Craniography
Using this method, both general and local changes in the bones of the skull are detected in case of brain tumors.
General changes in the bones of the skull develop as a result of a long-term increase in intracranial pressure, which is observed with brain tumors. The nature and extent of development of these changes mainly depend on the location of the tumor and its relationship to the cerebrospinal fluid pathways and the great cerebral vein of Galen.
When a rapidly growing tumor is located along the cerebrospinal fluid ducts (III ventricle, Sylvian aqueduct, IV ventricle), secondary occlusive hydrocele gradually develops and, as a consequence, changes appear in the vault and base of the skull. On a number of radiographs taken in the same patient over several weeks or months, a gradually developing thinning of the bones of the cranial vault (general osteoporosis), flattening of its base, smoothing of the basal angle, as well as shortening and thinning of the back of the sella turcica, up to complete its destruction. The bottom of the sella turcica deepens, sometimes its destruction is observed. The sinus of the main bone is compressed. Along with these changes, osteoporosis is detected, and sometimes destruction of the anterior and posterior wedge-shaped processes.
With a slowly developing increase in intracranial pressure, a mostly symmetrical expansion of the normally preformed openings of the skull base is determined, namely the optic nerves, round, oval and ragged foramina, and internal auditory canals. Thinning of the edge of the foramen magnum is also often observed. In an advanced stage of the disease, especially with subtentorial tumors, osteoporosis of the apices of both pyramids is noted. The development of osteoporosis at the apex of only one pyramid on the side of the tumor is observed when it is located at the base of the temporal lobe of the brain.
With pronounced phenomena of increased intracranial pressure in young people and especially in children, divergence of cranial sutures is also detected; they are stretched and gaping. As a result of the increased pressure of the cerebral convolutions on the cranial vault, the pattern of digital impressions and ridges intensifies. These changes are mostly found in subtentorial tumors. With large supratentorial tumors located in the midline, pronounced general signs of increased intracranial pressure from the bones of the vault with symptoms of significant divergence of cranial sutures are often also observed.
As a result of tumor-induced disturbances in cerebral circulation in the skull, diffuse dilation of the diploe vein canals is often observed. It is sometimes evenly expressed in both halves of the skull. Wide channels of diploic veins on radiographs are revealed in the form of poorly tortuous, short grooves directed towards one center. The pits of pachyonic granulations and venous outlets also change their appearance when blood circulation is difficult. They expand and deepen significantly.
General changes in the bones of the skull revealed in the images when a brain tumor is suspected confirm its presence, but do not give indications of its location.
For topical diagnosis, it is important to identify local changes on radiographs caused by the tumor coming into direct contact with the bones of the skull or the deposition of calcareous inclusions in it.
Local changes in the bones of the vault and base of the skull in brain tumors are revealed on radiographs in the form of local hyperostoses, usurs, foci of pathological calcification inside the tumor or along its periphery and increased development of vascular grooves involved in the blood supply to the tumor.
Local changes in the bones of the skull (hyperostosis, foci of destruction) are most often observed in arachnoidendotheliomas. Detection of these changes in the bones of the skull is important not only for determining the exact location of the tumor; in some patients these changes make it possible to judge its probable histological structure.
B. G. Egorov, out of 508 patients with arachnoidendotheliomas, identified various local changes in the bones of the vault and base of the skull in 50.2% of them. K. G. Terian, with arachnoidendotheliomas, discovered the presence of hyperostoses directly at the point of contact of these tumors with the bones of the skull in 44% of patients. I. Ya. Razdolsky observed local changes in the bones of the skull in 46% of patients with arachnoidendotheliomas. Our data show that with a thorough X-ray examination of the skull, local changes in its bones are detected in 70-75% of patients with arachnoidendotheliomas, especially when they are localized at the base of the skull.
Hyperostoses of the skull bones (endostoses, exostoses) are revealed on radiographs in the form of various shapes and sizes of limited compactions. They are often detected in the small wings of the main bone, in the area of which arachnoidendotheliomas are often localized. Sometimes hyperostoses are also found in the area of the tubercle of the sella turcica and the olfactory fossa. Severe hyperostoses in the form of needle periostitis are detected mainly in arachnoidendotheliomas of the calvarium and can spread to fairly large areas of the bone.
In the presence of hyperostoses and usurs, the differential diagnosis should take into account not only arachnoidendotheliomas, but also diseases of the skull bones themselves, such as benign and malignant tumors, localized fibrous dysplasia, syphilis and tuberculosis.
Local bone changes are not detected on craniograms when arachnoidendotheliomas are located away from the vault and base of the skull. Local destructive changes in the bones of the skull are most often found in tumors of the cerebral appendage. We observed them in 97.3% of 355 patients with pituitary tumors. With intrascidal tumors, these changes are expressed in a cup-shaped expansion of the sella turcica, destruction of its bottom, straightening of the back, its destruction, elevation and undermining of the anterior wedge-shaped processes. The presence of double contour of the bottom of the sella turcica usually indicates uneven tumor growth.
A greater narrowing of one of the halves of the main sinus revealed on targeted images and tomograms of the sella turcica indicates a preferential direction of tumor growth in this direction.
