Ischemic stroke
The most common form of stroke, occurring in more than 80% of cases, is ischemic stroke. This is a clinical syndrome or emergency condition that develops suddenly due to blockage of blood vessels by a thrombus or blood clot . Since blood flow is disrupted, certain areas of the brain begin to die. A kind of cerebral infarction occurs. You may also be interested in reading about what a cerebral infarction is.
The first hints of a stroke:
- A sharp attack of headache.
- Weakness , dizziness.
- Nausea , vomiting.
- Hyperhidrosis and hot flashes.
- Bradycardia.
- Numbness in one part of the body.
- Retardation, speech impairment.
In the previous article we discussed the issue of pre-stroke condition.
As the condition worsens, the following are observed:
- Fainting episode, which may periodically be accompanied by convulsions.
- loss .
- Decreased visual acuity.
- Confusion .
- defects and complete loss of speech.
- Clear asymmetry of the left and right halves of the face.
- Uneven breathing.
- Hypotension.
- failure .
- Urgent urinary incontinence.
- Paralysis or paresis of the limbs.
- loss .
Risk factors
- Arterial hypertension. The risk of cerebral infarction in patients with high blood pressure is significantly higher than in those who have normal levels. Learn more about blood pressure during stroke.
- Diseases of the cardiovascular system. The most common precursor of ischemic stroke is atrial fibrillation.
- Diabetes. With this somatic disease, all types of metabolism are disrupted, which leads to the development of atherosclerosis of large arteries, the formation of plaques and platelet aggregation.
- Advanced age. After 70 years of age, the risk of ischemic stroke is much higher than at 50 years of age.
- Alcohol abuse, smoking. Active and passive smoking contributes to the development of atherosclerosis, vascular spasm and thrombosis. And stopping smoking reduces the risk of stroke only after 4 years.
- Taking oral contraceptives. Estrogens in dosages above 50 mg are guaranteed to increase the risk of developing the clinical syndrome.
- Transient ischemic attacks.
- Obesity, high cholesterol.
Causes of the disease
Experts believe that a stroke can occur in anyone, regardless of age, but the likelihood of it happening is much higher in people over 60 years of age. This is due to the fact that they are much more likely to suffer from diseases that cause problems with blood vessels. In general, the causes of stroke in older people are similar to other age categories. These include:
- pathologies of the cardiovascular system. First of all, these include hypertension, since most people after 50 years have high blood pressure;
- disorders of the endocrine system (diabetes, obesity);
- infectious diseases in severe form. Most diseases of this type negatively affect the elasticity of the arteries, which is accompanied by tissue destruction;
- disturbance of the normal rhythm of the heart (atrial fibrillation);
- malignant tumors localized in the brain;
- diseases of the joints and muscles (for example, rheumatism);
- high blood cholesterol levels. This affects the formation of blood clots in the vessels.
Important! The risk group includes people leading a sedentary lifestyle.
Prognosis for life with ischemic stroke
To predict the further condition, it is necessary to exclude the possibility of death, assess possible complications and the likelihood of recurrent cerebrovascular accident.
Factors influencing prognosis
Key factors to consider:
- Advanced age. It contributes to a more severe course of the disease and increases the risk of death or disability.
- Location of stroke foci. If they are located in the area of vital centers, then the fatal outcome is more predictable.
- Causes of the clinical syndrome. If this is atherosclerosis, then the likelihood of repeated cerebral ischemia is very high.
- Severity of the disease. If the affected area is large, then the recovery period will be long.
- How quickly first aid was provided. If it was provided within three hours after the clinical manifestation, the prognosis becomes more favorable.
If the patient strictly follows all the recommendations of doctors and has a positive attitude (this also applies to his relatives), this will contribute to a favorable prognosis and will have a good effect on the speed of the recovery process.
