased thyroid function leads to a decrease in the intensity of metabolic processes, impaired thermoregulation and chilliness of the extremities.
Numbness of the feet Decreased skin sensitivity, numbness of the feet, and a crawling sensation in the legs may be the result of pathology of the regional nerve trunks or peripheral neuropathy. Its cause is most often diabetes mellitus and chronic alcohol intoxication. The disease cannot be cured; therapy involves the prescription of symptomatic medications.
Sudden numbness of a limb, weakness and heaviness in the leg, combined with the same sensations in the arm on the same side of the body, is a sign of cerebrovascular accident (stroke) and a signal to immediately call an ambulance. Numbness in the leg can persist after a stroke; it can be a sign of radicular syndrome, that is, pinching of part of the nerve fibers going to the limb from the spinal cord.
Lack of hair on the toes Hair loss on the toes can be caused by impaired peripheral circulation in diseases such as atherosclerosis, obliterating endarteritis, varicose veins of the lower extremities, diabetic angiopathy, chronic anemia, poisoning with certain substances, the use of antitumor chemotherapy drugs, and radiation exposure.
The most common cause of hair loss on the legs in men is obliterating endarteritis. The disease usually affects heavy smokers under 40 years of age and is accompanied by a decrease in the lumen and closure of the arteries of the lower extremities, which leads to tissue starvation and atrophy. Symptoms of the disease are chilliness and numbness of the legs, weakness in the leg muscles, pallor and dry skin.
Non-healing ulcer on the feet If every wound on the foot turns into a long-term non-healing ulcer, first of all, you should think about diabetes. The disease is accompanied by damage to blood vessels and nerve trunks, disruption of tissue nutrition, slowdown of regeneration processes, and high levels of glucose in the blood become an aggravating factor.
Diabetic foot ulcers are extremely difficult to treat and require a lot of patience from the patient and the skill, if not the “golden hands” of the doctor. Stabilizing blood glucose levels is of great importance. However, despite the high level of medicine, it must be noted that diabetic ulcers often lead to amputation of the foot. Patients with diabetes should pay special attention to foot care. Shoes should be comfortable, fit the size of the foot, and should not press or rub. Any callus or corns in the presence of diabetes threatens to turn into an ulcer. Trimming pedicures should be avoided and walking barefoot is not recommended.
Itching and burning of the feet Itching and burning in the area of the feet, redness and scaly peeling of the skin are most often caused by a fungal infection of the skin. The disease is often called “athlete’s foot”; it is easy to catch in locker rooms and showers in gyms and swimming pools. However, you can encounter fungus in the bathhouse, on the beach, and even at home if someone close to you suffers from fungal infections of the nails and skin.
Athlete's foot, as the fungus is scientifically called, begins with the appearance of a red, itchy patch on the skin. Growing into the epidermis, the fungus loosens it and leads to its necrosis and rejection, which is manifested by peeling. The skin of the feet appears whitish, covered with scales and red spots. The epidermis containing fungi that falls off lingers in shoes, socks, carpets, and the floor and becomes a source of infection for healthy people. Treatment of athlete's foot involves the use of antifungal agents; in most cases, topical application of creams and gels is possible, sometimes drugs are prescribed orally. To prevent athlete's foot, it is recommended to treat your feet with an antifungal agent every time after visiting public places.
Plantar Warts Plantar warts are hard, round growths on the sole of the foot. Most often they appear in the area of the fingers, initially single, then merging into large conglomerates. Warts are a viral skin disease. The pathogen penetrates the skin through cracks and wounds of the foot. The source of infection is a sick person; infection usually occurs in public places where it is customary to walk barefoot, for example, in a bathhouse or swimming pool.
You can deal with single warts yourself using an alcohol solution of salicylic acid, celandine juice, and antiviral drugs. With large formations, it is better to consult a dermatologist; they require cauterization, freezing, laser therapy or surgical removal.
source
Taken from: https://zdorowya.ru/blog/43618213616/O-chyom-mogut-rasskazat-nogi
Causes of a pinched nerve in the leg
A pinched nerve in the lower extremities can form due to the following factors:
- Osteochondrosis at the acute stage. Cartilage and discs, changing their shape, leave a small space that highlights the vertebrae. This has a positive effect on increasing compression in the area of the nerve branches. If we talk about muscles, then they, being in a much more active state and with increased tone, further aggravate the situation. Indeed, in connection with this, painful sensations turn out to be much more noticeable;
- Radiculitis. As you know, a large number of people over the age of 45 are faced with this disease. It is this disease that can cause a pinched nerve in the leg. The pain can be so severe that prolonged loss of consciousness is even possible. In this regard, at a critical moment it is necessary to reduce pain as soon as possible;
- Tumors of any origin;
- Loads that involve heavy or prolonged physical labor;
- Received injuries that change the optimal structure of the bones and thereby affect pinching.
