A transient ischemic attack (or simply a microstroke) is a disorder in the cerebral circulation. A micro-stroke occurs when oxygen stops flowing through the blood to the brain. This condition differs from a massive ischemic stroke only in that the body is able to independently again ensure sufficient blood flow to the brain. Despite the fact that the recovery process occurs quite quickly and without the help of doctors, a small stroke is still very dangerous and such a condition cannot be ignored.
This article will discuss methods for diagnosing a microstroke, its consequences, treatment and recovery of the body after the disease.
What is a microstroke
It should be immediately clarified that such a diagnosis and disease as microstroke does not exist in the International Classification of Diseases, but despite the fact that the term is colloquial, it is used by both patients and doctors. What we call a microstroke is interpreted in medicine as a transient disturbance of cerebral blood flow. This is the most common type of vascular dysfunction, which is a “warning” of the body about an impending much more terrible problem - a stroke.
In simple terms, a transient ischemic attack is a sudden blockage of the arterial lumen by a blood clot, the body copes with the dissolution of which on its own, and the flow of blood to the brain is resumed. Cerebral blood flow is restored within a few minutes and the signs of an ischemic attack that have already appeared disappear without a trace. Then what is the difference between a microstroke of the brain and a major stroke?
Features of symptoms
In the initial stage of stroke development, headache, dizziness against a background of general weakness, vomiting, and blurred vision may occur. These are precursors characteristic of both types of stroke: ischemic and hemorrhagic. Let us consider in detail how ischemic stroke differs from hemorrhagic stroke.
Clinical picture:
- If hemorrhage is observed, the condition is accompanied by complete or partial muscle paresthesia. The patient's motor function and spoken speech are impaired, and red circles appear before the eyes.
- Ischemia is characterized by a sensation of a blow to the head followed by loss of consciousness. One-sided weakness in the affected part of the body is accompanied by a sharp headache, severe nausea, and vomiting. In severe cases, coma may develop.
Hemorrhage begins suddenly as a consequence of physical or emotional stress. At a young age, stroke often occurs without warning.
General cerebral symptoms prevail over focal ones. These include:
- severe headache;
- vomiting;
- disorientation, disturbances of consciousness.
During coma, there is a sharp drop in blood pressure, respiratory depression, and there is no reaction to conditioned stimuli. Facial hyperemia is noted against the background of bluish lips; cold clammy skin.
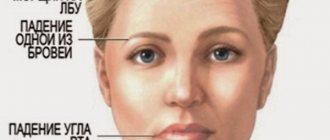
How to recognize a stroke
Since the condition develops at lightning speed, you need to remember several simple algorithms based on which you can suspect a stroke. The sooner the patient receives qualified medical care, the more successful the treatment and the minimal the consequences.
If a stroke is suspected, ask the victim:
- Smile - as a result of paralysis, the smile will be unnatural, the corners of the lips will be unevenly raised.
- Speak – the patient finds it difficult to pronounce speech and is characterized by retardation.
- Raise your arms at the same level: a person in a pre-stroke state will not be able to do this.
Stroke Clinic
The difference between ischemic and hemorrhagic stroke is significant, so treatment and recovery programs differ.
Do you know? Scientists from the University of California have found that stimulating biologically active points on a person’s fingers, lips and face helps normalize blood circulation in the brain, being an excellent means of prevention.
Differences from stroke
Firstly, during a massive hemorrhage in the brain, a large blood clot forms and the body is not able to cope with it quickly. The blood clot disappears only after a few hours or days. During this period, brain cells and tissues rapidly die due to nutritional deficiency and oxygen starvation. They will never be able to recover, so the patient’s severe consequences remain for life.
Secondly, the symptoms of a microstroke are less pronounced, and doctors mistakenly diagnose many patients with “vegetative-vascular dystonia,” attributing the ailment to a violation of cerebral vascular tone. A minor stroke is a serious signal that the blood supply to the brain has failed and the risk of a severe stroke is high. It should be remembered that a repeated micro-stroke can cause the same tragic consequences as a massive cerebral hemorrhage.
Clinical picture
Symptoms of ischemic stroke
Ischemic stroke - symptoms
Symptoms of manifestation are very diverse and depend on the part of the brain in which ischemia occurred.
