Prognosis and outcomes of the disease
The causative agent of the disease is the bacterium Neisseria meningitis, which is divided into 13 groups according to its properties. The disease in humans is most often caused by groups A, B, C, Y. In the winter-spring period, the pathology is mainly caused by group A, in the off-season - by group B.
- Meningococcus is a bacterium that requires the presence of oxygen in the tissue to grow. The optimal temperature for it is 36-37°. The main toxic substance is released when this bacterium dies.
Meningococcus is unstable in the external environment. He dies:
- at 50°C – in 5 minutes;
- in direct sunlight - 2-8 hours;
- at -10°C – 2 hours;
- when boiling – in 30 seconds;
- under the influence of UV rays - instantly;
- when treated with disinfectants - very quickly;
- On linen at room temperature it can live for about 12 hours.
The patient is contagious as long as meningococcus is detected in his nasopharynx. In healthy carriers and patients with nasopharyngitis, the bacterium disappears on its own after 2-4 weeks, and throughout this period such a person is dangerous to his colleagues and loved ones, especially children. In generalized forms, the period of infectivity is very short due to early treatment with antibiotics.
There are 2 types of forms of the disease: localized and generalized. The first include: carriage, nasopharyngitis. The second: meningococcemia (circulation of bacteria in the patient’s blood), meningitis, meningoencephalitis.
Meningococcal infection in children can penetrate the body from a carrier (provided they stay within 0.5 m of an infected person for a long time). Some adults may not be aware of their condition, since some forms of the disease have no symptoms and can transmit meningococci to a child through close contact (talking, coughing, sneezing).
The following factors can increase the likelihood of children contracting this infection:
- severe weakening of the child’s immune system;
- age up to 1 year;
- malignant tumor processes;
- frequent long-term contact with an infected person;
- side effects of medication administration;
- neurosurgical intervention;
- history of traumatic brain injury.
Meningococcal infection in children, the symptoms of which are acute, has a favorable prognosis, subject to timely detection and treatment of the disease. However, when complications occur after meningitis, the outcome is most often poor. The prognosis for children depends on the age and form of the disease (in the younger age category the likelihood of death increases).
Untimely treatment of meningitis can provoke the development of deafness, blindness, epileptic syndrome, and in children - the formation of hydrocephalus, delayed development, and asthenic syndrome. Without treatment for meningococcemia, the mortality rate is 100 percent.
Meningococcus is transmitted by airborne droplets. You can become infected through close and prolonged contact with a sick person. The danger is that many sick people do not know about the presence of bacteria in their body, since the infection does not manifest itself in any way at the initial stage, but they are carriers of meningococcus. Accordingly, such people do not stop close contact with others and do not isolate themselves, exposing them to the risk of infection, in particular children.
Factors provoking the development of the disease:
- age up to 1 year;
- weak immune system;
- long contact indoors with a carrier of infection.
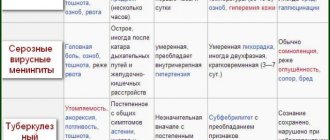
Viral meningitis in children is more common than other forms. Viruses are the causes of meningitis:
- enteroviruses, including Coxsackie;
- influenza viruses, chickenpox, shingles;
- arboviruses, including encephalitis virus,
- herpes viruses types 1 and 2;
- mumps virus;
- cytomegalovirus.
Bacterial meningitis in children and adults is caused by:
- meningococcus;
- Pneumococcus;
- staphylococcus;
- listeria (with weak immunity and in the elderly);
- tuberculosis bacillus (causes secondary meningitis);
- E. coli (a common cause of meningitis in newborns);
- Haemophilus influenzae.
Spirochetes that cause meningitis are:
- Treponema pallidum, which causes syphilis;
- Borrelia, which causes Lyme disease;
- Leptospira.
Meningococcal infection: what you need to know to protect yourself and your loved ones
In January 2020, the World Health Organization recognized vaccine refusal as one of the main global threats to humanity1. WHO experts explain that vaccination is one of the ways to combat diseases, which can prevent up to 3 million deaths annually. Another 1.5 million lives could be saved1 if more people were vaccinated. Refusal of vaccinations negates the progress that has been made in the fight against various infections.
What is meningococcal infection and how common is it?
The infection, caused by the bacterium Neisseria meningitidis, is transmitted only from person to person. Infection occurs through airborne droplets upon contact with an infected person. For example, while sneezing, coughing, kissing, or using shared utensils.
For many years, the incidence of meningococcal infection in Russia has been declining2, but since 2020 its increase has been observed: in 2018, the incidence was 0.7 per 100 thousand population, which is 40% more than in 2020, when a historic minimum. In 2020, the increase in incidence continued3, with the number of cases increasing by another 16%.
How to recognize meningococcal infection?
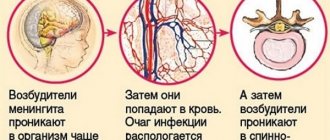
The incubation period of meningococcal infection4 ranges from 2 to 10 days. After entering the body, bacteria begin to multiply on the mucous membranes of the upper respiratory tract - in the nasopharynx. This process can be asymptomatic, or accompanied by nasopharyngitis and its characteristic symptoms - redness of the mucous membrane, runny nose, swelling, pain and sore throat, and sometimes fever.
