Aggravation is not yet a simulation, but already a norm of behavior
We talk about such a phenomenon as aggravation when the patient does not have any pathology at all - it is there, but it is much less expressed than the patient himself tries to present it to the doctor.
This is its fundamental difference from simulation, when the disease is completely absent and the patient is not one.
A striking example of aggravation can be a child showing an abrasion on his knee with such sorrowful emotions, as if we were talking about the end of his life. In this case, everything is clear: the child wants to be pitied.
A typical portrait of an aggravant
What does an adult aggravant want? About the same. After all, most often people who are lonely and helpless in life, who have no one to rely on, come to see a doctor with such greatly exaggerated complaints. Or having a family, but not finding support in it.
The portrait of a typical representative of this category in everyday life is as follows. This is a middle-aged woman with an unfulfilled destiny, usually childless. She is burdened with numerous problems with work and is ready to “cry into her vest” to the first person she manages to talk to.
It is extremely difficult to get rid of such a person, who is in no hurry to shut up and always finds new reasons to hold someone else’s attention for at least a few more minutes.
The face is very characteristic. These are sharpened features, mournfully pursed lips with downturned corners of the mouth and equally mournful, pleadingly waiting and at the same time empty eyes, as if for her everything had long been decided and finished. Moreover, it is not in her favor.
The movements of the arms express powerlessness; they often seem to fall limply and helplessly, although outwardly their development looks quite normal.
The manifestation of emotions in the course of presenting endless complaints or detailing one of them looks at the same time as carefully restrained, stingy and bashful, but at the same time methodical and unhurried. Even the pauses between phrases look like a continuation of complaints.
Behavior in a neuropsychiatrist's office is not very different from behavior in everyday life and leaves the impression that the patient has nowhere else to go and that she is ready to aggravate the rest of her life in the doctor's office.
Male aggravants look approximately the same and adhere to approximately the same line of behavior. Behavior dictated by the characteristics of a certain mentality.
Variety of reasons and types
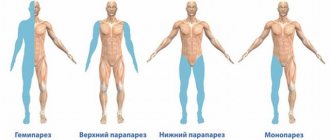
Actively contributing to the deterioration of one’s own health, or taking measures to delay recovery are classified as active aggravation behavior, while exaggerating the severity of the condition and the significance of individual symptoms is regarded as passive aggravation.
By type, aggravation disorders are divided into:
- subconscious;
- intentional;
- pathological.
The reasons for their occurrence fully or partially correspond to the category of disorder.
If the subconscious type is based on the existence of an actual somatic disease, then the intentional one is a certain line of behavior that implies gaining benefit or giving current events the desired outcome.
Pathological exaggeration of the severity of one’s condition is characteristic of mentally ill people or persons with mental states approaching psychopathology. That is, those suffering:
- hypochondria;
- iatrogeny;
- psychopathy;
- hysteria;
- anxiety-hypochondriac syndrome.
Drawing a strict line between subconscious and pathological aggravation is as difficult as assessing whether a patient is truly ill. Because the subconscious motivation in both options is the same - attracting attention, receiving sympathy and moral support.
On the aggravation of psychological and psychiatric disorders
In easily suggestible people with psychological disorders, increased suspiciousness leads to aggravation, forcing them to carefully examine their health indicators at home using all available methods in search of deviations from the norm. This could be measuring blood pressure and pulse, blood sugar, looking at the tongue in a mirror, or studying the surface of the skin.
And whoever searches will definitely find it. The next question is: what did self-inquiry give?
In search of an answer to this question, medical literature is methodically studied, television programs devoted to health are watched, or advice is sought from “those who know the truth” - fortune tellers and psychics. The information obtained contributes to even greater confidence in the seriousness of the existing symptom and the inevitable fatal outcome.
Conducted medical studies do not convince the patient of the insignificance of his disorder; on the contrary, they lead to the conviction that doctors are hiding something from him. Hence the insistence of demands to repeat the study, and to repeat it as thoroughly as possible.
Aggravations in psychiatric disorders are the conviction of a patient with a proven stable mental disorder in the mortal danger lurking behind the most harmless symptom. Thus, diarrhea repeated twice in a row can be regarded as a sign that, following the eruption of intestinal contents from the anus, the intestines will turn out, and then the entire body.
In psychiatric diseases, the patient’s attention can either be stubbornly focused on any one particularly disturbing symptom, or fixated on successively occurring conditions. The second category is more typical for elderly and senile people.
Aggravations in psychiatric disorders are divided into:
- meta-aggravation;
- super-aggravation;
- dissimulation.
The first option involves deliberately delaying the most acute stage of the disease, the second - complaints about symptoms that cannot exist in principle with a truly established disease.
Article on the topic: Which antibiotics for sinusitis are better and more effective?
Dissimulation is said to occur when there is an attempt to hide individual symptoms or the fact of exacerbation of psychopathology for one reason or another dictated by the disease.