Complex of medical procedures
There are two different approaches to treating plantar fibrosis. The choice of method depends on the neglect and complexity of a particular case.
Conservative treatment
The main point is the refusal of surgical intervention.
First of all, it is planned to significantly reduce the load on the feet and make their work easier. This approach is appropriate at the initial stages of the disease. If the help of a competent specialist was not received on time, then surgery becomes the only and mandatory way to solve the problem.
If the operation is impossible or undesirable for a number of reasons, then it is recommended to resort to conservative methods, which include the following set of procedures:
- use of comfortable shoes with soles without heels;
- wearing specialized orthopedic insoles;
- the use of devices that separate the fingers, which will eliminate the possibility of deformation of the fingers and foot as a whole;
- eliminating stress on the feet, so it is necessary to minimize the time spent in a standing position;
- It is recommended to use orthopedic shoes that correct the surface of the foot in accordance with individual characteristics;
- regular foot massage.
If you use this complex, the pain syndrome will disappear in a few months. Often conservative methods do not have the desired effect and the pain becomes more intense. In this case, it is advisable to use painkillers.
The following drugs are used to suppress pain:
Among the advantages of a conservative approach to the treatment of Morton's neuroma, it is worth highlighting:
- no recovery period;
- painful sensations that are typical in the postoperative period are excluded;
- treatment is carried out without disturbing the usual schedule, there is no need to change the existing rhythm of life, since there is no need to regularly visit the attending physician.
Among the disadvantages it is worth noting the following:
- duration of treatment;
- this method requires large financial investments in comparison with surgical ones;
- side effects from the use of various medications are possible, the functioning of the digestive tract and cardiovascular system is disrupted;
- the most important disadvantage is that there is no guarantee that the therapy will be successful.
Surgical approach
The operation is performed if conservative measures do not bring the desired result.
Three intervention techniques are used:
- normal removal;
- artificially performed bone fracture;
- removal of the inflamed area of the nerve and part of the muscle.
Among the advantages of prompt resolution, the following should be noted:
Place of incisions after surgery
- low cash costs;
- efficiency;
- long recovery;
- At first there will be discomfort while walking.
Treatment for a pinched nerve in the leg
First of all, when starting treatment, you should release the nerve endings or fibers from the compressed state. This is explained by the fact that it is this phenomenon that provokes pain in the leg area in case of a pinched nerve. In order to achieve the stated goal, specialists use manual therapy and some types of massage (in particular, acupressure, electric massage, vibration massage). Acupuncture and shock wave therapy are considered no less effective, which, however, are not recommended for people over 60 years of age. Additional recovery methods include osteopathy, magnetic therapy and electrical stimulation.
Etiological factors
- Staying in an uncomfortable position for a long time - the leg is pressed against a hard surface. The process develops due to impaired innervation and blood circulation in the leg area. Changing postures and physical activity restore blood circulation.
- The toes become numb due to the habit of sitting on a chair with one leg thrown back or tucked under. This position will cause varicose veins in the legs and groin area, which will worsen your appearance and affect your gait and normal functioning.
- Shoes that are inappropriate in size, instep, or thickness, with narrow toes or high heels. Being in it leads to compression of nerves and blood vessels, numbness and loss of sensitivity in the toes develops. If your toe goes numb after wearing a certain pair of shoes, stop wearing them. Buy high-quality orthopedic shoes that suit all parameters.
- Freezing or wet feet.
Causes and provoking factors
The anatomically correct relationship of the structures of the spine and pelvic bones with the lower extremities and muscular-ligamentous elements of the human skeleton eliminates the appearance of discomfort and limited movement in them. By a condition where the nerves in the leg are pinched, we mean deformations in the listed objects - traumatic, tumor or inflammatory in nature.
Directly depending on the location of the pathological focus - the level at which the muscle is pinched in the leg, doctors traditionally distinguish radicular syndrome, damage to the piriformis muscle, inflammation of the sciatic or greater tibial nerve.
Most often, people seek medical help due to injury - a direct blow to the body and legs, a car accident, or a fall from a height. The result of such a situation will be bone fractures, sprains/ruptures of the ligament or tendon apparatus. At the same time, a negative effect is exerted directly on the nerve fiber in the leg, or it is compressed by an internal hematoma.