- Impaired consciousness;
- Strong headache;
- Nausea;
- Vomit;
- Increased sweating;
- Dry mouth;
- Gait disturbance;
- Visual disturbances in the form of double vision, decreased vision;
- Changes in hearing up to complete deafness;
- Dysarthria, aphasia;
- Memory loss.
Symptoms of hemorrhagic stroke
Hemorrhagic stroke - symptoms
Hemorrhage occurs with severe consequences and death occurs in 50–90%. It develops very quickly and the first harbinger of an upcoming brain catastrophe is a headache, a feeling of fullness in the head, vomiting, and impaired consciousness. After a few minutes, paresis and loss of consciousness may occur. The time during which medical workers can provide assistance and prevent the death of a patient is very short and ranges from 3 minutes to several hours.
- Confusion and loss of consciousness;
- Weakness;
- Vomit;
- Headache;
- Hemodynamic disorders.
- Paresis, paralysis of the limbs, a certain side of the body, facial muscles;
- When the left temporal lobe is damaged, speech impairment occurs;
- Visual and hearing disorders.
Hemorrhagic and ischemic stroke have fairly similar symptoms, the difference between them is that in the hemorrhagic form of the disease the symptoms are more pronounced and the patient’s condition is assessed more severely.
Ischemic microstroke: who is at risk
An attack, as a rule, appears against the background of certain predisposing external or internal factors. Most often, many chronic diseases lead to illness:
- Atherosclerosis (systemic vascular damage). If a person suffers from cardiac ischemia, then atherosclerotic plaques will also be in the vessels of his brain.;
- Hypertension;
- Diseases of the cardiovascular system;
- Diabetes;
- Severe obesity
- High cholesterol levels in the blood;
- Major blood loss suffered in the past;
- Heart disease (tachycardia, myocardial infarction);
- High concentration of red blood cells in the blood.
A large number of people facing ischemia lead a sedentary lifestyle, abuse alcohol and smoke for quite a long time.
Regular headaches and taking oral contraceptives also increase the risk of developing an attack.
Knowing the causes of a micro-stroke and being able to recognize it in time, one should begin to prevent more severe disorders in the body, with the ensuing consequence of a stroke.
By periods of development
During an ischemic stroke, a number of processes occur that together lead to the death of neurons. Cells begin to die against the background of cerebral edema.
At the same time, the brain enlarges and intracranial pressure increases. Cell swelling leads to displacement of the temporal lobe and compression of the midbrain.
Sometimes compression of the medulla oblongata is observed due to wedging of the cerebellar tonsils into the foramen magnum.
Often this process ends in death. Therefore, when the first signs of a stroke appear, it is necessary to hospitalize the victim as quickly as possible.
The development of ischemic stroke is divided into certain periods:
- The sharpest. Lasts on average 4-5 hours. It is in the first hours that you need to have time to provide medical assistance to the patient. Timely measures taken will help avoid progression of the disease and prevent complications of varying degrees.
- Spicy. This period begins two days after the attack and lasts 2-3 weeks. All this time, the patient continues to be in a specialized department of the hospital, where he is undergoing treatment. Drug therapy is aimed at reducing tissue swelling, inflammation, improving blood circulation in the brain, maintaining blood pressure and the functioning of the cardiovascular system. The next period is called subacute, which lasts 2-2.5 months.
- Early recovery. The early recovery stage is considered to be the period from 3 to 6 months after the first signs of pathology. In order to fully eliminate the consequences of an ischemic stroke, the patient is prescribed various measures to restore sensitivity in the arms, legs and other parts of the body, in case of speech impairment, work with a speech therapist, and, if necessary, continue the course of drug therapy.
- Late recovery. Duration from 6 months to a year. By this time, the results of treatment and rehabilitation measures are already visible. If the patient worked hard and carried out everything strictly according to plan, then after a year his speech and sensitivity of the limbs are restored, motor skills improve, some can already move independently and take care of themselves.
- Residual effects and consequences. This period begins a year after the attack, and is no longer limited in time. Recovery after a stroke (ischemic, hemorrhagic) is a very long and labor-intensive process, so you need to be patient and continue to engage in physical therapy, adhere to a diet, and undergo treatment in a sanatorium at least once a year.