To make a diagnosis
During a medical investigation of the fact of aggravation, the patient’s persistent arguments in favor of the presence of one or another symptom or syndrome are only taken into account, but the final judgment is made based on the analysis of objective data established by accurate research.
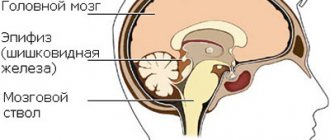
Including EEG, radiography with examination of cerebral vessels and other methods that allow assessing the level of cerebral blood supply.
If there is a pathological case, the patient is examined for mental disorder. In the case of a crime before the law, a forensic medical examination is carried out, and if necessary, the examination is carried out in a hospital setting. If the fact of pathological aggravation is identified and proven, the person is recognized as not responsible for his actions.
General approach to treatment
To apply the most rational and most gentle method of therapy, the type of aggravation disorder is taken into account.
And if in a deliberate case, the exposed pseudo-patient is liable before the law, then in the case of a subconscious disorder, methods from the arsenal of psychotherapy are used:
- hypnotherapy;
- auto-training;
- relaxation therapy and the like.
If necessary, drug therapy is prescribed, including the use of targeted and general action drugs:
- vasodilators;
- sedatives;
- nootropic;
- general strengthening.
It is rational to use exercise therapy, massage and similar methods that heal not only the patient’s psyche, but also his entire body.
Pathological aggravations that have a psychiatric basis are treated by doctors of the appropriate profile.
About the consequences
Considering the thin line separating a neurotic disorder from a serious mental pathology, which often develops into a psychiatric one, relatives and friends should draw the patient’s attention to the fact of increasingly frequent cases of aggravation. And then gently encourage him to take measures to eliminate the causes that cause it. Measures taken together with the patient.
Measures that do not allow the knot of fears and life problems to transmit every day the increasingly thinning intangible structure called the will to live.
Source: //med-anketa.ru/aggravaciya-esche-ne-simulyaciya-no-uzhe-norma-povedeniya/
LiveInternetLiveInternet
EspanaCuba
all posts by the author
V.Zh. Darbinyan, MD, Professor On May 10-12 of this year, the XI International Scientific and Practical Conference of the Ukrainian Antiepileptic League, dedicated to the optimization of diagnosis and treatment of epilepsy, was held on the basis of Europe's largest psychiatric hospital - psychoneurological hospital No. 1 in Kiev. in adults and children.
The conference was attended by epileptologists from different regions of our country, as well as authoritative scientists from neighboring countries. The relevance of the problem of epilepsy as a disease leading to social maladjustment and stigmatization of its victims is growing every year. According to statistics from developed countries, the frequency of this pathology in the population is 10-12 per 1 thousand population. In Ukraine, from 44 to 188 cases of epilepsy per 100 thousand population per year are registered annually, and this is only the tip of the iceberg: many patients are not even aware of their disease and do not receive treatment. Recent decades have been characterized by a significant expansion of diagnostic capabilities with the deciphering of a number of epileptic syndromes at the genetic level and fundamental research that has allowed us to take a fresh look at the phenomenon of pharmacoresistance, registered in 30% of patients. And yet, perhaps, the greatest success has been achieved in the development, study of the effectiveness and introduction of new antiepileptic drugs (AEDs). Thanks to them, most patients have the opportunity to remain full-fledged members of society, but recently the issue of tolerability of long-term pharmacotherapy for epilepsy, the relationship between medical and social benefits and side effects from taking AEDs has become acute. One of the leading epileptologists in Russia, Doctor of Medical Sciences, Professor V.Zh. Darbinyan (Department of Nervous Diseases, Institute of Advanced Studies, Moscow)
.
We present to your attention a brief overview of his speech. – The two most common questions asked to a doctor by patients newly diagnosed with epilepsy when prescribing therapy sound something like this: “Are you sure that taking medications on a regular basis will improve my condition?” and “How harmless is this to my health?” It should be said right away that there are no clear answers to them and it is unlikely that they will be found in the foreseeable future. But the doctor must learn to achieve and maintain a balance between the benefits and harms of AEDs for each individual patient throughout the entire period of treatment. How important is the need for long-term therapy, what do we save the patient from, how do we motivate him to take medications for many years?
