Clinical methods for studying the oculomotor system
are mainly used to diagnose the initial stages of paresis of the nerves innervating the eye muscles, especially in cases where patients complain of double vision, but there is a noticeable deviation of the eye.
In concomitant strabismus, the use of these methods is limited; they are used to determine the participation of the paretic component in its origin. It should be remembered that with long-term strabismus, secondary changes in the muscles of the eye can simulate signs of paresis. It is very difficult to differentiate these conditions, therefore, when identifying such signs, it is better to talk about muscle insufficiency, keeping in mind that this term can hide both its true paresis and secondary weakness.
In preschool children, the state of the oculomotor system is judged by the degree of eye mobility in different directions (determination of the visual field). In older children, coordimetry and “provoked” diplopia methods can be used for this purpose.
A simplified way to determine the field of view is as follows.
The patient sits opposite the doctor at a distance of 50-60 cm. The doctor fixes the patient’s head with his left hand and invites him to follow with each eye in turn (the other eye is covered at this time) the movement of an object in 8 directions (pencil, manual ophthalmoscope, etc.), which he holds in his right hand. Muscle deficiency is judged by the limitation of eye mobility in one direction or another. In this case, use the rules given in table. 14.
Table 14. Rules for determining the affected muscle when eye mobility is limited
Using this method, only severe limitations in eye mobility can be identified. A simplified method for determining the field of view allows you to obtain clearer results in case of insufficiency of the vertical muscles. If there is a visible vertical deviation of one eye, a simple abduction method can be used to identify the paretic muscle. It is based on the fact that the lifting and lowering action of the oblique muscles is most pronounced in the adduction position of the eye, and the rectus muscles - in the abduction position. The patient is asked to look at an object, move it to the right and left, and observe whether the vertical deviation increases or decreases with extreme deviations of gaze. The rules for determining the affected muscle are given in table. 15.
Table 15. Rules for determining the affected muscle by the method of abduction - adduction
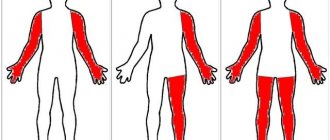
Examples of determining the affected muscle using this method are presented in Fig. 47. A unilateral increase in eye deviation in the abduction or adduction position, as a rule, indicates muscle paresis, a symmetrical bilateral increase indicates vertical phoria.
Rice. 47. Paresis of the superior oblique muscle of the right eye. The upward deviation of the right eye is especially pronounced in the adduction position
Coordimetry method
is based on separating the visual fields of the right and left eyes using red and green filters colored in complementary colors. When these colors are superimposed on each other, the effect of completely blanking the image occurs. The method makes it possible to judge the localization in space of the image of both eyes during strabismus.
Let's turn to Fig. 48. The right eye fixes the luminous point O. The visual line of the left, squinting eye is deviated from the point of fixation to the right by 20° and is directed to point O1. Obviously, the image of point O will be located in the nasal half of the retina of the squinting eye, 20° from the central fovea. As is known, with a normally functioning visual analyzer, an image located 20° inward from the central fovea of the retina is projected in space 20° outward from the point of fixation.
Rice. 48. Options for localizing an image with a squinting eye. Explanation in the text
By association with these habitual spatial relationships, the patient falsely places the image of point O with his left eye at the corresponding angle towards the temple, and it turns out to be located at point O2. Now let’s put a red glass on the patient’s right eye, and a green glass on the left. Then we will direct a green beam of light to point O, give the patient a red flashlight and ask him to combine its beam with point O. For this to happen, the patient must obviously direct the beam of red light to point O2. This principle is the basis of coordimetry.
To conduct the study, you must have a graphic screen (1), red (2) and green (3) flashlights and red-green glasses (4) (Fig. 49). The study is performed in a darkened room, on one of the walls of which there is a screen divided into small squares. The dimensions of the screen are 2X2 m, each square is 5.25X5.25 cm. With such ratios, the study is carried out from a distance of 1 m. In this case, the side of each square is equal to three angular degrees. In the central part of the screen there are nine marks placed in the form of a square, the position of which corresponds to the isolated physiological action of the oculomotor muscles. A patient wearing red-green glasses sits at a distance of 1 m from the screen.
Rice. 49. Set for coordimetry. Explanation in the text
To examine the right eye, the patient is given a red flashlight (red glass in front of the right eye). The doctor holds a green flashlight in his hands, the beam of light from which he directs one by one to all nine points and invites the patient to combine the light spot from his red flashlight with it. When trying to combine both light spots, the examinee usually makes a mistake by some amount. The position of the fixed green and trimmed red spots is recorded by the doctor on a diagram (sheet of graph paper), which is a reduced copy of the screen.
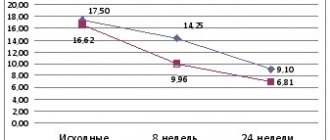
Results of coordimetric examination of one eye
do not allow us to judge the state of the oculomotor system. It is necessary to compare the results of coordimetry of both eyes with the position of all nine fixation points. For this purpose, the doctor and the patient exchange flashlights, and the study is repeated. When analyzing the data obtained, it is necessary to remember that insufficiency of the activity of any muscle leads to a change in the field of view of one or both eyes, therefore it differs from the square of fixation. The field is shortened in the direction of action of the weakened muscle. At the same time, there is usually a compensatory increase in the tracking field of the second eye towards the synergist of the affected muscle. Examples of recording results and coordimetric studies are presented in Fig. 50 and 51.