The first signs of a microstroke
Above, we tried to figure out who can be “overtaken” by a microstroke and what it is. Now let's talk about how to identify a microstroke by its primary symptoms. It is not difficult to suspect a minor ischemic stroke in yourself or someone nearby, knowing what symptoms are characteristic of it:
- The patient complains of dizziness and increasing severe headache;
- Vision deterioration often occurs: flashes and “spots” appear before the eyes;
- Coordination of movements is impaired: a person may stagger and even fall;
- Part of the face or limb goes numb;
- Blood pressure changes, vomiting is possible;
- Bright light and noise cause irritability and worsen headaches;
- The ability to speak deteriorates: it is difficult for a person to answer basic questions, speech becomes inarticulate.
Be sure to call an ambulance!
It is important to note here that even if the signs of the disease completely subsided after a few minutes, the state of health became normal, an ambulance should still be called. Timely detection of an attack significantly increases the chances of complete recovery.
An ischemic attack of the brain may recur soon and possibly in a more serious form. Statistics say that a third of people experience the symptoms of a mini-stroke again. Every tenth person after a “minor hemorrhage” experiences a major stroke within three months. Moreover, 50% of attacks occur within the first 48 hours.
A microstroke and its symptoms are the first signs of an approaching major stroke.
Specificity of signs: why is a microstroke dangerous?
Many patients attribute the first symptoms of a micro-stroke (dizziness, headache of any intensity, general weakness) to constant fatigue and stress, weather changes and magnetic storms. Often, some symptoms of an attack are absent or mild, however, 4-5 signs are enough to make a diagnosis.
Classic neurological signs of the disease develop to a greater extent in men. At the same time, the risk of cerebrovascular accidents in women from 20 to 40 years of age is higher compared to men of the same age.
Often, a person’s attack can be noticed quickly by those around him: the patient’s speech suddenly becomes incoherent, he becomes silent or stops responding to calls. The man looks like he's drunk.
Differential diagnosis - how doctors detect stroke
Differential diagnosis is extremely important for identifying types of stroke for which treatment is different. Diagnosis is carried out using instrumental studies:
- Computed tomography . Necessary to determine the amount of hemorrhage and the type of stroke.
- Diffusion-weighted tomography . It is needed to identify areas of the brain with impaired blood circulation and takes 1-2 minutes.
- Angiography . Allows you to assess the condition of blood vessels and identify the presence of blood clots in them.
An MRI is rarely done if a stroke is suspected. This is due to the duration of the study.
Additional studies that are prescribed for illness:
- ECG;
- Ultrasound of the heart;
- ECHO KG.
Differential diagnosis is also performed based on symptoms. Its data is presented in the table
Difference in symptoms:
| Symptoms | Ischemic form | Hemorrhagic form |
| Development speed | Gradual | Swift |
| Change in the patient's appearance | Absent | There is redness of the face and heavy sweating |
| Headache with nausea | Rarely | Often |
| Change in muscle tone | Present | Present |
| Loss of consciousness | Short term | Sequels |
| Increased blood pressure | Yes | Sometimes |
| Problematic speech | Yes | Sometimes |
| Retinal condition | Clean | With hemorrhages |
Data from instrumental differential diagnostics for stroke
| Research | Result in ischemic form | Results for hemorrhagic form |
| ECG | Presence of arrhythmia | Enlargement of the heart |
| Fundus examination | Vascular changes | Hemorrhages |
| ECHO | No offset | With a shift to the healthy hemisphere |
First aid
What to do before the doctors arrive if a micro-stroke begins in a loved one?
First of all, you should put the patient to bed and ensure maximum peace in the room where he is located. To make breathing easier, you need to remove tight clothes (at least unfasten the collar, loosen the belt). Place a pillow (folded clothes, blanket, etc.) under the patient’s head so that the shoulders are also raised: this is necessary so that the blood flow in the vertebral arteries does not deteriorate. If blood pressure readings are above 140/90, then the patient can be given medications that lower blood pressure.
It is important to know: the neurological symptoms characteristic of cerebral hemorrhages are similar to the clinical manifestations of myocardial infarction. Sometimes diagnosis is difficult even for experienced specialists, so you should not take or give the patient numerous medications on your own: taking the wrong pills can only aggravate the condition.