A detailed study of some features of pathological changes in the bony skeleton of the sella turcica makes it possible to presumably speak in favor of one or another histological structure of the intrasellar tumor.
With eosinophilic adenomas, most often accompanied by acromegalic syndrome, the sella turcica is usually cup-shaped, widened, deepened and increased in anteroposterior size. Its back is sharply straightened, deviated posteriorly and sharply sparse. Along with this, there is also a significant increase in the size of the air sinuses of the skull and their increased pneumatization. We observed such changes in the sella turcica and paranasal cavities in 82% of patients with eosinophilic pituitary adenomas. With chromophobe and basophilic adenomas, only destructive changes in the sella turcica, expressed to varying degrees, are determined.
Differential diagnosis between these two groups of tumors cannot be carried out without analyzing the clinical picture of the disease and studying the fundus, field and visual acuity of the patient being studied.
By the nature of the destruction of the sella turcica, one can also presumably judge the suprascidal, parascidal, posterior sciatic and anterior sciatic localization of the tumor.
With a supraschillar tumor, the back of the sella turcica is tilted anteriorly, destroyed and shortened. The anterior wedge-shaped processes are deflected downwards and destroyed. The bottom of the sella turcica is compressed, the lumen of the sinus of the main bone is reduced.
With a peri-saddle tumor (tumor of the temporal lobe, tumor of the membranes), predominantly unilateral destruction of the sella turcica is observed on the side where this tumor is located. In these cases, craniograms often reveal destruction of part of the dorsum of the sella turcica, which is sometimes combined with unilateral destruction of the anterior sphenoid process.
With a posterior sciatic tumor, the dorsum of the sella turcica is pressed anteriorly. The posterior wedge-shaped processes are shortened and destroyed. Sometimes destruction of the Blumenbach clivus is observed. With further growth of the tumor as a result of compression of the Sylvian aqueduct and the development of hydrocephalus, secondary changes in the sella turcica appear, characteristic of a chronic increase in intracranial pressure.
Anterior sphenoid tumors cause destruction of the anterior sphenoid processes and destruction of the sella turcica of one type or another. These tumors are detected on radiographs due to the presence of hyperostoses in the area of the olfactory fossa or the area of the small wings of the sphenoid bone.
In some cases, tumors develop in the sinus of the main bone and grow into the sella turcica from below. With this localization of tumors, the cavity of the sella turcica sharply narrows, its bottom either bends upward or collapses. The lumen of the sinus of the main bone is not differentiated. The most common tumors that develop in this area are craniopharyngiomas—tumors arising from Rathke's pouch—and malignant tumors of the skull base. Characteristic of craniopharyngiomas is the deposition of lime in the tumor shell or inside its cystic contents.
Lime deposits are one of the most important local radiological signs of brain tumors. The presence of this sign makes it possible not only to establish the location of the tumor, but sometimes to correctly determine its histological nature. It is known that such normally preformed formations as the pineal gland, choroid plexuses of the lateral ventricles, the large falciform process, the dura mater, and pachyonic granulations also become calcified under physiological conditions in some people. Especially often, in at least 50-80% of healthy people, calcification of the pineal gland is observed. Its displacement by a brain tumor is of great diagnostic importance. Under the influence of tumor growth, the calcified pineal gland, as a rule, shifts from the midline in the direction opposite to the tumor.
Various physiological calcifications must be differentiated from lime deposits in brain tumors. Intratumoral lime deposits can be homogeneous. Sometimes they appear in the form of linear shadows, individual amorphous lumps or small dotted inclusions. In some tumors, for example in arachnoidendotheliomas, lime is deposited only in their membrane, which gives a certain idea of the size of these tumors. Sometimes, during long-term observation of the patient, it is possible to see increasing calcification of the tumor on radiographs.
Most often, lime is deposited in arachnoidendotheliomas. It is determined in them in the form of linear calcifications bordering their periphery, and sometimes in the form of point inclusions located inside the tumor. Much less often, calcareous inclusions are detected in intracerebral tumors of neuroectodermal origin. Most often we found them in oligodendrogliomas. Lime in these tumors occurs in the form of linear formations, in places merging with each other. The same form of calcification is occasionally observed in astrocytomas. Therefore, it is usually not possible to distinguish them from oligodendrogliomas by the nature of calcification.
Characteristic lime deposits are observed in craniopharyngiomas. Along the periphery of these tumors, lime is deposited in the form of linear or lamellar formations, and in the thickness of the tumor - in the form of amorphous lumps of varying sizes. The presence of this kind of calcification, taking into account their localization, allowed us to establish the correct diagnosis in 28 out of 32 patients with craniopharyngiomas. When making differential diagnoses, it should be taken into account that calcifications of a similar nature can also be observed with cholesteatomas.
It should be borne in mind that lime deposition is determined not only in tumors, but also in pathological processes of a non-tumor nature, for example, brain cysticerci, brain scars and long-term inflammatory foci. Differential diagnosis in these cases between tumor and non-tumor diseases of the brain based on craniography data is difficult.