Rice. 50. Results of coordimetric study: paresis of the superior rectus muscle of the left eye
Method for studying the oculomotor system in conditions of “provoked” diplopia
is based on an assessment of the relative position in space of images belonging to the fixating and rejected (affected) eye. Diplopia is caused by placing a red glass over one eye. This allows you to simultaneously determine which of the double images belongs to the right and which to the left eye.
Rice.
51. Results of a coordimetric study: paresis of the external rectus muscle of the right eye
The study is usually carried out by moving a light source located at a distance of 2-3 m in front of the patient in horizontal, vertical and oblique directions. The study can be performed with a stationary light source, changing the direction of gaze by turning or tilting the patient's head. It must be remembered that the movement of the eyes is opposite to the movement of the head.
To conduct research, it is more convenient to use a black screen measuring 1.5X1.5 m. Nine horizontal slits, 8 cm long and 0.4 cm wide, are cut in the screen. The distance between the slits horizontally is 30 cm, vertically 40 cm. Behind each slits there are two light bulbs that turn on on a portable control panel.
The study is carried out in a dimly lit room.
The patient is seated opposite the screen at a distance of 50 cm. His head should be motionless, his eyes should be at the level of the middle of the screen. Red glass is placed in front of the squinting eye. The patient holds a pointer in his hands, with chalk attached to the end. The doctor turns on one or another light bulb in a certain sequence. The patient is asked to look at the glowing slit. At the same time, he sees two stripes (red and white) and marks the position of the red stripe with chalk on the screen. At the end of the study, the distance between the slit and the false image is measured in nine viewing directions. The data is transferred to a diagram, which is a miniature screen (Fig. 52 and 53).
Rice. 52. Results of the study using the “provoked” diplopia method: paresis of the external rectus muscle of the left eye
When assessing the results of a study, the following rules are used:
1) the muscle of the eye whose image moves further from the middle horizontal or vertical line is affected (virtual image); 2) the virtual image is always projected in the direction of action of the paralyzed muscle, therefore the same-named diplopia occurs when the muscles that deflect the eye outward are damaged, and the opposite diplopia occurs when the adductor muscles are damaged; 3) the distance between double images increases as the gaze moves towards the action of the affected muscle.
Rice. 53. Results of the study using the “provoked” diplopia method: paresis of the superior oblique muscle of the left eye
What is abducens nerve palsy?
Paresis of the abducens nerve of the left eye and the right eye occurs with the same frequency. In most cases, the disease affects one side, rarely both. Paresis of the abducens nerve can be suspected by characteristic features: the patient has difficulty turning his eye towards the affected nerve. Paresis of the abducens nerve impairs the function of the rectus lateralis muscle, and the patient cannot fully avert the eye to the side. The patient experiences diplopia when looking straight ahead, which intensifies when the eye is turned towards the affected side. Other symptoms of abducens nerve palsy include:
- forced position of the head (impaired vision leads to an attempt to adapt to the changes that have arisen, which provokes the occurrence of involuntary positions);
- uneven gait (also associated with visual impairment);
- loss of orientation;
- dizziness.
Prevention
To avoid paralysis of the muscles and nerves of the left or right organ of vision, head and face injuries should be avoided. People who have problems with the heart or blood vessels are advised to undergo a routine examination by a doctor and carefully take prescribed medications. It is necessary to avoid stress - one of the main causes of stroke, which leads to paralysis of the eye structures. All chronic diseases that can cause pathology should be kept in remission.
The combination of neurological pathologies of the visual apparatus poses a great danger to humans, so it is important to monitor not only the state of vision, but also the health of the eye itself. One of the most serious diseases in this regard is paresis of the oculomotor nerve, which causes paralysis of the eyeball and other complications. In turn, the problem can only be a symptom of other diseases. It is difficult to treat and stop, so when you detect the first signs of a disorder, it is important to consult a doctor as soon as possible.
Why does abducens ophthalmic nerve paresis occur?
Paresis of the abducens ophthalmic nerve is a consequence of any disease in the head, central nervous system, or other organs and systems. Paresis of the abducens ophthalmic nerve can be caused by:
- infectious and inflammatory diseases of the brain (encephalitis, meningitis);
- infectious and inflammatory diseases such as syphilis, diphtheria, influenza, etc.;
- severe intoxication (alcohol, drugs, chemicals);
- botulism;
- stroke;
- heart attack in the head area;
- otolaryngological diseases;
- tumors in the brain;
- increased intracranial pressure;
- diabetes mellitus (in which the functioning and structure of blood vessels is disrupted);
- multiple sclerosis.
What is ophthalmoplegia, its types and treatment methods
The optic nerve belongs to the cranial peripheral nerves, but essentially it is not a peripheral nerve either in origin, or in structure, or in function.
This is the white matter of the cerebrum, the pathways that connect and transmit visual sensations from the retina to the cerebral cortex. The optic nerve delivers nerve messages to the area of the brain responsible for processing and perceiving light information. It is the most important part of the entire process of converting light information.
Its first and most significant function is the delivery of visual messages from the retina to the areas of the brain responsible for vision. Even the smallest injuries to this area can have serious complications and consequences.
Optic atrophy according to the ICD has ICD code 10
How does oculomotor nerve palsy manifest?
The most negatively affecting the functioning of the visual organs is paresis of the oculomotor nerve. Symptoms of the disease will be pronounced and will allow the doctor to suspect this pathology. The oculomotor nerve performs a very important function in eye movement. It provides the work of the superior, inferior and medial rectus muscles, the inferior oblique muscle, and the muscle responsible for raising the upper eyelid. The oculomotor nerve innervates the sphincter of the pupil, ensuring its response to light (constriction and dilation). Therefore, if the oculomotor nerve is damaged, performing many eye movements becomes impossible.