Bacteria can enter the blood and spread throughout the body through blood vessels, causing meningococcemia - meningococcal sepsis, which affects various human organs. When bacteria cross the blood-brain barrier and enter the brain, meningococcal meningitis occurs. Both of these conditions can develop rapidly and be fatal.
The progression of meningococcemia is accompanied by high (up to 40 degrees) temperature, chills develop, pulse quickens, and blood pressure drops. Another alarming symptom is a dark rash covering the entire body that does not disappear with strong pressure on the skin.
Characteristic signs of meningitis include stiffness (severe tension) of the neck muscles, which makes it impossible to press the head to the chest. There is also a headache, often convulsions, which are usually found in children, as well as vomiting and disturbances of consciousness.
Symptoms of meningococcal meningitis in children also include high fever, photophobia, vomiting that does not bring relief, and headache, which can be recognized by high-pitched crying.
What is the danger of infection and how is it treated?
Meningococcal infection is treated with antibiotics4. Therapy must be started immediately, as the patient’s condition is rapidly deteriorating. Unfortunately, even timely treatment does not always help save lives. Even if treatment is started on time, every fifth patient dies2. If left untreated, in 50% of cases the disease ends5 in death.
Approximately every fifth6 patient who has recovered from meningococcal infection continues to have consequences of the disease that significantly change the quality of life and even lead to disability, for example, hearing loss and brain damage. In place of the rash elements, ulcers and necrotic elements may appear, which can lead to gangrene of the fingers and toes and subsequent amputation.
Who is at risk?
People at risk for meningococcal infection include7:
- children under 5 years of age;
- teenagers from 13 to 17 years old;
- people over 60 years of age;
- conscripts;
- people living in dormitories;
- health workers of infectious diseases departments;
- specialists who work with live culture of meningococcus;
- people traveling to areas where meningococcal infection is endemic;
- staff and pupils of social institutions with round-the-clock stay;
- participants in mass international sports and cultural events;
- patients who have undergone cochlear implantation;
- patients with liquorrhea;
- patients with primary and secondary immunodeficiency conditions.
One of the ways to prevent meningococcal infection is vaccination. In Russia, vaccination against meningococcal infection is not included in the National Calendar, but is included in the calendar of vaccinations that are given for epidemic indications.
The Ministry of Health is considering the possibility of expanding the National Preventive Vaccination Calendar8 and, perhaps, soon it will be possible to get vaccinated against meningococcus in a regular clinic.
Does vaccination cause autism?
One of the arguments that makes parents refuse or fear vaccination is the fear of vaccine-induced autism. Talk about a possible connection began about 20 years ago, when a publication by a team of scientists led by Andrew Wakefield appeared in the Lancet. The authors of the article argued that there is a connection between autism and vaccines that protect against measles, mumps and rubella.
The study9 found inaccuracies and facts indicating data fraud; other research groups were unable to repeat the results. Wakefield's article was retracted, and he himself was deprived of the right to practice medicine.
Two decades have passed since the publication, and a large body of scientific research has now accumulated10,11,12, the results of which indicate that vaccines do not cause autism.
THE INFORMATION PRESENTED DOES NOT REPLACE CONSULTATION WITH A SPECIALIST, CONSULT YOUR DOCTOR
Notes
1 WHO report “10 global health threats”
2 State report “On the state of sanitary and epidemiological well-being of the population in the Russian Federation in 2020”
3 Comparison of infectious disease indicators in the Central Federal District according to NGO Krista
4Meningococcal infection. Clinical recommendations of the Ministry of Health of the Russian Federation. Electronic resource https://cr.rosminzdrav.ru/#! /schema/892 (as of 06/29/2020)
5Meningococcal meningitis. WHO. Electronic resource https://www.who.int/ru/news-room/fact-sheets/detail/meningococcal-meningitis (as of June 29, 2020)
6Meningococcal infection: diagnosis, treatment and consequences. Electronic resource https://www.cdc.gov/meningococcal/about/diagnosis-treatment.html#complications (as of June 29, 2020)
7Prevention of meningococcal infection. Sanitary regulations SP.3.1.3542-18 dated December 20, 2018. Electronic resource https://docs.cntd.ru/document/552061091 (as of June 29, 2020)
8National calendar of preventive vaccinations. Appendix No. 1 to the order of the Ministry of Health of the Russian Federation dated March 21, 2014 No. 125n
9Publication in the Lancet RETRACTED: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Electronic resource https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(97)11096-0/fulltext (as of June 29, 2020)
10Report from the Centers for Disease Control and Prevention. Vaccines Do Not Cause Autism Electronic resource: https://www.cdc.gov/vaccinesafety/concerns/autism.html (as of June 29, 2020)
11Research by Jeffrey S. Gerber and Paul A. Offit Vaccines and Autism: A Tale of Shifting Hypotheses Electronic resource https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2908388/ (as of 06/29/2020)
12Report of the National Capital Poison Center Vaccines Do Not Cause Autism Electronic resource https://www.poison.org/articles/2010-oct/vaccines-do-not-cause-autism (as of June 29, 2020)
The material was prepared jointly with the French pharmaceutical company, which is engaged in scientific research, production of medicines and vaccines, including in Russia. Learn more about the company with more than 100,000 employees worldwide here.