Occurrence of stroke
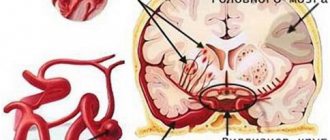
After 80 years, the likelihood of cerebral hemorrhage increases; it can be triggered by certain diseases that are common in older people:
- arterial hypertension. The main characteristic of this pathology is high blood pressure, which cannot be lowered even with the help of modern medications. In people suffering from this disease, the pressure usually remains around 140/90 mmHg, which has an extremely adverse effect on their health;
- vascular aneurysm;
- dysfunction of the endocrine system;
- kidney problems;
- diabetes;
- rheumatism;
- excessive accumulation of cholesterol on the inner walls of the vessel.
Stroke course options
Symptoms of ischemic stroke depend on the nature of the vascular basin of the damaged area. A stroke can affect the right or left hemisphere. Since the nerve bundles in the brain intersect, the lack of voluntary movements will affect the side opposite the lesion.
When the right hemisphere is damaged,
- paralysis of the left side of the body;
- speech problems;
- cautious, slow behavior;
- language memory deficit.
We have already discussed in detail the issue of ischemic and hemorrhagic stroke on the right side in another article.
When the left hemisphere is damaged, the following are observed:
- paralysis of the right side of the body;
- problems with the perception of space;
- quick, impulsive behavior;
- motor memory deficit.
You will also be interested to read about the consequences of a hemorrhagic stroke on the left side and how many people live with it.
If we take into account the consequences, the options for the course of a stroke can be divided into:
- Favorable - this is an option when the loss of consciousness was short-term, the neurological deficit is mild. With timely treatment, all impaired brain functions can be restored.
- Intermittent – this option is characterized by an emergency condition. The loss of consciousness is prolonged (sometimes a person can remain unconscious for more than three days), the neurological deficit is clearly pronounced. Another stroke is possible. The recovery period is very long with various complications.
- Progressively severe - the patient is in a coma. The condition constantly worsens and often ends in death.
Consequences of a stroke
The transferred disease has consequences that, depending on the type and course of the pathology, can remain for many years, or may disappear after a certain period of time.
Manifestations of the disease are divided into several groups:
- speech disorders. A stroke affects different parts of the brain, so the patient may experience changes in articulation or speech production;
- motor disorders. An elderly person may have impaired mobility of the limbs or mobility of the face;
- cognitive disorders. They are characterized by absent-minded attention, decreased intelligence, memory loss;
- emotional-volitional disorders. A person with such manifestations after a stroke becomes “tearful”, as a result of which he can plunge into a prolonged depressive state.
These consequences arise only after the end of the acute period of pathology. In the first weeks after a stroke, the patient has symptoms such as speech impairment, frequent headaches, unstable blood pressure, and arrhythmia. In some cases, high body temperature, tremors, and convulsions are noted.
Possible complications
The patient is guaranteed a wide variety of complications. They depend on the location of the ischemic focus and the degree of damage. The most life-threatening complication of the first days of the disease is swelling of the brain stem and the development of repeated strokes. Often complications are associated with the fact that the patient remains motionless in a supine position for a long time. This leads to bedsores, thrombosis, myocardial infarction and congestive pneumonia.
Consequences after an emergency are an integral part of the disease and you need to be prepared for them.
The most likely complications and consequences:
- Mental disorders. As a result of a stroke, a depressive state often develops. The patient feels depressed due to the restrictions that have appeared, due to the fact that he is causing inconvenience to his family. Mood fluctuations for no reason, aggressiveness, and panic are also noted.
- Loss of sensitivity in the face and limbs. Since the nerve fibers responsible for sensitivity are restored much more slowly than the nerve fibers responsible for movement, muscle strength may already return, but sensitivity will still have to wait.
- Impaired motor function . Strength in the limb will return gradually and may not be fully restored. Often people who have suffered a stroke walk with a cane and cannot independently perform usual manual manipulations.
- Cognitive impairment. The person becomes disoriented in space. Ceases to feel time, cannot sensibly assess the situation.
- Speech disorders. It is difficult for a person to express his thoughts; he speaks incoherently and in fits and starts.
- Coordination problems. There is no clarity in movements, swaying when walking, falls are possible during sudden movements and turns.
- Epilepsy. A fairly rare complication, but occurs in 10% of patients.