Patients experience double vision, the pupil does not respond to light, ptosis develops, difficulty opening and closing the eye, and difficulty moving the eye.
Rarely, only the oculomotor nerve is affected. Usually the condition is accompanied by disruption of the abducens, trigeminal and lateral nerves. The pathology occurs against the background of diabetes mellitus, arterial hypertension, brain cancer, microinfarctions of the head vessels, and strokes.
Symptoms of atrophy
Drug treatment
In order to reduce pain, relieve spasms and strengthen muscles, acupuncture, electrophoresis and phonophoresis with medications are prescribed.
Since the optic nerve carries visual images, the most common signs of its inflammation are the following:
- sudden deterioration of vision in one or both eyes;
- the appearance of black and white vision. Color vision, being more perfect, suffers first;
- Pain appears when moving the eyes. An optional symptom that may be absent if there are no signs of classic inflammation and swelling of the retrobulbar tissue;
The main sign of optic nerve atrophy is a decrease in visual acuity that cannot be corrected with glasses and lenses.
- With progressive atrophy, a decrease in visual function develops over a period of several days to several months and can result in complete blindness.
- In the case of partial atrophy of the optic nerve, pathological changes reach a certain point and do not develop further, and therefore vision is partially lost.
With partial atrophy, the process of vision deterioration stops at some stage, and vision stabilizes. Thus, it is possible to distinguish between progressive and complete atrophy.
Paresis of the oculomotor nerve and abducens nerve: treatment in Moscow
The main method of treatment for paresis of the oculomotor and abducens nerve is the elimination of the disease that caused it. The Yusupov Hospital provides comprehensive treatment for this pathology, which helps eliminate the underlying disease and its consequences. Before prescribing therapy, the patient undergoes a thorough examination, which will help identify the underlying disease and the extent of nerve damage. At the Yusupov Hospital, diagnostics are performed using the latest high-precision equipment, which allows us to determine the cause of the disease even in the most difficult cases. After making a diagnosis and determining the condition of the patient’s body, the doctor draws up the most optimal treatment strategy.
Complex treatment of paresis of the oculomotor and abducens nerve will include drug therapy (drugs are selected depending on the type of underlying disease) and rehabilitation. The course of physiotherapy and rehabilitation is carried out in a specialized center at the Yusupov Hospital, where experienced specialists work in the field of restoring lost functions. Without a course of rehabilitation, paresis of the oculomotor and abducens nerves may resolve within 2-3 months after getting rid of the underlying disease. A rehabilitation course at the Yusupov Hospital allows you to speed up the process of restoring lost functions, contributes to the effective elimination of the consequences of the disease, the patient’s speedy recovery and return to a full life.
You can make an appointment with neurologists, rehabilitation specialists, physiotherapists and other clinic specialists, get information about the work of the neurology clinic, rehabilitation, or clarify other questions of interest by calling the Yusupov Hospital.
Prices for services *
*The information on the site is for informational purposes only. All materials and prices posted on the site are not a public offer, defined by the provisions of Art. 437 Civil Code of the Russian Federation. For accurate information, please contact the clinic staff or visit our clinic. The list of paid services provided is indicated in the price list of the Yusupov Hospital.
*The information on the site is for informational purposes only. All materials and prices posted on the site are not a public offer, defined by the provisions of Art. 437 Civil Code of the Russian Federation. For accurate information, please contact the clinic staff or visit our clinic.
The presence of double vision in a patient with sufficient visual acuity implies involvement of the eye muscles or oculomotor nerves or their nuclei in the pathological process. Deviation of the eyes from the neutral position (squint) is always noted and can be detected by direct examination or using instruments. This paralytic strabismus can occur with the following three lesions:
A. Damage at the muscle level
or mechanical damage to the orbit:
- Ocular form of muscular dystrophy.
- Kearns-Sayre syndrome.
- Acute ocular myositis (pseudotumor).
- Orbital tumors.
- Hyperthyroidism.
- Brown's syndrome.
- Myasthenia gravis.
- Other causes (orbital trauma, dysthyroid orbitopathy).
B. Damage to the oculomotor
(one or more) nerves:
- Injury.
- Compression by a tumor (often parasellar) or an aneurysm.
- Arteriovenous fistula in the cavernous sinus.
- General increase in intracranial pressure (abducens and oculomotor nerves).
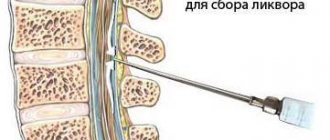
- After lumbar puncture (abducens nerve).
- Infections and parainfectious processes.
- Tolosa-Hunt syndrome.
- Meningitis.
- Neoplastic and leukemic infiltration of meningeal membranes.
- Cranial polyneuropathy (as part of Guillain-Barré syndrome, isolated cranial polyneuropathy: Fisher syndrome, idiopathic cranial polyneuropathy).
- Diabetes mellitus (microvascular ischemia).
- Ophthalmoplegic migraine.
- Multiple sclerosis.
- Isolated lesion of the abducens nerve or oculomotor nerve of an idiopathic nature (completely reversible).
C. Damage to the oculomotor nuclei:
- Vascular strokes (VAS) in the brain stem.
- Brain stem tumors, especially gliomas and metastases.
- Trauma with hematoma in the brain stem area.
- Syringobulbia.
