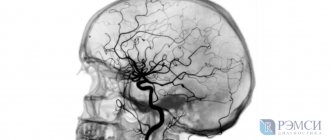
Magnetic resonance angiography (MR angiography or MRA) is currently the method of choice for diagnosing pathological changes in cerebral vessels. The method is based on the ability of the MRI machine to “see” flowing blood in the vessels against the background of motionless brain matter.
The human brain is abundantly supplied with blood from the pool of four main arteries, two on the right and on the left: the internal carotid and a pair of vertebral arteries. Each of which gives off many branches in the cranial cavity. The anterior, middle and posterior cerebral arteries, connecting with the vertebral arteries, form the Circle of Wellis. Venous blood flows through the system of so-called venous sinuses; these are wide veins tightly fused with the membranes of the brain and the bones of the skull.
Methodology
Magnetic resonance imaging involves placing a person in a constant magnetic field. An RF signal is then sent. It changes the magnetic field.
This phenomenon causes hydrogen protons to move within cells. This is what is recorded by special receivers. Subsequently, the information is processed, and then the image is generated by the program.
After exposure to the radio frequency signal, the protons begin to return to their position (63% to the original T1 position, 37% to T2 relaxation).
Based on this, slices 3–4 mm thick are formed in two modes: T1 and T2 images.
MR angiography is no different from a conventional study. The only difference is the special vascular program. It is aimed at clear visualization of the network of arteries and veins in the area of interest.
Contrasting is usually not required. The course of the vessels is clearly traced to the capillary network.
Contrast-enhanced MRI differs from conventional examination by the intravenous administration of paramagnetic gadolinium salts. The substance can be administered before the procedure or as a drip during the MRI.
This is a generalized idea of the methodology. More detailed information is in the video:
Angiography
Up
Angiography, or MRI with contrast, involves injecting the patient intravenously with a substance that will be visible on X-rays. Thanks to this study, you can see arteries, veins and vessels of any size - from the aorta to the smallest capillaries.
During this procedure, the patient is admitted to the hospital under constant observation before and after angiography. This procedure is not entirely safe, for which not only a general blood test is performed, but also its group and Rh factor are determined.
Contraindications
As with other types of examinations, MRI is not recommended in selected cases. The list can be divided into absolute and relative.
The first group of contraindications includes:
- The presence of metal permanent implants in the patient’s body or pacemakers (with the exception of titanium structures).
- The weight of the subject exceeds the permissible limit (depending on the tomograph 130-150 kg).
- The patient's serious condition requires constant hardware support.
- Allergic reactions to the administration of gadolinium salts during a previous scan (for contrast tomography).
The following are considered relative contraindications:
- Pregnancy and breastfeeding. In the first trimester, MRI is performed in exceptional cases. The rest of the time according to indications.
- Claustrophobia. Diagnostics are carried out in open tomographs or under anesthesia.
How to prepare for an MRI of the brain?
No special, lengthy preparatory manipulations are required before the session, but a number of recommendations should be followed to ensure that the MRI of the brain is comfortable and without complications. First, be sure to warn your doctor about the presence of permanent metal implants. If it is possible to remove such parts for a while, this should be done in advance, for example, visit the dentist and remove the braces. Before going to the clinic, leave all body jewelry at home.
Secondly, take care of comfortable, loose clothing for the duration of the procedure. The diagnosis is carried out in a lying position, so items of clothing should not hinder movement (a miniskirt and skinny jeans will definitely not fit). Clothes should not have metal fasteners, buttons, belts, etc. Check your pockets for lost keys, small change, magnetic cards, etc.
Before going for an examination, you need to prepare the necessary medical documentation, including a referral from the treating specialist, a card or an extract from it, the results of other studies and previous photographs, if available.
It is better for women to avoid wearing makeup on this day, as many cosmetic and decorative products contain metallic inclusions. Before screening, each patient will have to complete a written questionnaire regarding health issues. This is required to identify cases of allergies to medications, chronic diseases that prevent the use of contrast, and other disorders that are subject to a ban on tomography.
Indications
MRI, tomography with contrast, MRI of the brain with blood vessels have different purposes and costs. The attending physician must determine what type of scan is needed. He will recommend an examination.
It is not advisable to self-select and then undergo an MRI. This is due to various indications and diagnostic capabilities.
When non-contrast magnetic resonance imaging is performed:
- traumatic brain injury and the long-term period after it;
- hydrocephalus of various origins;
- abnormalities in the development of cerebral structures;
- inflammatory processes;
- neurological symptoms (syncope, epilepsy, headache of unknown origin, visual and behavioral disturbances, memory disorders).
