Tumors of neuroepithelial tissue. Embryonic tumors. ICD/O 9470/3 (G IV). Medulloblastoma
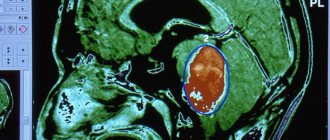
Medulloblastoma is more common in children and is located infratentorially, representing a cystic-solid tumor (Fig. 747, 748), arising from the cerebellar vermis, with a tendency to grow into the lumen of the fourth ventricle.
7% of all CNS tumors in childhood and 0.4-1% in adults. The age range of occurrence is 5-15 years. Peak age 5-9 years.
Medulloblastoma (MB) is an embryonal tumor. Previously, it belonged to the group of primitive neuroectodermal tumors (PNET) from the category of embryonal tumors [2]. Today, many authors continue to consider it as part of PNET, however, it differs from other representatives of the PNET group in the neurobiology of its behavior and clinical neurological manifestations [2].
Medulloblastoma is structurally a round, solid, cystic-solid (in 65%, sometimes, less often, entirely solid) formation with clear contours, located in the cavity of the fourth ventricle, typically growing from the cerebellar vermis in childhood, as well as in the cerebellar hemisphere in older age. in older age groups, it can invasively grow, infiltrate and grow into its hemispheres, as well as into the dorsal sections of the pons, causing obstruction of the openings of the fourth ventricle and forming a cerebrospinal fluid block, leading to hydrocephalus (in 90-95%). The tumor has a pronounced mass effect, crowding the brainstem and cerebellum.
A solid space-occupying formation (asterisks in Fig. 751-753), filling the IV ventricle, growing from the cerebellar vermis (arrows in Fig. 751) and leading to obstructive hydrocephalus (arrowheads in Fig. 753) and herniated cerebellar tonsils (arrow in Fig. 753). 753).
On MRI, the tumor has ↑↓ MR signal intensity in T2, predominantly ↑ and ↓ in T1. On CT, more often ↑ (90%), less often ↑↓ density relative to the brain substance, petrification in 17% of cases [14]. In 20% of cases, there are intratumoral hemorrhages [2]. ↑DWI reflects the dense nature of the tumor, which limits the diffusion of extracellular water protons and has a high nuclear-cytoplasmic ratio [9]. The mass is sharply demarcated and often surrounded by vasogenic edema [2].
Medulloblastomas are usually midline tumors and the most common are the vermis and inferior medullary velum (80% of cases). Less commonly, the tumor is located in the lateral hemisphere of the cerebellum, which occurs in older children. The vast majority of MB (94% of cases) arises in the cerebellum, and grows mainly from the vermis (75% of cases), protruding into the IV ventricle from its roof, sometimes growing into the brain stem [2].
Cystic-solid space-occupying formation - medulloblastoma (asterisks in Fig. 754-756) in the IV ventricle with mild perifocal edema (arrows in Fig. 754,756).
Rapid aggressive growth with rapid development of clinical symptoms. There is a tendency for a more benign course when occurring in adults than in children, where the prognosis is often unfavorable. Medulloblastoma can metastasize to the membranes of the brain and spinal cord, which occurs in 60% of cases [13]. Pressure can provoke herniation of the cerebellar vermis through the tentorial foramen, as well as the cerebellar tonsils through the foramen magnum [2]. In the vast majority of cases, the mass grows into the fourth ventricle and infiltrates its floor [2].
Hydrocephalus is an expansion of the lateral ventricles, accompanied by periventricular transependymal permeation of the cerebrospinal fluid with the development of gliosis (arrowheads in Fig. 757, 758). Herniation of the cerebellar tonsils into the foramen magnum and hydrocephalus (arrow in Fig. 758). Metastases into the pia mater of the spinal cord and brain are clearly visible after contrast (arrows in Fig. 759).
Contrast enhancement is pronounced and heterogeneous in 90%, but in 20% of cases it may be absent (Fig. 760-762).