A. Lesion at the muscular level or mechanical damage to the orbit
Such processes can lead to impaired eye movements. With the slow development of the process, double vision is not detected. Muscle damage can be slowly progressive (oculomotor dystrophy), rapidly progressive (ocular myositis), sudden and intermittent (Brown's syndrome); it can be of varying intensity and different localization (myasthenia gravis).
The ocular form of muscular dystrophy progresses over the years, always manifests itself as ptosis, and later the neck and shoulder muscles are involved (rarely).
Kearns-Sayre syndrome, which includes, in addition to slowly progressive external ophthalmoplegia, retinal pigmentary degeneration, heart blocks, ataxia, deafness and short stature.
Acute ocular myositis, also called orbital pseudotumor (increases rapidly during the day, usually bilateral, periorbital edema, proptosis (exophthalmos), pain.
Orbital tumors. The lesion is unilateral, leads to slowly increasing proptosis (exophthalmos), limitation of movements of the eyeball, and later to disruption of the pupillary innervation and involvement of the optic nerve (visual impairment).
Hyperthyroidism is manifested by exophthalmos (with severe exophthalmos, sometimes there is a limitation in the range of movements of the eyeball with double vision), which can be one-sided; positive Graefe symptom; other somatic symptoms of hyperthyroidism.
Brown's syndrome (strongrown), which is associated with mechanical obstruction (fibrosis and shortening) of the tendons of the superior oblique muscle (sudden, transient, recurring symptoms are noted, the inability to move the eye upward and inward, which leads to double vision).
Miasthenia gravis (involvement of the eye muscles with varying localization and intensity, usually with severe ptosis, worsening during the day, usually involving the facial muscles and swallowing disorders).
Other causes: orbital trauma involving muscles: dysthyroid orbitopathy.
Bilateral lesion
It occurs more often with increased ICP, or intracranial pressure, and causes convergent strabismus. The diagnosis is confirmed by ophthalmoscopy when a congestive optic disc is detected.
With such a lesion, pathology often occurs, expressed in the displacement of brain tissue towards solid formations, and compression of the abducens nerves occurs.
Other types of brain dislocation can cause the death of the patient.
Fortunately, nerve damage is not an irreversible process and doctors give patients hope for a positive treatment outcome.
The abducens nerve (nervus abducens) is the fourth pair of cranial nerves that passes through the lateral rectus muscle and is responsible for abduction and movement of the eyeball.
B. Damage to the oculomotor (one or more) nerves:
Symptoms depend on which nerve is affected. Such injuries cause paralysis that is easily recognized. With paresis of the oculomotor nerve, in addition to strabismus, mild exophthalmos may be observed, caused by hypotonia of the rectus muscle with preserved tone of the oblique muscles, which contribute to the protrusion of the eyeball outward.
The following causes may lead to damage to one or more oculomotor nerves:
Trauma (history is helpful) sometimes results in bilateral orbital hematomas or, in extreme cases, rupture of the oculomotor nerve.
Compression by a tumor (or giant aneurysm), especially a parasellar one, causes slowly increasing paresis of the extraocular muscles and is often accompanied by involvement of the optic nerve, as well as the first branch of the trigeminal nerve.
Other space-occupying lesions, such as supraclinoid or infraclinoid aneurysms of the carotid artery (characterized by all of the above, slowly increasing involvement of the oculomotor nerve, pain and sensory loss in the area of the first branch of the trigeminal nerve, rarely calcification of the aneurysm, which is visible on a simple x-ray of the skull; later - acute subarachnoid hemorrhages).
An arteriovenous fistula in the cavernous sinus (a consequence of repeated trauma) ultimately leads to pulsating exophthalmos, a pulse-synchronous noise that is always heard, congestion in the conjunctival veins and in the fundus. When the oculomotor nerve is compressed, the early symptom is mydriasis, which often appears before paralysis of eye movements.
General increase in intracranial pressure (usually the abducens nerve is involved first, later the oculomotor nerve).
After lumbar puncture (after it, a picture of damage to the abducens nerve is sometimes noted, but with spontaneous recovery).
Infections and parainfectious processes (spontaneous recovery is also noted here).
Tolosa-Hunt syndrome (and paratrigeminal Roeder syndrome) are very painful conditions that present with incomplete external ophthalmoplegia and sometimes involvement of the first branch of the trigeminal nerve; characterized by spontaneous regression within a few days or weeks; steroid therapy is effective; relapses are possible.
Meningitis (includes symptoms such as fever, meningism, general malaise, damage to other cranial nerves; it can be bilateral; cerebrospinal fluid syndrome).
Neoplastic and leukemic infiltration of the meningeal membranes is one of the known causes of damage to the oculomotor nerves at the base of the brain.
Cranial polyneuropathies as part of spinal polyradiculopathies of the Guillain-Barre type; isolated cranial polyneuropathy: Miller Fisher syndrome (often manifests itself only in bilateral incomplete external ophthalmoplegia; ataxia, areflexia, paralysis of the facial muscles, protein-cell dissociation in the cerebrospinal fluid are also noted), idiopathic cranial polyneuropathy.
Diabetes mellitus (an uncommon complication of diabetes, observed even in its mild form, the oculomotor and abducens nerves are usually involved, without pupillary disorders; this syndrome is accompanied by pain and ends with spontaneous recovery within 3 months. It is based on microvascular ischemia of the nerve.
Ophthalmoplegic migraine (a rare manifestation of migraine; a history of migraine helps the diagnosis, but other possible causes must always be excluded).
Multiple sclerosis. Damage to the oculomotor nerves is often the first symptom of the disease. Recognition is based on generally accepted diagnostic criteria for multiple sclerosis.
Idiopathic and completely reversible isolated lesion of the abducens nerve (most often found in children) or oculomotor nerve.