Indications for MRI with contrast:
- identification of multiple sclerosis with determination of the degree of its activity;
- differential diagnosis of benign and malignant formations;
- suspicion of pituitary adenoma;
- postoperative observation;
- questionable results of an MRI without contrast.
Indications for MR angiography:
- detection and control of vascular aneurysms and malformations;
- ischemic cerebral lesions;
- stenosis of the carotid or coronary arteries;
- congenital heart defects;
- assessment of cerebrospinal fluid flow in the clinic of increased intracranial pressure, hydrocephalus.
This list of indications and its division is very arbitrary. Methods can complement each other, carried out jointly or sequentially.
In addition, all types of MRI are sometimes combined with examination of other areas and zones. Most often, cerebral vascular tomography is performed with a scan of the cervical spine.
Performing magnetic resonance imaging
The scanning process with a magnetic resonance imaging scanner is completely painless, but it may take some time, which may not be very convenient, since moving during the examination is prohibited. You should also remove your electronics before undergoing the scan.
The sequence of actions for this study is approximately as follows:
- The patient is placed on a special couch, the limbs are fixed with belts. If the patient has difficulty controlling his own body, he is first prescribed the necessary sedatives.
- The head is also fixed using a special roller.
- Next, the couch goes inside the apparatus tunnel, and the scanning process begins. If necessary, you can contact a health worker using a special microphone.
- In the case of vascular examination, a contrast agent (often gadolinium-based) is administered, and the procedure itself takes slightly longer.
During the scan, the patient does not feel pain or any discomfort, and immediately after the procedure is completed, he can go about his business.
Diagnostic criteria
The tomographic method allows us to identify a large number of organic pathologies of the brain. Each violation has its own signs and criteria. Below we present a few of them.
Congenital malformations
Arnold-Chiari I malformation
A common pathology. It belongs to the group of anomalies (1–4).
It is based on the displacement of the cerebellar tonsil below the level of the foramen magnum.
A change of 3 mm has no clinical manifestations. The disorder may be an incidental finding in adults.
When the deformation is more than 5 mm, brain symptoms appear. T2 tomograms in the midsagittal projection show prolapse of the tonsil below the level of the foramen magnum.
The first photo shows the Arnold-Chiari malformation, the second shows the norm for comparison
There is also a decrease in the size of the occipital cistern (or its complete absence). The brain stem is displaced.
Rechlinghausen's disease
The most common type of neurofibromatosis. Its most common manifestation is optic nerve glioma. On tomograms, the pathology appears hypo-intense on T1 images and hyperintense on T2.
The usual localization of glioma is in the area of the bottom of the 3rd ventricle. A combination with damage to the circulatory system (stenosis, aneurysm) and bone structures of the skull is possible.
Choroid plexus cysts
A common pathology that is easily diagnosed by ultrasound in children under one year old, so MRI is not required. After 12 months of life, these formations, with rare exceptions, disappear. MRI is indicated only in the presence of neurological symptoms.
Hydrocephalus
The expansion of the liquor-containing cerebral system can be communicating and occlusive. Signs of GM dropsy are general. Their difference is only in the mechanism of development.
With occlusion, an obstruction to the outflow of cerebrospinal fluid is formed. When open, the production of cerebrospinal fluid is disrupted.
Signs of hydrocephalus are:
- dilatation of the ventricles of the GM;
- deformation of the corpus callosum;
- narrowing of the subarachnoid fissure.
Non-contrast MRI is usually sufficient to make a diagnosis.
accumulation of fluid and compression and deformation of neurostructures by it
Vascular diseases
Venous malformations
Often located in the pia mater. Accompanied by convulsive syndrome.
When performing MRI diagnostics, doctors prefer to conduct the study in angiography mode. It shows a collection of vessels passing through the parenchyma and flowing into the collector vein. This picture is called the “jellyfish” symptom.
Arteriovenous malformations
They are considered common. They are of greater clinical importance, since pathology often causes ischemia or hemorrhage. The anomaly is a conglomerate of vessels of various diameters.
Arteries and veins take part in the formation of malformation. The size of the plexus and the number of feeding vessels are variable. With standard MRI, the malformation appears as a hypointense area on T1, T2 images.
MR angiography allows you to identify the feeding arterial vessel and determine whether it is involved in the trophism of normal brain tissue.
photo:
Shunting vascular tangle on a feeding pedicle
This is important for management tactics, as well as the possibility of clipping the feeding artery.
The larger the size of the malformation and the number of vessels, the more pronounced the disturbance of cerebral hemodynamics. This means there is a risk of developing hemorrhages.