Representative office of Sanofi-aventis Group JSC (France). 125009, Moscow, st. Tverskaya, 22. Tel.: (495) 721-14-00, fax www.sanofi.ru. SPRU.MENAC.20.05.0128
Features in children
- Most often, generalized forms are preceded by meningococcal nasopharyngitis.
- Carriage of the bacterium is not observed in children 0-3 years of age.
- Meningococcal infection can be transmitted in utero. In this case, the child usually does not die, but is born with hydrocephalus.
- Nasopharyngitis in children 0-3 years old is characterized by severe runny nose with the release of mucopurulent discharge.
- In children under 3 years of age, generalized forms most often develop, while up to 1 year of age they are often complicated by shock.
- In infants, meningitis caused by meningococcus begins and progresses quickly: the temperature rises sharply, the child becomes lethargic (sometimes restless), he screams and cries, resists being picked up, and a large fontanelle bulges. Children often experience convulsions, breathing problems, and hand tremors.
Diagnostics
Meningococcal infection can be suspected based on clinical manifestations, characteristic rash, and results of a cerebrospinal fluid analysis.
It is possible to say for sure that this particular infection is taking place by bacteriological analysis of blood, cerebrospinal fluid and nasopharyngeal swabs, carried out on specific media in which Neisseria meningitidis is detected.
In some cases, PCR testing of the cerebrospinal fluid or blood helps to establish the diagnosis (this is very important if the puncture was done after the start of antibiotic therapy), where Neisseria DNA is detected.
When to seek help for meningococcal infection
Don't wait—take action right away if your child has one or more of the symptoms of meningococcal disease. So what to do:
- Act now
- Call the hospital/ambulance at any time of the day
- Describe your symptoms to medical staff
- Insist on immediate action, any delay could endanger the child’s life
- Monitor your child even if he or she has already been seen by a doctor. Ask your doctor what to watch for
- Go to the doctor if your child gets worse
- Don't leave your child alone
Symptoms of the initial stage
Manifestations of the disease differ depending on the form of infection, which can be local or general. General signs of the disease that appear with nosopharyngitis:
- sore throat;
- redness of the throat;
- dry cough;
- nasal congestion;
- headache;
- conjunctivitis;
- slight increase in body temperature (up to 37.5 degrees).
This form of meningococcus is treated until complete recovery within 1 week. Sometimes it can provoke the development of more dangerous types of disease, for example, when an infection enters the blood or damages the central nervous system.
Main features:
- nausea and vomiting;
- diarrhea;
- a sharp increase in body temperature;
- dry mouth mucous membranes;
- rash.
The nature of the appearance of the rash (see photo) indicates the severity of the disease: the earlier the spots appeared, the more difficult the treatment. Most often, the rash is detected on the first or second day on the thighs, abdomen, and buttocks. If spots cover the face, it means that the disease is in severe forms. The size and color of the rash can vary from small pink spots to large purple elements.
Meningococcal rash is different in that it does not disappear with pressure. This is explained by the fact that it appears due to hemorrhage into the skin. The spots last for 3–4 days and then disappear.
The rash is dangerous due to the formation of necrosis - this is the death of tissue that develops in the middle of large spots. In their place, a dense crust forms, and then ulcers. Necrosis affects the phalanges of the fingers, nose and ears.
Dangerous symptoms requiring emergency care:
- nosebleeds;
- hemorrhages in vital organs;
- damage to the kidneys, heart, lungs;
- shortness of breath;
- cardiopalmus;
- decreased blood pressure;
- change in urine color;
- joint pain and swelling;
- decrease in body temperature below normal;
- renal failure.
The appearance of these symptoms indicates the development of a severe form of meningococcal infection - meningococcemia. Failure to provide assistance in a timely manner can lead to the death of the child. Bacteria develop rapidly, so it is important to show your baby to the doctor as soon as dangerous manifestations are discovered.
The development of a purulent inflammatory process (see photo) is characterized by the following signs:
- incessant crying;
- severe anxiety and irritability;
- fever, chills (temperature does not decrease after taking antipyretic drugs);
- lack of appetite;
- diarrhea, nausea, vomiting;
- confusion;
- increased muscle tone;
- convulsions;
- headache;
- lethargy;
- pallor of the skin.
Meningococcal infection in children, the symptoms of which develop quickly, has an incubation period of several days; in adults it increases several times (from 2 days to 1.5 weeks). Localized forms of the disease are usually asymptomatic or may be mild. Generalized ones, in turn, develop rapidly (within 1–2 days after infection).
Clinical signs of the initial stage of the inflammatory process include:
- A rapid increase in body temperature to 38 - 39.5 degrees, which is quite difficult to reduce with antipyretic drugs.