Infectious diseases such as diphtheria and intoxication due to botulism (swallowing paralysis and impaired accommodation are noted).
Course of therapy
Treatment methods for paresis of the eye muscles in children are not particularly different from those in adults. However, it must be borne in mind that most congenital anomalies are corrected through surgery. If the operation is successfully performed, the extraocular muscles are partially or completely restored. If the problem is compression of the nerve pathway, then the main task is to eliminate the cause.
After eliminating the factor influencing the development of muscle paresis, treatment is adjusted towards restoring blood flow and damaged nerve fibers. For this purpose, exercises that strengthen the oculomotor muscles are often used. They serve as the basis for the treatment of minor injuries and are a good preventive measure. In severe cases of the disease, therapeutic exercises well complement the main course of therapy.
Drug therapy for paresis may include the following:
- Vitamin complexes;
- Preparations for strengthening the extraocular muscles and restoring their innervation;
- Eye drops;
- Medicines that improve blood circulation;
- Corrective glasses and bandages.
The pathology can be treated with medications only according to the regimen prescribed by the doctor, so as not to aggravate its course and not to impair vision, especially if the child is sick. It is recommended to combine drug therapy with other methods, namely:
- Steriopictures. By watching them, the extraocular muscles are trained and blood flow improves. The nerve tissues that innervate the muscles of the eye are extremely tense during the procedure, due to this the lost innervation is restored. The procedure must be carried out under the supervision of a specialist so as not to cause complications;
- Electropheresis. This physiotherapeutic procedure is carried out with a 1.5% solution of Neuromidin. The duration of one session of electropheresis usually does not exceed 20 minutes, and it acts directly on the synapses (junctions) of the muscle and nervous tissue of the eyeball. After a course of such therapy, the patient’s severity of paresis decreases and the innervation of the eye muscles improves.
It is impossible to eliminate some causes of paresis in children, for example, congenital anomalies, without surgical intervention. Their duration and degree of risk depend on the type of operation and the factor that influenced the development of the pathology. In the case of severe damage to the optic nerves, it will not be possible to completely eliminate the problem, but there will be a chance to save the child’s vision.
Due to paresis of the extraocular muscles, many complications develop, such as strabismus, ptosis, etc. In children, this pathological process is often a consequence of congenital anomalies. It may not appear immediately, but only over time. This is why it is important to see an ophthalmologist and other doctors, especially in the first years of a child’s life.
In the oculomotor nerve, which is mixed, the nuclei lie on the cerebral aqueduct, in the covering of the cerebral peduncles, at the level of the superior colliculi of the midbrain roof.
From the medulla, the oculomotor nerve enters the zones of the medial surface of the peduncle, in the interpeduncular fossa, at the base of the brain at the anterior edge of the pons.
Next, the oculomotor nerve is placed between the posterior cerebral artery and the superior cerebellar artery, and through the dura mater and the superior wall of the cavernous sinus it enters the orbital cavity outside the internal carotid artery through the superior orbital fissure.
Before entering the orbit, the nerve divides into superior and inferior branches.
This nerve activates four of the six extraocular muscles, which is responsible for the movement of the eyeball - adduction, descent, elevation and rotation.
Complete nerve damage has characteristic syndromes. For example, ptosis, or drooping eyelid, or divergent strabismus, in which there is a fixed position of the eye, and the pupil is directed outward and slightly downward, since the muscles that are innervated by the fourth and sixth pairs of cranial muscles do not meet resistance.
Double vision, or diplopia, is a subjective phenomenon that occurs when the patient looks with both eyes. This effect increases if you fix your gaze on a nearby object, or when you try to turn your gaze towards the internal rectus muscle of the eye, which is paralyzed. In both eyes, the object being focused is located on inappropriate areas of the retina.
Pupil dilation (mydriasis) and lack of pupillary response to light and accommodation is also one of the symptoms of the disease and is due to the fact that this nerve is part of the reflex arc of the pupillary reflex to light.
With accommodation paralysis, there is deterioration in vision at close distances.
Accommodation of the eye is a change in the refractive power of the eye, necessary for the possibility of perceiving objects that are located at different distances from it. Accommodation is determined by the state of the curvature of the lens, which is also regulated by the intrinsic muscle of the eye innervated by the oculomotor nerve. When this nerve is damaged, paralysis of accommodation occurs.
There is also convergence palsy, in which it is impossible to turn the eyeballs inward, as well as restrictions in the movement of the eyeball down, up, and inward, as a result of paralysis of the muscles innervated by the oculomotor nerve.
The most common causes of damage to both the nucleus and the passing fibers of the abducens nerve are tumors, infarction, hemorrhage, multiple vascular sclerosis and malformations.
Treatment of oculomotor nerve palsy
Treatment of oculomotor nerve paresis consists of eliminating the underlying cause, but often this cause is extremely difficult to find out, even with a comprehensive examination. Most cases are still caused by microinfarctions, which are not uncommon in diabetes mellitus or other diseases in which microcirculation disturbances are observed. In some cases, the disease develops as a result of infection, in particular, this can happen after the flu.
Temporary use of prisms or a bandage may reduce diplopia until the paralysis subsides. If the necessary improvement is not observed, an operation is prescribed, which in most cases restores its position, at least in the basic position. If nerve function cannot be restored, re-treatment is prescribed to search for hidden causes, which may be chordomas, carotid-cavernous fistula, diffuse tumor infiltration of the meninges, myasthenia gravis.