– It should be remembered that the main risk that patients with epilepsy are exposed to is psychosocial maladaptation due to the inability to perform one or another type of work and a decrease in cognitive functions. The disease radically changes a person’s attitude towards life and society, as well as society’s attitude towards him. It is necessary to inform the patient about the increased risk of injury during seizures and about the possibility of fatal complications. Sudden death during a seizure occurs in 8-17% of cases, and in patients with poorly controlled disease - in 50% of cases. From 7 to 22% of patients with epilepsy commit suicide. This is already enough to convince the patient of the need for treatment. On the second side of the scale lies the effectiveness of AEDs. World statistics show that in 75% of all patients it is possible to achieve control over the occurrence of seizures, and with idiopathic epilepsy and adequate selection of drugs this figure reaches 85%. However, complete control, according to our data, is possible only in 42% of patients, good – in 28%, and in the remaining 30%, treatment results leave much to be desired. However, the benefits of epilepsy therapy are achievable in most cases. According to the results of a special survey of our patients, 62% of them who received adequate treatment with AEDs for an average of 8 years noted an increase in the quality of their life, which should be understood not only as a decrease in the frequency of seizures, but also as an improvement in psychosocial adaptation. It is necessary to prepare a new patient for the fact that initial therapy is successful only in 47% of cases, and the remaining percentage of failures is due to intolerance or ineffectiveness of the first drug. However, when switching to alternative AEDs, it is possible to achieve control over the course of epilepsy in almost half of the cases, so continuing the selection of drugs is advisable and necessary. The effectiveness of treatment largely depends on the adequacy of diagnosis. In special studies, depressing results were obtained: only in 16.7% of cases doctors know for sure that they are treating epilepsy, in the rest there are diagnostic errors due to incorrect classification and definition of the form of epilepsy, as well as ignoring differential diagnosis. In any case, the doctor must remember the situations in which the prescription of AEDs is not justified and further observation of the patient with differentiation of the convulsive syndrome is required: - the reactive nature of seizures (febrile seizures, withdrawal syndrome of neurotropic drugs) with confidence that they are not mixed (they do not occur); against the background of true epilepsy); – when the trigger factor is easy to avoid (drug withdrawal syndrome, “hot water” syndrome, photostimulated seizures); – the first seizure in the patient’s life; – seizures in persons who have undergone craniotomy, severe traumatic brain injury, meningitis, encephalitis (as a nonspecific reaction of the brain to its acute damage); – the first isolated unprovoked seizure (further search for the provoking factor is required); – lack of confidence in the epileptic nature of the paroxysm (it must be differentiated from convulsive syncope and other similar conditions); – patient’s refusal to take AEDs. The advisability of prolonging AED therapy after spontaneous or pharmacoinduced recovery of patients from the acute phase of self-limiting (age-related) forms of epilepsy remains debatable. These are occipital partial epilepsy in children, the manifestations of which, as a rule, disappear during puberty, benign neonatal seizures, generalized myoclonic seizures in infants and children, as well as some forms of absence epilepsy. Ultimately, even if the seizures recur, the amount of damage to the patient will be comparable both with the prescription of AEDs and with no therapy for several years.
What does the patient pay for the treatment effect?
– Each drug has its own characteristics of pharmacokinetics and pharmacodynamics, but if we summarize all the accumulated experience, the main complications of long-term therapy with AEDs are dose-dependent neurological side effects, effects on behavior and psyche, aggravation of seizures, metabolic and endocrine effects, idiosyncrasies, as well as complications caused by drug interactions.
The choice of a specific AED for a particular patient depends on many factors: • the effectiveness of the drug for different types of seizures; • range of side effects and drug interactions; • the speed of achieving therapeutic concentration in the blood and the onset of the antiepileptic effect; • reception frequencies; • the need for periodic laboratory monitoring to confirm the safety of therapy; • personal experience of using this AED from a doctor; • cost and availability of the drug on the market. Are there defining, main criteria for choosing PEP?
– There is no definite answer to this question.
Each of the above factors must be taken into account. Differences in the effectiveness of drugs when first prescribed in cases of newly diagnosed epilepsy remain controversial. The main pattern can be formulated as follows: in case of syndromes that are sensitive to treatment, a response to taking any AED will be observed, but in case of an initially resistant syndrome, such an effect cannot be achieved. About 37% of seizures in adults remain undiagnosed, and it is not possible to specifically prescribe a suitable AED. This leads to a logical conclusion about the advisability of prescribing drugs with the widest possible spectrum of action on various types of epileptic syndromes. At the very least, this will make it possible to smooth out the failures of initial treatment due to diagnostic inaccuracies. Which AEDs available in the modern arsenal meet the requirement of maximum broad spectrum of action with minimal side effects?
– Of course, valproate comes first; all other AEDs act either extremely selectively or cannot be prescribed for a long time due to pronounced dose-dependent side effects.