Pilocytic astrocytoma has a later age peak than medulloblastoma and is much less common. It often arises from the cerebellar hemisphere (which should be taken into account in differential diagnosis with “late” medulloblastomas), and not from the vermis. It is characterized by less aggressive growth, as well as the absence of metastases.
A volumetric formation in the form of a cyst (asterisks in Fig. 763-765) with a parietal node (arrow in Fig. 764, 765), compressing the IV ventricle (arrow heads in Fig. 763-765) and leading to occlusive hydrocephalus (black arrow heads in Fig. 763-765) Fig.765).
Ependymoma has a cellular structure, tends to spread through the foramina of Luschka and Magendie into the basal cisterns, and does not invade surrounding structures, and is characterized by modest growth dynamics. Ependymomas are usually → on CT and → on T1, and medulloblastoma is ↑ on CT and ↓ on T1.
A cystic-solid formation of the fourth ventricle, spreading through the left foramen of Magendie into the subarachnoid space (arrow heads in Fig. 766-768) and intensively accumulating contrast agent (arrow in Fig. 768).
Choroid papilloma is most often located in the lateral ventricles, does not invade their walls, and causes the occurrence not of occlusive hydrocephalus, but due to overproduction of cerebrospinal fluid (the only variant of cerebral pathology in which there is a predominance of cerebrospinal fluid production over its resorption).
Solid formation of the IV ventricle associated with the choroid plexus (arrows in Fig. 769-771) and hyperproductive hydrocephalus (arrowheads in Fig. 771).
The idea of metastasis makes most sense when it comes to a single cerebellar mass in adulthood, since metastasis is a much rarer occurrence in childhood. Metastasis has pronounced perifocal edema, unclear contours without IV enhancement, and after enhancement they indicate a relatively clear border with homogeneous accumulation or corona effect. Some metastases, when growing, spread to the bones of the skull, causing their destruction and periosteal reaction of the outer plate of diploe.
Metastasis to the cerebellum with pronounced perifocal edema (arrowheads in Fig. 772) and invasion into the squama of the occipital bone, with its germination (arrows in Fig. 772). Metastasis in the cerebellum with a pronounced mass effect in the form of compression of the lumen of the fourth ventricle (arrowheads in Fig. 773) and herniation of the cerebellar tonsils (arrow in Fig. 773). Hypodense formation in the cerebellum on CT (arrowheads in Fig. 774).
Hemangioblastoma is a cystic tumor with a small parietal node, located infratentorially, can occur intramedullary in the spinal cord, and is associated with von Hippel-Lindau disease, which affects other organs and systems, in particular the lungs and kidneys (polycystic disease). Character for older age groups.
A large cyst of the IV ventricle (asterisks in Fig. 775-777) with a parietal papilla (arrows in Fig. 775-777) and leads to hydrocephalus (arrowheads in Fig. 777).
Clinical manifestations are mainly determined by intracranial hypertension, nausea and vomiting, as well as visual impairment, which is associated with occlusive hydrocephalus and direct pressure of the tumor mass on the bottom of the fourth ventricle. Symptoms progress rapidly at the rate of medulloblastoma growth, over weeks to months.
Treatment includes surgical removal, radiation and chemotherapy. The tumor has good radiosensitivity. Median survival from initial detection of relapse is 10.5 months. 76% of relapses occur within the first 2 years. After surgical resection of the tumor, chemotherapy and radiation therapy play an important role in the treatment of medulloblastomas [2].
Causes and provoking factors
Basically, such neoplasms are irregular in nature.
An exception to this rule are people suffering from hereditary diseases, which significantly increase the risk of developing malignant processes in the body. This is possible if the patient has Turcot, Gorbin and others syndrome. The exact cause of the development of the pathological condition could not be determined. Scientists identify only certain factors that increase the risk of tumor formation. The disease can occur under the influence of:
- early age of the patient and the associated immaturity of the body;
- ionizing radiation;
- viral diseases that contribute to damage to the genome of cells. These are herpes, cytomegalovirus, human papillomavirus and others;
- hereditary predisposition;
- carcinogenic substances found in food and household chemicals.