C. Damage to the oculomotor nuclei:
Since the oculomotor nuclei are located in the brain stem among other structures, damage to these nuclei is manifested not only by paresis of the external eye muscles, but also by other symptoms, which makes it possible to distinguish them from damage to the corresponding nerves:
Such disorders are almost always accompanied by other symptoms of central nervous system damage and are usually bilateral.
In nuclear oculomotor palsy, the different muscles innervated by the oculomotor nerve rarely exhibit the same degree of weakness. Ptosis usually appears only after paralysis of the external eye muscles (“the curtain falls last”). The intrinsic eye muscles are often spared.
Internuclear ophthalmoplegia leads to strabismus in a certain direction of gaze and diplopia when looking to the side. Most common reasons
nuclear eye movement disorders are:
CVA in the brainstem (sudden onset, accompanied by other brainstem symptoms, mainly cross-symptoms and dizziness. Brainstem symptoms, usually including nuclear oculomotor disorders, are manifested by well-known alternating syndromes.
Tumors, especially stem gliomas and metastases.
Traumatic brain injury with hematoma in the brain stem area.
Syringobulbia (does not progress for a long period, there are symptoms of damage along the length, dissociated sensitivity disorders on the face).
Double vision can also be observed in some other lesions, such as chronic progressive ophthalmoplegia, toxic ophthalmoplegia due to botulism or diphtheria, Guillain-Barré syndrome, Wernicke encephalopathy, Lambert-Eaton syndrome, myotonic dystrophy.
Finally, diplopia has been described in cases of clouding of the lens, incorrect correction of refraction, and diseases of the cornea.
Symptoms and signs of damage
In the early stages of oculomotor nerve paresis, there are practically no symptoms, which complicates its diagnosis and further treatment. With a longer course of the disease, the following symptoms gradually begin to appear:
- Drooping of the upper eyelid (partial or complete);
- Lack of reaction (constriction/dilation) of the pupil;
- Diplopia (double vision due to loss of motor ability of the eye);
- Divergent strabismus (occurs due to lack of resistance of the upper and lower muscles of the eyeball);
- Loss of focusing and adaptation to changes in the distance between the eye and the object;
- Loss of motor ability;
- Protrusion of the eye.
With extensive damage, immobility can become only part of the entire symptomatology of the disease if other cranial nerves are also damaged. In addition, oculomotor nerve palsy itself may be a symptom of a more serious systemic disease. Most often, the lesion affects only one eye.
D. Monocular double vision (double vision when looking with one eye)
Monocular diplopia is always intriguing to the neurologist. This condition can often be either psychogenic or caused by a refractive error in the eye (astigmatism, impaired transparency of the cornea or lens, dystrophic changes in the cornea, changes in the iris, a foreign body in the media of the eye, a defect in the retina, a cyst in it, defective contact lenses).
Other Possible Causes
(rare): damage to the occipital lobe (epilepsy, stroke, migraine, tumor, trauma), tonic gaze deviation (common), disruption of the connection between the frontal visual field and the occipital region, palinopsia, monocular oscillopsia (nystagmus, mokymia of the superior oblique muscle, eyelid twitching )
Double vision in the vertical plane
This situation doesn't happen often. Its main reasons:
orbital base fracture involving the inferior rectus muscle; thyroid orbitopathy involving the inferior rectus muscle, ocular myasthenia, damage to the third (oculomotor) cranial nerve, damage to the fourth (trochlear) cranial nerve, skew deviation, myasthenia.
More rare causes:
orbital pseudotumor; myositis of the oculomotor muscles; primary orbital tumor; entrapment of the inferior rectus muscle; third nerve neuropathy; aberranetic reinnervation in case of damage to the third nerve; Brown's syndrome (strongrown) is a form of strabismus caused by fibrosis and shortening of the tendon of the superior oblique muscle of the eye; double elevator paralysis; chronic progressive external ophthalmoplegia; Miller Fisher syndrome; botulism; monocular supranuclear gaze palsy; vertical nystagmus (oscillopsia); myokymia of the superior oblique muscle of the eye; dissociated vertical deviation; Wernicke's encephalopathy; vertical one and a half syndrome; monocular vertical diplopia.
The movement of the eye is controlled by six motor muscles, which receive nerve impulses from three paired nerves of the skull:
- the oculomotor nerve supplies the internal, superior nerves, penetrates the inferior rectus muscle and penetrates the inferior oblique muscle;
- the trochlear nerve innervates the superior oblique muscle;
- The abducens nerve penetrates with its fibers into the external rectus (lateral) muscle.
The abducens nerve “supports” the eye
A nerve called the abducens nerve plays a small regulatory role in eye motility by retracting it outward. These nerve fibers enter the oculomotor apparatus of the organ and, together with other nerves, control complex eye movements.
The eye can turn from side to side horizontally, make circular movements, and move in a vertical direction.
Abducens nerve function
The nerve originates in the nucleus, located in the middle part of the medulla. Its fibrous structure crosses the pons and the brain center, passing its surface, called the basal. Then the path of the fibers flows along a groove located in the medulla oblongata.
Next, the fibrous threads of the nerve cross the membrane of the brain region, pass close to the carotid artery, move to the upper part of the orbital fissure and end their path in the orbit, firmly attached to the eye.
Nerve fibers control the rectus externus (lateral) muscle, which moves the eye outward and makes it possible to move the eyes to the sides without turning the head. The muscle is the opposite of the internal muscle tissue that pulls the eye toward the center. They balance each other out.
If one of the two muscles is affected, it develops, since the other muscle pulls the eye organ towards itself, and the affected one cannot maintain balance. It is impossible to check the abducens nerve in isolation; it is examined together with the other two nerves.