How to recognize a micro-stroke
Diagnosis of this disease is based on a complete examination of the state of the cardiovascular system. Usually, for the accuracy of the diagnosis, consultation with an ophthalmologist, cardiologist, or therapist is required.
Studies that help make an accurate diagnosis include:
- Electrocardiogram (ECG),
- Echocardiogram,
- Complete blood test
- Computed tomography (CT),
- Magnetic resonance diagnostics,
- Blood clotting test (coagulogram),
- MRI (magnetic resonance imaging).
A doctor can decide how to treat a microstroke only after studying the results of the examination. Thus, the result of an electrocardiogram may indicate that the formation of a blood clot, which prevented the flow of blood to the brain, occurred in the heart. In such cases, the doctor may decide to prescribe anticoagulants. The result of an ultrasound examination of the carotid arteries can show whether there are atherosclerotic lesions of the vessels (their lumen is too narrow due to atherosclerosis). As a measure to prevent ischemia and stroke, surgery may be recommended in such situations.
Causes of stroke and risk factors
In addition to the causes of stroke, it is necessary to note those risk factors that increase the risk of developing a certain form of the disease. Preventive measures against pathology are aimed primarily at eliminating these factors in specific patients and the population of the country as a whole.
- changes in blood composition: high cholesterol and LDL;
- heart disease: heart attack, arrhythmia;
- sedentary lifestyle;
- diabetes;
- overweight;
- high blood pressure;
- old age - from 55 years and older;
- bad habits: smoking, alcoholism and drug addiction;
- blood clotting pathologies;
- carotid artery stenosis;
- excessive physical activity.
Consequences
The consequences of a micro-stroke may not be noticeable if it was experienced only once. Otherwise, brain cells begin to experience “oxygen starvation.” It leads to:
- Memory impairment;
- The appearance of dementia;
- Change of character for the worse.
Every micro-stroke a person experiences is a blow to the health of the brain, leading to premature aging.
Treatment involves restoring cerebral blood flow to the affected area. Rehabilitation after a mini-stroke begins, first of all, with studying the medical history: this allows you to identify the true cause of the disease and select appropriate medications for the recovery period.
Treatment
The drugs most often used in the complex treatment of disorders of this disease are aimed at:
- Restoration of blood microcirculation in blood vessels;
- Improving blood flow, dilating blood vessels;
- Preventing the accumulation of platelets on the walls of blood vessels;
- Improved brain activity;
- Normalization of blood pressure;
- Improving metabolic processes (blood oxygen saturation).
Recovery after a mini-stroke is aimed at preventing recurrent attacks. Treatment at the rehabilitation stage may also include physiotherapeutic procedures: massage, therapeutic exercises, circular shower, electrophoresis. In specialized centers, hirudotherapy (treatment with leeches) is often used, which helps normalize blood flow and cleanse blood vessels of blood clots.
To exclude a relapse, the patient must be observed by a doctor for some period.
What is the treatment for microstroke at home?
If the attack was caused by any chronic disease, then most of the medical therapy is aimed specifically at eliminating it. When the cause of an attack is an incorrect lifestyle, it is strongly recommended:
- Minimize stressful situations;
- Stop drinking alcohol and cigarettes;
- Normalize weight (this is also important for stabilizing blood pressure);
- Reduce the amount of salty, fatty or smoked foods you consume - nutrition after a mini-stroke should be healthy and balanced;
- Eat more fish, legumes, fresh herbs, fruits and vegetables;
- Normalize the work and rest schedule.
What to do with the consequences?
Memory impairment, general malaise, weakness in the arms and legs, difficulty swallowing, and sensory disturbances in the limbs are extremely rare consequences of several experienced transient ischemic attacks. It is also possible to develop depression and stuttering. Such conditions may require the intervention of not only doctors, but even psychologists and speech therapists.
First aid for a stroke before the ambulance arrives
It is difficult to provide first aid to yourself for a stroke. Therefore, you need to immediately call an ambulance and call relatives and neighbors.
Basic rules for what to do in case of a stroke before the ambulance arrives, if no one is nearby:
- free your chest from clothing;
- open a window in the room;
- lie on your back so that your head is higher than your body;
- do not move unless necessary.
Algorithm of what to do and how to help a person with a stroke before the ambulance arrives:
- Reassure the patient if possible . Stress aggravates the condition of the brain and contributes to the rapid progression of the disease.