Only valproic acid has proven effectiveness against manifestations of the entire epileptic continuum: from absence seizures to simple partial seizures, providing acceptable tolerability of long-term therapy. Another risk factor in the initial treatment of epilepsy is the phenomenon of seizure aggravation, i.e., an increase in their frequency and severity after the administration of AEDs. In this context, it must be clarified that aggravation is not a patient feigning seizures or a side effect of anticonvulsant medications. First of all, myoclonus and absence seizures aggravate, which can cause an increase in generalized tonic-clonic seizures. Currently, EEG markers of aggravation are known, which make it possible to detect disinhibition of myoclonic and absence electrical activity of the brain even before the clinical manifestation of seizures. Aggravation of certain types of seizures is associated with various AEDs, but a cumulative analysis of the evidence base confirms that the minimal risk of aggravation of any types of seizures is observed when prescribing valproic acid, although if you are confident that the nature of the seizures is partial, it is rational to prescribe carbamazepine, which has a proven advantage over valproate in relation to the overall safety profile. Continuing the topic of the relationship between the safety and effectiveness of treatment, it should be noted that it can vary significantly depending on the choice of drug form. Thus, in some studies it was noted that even initial therapy with calcium valproate (Convulsofin) may be more effective compared to therapy with the sodium salt of valproic acid (G.G. Shanko, E.N. Ivashina, N.M. Charukhina, 2001). Our study examined the tolerability of various valproic acid preparations when initially prescribed for the treatment of epilepsy in 170 patients. Intolerance to Depakine Enterik was registered in 18% of patients, Depakine Chrono - in 9%, Konvulex - in 15%, and Konvulsofin - only in 4%. The study continued to replace the intolerable form of valproate with an alternative. As a result of switching from Depakine Enteric to Depakine Chrono, the effectiveness of treatment was 7%, to Convulex – 8%, to Convulsofin – 27%. When replacing the intolerable Konvulex with Depakin Enterik, success of therapy was noted in 4% of cases, with Depakin Chrono - in 7%, and with Convulsofin - in 41% (V. Darbinyan, I. Zhelambekov, 2007) These results convince us that if there is indications for the prescription of valproate and intolerance to the first prescribed drug, one should not immediately abandon this class of AEDs; in many cases, there is an alternative replacement option. The next question is the choice of AED dosage. Rapid dose increases may compromise the safety of some drugs that require slow titration in the eyes of the physician and patient. This applies primarily to carbamazepine, lamotrigine and tiagabine. In addition, you should always remember the individuality of dosages and the benefits of monitoring the concentration of the active substance in the patient’s blood. Should the dose be increased if the seizures are well controlled with the current treatment regimen?
– As part of our study, AED doses in the group of patients were increased based on the fact that 31% of them had good control, but insufficient drug concentrations in the blood.
This did not affect the prognosis, but the frequency of treatment intolerance increased when the dosage was increased by 20-25% and the theoretically optimal therapeutic concentration of AEDs was achieved. The drug had to be discontinued due to a significant increase in side effects in 11% of patients (V. Darbinyan et al., 2007). Another study examined the effects of doubling the daily dose of AEDs in patients with poor symptom control. A significant increase in the effectiveness of therapy was achieved by doubling the dose of carbamazepine, valproic acid and lamotrigine. In what cases should polytherapy be prescribed for epilepsy?
– First of all, if the previously considered options for optimizing monotherapy are ineffective, namely, primary therapy with drugs of choice with a wide spectrum of action, increasing their dose to the maximum tolerated, changing the form of the drug or replacing it with alternative second-line AEDs.
It is worth remembering situations in which the combination of AEDs is unjustified, since it does not improve seizure control compared to monotherapy: - refractory epilepsy when recovering from Lennox-Gastaut syndrome (in this case, polytherapy will only provide polyintolerance to the drugs); – progressive malignant temporal lobe epilepsy, when surgical treatment should be considered; – rare seizures that do not significantly bother the patient; – pregnancy and liver disease, when an additional AED may cause more harm than another seizure. Antagonistic or ineffective combinations of AEDs include: – valproic acid with phenobarbital; – valproic acid with phenytoin; – carbamazepine with lamotrigine; – carbamazepine with tiagabine; - phenobarbital with phenytoin. In some cases, a synergistic effect can be obtained by combining the following AEDs: – valproic acid with ethosuximide for myoclonus and absence seizures (provided that previous monotherapy with valproate is ineffective and this combination is tolerable); – valproate with carbamazepine for partial seizures; – valproate with lamotrigine (initially proven effective for myoclonus and absence seizures, but good results have already been obtained for partial syndromes). Thus, the choice of initial therapy for epilepsy seems to be a difficult task for the doctor, and the key to solving it is not universal, since it is necessary to take into account many factors depending on the characteristics of the AED and the clinical situation. Prepared by Dmitry Molchanov,
the article was published in issue 11/1 for June 2007, on pp. 26-27
Aggravation: symptoms and methods of correcting this condition – Suppressed
This is its fundamental difference from simulation, when the disease is completely absent and the patient is not one.
A striking example of aggravation can be a child showing an abrasion on his knee with such sorrowful emotions, as if we were talking about the end of his life. In this case, everything is clear: the child wants to be pitied.