No less often, specialists encounter pain in people in the leg area due to a pinched nerve by an inflammatory focus - in bone structures, soft tissues, or pelvic organs. Various infections and destructive processes over time and in the absence of treatment can result in impaired movement in the leg. Less commonly, such a result appears due to tumors - benign or malignant.
Provoking factors are:
- obesity;
- avitaminosis;
- excessive physical activity;
- heavy sports;
- incorrect posture;
- tight clothes, shoes.
Only a doctor can correlate the symptoms of a pinched nerve in the leg with possible causes. He also prescribes adequate treatment.
Features of neuritis of the lower extremities
What is neuritis
There are three types of nerve fibers:
The symptoms of mononeuritis are the same in any part of the leg - pain and numbness. In severe forms, tendon reflexes are lost. Muscle atrophy occurs at the site of nerve damage, but paralysis is practically excluded with local neuritis. An endemic form of neuritis is common among pregnant women, caused by a lack of B vitamins.
Neuritis is inflammatory damage to a peripheral nerve. If one nerve is inflamed, then they speak of mononeuritis, or local neuritis. When several nerves are affected, we are talking about polyneuritis.
Causes and localization
Doctors distinguish the following types of neuritis according to their location on the legs.
It is noticeable that neuritis is located mainly in the upper part of the legs - on the hips and in the pelvic area. But the nerves begin to inflame from afar, that is, from the feet. It’s just that the symptoms are not obvious, and there is no severe pain yet.
Muscle performance and blood circulation in the affected area of the legs are not immediately impaired.
Characteristics of polyneuritis
Polyneuritis is divided depending on the reasons that caused it.
Polyneuritis differs from neuritis in the severity of the patient’s general condition and the symmetrical distribution of symptoms in the legs.
Treatment of polyneuritis, neuritis and neuralgia
Therapy for these neurological diseases consists of eliminating the underlying disease that caused damage to the nerves of the legs. Treatment methods are chosen based on the stage of the disease. The success of treatment largely depends on starting it as early as possible. First of all, painkillers are used, anti-inflammatory drugs and drugs that accelerate metabolism in tissues are prescribed. Vasodilators and anticonvulsants are often used. In the acute stage, physiotherapeutic treatment is carried out: electrophoresis, UHF. There are no special medications that relieve inflammation in the nerves. Vitamin therapy, massage, and mud baths are used.
Of course, a healthy lifestyle, hardening, physical exercise, limiting contact with toxic substances is the prevention of any neurological diseases.
Angioneurosis is a disease of the vascular nerves
As angioneurosis progresses, attacks become more frequent, pain appears, and the lower extremities may turn blue and become blistered. At the critical stage of angioneurosis, the nail phalanges die. The causes of angioneurosis are the same factors as those of the previously discussed neurological diseases. These are intoxication with harmful substances and alcohol, infections, physical and mental injuries, frostbite of the extremities, hormonal disorders, finger injuries and vibration in industrial activities. This neurogenic disease is incurable and becomes chronic.
Neuritis, polyneuritis and angioneurosis often develop as a secondary disease. Therefore, it is so important to monitor your health, not to neglect the underlying disease and promptly treat neurological disorders. Take care of your nervous system!
https://nashinogi.ru/bolezni/nevrit-nizhnih-konechnostej.html
Symptoms
At the initial stage of its appearance, a pinched nerve in the leg resembles lumbago in its symptoms - limited movement and pain. However, the signs of a pathological disorder have a number of differences:
- passive movements allow you to lift your leg completely up - without reflexive resistance of muscle groups in the back;
- at night, discomfort does not decrease - a person constantly has a desire to change the position of his legs in space, to make them more comfortable;
- there is muscle weakness, and even a decrease in muscle volume - with a persistent chronic course of the disease;
- cramps appear in the calf muscles, in the foot;
- the pain syndrome does not depend on physical activity or the position of the body in space;
- after a few days, inflammation of the nerve in people leads to pins and needles in the legs, coldness of one area of the integumentary tissue;
- in the area of the joint closest to the lesion, not only sensitive, but also motor function is impaired - flexion, extension, abduction, for example, if a nerve is pinched in the knee.
In severe cases of pinched nerve in the knee joint, the symptoms will be so severe that the person may become disabled. He needs constant outside help and care.
Features of neuritis of the lower extremities
What is neuritis
There are three types of nerve fibers:
The symptoms of mononeuritis are the same in any part of the leg - pain and numbness. In severe forms, tendon reflexes are lost. Muscle atrophy occurs at the site of nerve damage, but paralysis is practically excluded with local neuritis. An endemic form of neuritis is common among pregnant women, caused by a lack of B vitamins.