Symptoms
General cerebral neurological symptoms in stroke
- headache – bursting and intense
- nausea
- vomiting, often repeated and not bringing relief
- loss of consciousness - up to deep coma
- convulsive syndrome
Although the group of general cerebral symptoms is more typical for hemorrhagic stroke, in its ischemic version it also occurs, mainly with extensive hemispheric strokes, accompanied by the capture of large areas of the brain matter.
In older people, such extensive IS occurs as a result of thrombosis or embolism of large cerebral arteries, such as the internal carotid, middle cerebral, in combination with the anterior or posterior cerebral arteries.
Focal neurological symptoms
The appearance of focal symptoms will depend on the location and size of the ischemic stroke focus in the brain. In older people or other age groups, this is equally important; the persistence and severity of neurological symptoms, as well as the prognosis for future recovery, depend on it.
Depending on the location of the lesion, brainstem neurological symptoms are distinguished:
- bulbar syndrome, which includes: dysphagia - impaired swallowing, dysphonia - impaired sound pronunciation, dysarthria - impaired speech articulation.
- Loss of motor coordination: cerebellar ataxia
- oculomotor disorders - damage to the 3rd, 4th, 6th pairs of cranial nerves
- power paresis - hemiparesis (involvement of 2 limbs: arms and legs of one half of the body), up to the development of tetraparesis or tetraplegia (involvement of all 4 limbs)
Hemispheric neurological symptoms:
- power paresis - mainly hemi-type
- speech disorders
- prosoparesis - decreased strength of facial muscles
- visual disturbances with loss of visual fields
- sensory disorders - from reduction to loss of sensitivity in the side of the body opposite to the affected hemisphere, mainly disorders of surface sensitivity
- deep sensitivity disorders (sensitive ataxia)
- disorders of praxis (the ability to perform conscious, coordinated movements), with the development of apraxia - in this case, a person finds it difficult to comb his hair, fasten buttons, bring a spoon to his mouth, open the door with a key, etc.
- disorders of higher brain functions (writing, reading, counting, etc.)
- coordination and vestibular disorders - the patient cannot stand and sit straight, begins to fall to the side, and appears unsteady when walking
These are the main and most common neurological disorders in stroke in older people. They are not the only ones; their character will directly depend on the localization of the lesion - in which lobe of which hemisphere (hemisphere) it is located, and also whether it affects the cerebral cortex.
Example - for example, acute cerebrovascular accident in the basin of the left middle cerebral artery or the right anterior cerebral artery, etc.
According to the clinical course, stroke is divided into
https://insultu-net.ru
- small – with complete disappearance of symptoms within three weeks from the onset of the disease;
- with persistent residual effects - with preservation of the clinical picture for more than one month from the onset of the disease.
In addition, according to the mechanism of development (TOAST classification), the following subtypes of ischemic stroke are distinguished:
- Atherothrombotic, occurs most often (up to 50%) among all ischemic strokes. It is due to the fact that an atherosclerotic plaque exists in the vascular bed for a long time, in its place a blood clot forms. Thus, this subtype occurs due to atherosclerosis of cerebral vessels and subsequent blockage of them by a blood clot.
- Cardioembolic, accounts for up to 20% of strokes. With it, emboli (particles that do not occur normally) formed in the body from the heart through the bloodstream enter the cerebral vessels and clog them. This situation is possible with atrial fibrillation, previous myocardial infarction, dilated cardiomyopathy, artificial valves, and infective endocarditis.
- Lacunar, caused by pathological changes in arterioles in diseases such as diabetes mellitus and arterial hypertension. Occurs in 25% of cases.
- Stroke of the hemorheological microocclusion type, associated with an increase in blood viscosity, as well as an increase in the ability of platelets to stick together.
- Hemodynamic, developing under the influence of cardiac conditions in which the amount of blood ejected by the heart decreases against the background of narrowing of one of the vessels of the brain. For example, with paroxysmal arrhythmias and collapse.
Hemorheological and hemodynamic strokes together account for up to 5% of cases of the disease.