Aggravation and simulation of mental disorders
Every attending physician, sooner or later, encounters a patient who exaggerates or invents the symptoms of the disease. This could be a student who doesn't want to go to school, a grandmother who is bored alone, or a person suffering from mental illness. How to distinguish imaginary diseases from real ones and simulation from aggravation?
Simulation or aggravation?
Aggravation and simulation are syndromes that are similar in their manifestation, but very different in the reasons for their development.
Simulation is the deliberate reproduction of certain symptoms of a disease. Absolutely healthy people with a specific (selfish) goal or people suffering from mental disorders can simulate. The main difference between malingerers is their rather caring attitude towards themselves and their health; they never do anything that could seriously harm it.
Aggravation is the intentional or unintentional exaggeration of the symptoms of a disease that a person feels or thinks he feels. Aggravants can deliberately harm themselves, not take medicine, or refuse treatment in order to worsen their condition.
The main difference between malingerers and aggravants is in their attitude to their condition and health.
The first ones know for sure that they are deceiving and they do not have this disease (at the same time, they may have other diseases that they do not complain about) and they always have a goal or benefit from such behavior (even if, at first glance, there is none , for example, in mentally ill patients, such Seconds are firmly convinced that they are sick, but little attention is paid to them and their main goal is to attract more attention to themselves, even if this means causing real harm to themselves.Sometimes aggravants also pursue selfish goals, but identifying their presence is much more difficult than with simulation.
Simulation
- Malingerers can be healthy people who deliberately feign illness for gain - deliberate malingering.
- Some malingerers reproduce symptoms for no apparent reason, as a result of psychiatric disorders - pathological malingering.
- Deliberate simulation of mental disorders is often found in psychiatric and judicial practice; it is resorted to in an attempt to avoid punishment, to obtain sick leave or exemption from military service.
RELATED MATERIALS: Why aggression appears in women
Simulation in children
In children, feigning illness can be caused by a desire not to attend an educational institution, as well as attempts to avoid punishment or to obtain some benefit.
Isolated cases of such behavior do not cause much concern, but if a child constantly feigns some kind of illness, it is imperative to understand the reason for such behavior. This may be caused by excessive strictness of parents, inflated expectations, mental characteristics of the child or neuropsychiatric disorders.
But no matter what causes the child’s behavior disorder, he definitely needs help, since in the future such a habit can cause neurosis or personality and behavior disorders.
Pathological simulation of mental disorders is observed in people with pathopsychology, who depict some kind of disease, while often concealing the existing symptoms of another, mental one.
Aggravation
Aggravation is a more difficult condition to diagnose, since the patient actually has certain signs of the disease, which can be confirmed by laboratory data, during examination, and so on.
The behavior of aggravation is characterized by peculiar symptoms, for example, people with neurosis, the elderly, patients with hypochondria, hysteria or some other pathologies suffer from it. They can be distinguished by demonstrative behavior, desire to attract attention, and so on.
Types and forms of aggravation
Subconscious - patients subconsciously try to attract attention to themselves, aggravating their condition, but at the same time, they sincerely consider themselves sick, requiring care and treatment.
Deliberate – patients deliberately exaggerate existing symptoms or consequences of injuries and diseases in order to obtain some benefit.
Pathological – occurs in mentally ill people, it can be both subconscious and intentional. Aggravation of mental disorders is often found in forensic psychiatric activities, when subjects deliberately aggravate their condition.
Passive and active aggravation:
- Active – patients deliberately worsen their condition and interfere with treatment.
- Passive - they exaggerate the manifestations of pathology, but do nothing to worsen the condition.
Source: //glpni.ru/lekapctva/aggravatsiya-simptomy-i-sposoby-korrektsii-takogo-sostoyaniya.html
Types of aggravation
Let's consider the classification of types of aggravation:
- Subconscious - when a person who is really sick speaks about the symptoms. A person aggravates to receive attention, care and support. Usually characteristic of hypochondriacs, hysterics, psychopaths, anxious and suspicious people who perceive absolutely any disease as fatal.
- Deliberate - when exaggeration occurs to obtain some benefit or outcome of events.
People of a sensitive nature should not read medical literature, communicate with sick people, or even just watch programs about diseases. Based on the information they receive, they begin to think that they themselves are sick. Headache occurs in almost any disease. As soon as a suspicious person feels a headache, he may think that he has the disease that causes it.
Deliberate aggravation is aimed at obtaining some benefit. It is divided into:
- Active – when a person deliberately delays the process of his recovery, for example, does not follow the doctor’s recommendations or takes pills that worsen his health. Often this behavior is criminally punishable if a person, by having an illness, tries to obtain material benefits from the state.
- Passive – when a person begins to talk about symptoms that are not characteristic of his disease.
To establish the true picture of health, the doctor resorts to diagnostic tests, which should show how sick a person is and whether he is sick at all.
go
Aggravation: causes, manifestations and treatment. Aggravation is not yet a simulation, but already a norm of behavior
The causes of aggravation can also be due to both the actual presence of the disease and the personal and motivational characteristics of the person.