- Intense bursting headache, which intensifies when turning the head. The patient's condition can be alleviated by adopting a horizontal position. In this case, double vision may occur in the visual organ.
- Severe feeling of nausea, which may result in vomiting. This symptom is not related to eating. In this case, antiemetic medications are powerless.
- You may experience pain in the back of your neck when you place your knees near your stomach.
- The patient is forced to take a characteristic position in the form of a slightly thrown back head.
- In addition, the patient develops aversion to light and increased pain in the head when loud sounds appear. Being in a quiet, dark room can alleviate the condition.
- A rash forms on the skin and quickly spreads throughout the body. This symptom is considered the most unfavorable and requires immediate hospitalization.
Symptoms of meningococcal nasopharyngitis manifest as:
- increase in body temperature (no more than 38 degrees);
- general weakness of the body;
- nasal congestion;
- pain in the throat when swallowing;
- runny nose with small amounts of mucus;
- drying of the mucous membrane of the nasopharynx.
Similar clinical signs also occur when a cold occurs, so when they appear, most people rarely turn to a doctor for help, which is extremely wrong. Lack of timely treatment of meningococcal nasopharyngitis leads to severe consequences, in some cases to death.
When meningitis develops, the following symptoms occur:
- rapid increase in body temperature;
- nausea followed by vomiting;
- intense headache that cannot be eliminated with medications;
- impaired consciousness;
- increased sensitivity to environmental stimuli;
- indigestion;
- convulsions.
Symptoms may vary depending on the individual characteristics of the patient and susceptibility to infections.
Severe development of meningococcal infection is characterized by the following complications:
- rapid heartbeat;
- sharp decrease in blood pressure;
- seizures;
- dysfunction of all organs;
- damage to the auditory nerves;
- epileptic syndrome;
- paralysis;
- brain abscess;
- confusion;
- coma.
To avoid such negative consequences for the patient’s health, it is necessary to carry out appropriate treatment in a timely manner. To a greater extent, the development of symptoms is influenced by the individual characteristics of the child’s body and its reaction to the spread of infections. The disease has the most unfavorable course in young children and premature infants.
Symptoms of meningococcal infection in children
Signs of meningococcal infection, which occurs in the form of nasopharyngitis in adults and children, will not differ from the symptoms of ARVI. The incubation period of the disease ranges from two to ten days (most often two to three days).
The disease begins with symptoms of general intoxication, high fever, chills, and muscle weakness. Then there are complaints of nasal congestion, pain and a sore throat.
The development of bright hyperemia and swelling of the PSG (posterior wall of the pharynx) is characteristic.
There is an increase in regional lymph nodes and tonsils.
The only sign, besides indicating a history of contact with a patient, that allows one to suspect the meningococcal nature of nasopharyngitis is the bluish tint of FSG.
The diagnosis is made only with bacteriological confirmation of the meningococcal nature of nasopharyngitis.
Meningococcal meningitis and meningococcemia
The main symptoms of a generalized course of infection will be a combination of:
- high fever;
- vomiting;
- intense headaches;
- photophobia;
- development of meningeal signs (stiff neck, Kerning, Brudzinski symptoms, etc.).
A rash with meningococcal infection is characteristic of the addition of meninococcemia.
Rashes with a generalized course of infection are pethial (hemorrhagic) in nature. Their number can vary from single elements to the appearance of confluent foci of purple-bluish color. The shape of the rash is star-shaped and irregular. The main clusters of rashes are located on the buttocks and thighs. In severe cases, it may spread to the legs, torso and arms. The rash is extremely rarely localized on the face and serves as an unfavorable prognostic sign.
Read further: Symptoms of meningitis in an adult, first signs, diagnosis and treatment
Signs of meningococcal infections in adults and children:
Signs of meningitis
Photo of meningococcal infection in children with fulminant meningococcemia
Skin rash due to meningococcemia
Specific symptoms of meningitis:
Waterhouse-Friderichsen syndrome
Acute adrenal insufficiency syndrome is the most severe and prognostically unfavorable form of meningococcal infection. This syndrome develops with severe meningococcemia and is manifested by shock, collapse and complete cessation of production of glucocorticoid and mineralocorticoid hormones by the adrenal glands.
Waterhouse-Friderichsen syndrome develops as a result of acute hemorrhage into the adrenal cortex, leading to its destruction.
Acute adrenal insufficiency is always extremely difficult. Within one to two hours, multiple hemorrhages appear on the patient’s skin. The petechial rash is confluent, bright, with necrotic foci. The patient's skin takes on a cadaverous hue, and the foci of a confluent rash become similar to cadaveric spots.
High fever, a sharp increase in meningeal symptoms, chills, impaired consciousness, delirium, stupor, and stupor are also noted. Convulsions may occur.
Later, bloody vomiting and symptoms of DN and HF occur. Gangrene of the fingers and toes may develop, requiring amputation.
In the absence of medical care, such patients die within a few hours. However, the mortality rate in this form of MCI is extremely high, even with timely initiation of therapy.
Ways of infection with meningococcal infection
The main route of infection with meningococcal infection is contact with an infected person. Most often, the disease manifests itself in childhood, but the carriers of the virus in most cases are adults.