The tumor gradually grows into the brain stem and affects the cranial nerves. This condition is typical for advanced stages of development of the pathological process.
Signs and symptoms
The specific symptoms associated with medulloblastoma will vary from one person to another depending on the exact location and size of the medulloblastoma and whether the tumor has spread to other areas. Affected people may not have all of the symptoms discussed below. Affected people should talk to their doctor and medical team about their specific case, associated symptoms, and overall prognosis.
Symptoms of medulloblastoma usually occur due to increased pressure in the skull (intracranial pressure). Medulloblastomas usually arise at or near the base of the skull, in an area known as the posterior fossa. The posterior fossa contains the brain stem and cerebellum.
Medulloblastomas usually involve the fluid-filled fourth cavity (ventricle) of the brain. The brain has four cavities called ventricles, which are filled with cerebrospinal fluid (CSF) and connected by channels through which the CSF circulates. Because tumor often fills the fourth ventricle, CSF circulation is obstructed, leading to hydrocephalus. Hydrocephalus is a condition in which the accumulation of excess CSF in the brain causes a variety of symptoms, including repeated, often severe vomiting, lethargy, and headaches that often begin in the morning and improve as the day progresses. Additional symptoms may include:
- irritability;
- increase in head size;
- paralysis (paresis) of the muscles that help control eye movements (extraocular muscles).
Many infants and children with medulloblastoma develop papilloedema, a condition in which the optic disc swells due to increased intracranial pressure. The optic nerve is the nerve that transmits impulses from the retina to the brain. Papilloedema can lead to decreased vision clarity. Because many symptoms associated with medulloblastoma are nonspecific and often subtle, papilloedema may be the first sign that raises suspicion for a neurologist.
Children with medulloblastoma often have signs of cerebellar dysfunction. Symptoms may include poor coordination, difficulty walking, and clumsiness (ataxia). Affected children may fall frequently and develop an unsteady, awkward way of walking (wobbly gait). They may stand with their legs wide apart, stagger or sway when walking, and lose their balance easily.
As the tumor grows or spreads, additional symptoms may appear. Such symptoms may include double vision (diplopia), rapid, sharp eye movements (nystagmus), facial muscle weakness, ringing in the ears (tinnitus), hearing loss, and neck stiffness. Some children with double vision may tilt their head to try to line up the two images.
Classification of medulloblastomas
Medulloblastoma is a neoplasm that in most cases is localized in the cerebellum. The tissues of the hemispheres may also be affected.
Depending on the structure of the tissues of the formation, several types of brain tumors are distinguished:
- classic medulloblastoma;
- formation with neuronal differentiation;
- medullomyoblastoma;
- desmoplastic medulloblastoma;
- lipomatous medulloblastoma, which consists primarily of fat cells.
In the presence of a cerebellar tumor in adults or another localization, the prognosis is made depending on the size, stage of development and general condition of the patient’s body.
Desmoplastic medulloblastoma is much less common than others. According to studies and subsequent results, with this pathology the prognosis is more favorable than in other cases. These malignant cells respond better to radiation and chemotherapy.
Terminology
Founder of American and world neurosurgery
H. Cushing
, who first used the term "medulloblastoma"
The term “cerebellar medulloblastoma” was first used by neurosurgeons Percival Bailey (English) Russian. and Harvey Cushing in 1925. By it they understood a highly malignant small cell tumor in the midline of the cerebellum[8].
The proposed definition remained unchanged until 1983, when scientists Rorke, Becker and Hinton suggested that all malignant small cell tumors of the central nervous system (including medulloblastoma) are primitive neuroectodermal tumors. (English)
primitive neuroectodermal tumors - PNET). According to their work, medulloblastoma differs from PNET only in its location[9][10]. Previously, the term PNET meant only supratentorial (located above the tentorium of the cerebellum) malignant small cell tumors.
These tumors are believed to originate from embryonic cells[2]. As of 2011, the question remains unresolved as to whether medulloblastoma is a primitive neuroectodermal tumor or a separate type of malignancy[1].