- Call an ambulance at 112 or 103 from your mobile phone .
- Provide resuscitation measuresI. If a person is not breathing, then artificial respiration is given to him (see the picture).
If there is no pulse, then first aid is supplemented with artificial heart massage until the ambulance arrives. Massage technique:- the right palm is placed on the left or vice versa;
- The lower palm is placed in the chest area, and the upper palm is pressed on it at intervals of 100 times per minute. Every 30 pressures, perform artificial respiration with 2 breaths into the patient’s mouth.
- Ensure the patient's body is in the correct position . If he is conscious, then he is placed on his back, so that the chest and head are in an elevated position. If there is no consciousness, the victim is placed on his side. In this position, he will not choke on vomit and saliva.
What to do if you have a stroke at home
It is possible to give medication to a victim for a stroke only if the ambulance is delayed for more than 40 minutes. List of medications that help prevent oxygen starvation of the brain:
- Piracetam;
- Furosemide;
- Lasix.
It is better to administer drugs for a stroke attack intramuscularly. This way they will act faster.
According to WHO statistics, correctly provided first aid helps save 50-60% of patients with a severe form of stroke and 75-90% with a mild one.
Why is it dangerous to have a mini-stroke on your feet?
Many people suffer a mini-stroke (and sometimes more than one) without seeking help from doctors. The consequences of such an attitude towards one’s own health are often tragic: a critical condition increases and turns into a massive stroke, after which only a few fully recover. Even short-term and mild signs (their totality) of an attack should be a reason for immediately contacting a doctor (calling an ambulance).
It is not at all necessary that after a mini-stroke a major stroke will occur: some people suffer several successive transient ischemic attacks without encountering a severe attack in the future. When performing a CT scan in such people, small numerous changes in the brain are detected, although nothing indicates a stroke. It is worth remembering that there is a direct connection between senile dementia and the number of transient ischemic attacks experienced.
Causes of the disease
Causes of ischemic stroke
Development of ischemic stroke
The causes of ischemic stroke are divided into:
Cardioembolic - occurs as a result of blockage of the artery lumen by an embolus. A common cause of blockage is emboli that occur due to heart defects, endocarditis, and other heart pathologies accompanied by the formation of blood clots. A common cause is atrial fibrillation.
Atherothrombotic - usually manifests itself as a consequence of atherosclerosis of large and medium arteries. The plaque narrows the lumen of the vessel and is a catalyst for the formation of a blood clot. This type develops gradually and often culminates during sleep. Often the harbinger is a transient ischemic attack.
Read also: Hemorrhagic stroke recovery period
Hemodynamic – caused by a change in the normal speed of blood movement through the vessels. The onset of the hemodynamic type of the disease can be different and manifest itself both during sleep and during wakefulness.
Lacunar – damage to the small vessels of the brain. A common cause is prolonged high blood pressure.
Rheological - occurs due to changes in the properties of blood. Thrombophilia, leukemia, erythrocytosis, erythremia can lead to a rheological type of disease.
Causes of hemorrhagic stroke
- Most often develops against the background of hypertension of 2 and 3 degrees. If a patient with hypertension has endocrine pathologies in the form of a pituitary adenoma, changes in the thyroid gland, then the possibility of the disease doubles.
- Aneurysm rupture.
- Pathological processes of connective tissue, during which a violation of the elasticity and strength of blood vessels occurs.
- Hemophilia.
- Overweight.
- Bad habits.
- Changes in lipid metabolism.
- Diabetes.
- Heart diseases.
- Depressive states.
Based on the above reasons, it is clear that the difference between hemorrhagic and ischemic stroke is that most often ischemic stroke is caused by diseases accompanied by the formation of emboli and blood clots, and in hemorrhagic stroke, the main catalyst is a history of hypertension.
Transient ischemic attack: symptoms and classification
Depending on the location of the cerebral vessel blocked by the thrombus, attacks can be divided into:
- transient ischemic attack in the vertebrobasilar region: diagnosed in 70% of cases;
- acute cerebral ischemia;
- transient attack in the carotid region
Symptoms and treatment for each type of attack may vary. The following distinctive features are characteristic of a vertebrobasilar attack:
- pain in the head is acute and localized in the back of the head;
- characterized by paralysis;
- the patient makes frequent movements of the eyeballs;
- Various visual impairments are characteristic: short-term blindness, simple visual hallucinations;
- Possible short-term memory loss.