Meningococcal infection in children can be prevented with timely vaccination.
Meningococcal infection in children, the symptoms of which are described below, can be transmitted to a healthy person:
- when talking with an infected person at a distance of no more than 1 m;
- with loud screaming or crying (in children);
- through airborne droplets (during prolonged contact with a carrier of infection);
- when the wearer coughs or sneezes.
People with weakened immune systems are more susceptible to infection. The disease poses the greatest danger to patients with affected respiratory tracts. There may be cases of re-infection a couple of years after recovery. Meningococci are found in the human nasal cavity and can survive in the external environment for no more than half an hour after “exiting” the host’s body.
There are 4 stages of infection development:
- Infection accompanied by the absence of clinical signs.
- The disease then progresses to the stage of meningococcal nasopharyngitis (inflammation of the nasopharynx). Such a runny nose is almost impossible to distinguish from a symptom of another disease. Determining the presence of meningococcal infection is possible only with a detailed examination of mucus taken from the nasopharynx.
- Then the disease progresses to a more serious stage - meningococcemia (meningococcal sepsis), in which pathogenic microorganisms penetrate the blood of an infected person.
- The most severe degree of infection is the development of meningitis, that is, inflammation of the lining of the brain.
The latter is considered a non-contagious form of the disease.
Infection with primary meningitis can be:
- Transplacental.
Occurs in the womb. In most cases of infection in this way, meningococcal meningitis develops.
- Hematogenous.
This method of infection involves transmission of meningococci through the blood.
- Airborne.
A common way to spread infection. The disease is transmitted when the carrier coughs, talks or sneezes.
- Fecal-oral.
Infection of a child can occur due to insufficient hygiene or when living together with a carrier of meningococci. Enteroviral or adenoviral meningitis can penetrate in this way.
Complications and consequences of meningococcal infection
The prognosis for the life and clinical recovery of a patient suffering from meningococcal infection directly depends on the timely diagnosis of the etiology of the patient’s pathological changes, as well as on the adequacy of the selection of a drug treatment regimen.
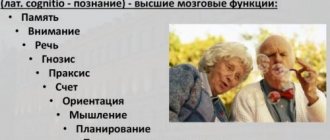
It should be taken into account that late presentation of a patient suffering from meningococcal infection in the form of purulent meningitis is extremely unfavorable for the patient, due to the development of an increased risk of a complicated course of the infection. Provided that drug correction of meningococcal infection is used in a timely manner, the patient recovers completely. The most common complication of meningococcal infection, manifested in varying degrees of severity, is damage to the auditory nerves with hearing loss, which can be either unilateral or bilateral. In pediatric practice, infectious disease specialists encounter more bacterial complications of meningococcal infection in the form of ventriculitis, hydrocephalus, subarachnoid empyema, brain abscess, paresis and paralysis. With meningococcal infection, which manifests itself in the form of meningococcemia, some patients experience secondary infection of the skin with the formation of extensive necrosis.
Numerous clinical and laboratory scientific observations confirm that even if the well-being of a patient who has suffered a meningococcal infection improves, complete restoration of impaired functions does not occur, and therefore, this category of patients is subject to medical examination by neurologists for up to three years.
The most common negative consequence of meningococcal infection in children is the development of signs of cerebrasthenic syndrome, which manifests itself in the form of increased fatigue, sleep and appetite disorders, decreased cognitive functions, psycho-emotional instability, motor disinhibition, absent-mindedness and even aggressiveness.
If there are even minimal clinical manifestations of cerebrovascular disease in a child, various types of psychocorrection should be used, as well as long-term use of nootropic drugs and multivitamin complexes.
Forms and types of infection
Main types of disease:
- Localized (carriage, nasopharyngitis). The disease is asymptomatic or signs appear, as in acute respiratory infections;
- Generalized (meningococcemia, meningitis, meningococcal sepsis). The disease poses a danger to the health and life of the child. Characteristic symptoms appear.
- Mixed (polyarthritis, pneumonia).
A localized infection affects the child’s nasopharynx, a generalized form affects the blood and central nervous system. The second form is dangerous due to severe consequences and the development of serious complications that can lead to death.
Forms of meningococcal infection:
- Spicy. Characterized by rapid development of symptoms (fever, headache, lethargy). With proper therapy, complete recovery is possible.
- Clinical. A rash and joint pain appears. The child cries constantly. The disease affects the kidneys, lungs, and eyes.
- Meningitis. Characterized by the appearance of seizures and signs of meningitis. The baby's reaction is inhibited.
- Encephalitis. A dangerous disease that develops rapidly, leaving little chance of recovery.
Symptoms
The nature of the rash and other features of the clinical picture help to understand the causes of the disease. For a disease caused by meningococcus, the following symptoms may occur:
Main characteristics of the rash:
- Consists of small pink spots on the limbs and torso.
- Gradually fades away and is replaced by other hemorrhagic elements.
- They look like spider veins that disappear when pressed.
- They can be located on any part of the body.