Anatomy
The abducens nerve is a pure motor nerve. It begins in the nucleus, which is located in the midbrain. Its fibers descend through the bridge to the basal surface of the brain and move further along the groove between the pyramids located in the medulla oblongata.
The processes of the nucleus pass through the membranes of the brain and end up in the cavernous sinus. There the fibers are located on the outside of the carotid artery. After the nerve has left the sinus, it enters the superior orbital fissure and finally enters the orbit. The abducens nerve innervates only one muscle, the rectus lateralis.
Nerve pathology
Pathology of the abducens nerve
The fibers of the abducens nerve are located superficially, so during injuries they can easily be pressed to the base of the skull. Damage to the nerve is expressed in paresis - limited outward movement of the eye organ or complete paralysis.
With normal functionality of the abducens nerve, the edge of the cornea should touch the outer edge, the junction of the eyelids. If this is not observed, then there is nerve pathology. It has the following signs:
- movement of the eye organ is limited;
- objects inspected are split into two;
- repeated deviation of the eye;
- forced position of the head, which can be involuntary;
- dizziness, disorientation in space, staggering gait.
Nerve damage can be caused by infections:
- disease with encephalitis;
- previous syphilis;
- diphtheria disease;
- influenza and its complications.
As a result of intoxication:
- ethyl alcohol;
- toxic metals;
- combustion products;
- a consequence of botulism.
Paralysis of the abducens nerve occurs for the following reasons:
- previous meningitis;
- presence of tumor inclusions;
- the presence of hemorrhage, with pressure surges;
- thrombosis;
- purulent diseases of the nasal passages;
- eye socket injuries;
- temple bruises;
- metabolic disease;
- multiple sclerosis;
- stroke.
Nerve damage is distinguished by location:
- Cortical and conductive – diseases are localized in the medulla and brainstem.
- Nuclear defeat.
- Radicular lesions are observed within the medulla. This lesion is called Fauville's palsy, when, on the one hand, there is damage to the abducens and facial nerves, and on the other hand, there is damage to the limbs.
Peripheral paralysis is divided into:
- intradural is located inside the dura mater;
- intracranial is localized in the cranial cavity;
- orbital is located in a circle.
Causes
Why does the abducens nerve become damaged? What diseases can become provocateurs?
Some types of infections and intoxications have a very negative effect on the central system. As a result, the abducens optic nerve also suffers.
What infections pose a huge danger? These are diphtheria, encephalitis, neurosyphilis, influenza and others.
Alcohol, botulism, carbon monoxide and lead poisoning can also cause eye disease. Hypertension, tumors, diabetes mellitus, brain injuries and many others are factors in the onset of the disease.
Paresis is divided into two types: organic and functional. The second group usually causes difficulties in determining the cause of the disease.
Paresis of the abducens ophthalmic nerve associated with ischemic damage to small vessels is more common in adults. Diseases such as hypertension and diabetes have an impact here. The disease disappears on its own after three months.
Treatment of paresis and abducens nerve palsy
The abducens nerve as a component of the nervous system
Recovery after paralysis occurs over a long period of time throughout the year. A well-known method of treatment is the use of physiotherapy - exposure to low-frequency electromagnetic field pulses and electric current stimulation.
The treatment method has an analgesic, anti-inflammatory, calming effect. The disadvantage is that recovery is very slow, and in some cases does not occur at all.
The oculo-occipital method of administering the drug (neuromidin) is also used to increase muscle contractility and influence defects in the connective muscles.
The method of using electrophoresis with a solution of 15% neuromidine has proven itself well. The duration of the sessions is 15 minutes daily for 15 days. After completing the procedure, it is recommended to lie down with your eyes closed for 10 minutes.
If improvement and restoration of the functioning of the abducens nerve is not observed after treatment, and the lesion does not go away on its own, surgical intervention is used. The essence of the method is as follows: an injection of ultracaine is made under the conjunctiva, and a half-circumference incision is made.
The superior external and inferior straight nerves are split into two bundles lengthwise and the lower fibers are sutured to the upper fibers. This allows you to rotate the eyeball by more than 15–20° within a day after surgery, in some patients up to 25°; binocular vision was restored in every fourth person operated on.
To alleviate the condition of impaired binocular vision, Fresnel prisms are used, which are attached to glasses. Prisms have different angles and are selected individually. Possibly also closing one eye.
Most nerve diseases are associated with a disorder of the central nervous system, so treatment is prescribed accordingly. After suffering infections and successful treatment, the nerve damage is restored. In rare cases, when the tumor is inoperable, there is serious injury to the skull and the nerve itself, recovery may not occur.
Learn more about the abducens nerve in the video lecture:
A person is able to move the eyeball thanks to 3 cranial nerve pathways. The main role in this process is played by the oculomotor nerve, which goes under number 3. It is responsible for the movements of the eyelid and eye, as well as its reaction to exposure to light. The abducens nerve controls the abduction of the eyeball, and the trochlear nerve turns it outward and downward. These nerve pathways are numbered 6 and 4. Any disturbances in the innervation of the extraocular muscles affect the ability to see fully. Among such disorders, paresis of the eye muscles in children can be identified, since, in addition to the main causes that are characteristic of adults, they often exhibit congenital anomalies. Treatment is usually carried out using a whole range of procedures; in especially severe cases, surgery is used.
Abducens nerve palsy manifests itself as isolated paralysis. In this case, a person cannot fully avert his eyes and a double image of one object appears (diplopia). This phenomenon occurs due to a violation of the innervation of the lateral muscle, for which the abducens nerve is responsible. Similar symptoms are characteristic of diseases of the orbit, so you should undergo detailed diagnostics to make a diagnosis.