Transient cerebral ischemic attack is usually detected in infants. Transistor microstroke has the most pronounced symptoms: the child sleeps poorly, he has tremors and nervous tics, natural reflexes are reduced, and dysfunction of muscle tone is often present.
Transient microstroke occurs in newborns due to oxygen starvation during pregnancy or childbirth. Treatment in infants depends on the severity of the disease, the specificity and severity of symptoms.
Types by development mechanism
Depending on the mechanism of occurrence, there are three main groups of stroke:
- Ischemic.
- Hemorrhagic.
- Transient ischemic attack (TIA).
In turn, each type of stroke is divided within the group into subtypes.
Ischemic stroke
This species is the most common, accounting for almost 80% of recorded cases.
Often, the pathology is diagnosed in people over 50 years of age with a history of cardiovascular diseases, diabetes, rheumatism, as well as in overweight people, long-term smokers and drug addicts.
The provoking factor of ischemia is the narrowing of the lumen of the artery, due to which blood flow in the brain worsens. This leads to oxygen starvation of brain neurons, and subsequently to their death.
Ischemic stroke is classified into the following types:
Atherothrombotic - develops with atherosclerosis of medium and large arteries. The blood supply to the brain is disrupted due to atherosclerotic plaques formed on the carotid and basilar arteries.
Another reason may be blockage of the vessel by a blood clot, which is a broken piece of fatty plaque. The extent of the damage may vary.
The pathogenesis of the development of the disease is stepwise, symptoms increase over several hours and sometimes days. Most often, attacks occur at night during sleep.
It is not uncommon for acute cerebrovascular accidents to be preceded by transient ischemic attacks or multiple microstrokes.
Embolic - causes cardiogenic embolism. Its culprit is a blood clot that forms in the heart. A heart clot can break off and become trapped in an artery closer to the brain (embolism).
The formation of blood clots in the heart can occur as a result of a heart attack, rheumatoid or infective endocarditis, atrial fibrillation, or heart valve abnormalities.
In most cases, this type of stroke occurs suddenly, usually during the day, with pronounced neurological symptoms.
Lacunar - characterized by damage to the perforating arteries, as a result of which small depressions called lacunae are formed in the brain.
Their size varies from 1 to 2 cm, and there are also small gaps measuring 1 mm. Foci form in the deep parts of the brain, including the white matter, cerebellum, ganglia, and thalamus, while the cerebral cortex remains untouched.
Lacunar stroke occurs without any clinical manifestations or is quite sparse. In other words, problems with vision, speech, and breathing are practically absent, the person does not suffer from headaches, nausea, and especially vomiting.
The only symptom is persistent high blood pressure that rises several hours before the stroke. Basically, the attack occurs at night, and the victim wakes up in the morning with characteristic signs of brain damage.
A person has problems with coordination, memory, spontaneous urination, there may be cramps and unilateral weakening of muscles in several parts of the body.
This pathology often becomes a consequence of a heart attack or develops against the background of arterial hypertension. No less common causes are atherosclerosis, inflammatory lesions of blood vessels, ischemic heart disease, and problems with blood clotting.
Hemodynamic - occurs due to severe stenosis of large arteries of the head or neck with a rapid drop in blood pressure.
Bradycardia, ischemia, acute heart failure, and vascular abnormalities can lead to a similar situation.
The onset of a pathological condition can be either sudden or gradually increasing, regardless of whether the person is at rest or awake.
Lesions are possible in any part of the brain, but are most often localized in the border zones of the adjacent blood circulation.
Hemorheological microocclusion - occurs due to noticeable hemorheological changes, disturbances in the blood coagulation-hemostasis system and fibrinolysis.
This picture can be observed with erythremia, hyperglycemia, and dyslipidemia.
Other possible causes include alcohol abuse, diuretic overdose, and taking drugs that change the rheological properties of the blood. This type of stroke is characterized by mild neurological symptoms.
The ischemic type of stroke develops gradually. Therefore, usually the victim does not attach much importance to the initial symptoms, such as weakness, headache, tinnitus, absent-mindedness, blurred vision, since they can periodically disappear and the patient begins to feel well.