- In the center of the element, a dark-colored area gradually appears - necrosis.
- Large necrosis causes complications.
- Sometimes hemorrhages occur in the eyes, nasal cavity, uterus, and gastrointestinal tract.
Classification of the disease
| Forms of the disease | Varieties |
| Localized | Divided into:
It is the most common form of the infection in question. It is asymptomatic. The incubation period lasts about 5 days (no more than 10). Accompanied by:
The duration of the disease is no more than 3 days. |
| Generalized | May appear as: This form of the disease without meningitis is observed in rare cases. It occurs acutely, with the following appearing:
Characterized by the occurrence of:
Contributes to aggravation of the course of the disease, provokes the occurrence of severe complications. This form of the disease is accompanied by:
|
| Rare forms of the disease are characterized by damage to 1 organ | These include:
|
Signs and symptoms of meningococcemia
The incubation period for meningococcemia ranges from 5 to 6 days. Fluctuations range from 1 to 10 days. The onset of the disease is most often acute and sudden. The generalization of the process is indicated by the deteriorating general condition of the patient, a significant increase in body temperature, increasing headache, increasing pallor of the skin, tachycardia and shortness of breath. Muscle and joint pains, rashes on the skin and hemorrhages on the mucous membranes appear.
A rash with meningococcemia appears in the first hours of the disease. Hemorrhagic elements can be enormous in size and accompanied by skin necrosis. Along with the hemorrhagic rash, hemorrhages are observed in the conjunctiva of the eyes and sclera, mucous membranes of the nose and pharynx, and internal organs. Sometimes gastric, nasal and uterine micro- and macrobleedings and subarachnoid hemorrhages occur.
An extremely severe form of meningococcemia is complicated by damage to the heart and its membranes, thrombosis of large vessels, infectious-toxic shock, hemorrhage in the adrenal glands (Waterhouse-Friderichsen syndrome). Violations of the functions of vital organs lead to the death of the patient.
In some cases, there is a milder course of the disease and atypical meningococcemia, which occurs without skin rashes. In this case, the clinical picture of the disease is dominated by symptoms of damage to one or another organ.
Very rarely, meningococcemia can become chronic or recurrent. The disease occurs with low-grade fever, often with a rash and joint damage. The disease lasts for months and even years. Months after the onset of the disease, the patient may develop endocarditis and meningitis. Periods of remission are characterized by the disappearance of the rash and normalization of body temperature. With chronic meningococcemia, erythema nodosum, subacute meningococcal endocarditis and nephritis can develop.
Meningitis in children - diagnosis
A comprehensive diagnosis of meningitis includes a survey, laboratory and instrumental studies, and a neurological examination. During the interview, the doctor finds out existing or recently suffered diseases, separately specifying the presence of such diagnoses as tuberculosis, rheumatism, syphilis. It is important to notify the doctor if the child has recently had the flu, otitis media, sinusitis, sinusitis, pneumonia, pharyngitis, has undergone surgery, been injured, traveled to another country, or received treatment with antibiotics or antiviral drugs.
Neurological examination can reveal characteristic signs of meningitis in children. First, the doctor checks the symptoms of Brudzinski, Kerning, Lesage, Flatau, and looks to see if there is muscle stiffness. In addition, pain and sensitivity are examined - with meningitis they are increased. The doctor must also conduct an examination of the cranial nerves, which are damaged during meningitis.
Instrumental testing to identify signs of meningitis in children includes an electroencephalogram and computed tomography. Laboratory tests include general and biochemical blood tests, PCR or latex test, cerebrospinal puncture, and cerebrospinal fluid analysis. Types of meningitis according to the pathological morphology of the cerebrospinal fluid:
- serous meningitis in children - the number of lymphocytes in the cerebrospinal fluid is increased, the membranes of the brain are swollen;
- purulent meningitis in children - in the cerebrospinal fluid there is a high content of neutrophils, an increased content of proteins, the membranes of the brain are purulent, thickened.
The basis for the diagnosis of meningococcal infection is the clinical picture, laboratory results and epidemiological history data. A bacteriological analysis of mucus from the nasopharynx, blood, and cerebrospinal fluid is carried out.
Diagnosis of the disease begins with interviewing parents. At the same time, the doctor learns about possible contacts with carriers of the virus and assesses the severity of the disease based on existing complaints and symptoms. Next, the child is examined. The specialist determines the presence of rashes and seizures, the condition of the fontanel in newborns. With a generalized form of infection, an accurate diagnosis can be made after examination.
It is necessary to diagnose this disease as early as possible and carry out therapy, since the disease rapidly worsens the patient’s condition, increasing the likelihood of death. Doctors have little time to make a diagnosis when a child is infected with meningococcal infection.
In the first minutes and hours of the development of the disease, there may be no symptoms, but within a day it can threaten the patient’s life. The pediatrician may suspect the onset of the disease when fever or hemorrhagic rashes appear.
The presence of infection in the body is diagnosed using the following studies:
- Serological (VIEF and RPGA).
- Bacteriological.