Lime deposits, as a rule, are also observed in Sturge-Weber disease. The characteristic pattern of thin double strips of lime located on the surface of the brain, in its cortex, makes it easy to distinguish these calcifications from those observed in various brain tumors.
Strengthening the vascular pattern of the skull bones in some cases is a pathognomonic sign of brain tumors. With arachnoidendotheliomas, cranograms often reveal a peculiar pattern of grooves in the branches of the meningeal arteries, characteristic of these tumors, involved in their nutrition. In these cases, in a limited area of the cranial vault, unevenly expanded, short, intertwined vascular grooves are revealed. On technically well-performed radiographs in these cases, it is sometimes possible to trace the groove of the arterial trunk entering this tangle that feeds the tumor.
With intracerebral tumors, predominantly on the side of the tumor, diffuse dilation of the diploic veins of the skull bones is sometimes observed, resulting from venous stagnation.
For tumors of the posterior cranial fossa (subtentorial), important radiological signs that contribute to their recognition are expansion of the internal auditory canal, osteoporosis, destruction of the apex of the pyramid, as well as the identification of intratumoral calcifications. Uniform expansion of the internal auditory canal is most often observed with acoustic neuroma. When assessing this symptom, it should be taken into account that the expansion of the ear canal is also observed in non-tumor processes, for example, with internal dropsy and limited arachnoiditis.
The most characteristic craniographic sign of a tumor in the cerebellopontine angle region is destruction of the apex of the pyramid. Its destruction is observed in both benign and malignant tumors of this area. In malignant tumors, destruction of the apex of the pyramid occurs more quickly and is more pronounced than in benign tumors.
A valuable craniographic sign of cerebellar tumors is the thinning of the edge of the foramen magnum on the side of the tumor.
Topical diagnosis of subtentorial tumors is facilitated by calcifications sometimes detected in them on radiographs. Foci of lime are most often detected in cholesteatomas and cerebellar gliomas.
In those patients in whom clinical examination data and craniography data are insufficient for the diagnosis of a brain tumor and its localization, they resort to contrast X-ray examination of the cerebrospinal fluid spaces of the brain and its vessels.
How is vascular examination performed?
Angiography and ultrasound are used to examine the veins and arteries of the brain. Both options are safe, informative and have a minimum of contraindications.
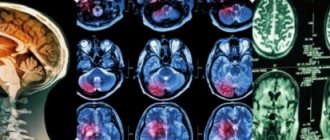
Gives the best results when examining small vessels and nerve trunks. During the study, the doctor will take an image of all the vessels in your brain. This will help diagnose micro-strokes and thromboses that are not visible on a regular MRI scan of the head. It is often prescribed by surgeons after operations to control the condition.
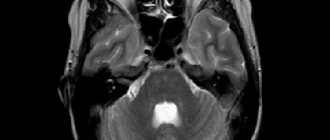
MRA is performed in the same way as conventional magnetic resonance imaging, and has the same features and contraindications. Before the procedure, you must remove all metal objects, and you must not move your head while the tomograph is operating. Often, for correct diagnosis, angiography should be combined with MRI of the brain - this will allow a more detailed examination of the area of pathology.
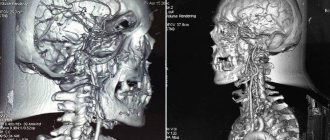
CA of cerebral vessels is similar in implementation to computed tomography. Following the procedure, the doctor will receive a three-dimensional model of the vessels of the head. In the resulting image, you can see anomalies in the structure of veins and arteries, atherosclerosis, narrowing of the lumen of blood vessels and neoplasms.
The doctor may prescribe this examination both to prepare for surgery and to monitor after treatment. In addition, this type of examination is an option for patients who, due to contraindications, cannot undergo MRA.
During computed tomography angiography, a contrast agent can be used to better visualize the damaged areas. Contraindications for the procedure are the same as for CT: pregnancy and childhood.
The ultrasound sensor is placed on the thinnest bones of the skull. Using ultrasound, you can find narrowing or thrombosis in the blood vessels of the brain, measure the speed of blood movement, detect aneurysms and areas with altered direction of blood flow. The image is shown on the monitor screen, and, if necessary, you can print the desired frame.
Using ultrasound, you can examine both the vessels inside the skull and in the neck if they have disrupted the blood flow in the brain. The method has no contraindications and is absolutely safe for patients of any age. UD does not require additional preparation or examination, however, before the procedure it is better to refrain from taking foods and medications that affect vascular tone.
Extracranial and intracranial vessels of the brain: what they are and their structure
The blood supply to the brain is carried out by a dense network of vessels - veins, arteries, capillaries. Through them, blood delivers oxygen and nutrients. It is very important that the blood supply to the brain is carried out in full, since nerve cells are the most vulnerable in the human body - they die from a lack of oxygen and nutrition before anyone else.
The daily blood requirement for an adult varies around fifty milliliters of blood per minute per hundred grams of brain matter.
Young children have a higher need because their bodies work harder. To ensure cerebral circulation, a person has two groups of vessels - intracranial and extracranial.