Despite this, the disease progresses and the ailments return, eventually causing paralysis.
Hemorrhagic stroke
Hemorrhagic stroke is characterized by bleeding in the brain. Hemorrhage occurs due to a ruptured aneurysm or weakened vessel.
The spilled blood forms a hematoma, which compresses and displaces brain tissue, and swelling appears in the affected area. The extent of the damage depends on the size of the damaged artery or vein.
The larger the vessel bursts, the more profuse the bleeding and the more serious the consequences. If a person has time to receive medical assistance in the first three hours after an attack, the chances of survival become greater.
In the vast majority of cases, this pathology occurs in people suffering from arterial hypertension. Therefore, hypertensive patients are always recommended to regularly measure their blood pressure and take all medications in a timely manner.
Other provoking factors include endocrine and cardiac diseases, cerebral vasculitis, encephalopathy, liver cirrhosis, brain tumors, and taking drugs that increase blood flow.
The peculiarity of hemorrhagic stroke is its rapid development, usually occurring during the daytime against the background of emotional or physical fatigue.
Symptoms of the pathology are manifested by sudden sharp severe pain in the head, hoarse breathing, hemorrhage in the eyes, facial paresis, paralysis of the limbs and vomiting. There may also be generalized seizures.
Based on the location of the foci of inflammation, where the vessel was damaged and a hematoma formed, the following types of hemorrhagic stroke are distinguished:
- Parenchymatous . The blood enters the thickness of the brain tissue - the parenchyma. Based on the area of hemorrhage, hemorrhages can be hemispheric, brainstem, cerebellar, or ventricular. In this case, the bleeding is very severe, which is most difficult to stop. It manifests itself as a sudden sharp headache, very often a person loses consciousness, and sometimes even falls into a coma.
- Subarachnoid. Hemorrhage occurs in the subarachnoid space, located between the arachnoid and pia mater of the brain. Most often, blood accumulates on the basal surface of the cerebral peduncles, pons, temporal lobes, and less often on the superolateral surface of the brain. It is usually registered in people aged 20-40 years and in young children. The main cause is vascular aneurysm and traumatic brain injury. Often such a defeat ends in death.
- Subdural . Blood spreads over the dura mater of the brain. In most cases, the cause is rupture of benign cystic brain tumors. At the time of the attack, a person may lose consciousness, but then there is an improvement that lasts several days, and then a sharp increase in neurological symptoms is possible.
- Subcortical. Hemorrhage in the subcortical area of the brain most often occurs due to high blood pressure. Damage to the hemispheres or individual junctions between the frontal, temporal, occipital and parietal areas of the brain is mainly noted.
- Ventricular. It is considered extremely dangerous because blood enters the ventricles of the brain. Occlusive hydrocephalus develops very quickly. The victim may instantly fall into a coma. Often accompanied by arrhythmia and breathing problems.
- Mixed . A rare phenomenon in which hemorrhages occur simultaneously in several areas.
Regardless of the area in which the bleeding occurred, the symptoms are almost the same. It is possible to reliably identify the types of hemorrhagic stroke only after a detailed examination.
This is an essential requirement for making the right decision about the advisability of surgical intervention and prescribing effective drug therapy.
The most dangerous period for hemorrhagic hemorrhage is the first day and two weeks after the attack. This time is considered the most critical, since a relapse may occur.
After 3-4 weeks, the risk of another stroke is significantly reduced.
Transient ischemic attack
The pathology is characterized by a short-term blockage of blood flow to the brain. It lasts no more than five minutes.
However, after the attack, a person may experience disturbed sleep, unexplained headaches, dizziness, problems with coordination and speech, the muscles of the arms and legs become sluggish, and they have difficulty listening.
But since the symptoms gradually subside and all body functions are restored, the victim does not even imagine that she suffered a mini-stroke. Due to the transience of the attack, many attribute such ailments to high blood pressure or bad weather.
However, this is an alarming signal warning that the main blow of a “big” stroke is not far off. For most people, it happens within a year of the first crisis.
As you know, each part of the brain is responsible for certain functions. Therefore, symptoms appear depending on the location of the lesion and its scale.
Many qualified specialists, even before hardware examination, can, based on the nature of the deviations that have arisen, guess the approximate location of the pathological focus.