The World Health Organization's 1993 classification of brain tumors defines medulloblastoma as a distinct embryonal tumor. PNET, according to the same classification, is a neoplasm, histologically indistinguishable from medulloblastoma, which is located outside the cerebellum[11]. In general, the terms “posterior fossa PNET” and “medulloblastoma” are considered synonymous[1].
What are medulloblastomas?
Medulloblastoma is the most common malignant brain tumor in children. Medulloblastomas, by definition, occur in the cerebellum, which is the part of the brain located at the base of the skull, just above the brain stem. The cerebellum is involved in many functions, including the coordination of voluntary movements (eg, walking, fine motor skills) and the regulation of balance and posture.
Medulloblastomas arise from primitive, undeveloped brain cells. Most medulloblastomas occur in infants and children. Less commonly, these tumors can develop in adults. Symptoms associated with medulloblastoma include headaches in the morning that get worse as the day goes on, intermittent vomiting, difficulty walking and balance. Medulloblastomas can spread to other areas of the central nervous system. The exact cause of medulloblastoma is unknown.
Clinical picture
Medulloblastomas have a main distinguishing feature that makes them one of the most dangerous tumors - the rapid spread of metastases. Cancer cells enter the cerebrospinal fluid circulation pathway and affect other organs and systems.
With such a pathological process, various manifestations may occur. It all depends on where in the brain the tumor appears. Damage to the cerebellum leads to cerebellar ataxia, the manifestations of which are:
- Impaired balance, as a result of which, in order not to fall, a person spreads his legs wide and balances with his hands. This gait is called cerebellar.
- Gait changes. She becomes unsteady, the patient rolls from side to side.
- Frequent injury due to falls.
- Problems with swallowing function.
- Breathing disorders. This indicates the spread of the tumor to the brain stem.
- Development of nystagmus.
- Decreased sensitivity of the limbs, which ends in the development of paralysis. With such symptoms, we can conclude that the malignant process has affected the spinal cord.
Complications of pathology
Most often, hydrocephalus develops, which is characterized by the accumulation of fluid in the cranial cavity. Swelling disrupts the functioning of all parts of the brain, blocking unconditioned reflexes.
Signs of meningitis may also occur when an inflammatory process develops in the membranes. The spread of metastases to vital organs causes disruption of their functioning. Damage to the kidneys and liver causes a sharp and rapid deterioration in the general condition. Cardiac and respiratory failure can cause death.
Increased intracranial pressure is fraught with the development of vascular heart attack and stroke, which increases the risk of death. Chemotherapy and radiation therapy have a number of complications, which also burden the performance of the body affected by cancer.
Pathological anatomy
On
microslide
medulloblastoma, the structures characteristic of this type of neoplasm are clearly visible in the form of the so-called. sockets
Macroscopically, medulloblastomas are a soft grayish-pink nodule, which is clearly demarcated from the surrounding tissue. Microscopically, the tumor consists of densely located undifferentiated cells that form peculiar structures in the form of regular or random rows, which are compared to “ridges” and “columns” [4].
The histological structure of medulloblastomas is characterized by structures in the form of “rosettes” formed by ring-shaped tumor cells, the processes of which converge in the center of the rosette. Tumor cells have increased mitotic activity.
The tumor stroma contains a small number of small, thin-walled vessels. Foci of necrosis and cysts are not typical for medulloblastomas. The growth of the neoplasm is infiltrative with germination of adjacent tissue and soft membrane of the brain [4].
Medulloblastomas metastasize mainly along the pathways of the outflow of cerebrospinal fluid into the pia mater of the brain and spinal cord and the ependyma of the ventricles of the brain. In the area of metastasis, flat, whitish nodules merging with each other are macroscopically determined, which turn into diffuse growths. It is extremely rare for medulloblastomas to metastasize beyond the central nervous system[4].