Neuritis is inflammatory damage to a peripheral nerve. If one nerve is inflamed, then they speak of mononeuritis, or local neuritis. When several nerves are affected, we are talking about polyneuritis.
Causes and localization
Doctors distinguish the following types of neuritis according to their location on the legs.
It is noticeable that neuritis is located mainly in the upper part of the legs - on the hips and in the pelvic area. But the nerves begin to inflame from afar, that is, from the feet. It’s just that the symptoms are not obvious, and there is no severe pain yet.
Muscle performance and blood circulation in the affected area of the legs are not immediately impaired.
Characteristics of polyneuritis
Polyneuritis is divided depending on the reasons that caused it.
Polyneuritis differs from neuritis in the severity of the patient’s general condition and the symmetrical distribution of symptoms in the legs.
Treatment of polyneuritis, neuritis and neuralgia
Therapy for these neurological diseases consists of eliminating the underlying disease that caused damage to the nerves of the legs. Treatment methods are chosen based on the stage of the disease. The success of treatment largely depends on starting it as early as possible. First of all, painkillers are used, anti-inflammatory drugs and drugs that accelerate metabolism in tissues are prescribed. Vasodilators and anticonvulsants are often used. In the acute stage, physiotherapeutic treatment is carried out: electrophoresis, UHF. There are no special medications that relieve inflammation in the nerves. Vitamin therapy, massage, and mud baths are used.
Of course, a healthy lifestyle, hardening, physical exercise, limiting contact with toxic substances is the prevention of any neurological diseases.
Diagnostics
Undoubtedly, to identify pinched nerve fibers in the leg, an experienced specialist only needs to listen carefully to the patient and conduct a neurological examination. However, it is necessary for instrumental diagnostics to confirm this assumption.
Degenerative changes in the structures of the spine can be detected using standard radiography. The method is available for use in any clinic. If there is the slightest doubt about the accuracy of the diagnosis, the specialist recommends a computer or magnetic resonance imaging scan of the leg. There is more information - on many images in different projections, hard and soft tissues, choroid plexuses and the smallest nerve defects are more clearly visible.
The inflammatory process in the leg can be provoked by specific as well as nonspecific infections. The pathogen will be diagnosed by laboratory testing of the cerebrospinal fluid. The laboratory technician takes the liquid during a lumbar puncture with a thin needle - the puncture is performed directly between the vertebrae in the lumbar spine.
Pathological lesions of neuromuscular conduction can be traced using electroneuromyography. The graphic image will allow the doctor to determine the level at which the pinching occurred in the legs. A radioisotope scan will indicate the presence of a neoplasm in the area of the neurovascular bundle of the pelvis.
What symptoms are you worried about?
If a man or woman has pinched nerve fibers in the lower limb, the following signs will be of concern:
- acute, sharp pain in the thigh, lower leg, ankle or foot area,
- formation of edema, local increase in skin temperature,
- limited mobility of the limb, while walking it feels like the leg is shooting and jerking,
- spread of pain to the lumbar region,
- radicular syndrome develops, in which striped pain appears in the leg,
- increased sweating.
Treatment tactics
Of course, a specialist should decide what to do if the nerves in a limb are pinched. As a rule, this is a neurologist. He analyzes information from diagnostic procedures and selects the optimal treatment regimen individually.
Thanks to the rapid pace of development of the pharmacological industry, doctors have a wide range of medications in their arsenal that can make people feel better if they have a pinched nerve in their leg. They are presented in the pharmacy chain in different forms - capsules and tablets, pinching ointment or gels, injection solutions and aerosols.
Prevention
Already several hundred years ago, experts expressed their opinion that prevention of joint diseases is the best direction in their treatment. The relevance these days is somewhat no less. To prevent pinching of the nerve fiber in the leg, it is enough to follow simple rules:
- avoid physical activity;
- if it is necessary to carry a heavy thing, position the body and limbs correctly;
- buy comfortable, not fashionable shoes;
- keep your feet warm, especially in the autumn-winter period;
- promptly treat all chronic diseases and infections;
- Seek medical help at the first sign of a possible pinched nerve in your legs.
Early detection and comprehensive treatment of neurological pathologies is the key to quickly getting rid of them. Advances in medicine make it possible to combat infringement at any stage of its course. However, at an early stage there are fewer complications and a greater choice of treatment methods.