Ischemic attacks are usually classified according to the location of the lesion, frequency of occurrence and severity. When examining the bloodstream, the following types of TIA are distinguished:
- Vertebrobasilar syndrome. This form is observed in 70% of patients. With such a lesion, patients complain of severe dizziness, nausea, excessive sweating, hearing loss, problems with coordination of movement, visual disturbances in which double objects and light flashes are observed. A similar picture occurs spontaneously or with a sharp turn of the head to the side.
- Hemispheric syndrome (carotid artery syndrome) - associated with atherosclerosis of the carotid arteries. It is characterized by acute pain in the back of the head and neck, weakness, nausea, tinnitus, dizziness, and possible fainting. numbness and deterioration of sensitivity of the limbs, sudden disappearance or severe deterioration of vision in one eye, which disappears after a few minutes, short-term speech disturbances are possible.
- SMA (spinal muscular atrophy). Changes in the carotid region lead to numbness and deterioration in the sensitivity of the limbs, short-term speech disturbances, sudden disappearance or deterioration of vision in one eye, which goes away after a few minutes, are possible.
- Transient global amnesia (TGA) is a unique syndrome in which a patient (usually middle-aged) suddenly loses short-term memory with relative preservation of memory for distant events.
With a mild or moderate ischemic attack, the clinical manifestations are rather mild. In such situations, an unspecified type of TIA is diagnosed.
Based on the dynamics of the disease, there are 3 degrees of TIA severity:
- Mild degree - lasts approximately 10 minutes, focal symptoms that disappear extremely quickly without consequences.
- Moderate degree - lasts more than 10 minutes, clinical manifestations can last up to several hours. They go away on their own or after special therapy. However, no negative consequences for human health are observed.
- Severe – neurological symptoms are observed for up to 24 hours. They disappear only with properly selected treatment, while some signs still remain, although they appear slightly.
Depending on the frequency of attacks, there are:
- rare - no more than 1-2 times a year;
- medium frequency - from 3 to 6 times a year;
- frequent - more than 6 times a year.
The difference between a transient attack and a regular stroke is the short duration of the disruption of cerebral blood supply.
In this case, the symptoms stop within 24 hours, since the damage is not so global and the function of the dead cells is taken over by healthy structures.
Consequences and treatment: prognosis
A favorable outcome of minor cerebral hemorrhage directly depends on the speed of timely detection of symptoms. Treatment must take place in a hospital under the constant supervision of doctors. In no case should you self-medicate or completely ignore the signs of an attack (their course can become chronic).
There is such a thing as a “silent stroke”; this is a major stroke that occurs in people who have previously suffered a transient ischemic attack. It is scary because no signs of an attack are observed, but disturbances in blood flow occur during this period, and irreversible negative processes occur in the brain cells.
Diagnostics
Preliminary differential diagnosis of different types of acute cerebrovascular accident at the prehospital stage is carried out according to the characteristics of the clinical picture. After the patient is admitted to the hospital, he is examined, based on the results of which it is possible to say exactly what form of stroke is observed in this particular case. The examination program includes the following methods:
- computed tomography or magnetic resonance imaging;
- angiography;
- lumbar puncture;
- non-invasive methods for studying the carotid arteries (plethysmography, duplex scanning, ultrasound);
- electroencephalography.
Treatment tactics depend on the type of acute cerebrovascular accident. Drug therapy for hemorrhagic stroke includes taking the following groups of drugs:
- painkillers;
- tranquilizers;
- antiemetics.
In addition, active correction of coagulopathies is carried out (prescription of protamine sulfate in case of overdose of heparin, vitamin K and fresh frozen plasma during treatment with indirect anticoagulants, platelet transfusion in case of thrombocytopenia).
For intracranial hematoma with a diameter of more than 3 cm, the issue of surgical intervention is considered.
Read also: How to get up after a stroke
The drug treatment regimen for ischemic stroke is somewhat different. It includes the following drugs:
- thrombolytics;
- anticoagulants of direct and indirect action;
- antiplatelet agents.
For any type of stroke, a whole range of general measures is carried out:
- 24-hour monitoring of the patient, since a sharp deterioration in his condition is possible at any time;
- monitoring blood pressure levels and maintaining them at an optimal level;
- adequate oxygenation;
- prevention and treatment of infectious complications;
- decrease in intracranial pressure.