If the brain stem is affected
When the spinal cord is damaged, various paralysis or paresis (weakening of muscles due to insufficiency of nerve signals causing their tone) of the muscles, as well as sensory disturbances, first develop.
When the cerebellum is damaged, cerebellar ataxia syndrome develops, expressed in loss of balance, affecting all motor skills and mainly gait. A “cerebellar gait” is when a person has difficulty maintaining balance on two legs, walking with their legs wide apart and actively balancing with their arms, while swaying from side to side and often falling, as if they were walking on the deck of a ship in a storm.
https://www.youtube.com/watch?v=7TlAp79fkjk
When a tumor develops, when in addition to the cerebellum it grows or metastasizes into the brain stem, the patient’s condition worsens extremely, since this organ is responsible for controlling the functioning of the main organs that support vital functions. At the same time, breathing and heartbeat disturbances, loss of the swallowing reflex, various eye symptoms in the form of blurred vision, nystgamp (involuntary fast-moving eyes), gaze paresis (eye freezing in one place) or malfunction of other organs, including sensory organs, begin.
The development of hydrocephalus also has its own symptoms:
- Dizziness, debilitating headaches.
- Severe nausea with causeless, painful vomiting.
- Epilepsy.
- Violation of muscle tone and reflexes.
- Neurological manifestations in the form of disruption of internal organs.
- Enlargement of the skull.
- Strabismus.
Since the brain is responsible not only for the functioning of the body and internal organs, but also for thinking and consciousness, psychoneurological symptoms develop accordingly:
- Psychomotor agitation.
- Change of consciousness.
- Increased irritability.
- Loss of orientation in space and time.
- Loss of one's own personality or orientation in it.
Also, to the general cerebral symptoms of a tumor after metastasis, pain symptoms and symptoms of dysfunction of the organs where it occurred are added.
How is the disease diagnosed?
An accurate diagnosis can be made only after a series of laboratory and instrumental studies. It is very difficult to determine the presence of a tumor in a child’s brain. It's connected with:
- structural features of the children's skull;
- plasticity of brain tissue;
- elasticity of blood vessels.
First of all, if medulloblastoma is suspected, anamnesis is collected and a physical examination is performed. This allows us to identify factors contributing to the development of the disease and characteristic symptoms. Thanks to this, it is also possible to predict the degree of development of the pathological process. After this, laboratory tests are prescribed, including:
- biochemical blood test, general analysis;
- general urine analysis;
- determination of tumor markers.
The most detailed information about the tumor and the patient’s condition can be obtained:
- With neurosonography. This procedure is performed to make a diagnosis in newborns, since their fontanel is not yet closed.
- Using computed tomography and magnetic resonance imaging. The study allows you to accurately determine the location and volume of formation, as well as infiltration.
- With two-photon emission tomography. This diagnostic measure makes it possible to detect metastases and even the smallest structural changes in brain tissue.
- Using a biopsy. This analysis allows us to finally confirm the assumption and determine the tactics for further action.
If necessary, a consultation with an ophthalmologist or surgeon may be recommended.
Disorders with similar symptoms
Symptoms of the following disorders may be similar to those of medulloblastoma. Comparisons may be useful for differential diagnosis.
Various types of brain tumors may result in increased intracranial pressure and generalized symptoms similar to those potentially associated with medulloblastomas, such as vomiting, headaches, gait disturbances, changes in consciousness, visual disturbances, enlarged heads in young children, and/or others. abnormalities. Such tumors may also lead to additional generalized or more localized symptoms not usually associated with medulloblastomas; differ in the average duration of symptoms before diagnosis; and/or have other clinical characteristics not typically seen in medulloblastomas. Confirming the presence of a brain tumor and determining the specific type of tumor usually requires a clinical and neurological examination, a complete medical history, advanced imaging, and other diagnostic measures.
How to make a treatment plan
To eliminate medulloblastoma in the cerebellum, a complex of therapeutic measures is carried out. The problem cannot be eliminated without surgical treatment. The choice of surgical treatment method is carried out depending on the stage of development of the tumor, where it is located, what its size is, taking into account the presence of concomitant diseases and the general health of the patient.