The material used is mucus from the nasopharynx, cerebrospinal fluid, and blood. A lumbar puncture is performed to detect meningitis. When diagnosing meningococcemia, it is necessary to distinguish skin rashes from possible allergic manifestations.
Causes
Meningococcus is a bacterium that rarely affects humans. However, if this happens, the consequences can be very serious. Main features of the pathogen:
- It is a round gram-negative bacterium, located in colonies in pairs (diplococcus).
- Very sensitive to the effects of adverse factors. It dies quickly in conditions of low or high temperature, under the influence of sunlight.
- Can persist outside the human body for no more than half an hour.
- It is transmitted exclusively from a person who is infected with the bacterium.
- It spreads quickly in close groups, for example, in kindergartens.
- A person easily becomes infected with the bacterium, but the disease develops in only 1 percent of cases.
- It is the cause of high mortality in childhood.
Not everyone who encounters meningococcus develops serious types of pathology. The mechanisms of pathology development are as follows:
- Diplococcus enters the human body through the mucous membrane of the respiratory tract.
- The carrier process begins.
- With a decrease in local or general immunity, nasopharyngitis begins, which resembles the clinical picture of ARVI.
- When bacteria penetrate the vascular wall, the meningococcemia phase begins (the microbe is in the bloodstream). This corresponds to a process called sepsis.
- In the blood, immune cells destroy the bacteria and release a toxin, which causes symptoms in the skin and internal organs.
- If the microbe enters the brain through the blood, the meninges become inflamed (meningitis).
What is the treatment?
Treatment of meningococcal infection can be carried out at home if the disease is asymptomatic, and also in the absence of preschool children. To treat nosopharyngitis, antibiotics are used, for example, Levomycetin and Furacilin for gargling. In other cases, the child is placed in infectious diseases institutions.
The following types of drugs are used for treatment:
- antibacterial (“Erythromycin”, “Penicillin”);
- hormonal (“Prednisolone”) - to prevent the development of shock;
- diuretics (Lasix);
- anticonvulsants (“Relanium”);
- cardiovascular (“Korglikon”);
- antihistamines (“Supravtin”).
Infectious-toxic shock: what to do?
Infectious toxic shock is a dangerous condition that occurs when dying bacteria release edotoxin. Main symptoms:
- fever;
- decreased blood pressure;
- heavy sweating;
- convulsions;
- vomit;
- diarrhea;
- loss of consciousness.
First aid when symptoms are detected:
- get rid of tight clothes;
- ensure horizontal position and fresh air flow.
These steps must be completed before the ambulance arrives. Treatment of infectious-toxic shock occurs in a hospital. As a rule, hormonal drugs and antibiotics are used. Therapy depends on the causative agent of the disease.
Memo to parents: emergency care
The effectiveness of treatment depends on timely procedures. Emergency care before the doctor arrives:
- for severe headaches, you can use painkillers;
- at high temperatures - antipyretics;
- to prevent infectious-toxic shock, it is necessary to inject a solution of metamizole sodium with drotaverine or papaverine;
- in case of severe vomiting, a solution of metoclopramide should be administered;
- During convulsions, you need to hold your head up.
Fulminant form of meningococcemia
The fulminant form of meningococcemia or Waterhouse-Friderichsen syndrome is an acute sepsis accompanied by multiple hemorrhages in the adrenal glands. The disease occurs in 10 - 20% of cases of generalized meningococcal infection and is the most unfavorable form in terms of prognosis. The mortality rate ranges from 80 to 100%.
Signs and symptoms of fulminant meningococcemia
With the disease, multiple extensive hemorrhages into the skin and the rapid development of bacterial shock are noted. With hemorrhages in the adrenal glands, a deficiency of gluco and mineralocorticoids occurs, as a result of which disturbances in the metabolism and function of a number of organs and systems quickly occur in the patient’s body. The developed crisis (acute adrenal insufficiency) proceeds like Addison's disease and often ends in death.
The fulminant form of meningococcemia occurs suddenly. Body temperature rises significantly - up to 40°C, severe headache and nausea appear. The patient becomes lethargic. Large areas of hemorrhage appear on the skin.
Blood pressure drops, tachycardia appears, the pulse becomes thready, breathing quickens, and diuresis decreases. The patient falls into a state of deep sleep (stupor). Coma develops.
Prehospital antibiotic treatment
Treatment of the patient at home is possible only with asymptomatic nasopharyngitis of meningococcal etiology (if there is only 1 child in the family). The doctor prescribes treatment, taking into account the patient’s condition, as well as the individual characteristics of his body.
It may consist of:
- the use of antibiotics in a dosage appropriate to the age category of the child;
- gargling with a solution of Furacilin or baking soda;
- irrigation of the oral cavity with Ectericide.
Therapy for a generalized form of infection consists of:
- carrying out antibacterial and detoxification therapy;
- use of hormonal drugs;
- symptomatic treatment.
Antibacterial therapy is carried out immediately when characteristic clinical signs of infection appear, since meningococci are highly susceptible to such drugs.
For this the following can be used:
- cephalosporins;
- tetracyclines;
- penicillins.