Aggravation of mental disorders
Aggravation of mental disorders is understood as the deliberate exaggeration of one’s symptoms at the level of the psyche or physical manifestations, which is often found in forensic practice. The person begins to refer to symptoms that were previously present in him, but have now stopped.
Psychiatric aggravation is divided into types of manifestation:
- Metagravion is the deliberate prolongation of the acute phase of one’s illness.
- Overaggravation is a reference to symptoms that should not appear in the disease that is actually diagnosed.
- Dissimulation is the concealment of the disease and its symptoms.
When mental disorders become aggravated, a person begins to exaggerate existing symptoms that he previously experienced. He is really sick, but has already undergone treatment or his symptoms have been stopped, and therefore cannot manifest themselves in the form that the person refers to.
This type of aggravation occurs when a person, at the first manifestations of his disease, received the desired result (for example, he was given a mitigating sentence). Now that his illness should not manifest itself in a bright form, he resorts to aggravation in order to again obtain the result that was achieved last time.
go
Symptoms
Behavior is considered aggravative when:
- A person contributes to the deterioration of his condition and prolongs the period of illness (active form). The patient may not comply with the required regimen, fail to follow doctor’s orders, and even self-harm. You may have come across this form in your life, when an elderly person removes the bandage, throws away the pills, claiming that they “don’t help” or refuses to get up and move, causing stagnation in the body.
- A person exaggerates existing symptoms and increases the number of complaints. The usefulness and effectiveness of treatment is often downplayed, although the clinical picture of the disease suggests the opposite (passive form). This is often encountered by social service workers, when one ward may complain several times a day about high blood pressure in general, while increasing the number of complaints - symptoms (tinnitus, numbness, tingling, changes in consciousness, pain, changes in clarity of vision and hearing, lethargy, feelings of heaviness, etc.) and claiming that nothing helps him. Although at the same time, the external manifestations of his well-being indicate completely the opposite: the pressure has clearly stabilized.
If we consider such a concept as aggravation, then we should not confuse it with simulation. After all, simulation serves to obtain an obligatory and perceived benefit (avoiding punishment, for example). And there are really no symptoms.
Aggravation is associated with a person’s real experiences. And if we draw a brief conclusion, we can say that such a patient really “hurts,” but not as much as he presents it.
Unlike conscious simulation, aggravation is often not conscious or not fully realized and is a symptom of psychopathology.
Most often, aggravation accompanies people with hypochondriacal and hysterical accentuations, as well as anxious and suspicious individuals. Remember, there is probably a person among your friends for whom even the most “harmless sneeze” causes panic. Such a subject will not really exclude the possibility that he has pneumonia or, in general, tuberculosis.
Many suspicious people, reading medical reference books or listening to advertisements, “discover” symptoms of a huge number of diseases.
Aggravation can also develop as a result of psychological trauma and be of a neurotic nature. Many authors are convinced that the root cause or main driving factor is a person’s desire to attract attention and be surrounded by care, at least as a “sick person.” Let us repeat once again: this need is not always realized.
So, a woman who finds out that her husband is leaving her for someone else ends up in the hospital with a heart attack. In panic and under pressure from relatives and public opinion, the man remains in the family “until his wife recovers.” However, subconsciously such a patient does not want to recover, because then the worst thing in her life will happen.
Naturally, the disease becomes “protracted” in nature.
A similar situation unfolds even if the man leaves, but other close people remain around the sick woman: children, acquaintances. And the more people who want to sympathize, the more clearly aggravation can manifest itself.
Source: //probol.info/nevralgiya/aggravatsiya-prichiny-proyavleniya-i-lechenie-aggravatsiya-eshhe-ne-simulyatsiya-no-uzhe-norma-povedeniya.html
Aggravation
Aggravation is an exaggeration by the subject of the described severity of symptoms that actually exist or are subjectively felt.
Aggravation can be a consciously determined activity or have a subconscious nature of occurrence.
The reasons for the aggravation of painful symptoms can be determined both by the true presence of the disease and by the personal and motivational characteristics of the person.
Behavior is considered aggravative when a person contributes to the deterioration of his own health or prolongs the period of illness (active form, when non-compliance with doctor’s recommendations, self-mutilation is possible) or exaggerates existing symptoms (passive form, when the number of complaints increases).
Pathological malingering is manifested not only by the subject’s intensification of the symptoms of the existing disease, but also by downplaying the effect of the treatment provided, which may not coincide with objective indicators of improvement. This condition is considered a mental disorder and requires appropriate clinical diagnosis and psychotherapy.
Unlike conscious simulation, aggravation can act as a symptom or characteristic of the degree of progression of psychopathology.
What is aggravation?
The causes of aggravation of existing symptoms are mental disorders or deviations that accompany hypochondriacal and hysterical accentuations, as well as those inherent in older people with significant mental changes.