During surgical excision, the tumor is removed, and if it has grown into the brain tissue, then part of it. After the procedure, chemotherapy is mandatory, as it is necessary to destroy malignant tumors.
Diagnostics
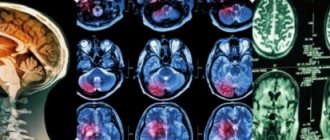
CT scan of the head of a 6-year-old girl with medulloblastoma in the posterior cranial fossa
In typical cases, medulloblastomas are identified on CT scans as round or oval voluminous formations that heterogeneously accumulate contrast material and are located in the projection of the cerebellar vermis.
On MRI it is characterized by a heterogeneously altered signal, reduced on T1-weighted images. On T2-weighted tomograms, the signal varies from hypo- to hyperintense. Images in the sagittal projection clearly determine the location of both the upper and lower poles of the tumor, which is usually located in the occipital cistern [20].
If a patient has medulloblastoma, an MRI examination of the spinal cord is recommended, which makes it possible to judge the presence or absence of metastases[20].
When conducting an examination with the introduction of contrast agents, their heterogeneous accumulation occurs in different parts of the tumor. Metastasis of medulloblastoma to the pia mater of the spinal cord and brain is better determined after the administration of contrast agents[20].
Affected Populations
Medulloblastomas can affect people of any age, but most often occur in children under 15 years of age, with peak incidence between 3 and 9 years of age. Medulloblastomas are the most common malignant brain tumor in children. Approximately 80 percent of victims are under 15 years of age. Medulloblastomas are extremely rare in adults, accounting for 1-2 percent of all cases of adult brain tumors. In adults, most medulloblastomas occur between the ages of 20 and 44 years. Medulloblastomas are extremely rare in people over 45 years of age.
Among children, boys get sick more often than girls. However, in adults this ratio is the same. The exact incidence of medulloblastomas is unknown, and many different estimates are given in the medical literature. Typically, medulloblastomas account for 2 percent of all primary brain tumors and 18 percent of all pediatric brain tumors.
Forecast
There are two prognostic groups - low and high risk. The low-risk group includes patients with T1 or T2 tumors, in the absence of M0 metastasis (according to the modified Chang classification), children over 3 years of age, total tumor removal.
Medulloblastomas T3-T4 (according to Chang's classification), metastasis (M1-M4), age less than 3 years, as well as subtotal tumor removal are a high-risk group [24]. The five-year survival rate (the number of patients who are alive 5 years after surgery) in the low-risk group is about 75%, in the high-risk group it is less than 35%[5][6].
The worst prognosis of the disease is in patients with tumor recurrence after surgery. The average life expectancy after detection of tumor growth at the original site after its removal is 13-18 months[7][25].
The relapse rate for medulloblastoma is quite high. Most often, the prognosis is disappointing.
With this diagnosis, most patients become disabled or die. The forecast will be as follows:
- 30% of patients survive after surgery for five years;
- How severe the malignant process will be depends on the age of the patient. In children, the involvement of the brain stem in the pathological process occurs very quickly;
- If the tumor recurs, there is no chance of survival.
How to treat after surgery
After completing the course of treatment in a medical institution, further therapy is carried out at home. Relatives should create a schedule for the patient’s day in which he will rest and stay awake for a sufficient amount of time.
An important part of the treatment of the disease is diet. The patient should not be forced to eat a lot. He should consume food in small portions as desired. The emphasis should be on citrus fruits. When preparing dishes, it is necessary to take into account the wishes of the patient, since under the influence of treatment he may develop new and sometimes strange taste preferences.
Some try to relieve pain and alleviate the condition using alternative medicine methods. You cannot use such means without the knowledge of a specialist. If your doctor allows you to feel better, you can do the following:
- aloe juice;
- decoction of dried apricots;
- walnuts and lemon;
- figs and honey;
- nettle and white mistletoe;
- sorrel and dill;
- tansy and celandine.
These means can maintain the patient's condition normal.