Brain tumors
The group is represented by a large number of benign and malignant formations, as well as metastatic processes. General criteria for cerebral tumor:
- The presence of a focus of pathology of varying intensity.
- Displacement of the midline structures of the brain.
- Development of occlusive hydrocephalus.
- Peripheral or focal cerebral edema.
large lesion in the frontal lobe with decay in the center, displacement of neighboring structures, including the median
Contrast magnetic resonance imaging reveals and differentiates benign and malignant processes. The latter are richly vascularized. They accumulate contrast well.
With multi-slice assessment, it is possible to identify the feeding vessel, which confirms a malignant neoplasm. More details about GM tumors in the video:
Action plan after brain MRI
The specialists of the diagnostic center are called upon only to obtain and describe the results of the examination; they do not make a final diagnosis. Ultimately, the patient receives documentation consisting of the images taken and the preliminary conclusion of a radiologist, radiologist or functional diagnostician. At the request of the client, the photo and description can be issued both in printed form and in electronic form on removable media or by e-mail. If you have the email address of the treating doctor, the clinic staff can send the results to him directly. In the case of printed documents, they are provided to the doctor during a personal meeting at a scheduled appointment. After examining the images, the doctor will make a final diagnosis and prescribe appropriate treatment. It is possible that the doctor will redirect you to another highly specialized specialist who is more competent in the identified ailment.
If an MRI of the brain was performed on the patient’s own initiative, and he does not know where to go next, he should consult with the radiologist who performed the screening. Often, diagnostic centers employ consulting doctors who are ready to accept and describe the current health situation. You can always find out about this service at the institution’s reception desk.
Survey histories
The frequency of brain MRIs is increasing every year. This makes scanning popular and often discussed by Internet users.
On numerous forums, patients are increasingly leaving their messages regarding the safety of the method. Recent data on the accumulation of gadolinium salts in brain structures in the long-term period after the procedure have caused much debate.
Many people are trying to find help in making a diagnosis and choosing therapy. In this mass it is difficult to find truly interesting clinical cases.
"Wrong tomography"
21.01.2018
Girl K. suddenly began to experience headaches for no apparent reason. Weakness and sudden weight gain forced her to visit the forum in search of the right advice. At that time, going to the doctor seemed completely unnecessary to her.
Having received advice on the Internet to go for an MRI, K. immediately decided to undergo the study, despite the high cost. The tomography results did not clarify anything. My health did not improve and this nevertheless led to an appointment with a doctor.
A trip to a neurologist brought K. to a standstill. He recommended contacting an endocrinologist. K. fulfilled the appointment: the next day she visited a specialist. The doctor advised me to donate blood for hormones and undergo an MRI.
K. remained silent about the fact that she had already had it done, but she donated blood for hormones. At the next appointment, the endocrinologist, based on test results, diagnosed a pituitary adenoma.
K. showed a conclusion where there was no tumor. Then the endocrinologist clarified that for diagnosis it is better to perform a scan with contrast.
After a second examination, but this time with a dye, the diagnosis was confirmed.
It turned out to be a microadenoma. It was not visible on a regular MRI, but produced large amounts of the hormone, which caused her to feel unwell.
Insidious tumor
05.06.2018
The story of 7-year-old girl A., as told by her sister, is very sad. At the end of September, the baby complained that her back and neck hurt.
After being examined by a pediatrician, the child and mother were sent to the regional hospital. Here, an MRI scan revealed a spinal cord tumor.
They began to prepare the child for a planned operation to remove the tumor, but the girl’s condition deteriorated sharply. This prompted emergency intervention.
The tumor was removed. It turned out that an intramedullary astrocytoma had developed. After long-term therapy and rehabilitation, the girl began to speak, write and tried to walk again. Everyone was confident in A’s speedy recovery.
But at one point the girl’s condition worsened. She was hospitalized again.
A thorough examination was carried out, including an MRI of the brain. It was she who showed 12–14 tumor formations measuring 2–4 mm in various parts of the brain. A few months later, despite the therapy, the girl died.
Now it is difficult to say whether these tumors were spinal cord tumors at the time of removal or not. The question of whether an immediate brain MRI would have saved the girl’s life also remains unanswered.
The Joy of Recovery
03.04.2015
E. suffered from epileptic seizures for a long time. This is what brought her to the scan.
MRI and then tomography of the brain vessels helped make the correct diagnosis – arteriovenous malformation. After consulting a neurosurgeon, we chose radical treatment with a gamma knife.