Also, this behavior can develop as a result of chronic psychological trauma (reminder by others of a defect, over-concern), and have a neurotic nature.
The difficulty in diagnosing this disorder lies in its initial and superficial similarity with simulation, however, simulation always has a selfish motivation, while aggravative actions are an unconscious manifestation of the hidden desires of the individual and contribute to receiving attention or care.
In the course of establishing the authenticity of mental status and forensic psychiatric examination, doctors and investigators are faced with such phenomena as simulation and aggravation.
To determine, coordinate and adjust further actions, as well as decide the fate of the subject, it is very important to distinguish one from the other.
Thus, simulation is a deliberate, conscious, often planned act of behavior aimed at deliberately simulating non-existent symptoms and manifestations of mental or somatic disorders, the purpose of which is most often to avoid judicial punishment.
There may be an intensification of aggravative behavior, both during the investigation and at critical moments of decisions on the future fate of those already convicted.
More often during simulation, simulated behavior with a description of anamnestic indications is used than directly acting out painful symptoms.
Determining the truth of the picture of complaints comes down to clinical research, observation of the subject and psychological examination.
Simulation and aggravation are different processes, although simulation against the background of the presence of pathological disorders of the psychiatric register is aggravation.
Types of aggravation. It can be subconscious (inherent in a sick person), intentional (in order to obtain a benefit or a necessary outcome of events) and pathological (in mentally ill people). The subconscious has a person’s desire to receive sympathy and support.
It is often found in patients with a hysterical, hypochondriacal and psychopathic type of accentuation, anxious and suspicious individuals who monitor their health parameters very carefully and any illness is immediately considered serious, painful sensations are exaggerated.
https://www.youtube.com/watch?v=NkHLEpJaupQ
The reasons for aggravation for suggestible people are in reading medical literature and attributing diseases to themselves, in careless statements by a doctor or any representative of the medical staff.
Deliberate aggravation is motivated by profit.
It is divided into active (when the patient himself delays recovery or independently worsens his condition) and passive (exaggeration of symptoms, complaints about other phenomena not characteristic of this disease) forms.
When deliberately exaggerating the symptoms of a disease, aggravative behavior is criminally punishable if used for illegal purposes (receiving insurance payments, exemption from the army, etc.).
When the need arises to establish the fact of aggravation, the doctor or bailiff primarily focuses on objective data from examining the patient, obtaining the necessary tests, and not on his subjective descriptions of his well-being.
Pathological aggravation is considered from the perspective of aggravation of mental disorders.
Aggravation of mental disorders
Pathological aggravation implies an exaggeration of the symptoms of somatic and psycho-emotional illnesses in mentally ill people. It is a fairly common phenomenon in forensic psychiatric activities, occurring in the form of deliberate complaints about symptoms that were previously inherent and characterized the disease, but have now been stopped.
Psychiatric aggravation is divided into three main types of manifestation: meta-aggravation, super-aggravation and dissimulation. With meta-aggravation, a person deliberately seeks to prolong the most acute phase of the disease (depression, build-up of affective arousal).
Over-aggravation implies complaints about symptoms that are excluded in the case of a really diagnosable disease (intellectual-mnestic disorders in schizophrenia).
Dissimulation is the concealment of the disease or its manifestations, which are determined by the disease and the characteristics of its course (with exacerbation of schizophrenia and psychotic states, a person is not able to assess his condition himself, and the motives dictated by the disease require concealment of all symptoms).
Pathological aggravation carries symptoms that are preserved in memory from actually previously existing or retained residual manifestations of mental disorders.
Most often it occurs when mental illnesses are based on an organic nature (head injuries, vascular and hereditary diseases, mental retardation).
The most common exaggeration of intellectual failure, problems in the mnestic sphere, headaches, loss of orientation in society, and depressive manifestations.
Aggravation becomes a habitual form of behavioral patterns when the first aggravative behavior led to a successful resolution of the situation or acts as a standard reaction of a changed personality in critical situations.
This response mechanism is consolidated and may further reflect the depth and severity of mental damage (thus, with a decrease in the intellectual-mnestic sphere, aggravative behavior begins to look more and more grotesque and ridiculous).
The form and degree of manifestation of aggravation serves as a way to assess the severity of mental disorders, the degree and rate of progression of the disease. The more primitive, crude, and absurd the manifestations of aggravation, the greater the degree of mental disorder we can speak of.
Aggravation therapy includes drug therapy for the underlying disease and psychotherapy. The main goal of psychotherapy will be to search for hidden motives, human needs and bring them into the realm of consciousness, and at subsequent stages, search for various socially acceptable, relevant and appropriate ways to satisfy the identified requests.
Author : Practical psychologist Vedmesh N.A.