The abducens nerve is damaged due to the following factors:
- Aneurysm;
- Damage to the carotid artery;
- Traumatic brain injuries;
- Infectious diseases;
- Oncological diseases;
- Microinfarctions and strokes;
- Pathologies of the nervous system;
- Multiple sclerosis.
The abducens nerve in children is also injured due to the above factors. However, other reasons are also common for children:
- Gradenigo syndrome;
- Duane's syndrome.
Damage to the trochlear nerve causes partial paralysis of the eye and the person has a double image in an oblique or vertical plane. This symptom intensifies when the eye is lowered down, so people suffering from this pathology often walk with their heads tilted to the healthy side to reduce the manifestation of diplopia. During diagnosis, myasthenia gravis (autoimmune pathology of nerve and muscle tissue) and diseases of the orbit should be excluded.
Damage to the trochlear nerve occurs in virtually the same way as to the abducens nerve, but in this case the main cause is trauma and micro-strokes. Oncological pathologies rarely affect this nerve pathway.
Oculomotor nerve palsy usually occurs in conjunction with disruptions of the facial, abducens, and trochlear nerve pathways. A separate form of pathology appears extremely rarely. This nerve is damaged primarily due to an aneurysm. It arises on the posterior communicating artery and gradually compresses the nervous tissue.
The nerve can be damaged by a growing tumor, as well as manifestations of stroke and multiple sclerosis. In most cases, such factors affect the nucleus of the nerve tract and the posterior longitudinal fasciculus. Sometimes neuropathy of the oculomotor nerve, caused by the above reasons, manifests itself in the form of bilateral drooping eyelids (ptosis). In more rare cases, paresis of the superior rectus muscle of the eye is observed. It is localized on the reverse side of the main site of damage.
According to statistics, the oculomotor nerve is often damaged due to a microinfarction. It can occur due to vascular pathologies, such as diabetes and hypertension. Such diseases usually do not immediately lead to disruptions in cerebral circulation and they should be predominantly in an advanced state. Neuritis of this nerve does not affect the reaction of the pupil to light, but in rare cases it is slightly weakened. A microinfarction occurs near the cavernous sinus or in the area of the interpeduncular fossa. It takes about 3 months for the oculomotor nerve to recover after suffering a disorder.
You should consult a doctor if you notice several symptoms characteristic of paresis of the eye muscles, especially when it comes to children. Among the common manifestations of optic neuropathy, the most basic can be identified:
- Diplopia;
- drooping eyelid;
- Strabismus;
- Decreased pupil reaction to light;
- Inability to turn the eyeball inward;
- Loss of the ability to quickly look at objects located at different distances from each other;
- Protrusion of the eye.
Treatment
The attending physician will tell you how best to treat the disorder, but there are quite common ways to restore the innervation of the eye. Such problems are treated with the help of electrophoresis, the duration of each procedure usually lasts up to 20 minutes, and about 15 sessions are required, they are carried out every day without skipping.
Various physiotherapeutic methods are used that allow impulses to be applied to the affected area. But the negative side of this effect is that some procedures have virtually no positive effect. Treatment with folk remedies is more likely aimed at preventing this disease than at eliminating the problem that has arisen.
If you notice the first symptoms, be sure to consult a doctor, get examined and, if necessary, begin treatment.
Diagnostics
It is easiest to recognize the lesion, since this pathological process is characterized by drooping eyelids, dilated pupils and abnormal deviations of the eyes. Based on such signs, making a diagnosis will not be a problem, but often they are combined with each other in various combinations, so the doctor suspects the secondary nature of the disease. To differentiate paresis of the eye muscles from other possible ailments, the ophthalmologist will need to prescribe an examination, which consists of the following procedures:
- Fundus examination;
- Determination of visual acuity and degree of mobility of the eyeball;
- Light reflex test;
- Angiography (to identify vascular pathologies);
- Magnetic resonance imaging (checks brain tissue for abnormalities).
Sometimes a consultation with a neurologist may be required. If it was not possible to determine the cause of the pathology, then the patient should be registered with a doctor and periodically examined. To prevent the condition from getting worse, your doctor may recommend special sets of exercises and other treatment methods.
Study
If the abducens is affected, other nerves responsible for ocular movement are studied. This requires professional diagnosis. As a rule, it is dealt with by an ophthalmologist, but a consultation with a neurologist is possible.
The study begins with an examination of the face for the presence of asymmetry, swelling and redness. This is necessary to eliminate inflammatory processes. The ophthalmologist examines the patient’s eyes: is there any drooping of the eyelid, retraction, or ability to focus. When looking into the distance, a healthy pupil expands; when looking close, it narrows.
The ophthalmologist checks the eyeball by moving his finger and hammer in different directions. The head is not involved. This method allows you to detect limited movement, that is, paralysis or paresis of one of the external muscles.
Medical examinations are carried out using special equipment and tests. Studying the condition of the fundus, the shape of the pupil, the width of the palpebral fissures, vision, reaction to light - all these procedures are included in the list of mandatory ones.
Additionally, the doctor performs magnetic resonance imaging of the brain.
Treatment is mainly aimed at eliminating the cause. But, unfortunately, difficulties arise precisely with its definition.
To eliminate double vision, the doctor prescribes botulinum toxin injections. A prerequisite on the path to recovery: there should be no self-medication or use of folk remedies. This is especially true for pregnant women, since even the most seemingly harmless medicine can harm the baby.