As immediate therapy at the prehospital stage, the doctor may prescribe:
- Cefotaxime;
- Erythromycin;
- Penicillin;
- Rifampicin;
- Levomycetin;
- Azithromycin;
- Rocephin.
To treat nasopharyngitis, Rifampicin or Levomycetin is used (10 mg/1 kg per day for 3 to 5 days). Meningococcal carriage is treated with a similar method for at least 2–3 days.
The prehospital stage of treatment for purulent meningitis consists of:
- use of Levomycetin succinate (25 mg/1 kg no more than 3 times/day);
- ensuring venous access;
- use of glucocorticoids (1 – 3 mg/1 kg);
- the use of Furosemide (1 – 2 mg/1 kg), antipyretics, saline solutions;
- antibacterial therapy (administration of benzylpenicillin 300–500 mg/1 kg up to 6 times/day);
- use of nootropics, B vitamins.
The prehospital period of treatment of meningococcemia is carried out as follows:
- venous access is provided;
- antibacterial therapy is carried out;
- Levomycetin is prescribed (25 mg/kg several times a day);
- glucocorticoids are used (2 – 3 mg/kg);
- infusion treatment with saline solutions is used.
Treatment tactics in the hospital
If a generalized infection develops, immediate hospitalization of the child is necessary. Patients with a local form of the disease can undergo therapy on an outpatient basis. To treat nasopharyngitis, in addition to using medications, the nasal cavity is washed with antiseptic solutions.
To increase the body's resistance to meningococci, vitamins and medications that have an immunomodulatory effect are prescribed. If a serious illness is suspected, treatment is immediately started, including the use of antibiotics and detoxification.
Intravenous administration of drugs with a diuretic effect is also carried out in order to eliminate swelling of the brain. High dosage corticosteroids and anticonvulsants are prescribed. In addition, treatment can be supplemented with plasmapheresis. In severe forms of the disease, an artificial respiration apparatus is used.
When treating infection, the following can be used:
- solutions for gargling (baking soda, Furacilin);
- detoxification medications (glucose solution or Ringer's);
- antihistamines (Tavegil, Suprastin, Loratadine);
- means for irrigating the oral cavity (Ectericide);
- drugs that have a diuretic effect;
- hormonal medications (Prednisolone or Hydrocortisone);
- anticonvulsants (Relanium, Diazepam, Sodium oxybutyrate);
- glucocorticoids (Dexamethasone);
- drugs that stimulate the cardiovascular system (for example, Cordiamine);
- inotropes (for example, Dopamine) are used to maintain hemodynamics;
Based on the severity of the disease, the patient may be hospitalized in the intensive care unit or in the neuroinfections department of an infectious diseases hospital. For the treatment of severe forms, Amikacin (no more than 20 mg/1 kg per day) and Netilmicin (no more than 2 mg/1 kg 3 times a day) are used.
Hormonal medications are also used to suppress the immune response to the spread of infection in the patient’s body and normalize blood pressure. In case of infectious-toxic shock development, therapy is carried out in intensive care.
Patients who have had the disease may experience complications such as:
- behavioral disorders;
- cerebral syndrome;
- aggressiveness;
- hyperactivity/inhibition;
- restless sleep;
- absent-minded attention;
- deterioration/loss of appetite.
Therefore, after completing hospital treatment, most people require follow-up therapy. Patients are discharged after the disappearance of clinical symptoms, as well as after normalization of laboratory parameters of the CBC and cerebrospinal fluid. After 3 days. After using antibiotics, a control swab is taken from the nasopharynx.
Most often, cerebrasthenic syndrome is observed, which is a consequence of meningococcal infection. Accompanied by restless sleep, deterioration/loss of appetite, increased fatigue, and altered behavior. Young children are characterized by the appearance of distracted attention, irritability, lethargy, and aggressiveness.
During the recovery period the following are prescribed:
- nootropics;
- multivitamins;
- vascular medications.
When diagnosing such a syndrome, parents should provide the child with a calm regime, increase the time of sleep and walking, and limit the period of time in front of television and computer monitors.
Dispensary observation of children
After discharge from the hospital, the child needs medical supervision for 2–3 years. He should visit not only a pediatrician, but also a neurologist (at least 1 time per month). This is necessary for timely detection of the consequences of meningococcal infection in children and their correction.
In the first few weeks (depending on the individual characteristics of the child), therapy with medications with a diuretic effect, as well as nootropic and vascular medications, continues, even in the absence of clinical symptoms. The child is exempted from physical activities for 6–12 months. Parents must also ensure a calm regime.
Diagnostics
Diagnostic measures in children and adults do not differ from each other. The diagnostic search largely depends on which organ system is affected by the microbe.
Additional studies include:
- Culture of nasal discharge, blood or cerebrospinal fluid. The resulting material is sown on a special medium and placed in conditions favorable for the bacteria. The most informative, but time-consuming research method.
- Serological test for antibodies to meningococcus. A good technique, however, it is not reliable if a person has suffered from any form of infection in the past or is currently simply a carrier.
In infants, diagnosis is complicated by the inability to collect a complete medical history. In this case, the role of laboratory techniques increases significantly.