Speaker of the Medical-Psychological
Source: https://psihomed.com/aggravatsiya/
Aggravation and simulation of mental disorders
Every attending physician, sooner or later, encounters a patient who exaggerates or invents the symptoms of the disease. This could be a student who doesn't want to go to school, a grandmother who is bored alone, or a person suffering from mental illness. How to distinguish imaginary diseases from real ones and simulation from aggravation?
Manifestations
Most often, patients choose to simulate diseases and symptoms that do not require much effort to depict: delusional disorders, hallucinations, memory impairment, and so on.
Patients with actual illnesses usually depict the most “colorful” manifestations of their illness. Thus, aggravation of epilepsy, reactive psychosis, memory disorder, and so on is common.
At the same time, aggravation of seizures can be accompanied by real damage: patients “in a seizure” injure themselves, bite their tongues, or deliberately “bring” themselves to an attack.
Diagnosis and treatment
Diagnosing these syndromes is quite difficult.
When simulating, laboratory tests and other diagnostic research methods that indicate the absence of pathology help to make a correct diagnosis.
In case of aggravation, such diagnostic methods often turn out to be ineffective, since the symptoms are really present, and the severity of the patient’s condition is quite difficult to assess.
The main difference between the symptoms of aggravation and simulation from the true disease:
- Contrast between the number of complaints and their visible manifestations.
- Insufficient symptoms - almost all diseases have a complex of symptoms that imaginary patients cannot imitate.
- The presence of symptoms of mental disorders and demonstrative behavior in the subject.
- Abnormal response to treatment or lack thereof.
- Constant discrepancies in medical history and complaints
To diagnose aggravation and simulation of mental disorders in psychiatry, a medical consultation is used, which can confirm or refute the diagnosis.
How to distinguish imaginary diseases from real ones and simulation from aggravation
Aggressive behavior in humans can be caused by a variety of reasons.
- abuse of alcohol, as well as drugs that weaken the nervous system, which provokes the development of an aggressive, inadequate reaction to minor situations;
- problems of a personal nature, unsettled personal life (lack of a life partner, a feeling of loneliness, intimate problems that cause depression, and later turn into an aggressive state and manifest themselves at every mention of the problem);
- mental trauma received in childhood (neurosis received in childhood due to poor parental relations);
- strict upbringing provokes future manifestations of aggressiveness towards children;
- passion for watching quest games and thrillers;
- overwork, refusal to rest.
Aggressive behavior is observed in a number of mental and nervous disorders. This condition is observed in patients with epilepsy, schizophrenia, due to injuries and organic lesions of the brain, meningitis, encephalitis, psychosomatic disorders, neurasthenia, epileptoid psychopathy.
The causes of aggression are subjective factors (customs, revenge, historical memory, extremism, fanaticism of some religious movements, the image of a strong person introduced through the media, and even the psychological individual traits of politicians).
There is a misconception that aggressive behavior is more characteristic of people with mental illness.
There is evidence that only 12% of people who committed aggressive acts and were referred for a forensic psychiatric examination were diagnosed with mental illness.
In half of the cases, aggressive behavior was a manifestation of psychosis, and the rest had inappropriate aggressive reactions. In fact, in all cases there is an exaggerated reaction to circumstances.
Observation of teenagers has shown that television perpetuates an aggressive state through crime programs, which further enhances the effect. Sociologists, such as Carolyn Wood Sheriff, challenge the popular belief that sports act as ersatz war without bloodshed.
Long-term observations of teenagers at a summer camp showed that sports competitions not only do not reduce mutual aggressiveness, but only intensify it. An interesting fact was discovered about the removal of aggressiveness in adolescents. Working together in the camp not only united the teenagers, but also helped relieve mutual aggressive tension.
Let's go to Airbnb
Getting closer to a "real world example", here's the problem we'll try to solve - Airbnb Home Search.
How can we quickly search for houses based on some query with many filters? This is a difficult task. It becomes more difficult when you consider that Airbnb maintains 4 million listings.
So, when users search for houses, there is a chance that they can “touch” the 4 million records stored in the database. Of course, the results are limited to the "top listings" shown on the site's home page, and a user is almost never too curious to sift through millions of listings. Let's assume that the user finds a good house after viewing no more than 1000 offers.
The most important factor here is the number of users online, because... This affects the data structures, the choice of database and the architecture of the project as a whole. Obviously, if we only have 100 users, we don't have to worry about this at all.
If the number of online users exceeds a million, we must think through every decision in the project. This is why companies hire the best talent, striving for excellence in service delivery.
Google, Facebook, Airbnb, Netflix, Amazon, Twitter and many others deal with massive amounts of data, and doing the right thing to serve millions of bytes of data every second starts with hiring good engineers. All these companies need is an engineer who can solve problems in the fastest and most efficient way.
So here's a classic example. The user visits the home page (we're still talking about Airbnb) and tries to filter through all the offers to find the best match. How would we deal with this problem?