The postoperative period was difficult: the attacks became more frequent, but after 11 months they passed. The last angiography 3 years after removal showed that E. is doing well and there is no more malformation.
The diagnosis is in doubt
01.05.2017
Yu's story is interesting from the standpoint of the reliability of the research. Suddenly, the girl began to experience headaches; they were paroxysmal and extremely intense. This problem led her to a neurologist.
The specialist recommended that she undergo magnetic resonance imaging. The conclusion was written: “MRI signs of vascular venous malformation in the frontal lobe.”
The neurologist thought the examination was not enough, and she prescribed an MRI with contrast. The conclusion sounded like “venous angioma in the left frontal lobe.”
After this, the doctor said that surgery was necessary. The tumor is very dangerous and can cause a stroke.
Yu was filled with fear, but she still agreed to the operation. After a planned hospitalization, neurosurgeons already prescribed MR angiography. The angiography result was surprising: no signs of AVM or arterial aneurysm were detected in the cerebral vessels.
Yu was discharged from the hospital without any interventions. An exact diagnosis was never made. Yu still doesn’t know what causes her headaches and what she should do next.
An unexpected find
09.09.2016
A. tells the story of her young man. The girl began to notice that her beloved often shuddered and gritted his teeth in his sleep. When she tried to talk about it, Sergei laughed it off: “it’s all because of the worms.”
A. did not calm down and insistently demanded to see a doctor. After the examination, the neurologist recommended undergoing magnetic resonance imaging. The result of the study was unexpected: hypoplasia of the cerebellar vermis, moderate external hydrocephalus of the brain.
Now they have to select the right therapy and be constantly monitored by a neurologist. This is how a harmless manifestation turned out to be a symptom of a serious illness.
History of the struggle
March 2018
Reviews from people with multiple sclerosis vary, but they are all very similar. The lives of patients change radically.
N.'s story began at the age of 14. It was during taekwondo training that N. became ill. I had problems with coordination; I couldn’t stand on one leg and repeat the trainer’s movements.
N. got home after class on her own. After talking with my parents about what happened, I came to the conclusion that these were manifestations of “adolescence.” It's about hormones.
Father and mother advised them to have a good rest and sleep. But it did not help. A few days later, numbness appeared in my left arm and a headache.
Later, the lower limbs also began to become difficult to obey. These symptoms forced me to consult a pediatrician. The doctor recommended “getting my head checked.”
At first we thought it was a joke. But she insisted and said that it was necessary to do an MRI.
Ten years ago, when this method was not so common, this turned out to be a big problem. But thanks to the persistence of the parents and the help of friends, the issue was resolved.
The MRI was done quickly. And then the then incomprehensible diagnosis of “multiple sclerosis”, hospitals, constant treatment and struggle.
Although the cost of therapy is extremely high, N. and her parents are still finding ways to receive all medications in full. I had to give up sports and start home schooling.
N. has been fighting the disease for 10 years. Exacerbations are now less frequent, and a lot of information about the pathology has appeared. Thanks to the Internet, it is possible to communicate with the same people.
Now N. plans to continue his studies at the university. He had to quit after the 2nd course due to an exacerbation. She also wants to travel the world.
The right decision
August 2015
K. has suffered from headaches for as long as she can remember. Coordination was also impaired, especially with sudden movements.
But for a long time K. did not pay attention to the headache, and there was no way to overcome the “clumsiness” at all. But at one point, a night attack of pain with nausea and vomiting forced me to go to the doctors.
After magnetic resonance imaging, a diagnosis was made - Arnold-Chiari malformation type 1. Having quickly read the information on the Internet and learned about the possible complications, K. decided to get rid of this disease as quickly as possible.
After the operation, K. feels great. Her only regret is that she did not decide to have an MRI earlier.
Reviews
Up
For several years I suffered from strange headaches, which were accompanied by vomiting and nausea. Painkillers stopped helping. I decided to do an MRI of the vessels of the head and neck, which revealed that I had problems with blood flow in my neck.
I am 59 years old. After several sharp surges in blood pressure, I was sent for an MRI. The procedure went without any problems, very quickly, and after a couple of hours I received a conclusion and several recommendations from the doctor. As it turned out, this is coronary disease. Thanks to MRI, it was detected at an early stage.
Alternative Methods
If MRI is not possible, the best alternative is CT, taking into account the characteristics and limitations of the method.
Other methods include: duplex scan; spectroscopy; echoencephalography; Doppler ultrasound; electroencephalography. All these methods, to a certain extent, make it possible to analyze specific aspects of brain functioning. The decision to use a particular method for a particular patient is made individually by the attending physician.