Source: nerv-info.ru
Source
Quite often, people begin to be bothered by first a dull, aching, and then a sharp, shooting pain in the leg area. Because of it, it is impossible to lead a normal life, sleep, or even just stand. A person begins to look for the causes of unpleasant sensations. Typically, a pinched nerve in the leg is the main cause of pain.
Recommendations for eliminating numbness of the limbs
If there is numbness in the limbs, the patient is advised to give up bad habits, in particular smoking. Nicotine is not only a poison that poisons the lungs, but also this substance causes vasospasm. Therefore, nicotine, alcohol, as well as strong black tea and coffee are strictly contraindicated for all those who suffer from numbness of the limbs.
Doctors also recommend changing your diet, namely focusing on hot dishes. Hardening the body, as well as constant movement and physical activity on the lower body are an indispensable aid for those who periodically experience loss of sensation in the limbs.
Traditional medicine recipes include taking contrast baths or showers, as well as warming your fingers with turpentine ointment. At night it is useful to make warming wraps using honey and camphor alcohol.
Why is a nerve pinched in the leg?
The unreasonable appearance of sharp pain in the leg is a signal: “The sciatic nerve has been pinched!” It begins in the sacral nerve plexus and stretches to the popliteal fossa, diverging there into many branches. Thanks to the sciatic nerve, a person moves his leg and also feels what is happening to it.
When a nerve is inflamed or pinched, the leg or back begins to hurt. The following factors contribute to the pathological condition:
- tumors;
- intervertebral hernia;
- injuries received;
- vertebral displacement;
- loads;
- osteochondrosis.
All the above reasons mainly relate to hip pain. Injuries, bruises, and constant stress on the limbs lead to pinched nerves in the knee joint. Also, the cause of pain is sometimes a meniscus tear, due to which the knee and lower leg may still swell.
Causes
A pinched nerve in the leg occurs under the influence of the following factors:
- Acute osteochondrosis. As the disease progresses, cartilage tissue and discs change their shape and location, as a result of which the nerves and muscles of the lower extremities can be pinched.
- Radiculitis. A common disease in older people, in which the roots of one of the spinal nerves become inflamed.
- Neoplasms of benign and malignant etiology.
- Excessive physical activity.
- Injuries, bruises, dislocations and subluxations. Incorrect location of the bone structures of the joint often causes a person to have a pinched nerve in the hip or ankle joint.
- Pregnancy. As the fetus and uterus increase in size, the sciatic nerve may become pinched and become inflamed.
Symptoms of a pinched nerve in the leg
The main symptom of a pinched nerve is sharp pain. It interferes not only with normal movement, but also with simply moving the leg. Painful sensations are especially aggravated at night, when the leg is at complete rest.
There are other symptoms that indicate problems associated with the sciatic nerve:
- swollen limb skin;
- redness at the pinched site;
- feeling of limb numbness;
- feeling of “running goosebumps”;
- inability to straighten the leg in the morning (occurs at an early stage);
- sharp or aching pain in the back.
These symptoms cannot be confused with signs of any other disease. Even with mild, dull pain, you should consult a doctor as soon as possible.
Morton's neuralgia - both feet hurt and toes “hum”
Morton's neuralgia (perineural plantar fibrosis) is a disease common throughout the civilized world.
It is accompanied by pain caused by unnatural compaction of the nerve of the foot. Most of the patients are representatives of the fairer sex. This is due to constant walking in long heels. Men are much less likely to go to the clinic with the corresponding symptoms. The source of the disease is located between the fourth and third toes. Despite this localization, the nerve is partially affected, on one side. Bilateral inflammation is extremely rare.
Diagnostics
To determine the nature of the pain and establish the cause of its occurrence, you need to know which doctor to see. A neurologist can make a diagnosis. He will also deal with the problem that has arisen.
To begin with, the doctor will prescribe an examination - an x-ray of the back. The resulting image shows the cause of the pain.
If radiography does not provide a complete picture of the disease, magnetic resonance or computed tomography is prescribed. Often this type of diagnosis reveals a tumor, which causes pain in the leg.
Only on the basis of the diagnosis does the doctor prescribe treatment for the patient. Often, a neurologist gives a referral to a chiropractor and prescribes a course of physical therapy.
Disease prevention
To prevent pinched nerves in the leg, you need to pay special attention to your health. It is necessary to walk more in the fresh air, and also follow simple recommendations:
- do gymnastics every morning;
- women should avoid walking in heels;
- spend less time in the cold;
- do not lift weights.
These tips will not get rid of the problem, but they will reduce the risk of pain recurring. Particular care should be taken when performing a complex of therapeutic exercises.