Increased intracranial pressure (ICP) is observed with head trauma, hydrocephalus, intracranial tumors, hepatic encephalopathy and cerebral edema. Increased ICP can lead to death or neurological complications due to decreased cerebral perfusion pressure (CPP), cerebral ischemia, or destruction of vital structures. Rapid diagnosis is critical in the management of ICP.
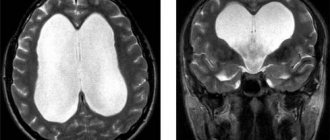
Normal (left) and gyrocephaly (right)
Intractable high ICP is the most common “terminal condition” leading to death in neurosurgical patients. The association between the severity of intracranial hypertension and poor outcome after severe head injury is well established.
The prognosis is generally good for patients with normal ICP, whereas patients with elevated ICP are much more likely to experience adverse outcomes. Traumatic brain injury (TBI) accompanied by elevated ICP has a mortality rate of about 20%.
Relationship between intracranial and blood pressure
Liquor is the cerebrospinal fluid located in the space of the skull and envelops every cell of the brain.
The relationship between intracranial and blood pressure can be described by the relationship: average cerebral tissue + effective cerebral propulsive = average arterial - (average cerebrospinal fluid + average venous).
CSF circulation
Therefore, intracranial pressure and blood pressure are normally described mathematically as follows (in mm Hg): 10 + 60 = 80 – (10 + 0). The body tries to correct any deviations from the normal cerebral propulsive pressure of 60 mmHg. Art., characterizing the necessary speed of blood flow to ensure the vital activity of nerve cells.
The situation is significantly aggravated if there are circulatory disorders, diseases and injuries that interfere with the normal regulation of the process. With insufficient autoregulation of cerebral circulation, intracranial and blood pressure correlate according to the following pattern: one jumps, the other rises.
Unpleasant sensations and headaches are caused by:
- spasms of arteries and veins;
- increased cerebral tissue and liquor pressure;
- metabolic disorders resulting from limited venous outflow.
Why does ICP decrease or increase?
The most important role of the circulatory system, in addition to transporting blood to all parts of the body, is to maintain optimal CPP. Formula for calculating CPP:
CPP = mean arterial pressure (MAP) – mean intracranial pressure (MICP) – cerebral venous pressure (CVP).
CPP is the main factor in determining cerebral blood flow (CBF). CBF is maintained constant, despite wide differences in CPP and SBP, by the mechanism of autoregulation.
Autoregulation is a homeostatic process of cerebral arterioles that maintains a constant cerebrovascular resistance within the CPP range. If the CPP rises, this causes stretching of the arteriolar walls and reduces intracranial pressure. Likewise, when pressure decreases, the arterioles constrict to maintain CPP.
If SBP is less than 65 mmHg. Art. or more than 150 mm Hg. Art., arterioles are unable to autoregulate, and blood flow becomes completely dependent on blood pressure. The CC is no longer constant, but depends on the CPP and is proportional to it.
Thus, if SBP (mean arterial pressure) falls below 65 mm Hg. Art., cerebral arterioles dilate to their maximum, and the brain is at risk of ischemia due to insufficient blood flow.
Similarly, with SBP exceeding 150 mm Hg. Art., the cerebral arterioles narrow as much as possible, and any further increase in pressure causes an excess of CBF, which can lead to an increase in ICP.
Autoregulation works well in a normal brain, but it is impaired in a damaged one. As a result, passive vascular flow occurs in and around the injured areas and possibly throughout the injured brain. Ideally, the treatment goal is to maintain a CPP greater than 60 mmHg. Art., and this can be done either by reducing ICP or increasing systolic blood pressure using vasoconstrictors. Caution should be exercised when using vasoconstrictors that do not increase ICP.
Invasive ICP monitoring in the intensive care unit
The cranial volume contains approximately 85% brain tissue and extracellular fluid, 10% blood, and 5% CSF. If brain volume increases, such as in cancer, there is a compensatory shift of CSF into spinal cord cells, followed by a decrease in intracranial blood volume through vasoconstriction and extracranial drainage. If these mechanisms work normally, ICP will remain unchanged. If these mechanisms are exhausted, further changes in intracranial volume can lead to a sharp increase in ICP.
The rate of changes in the brain affects the prognosis of ICP treatment. For example, a slow-growing tumor is often accompanied by normal or minimally elevated ICP as the brain has time to adapt to the changes. On the other hand, sudden small intracranial bleeding can threaten a sharp increase in ICP. Ultimately, acute changes in ICP exhaust compensatory mechanisms and can lead to the death of the patient.
The relationship between ICP and intracranial volume is described by a sigmoidal volume pressure curve. Volume expansion up to 30 cm usually results in little change in ICP because it can be compensated for by extrusion of CSF from the intracranial cavity into the posterior spinal sac and, to a lesser extent, by extrusion of venous blood from the skull.
If these compensatory mechanisms are exhausted, ICP increases rapidly with further increases in volume until it reaches a level comparable to the pressure within the cerebral arterioles (which depend on SBP and cerebrovascular resistance). At this stage, the increase in ICP stops, the cerebral arterioles begin to collapse and the blood flow completely stops.
Intracranial pressure monitor
The relationship between ICP and CSF and physiological effects has been described in detail by Simon and colleagues as follows:
- CSF 50 ml/100 g/min: normal values;
- CSF 25 ml/100 g/min: slowing electroencephalogram;
- CSF 15 ml/100 g/min: isoelectric electroencephalogram;
- CSF from 6 to 15 ml/100 g/min: presence of ischemic penumbra;
- CSF less than 6 ml/100 g/min: neuronal death.
The above indicators help the doctor recognize high ICP and diagnose the cause of the disease.
ICP: normal or pathological?
Absolutely healthy people are rare. In addition, physiological norms vary significantly. High intracranial pressure (ICP), which in medicine is usually described as cerebrospinal fluid pressure, can become normal in some blood diseases, endocrine disorders, and non-standard structure of the cardiovascular chain.
In all other cases, high ICP is not the norm, but a pathology. The main causes of cerebral hypertension:
- displacement of segments of the cervical spine;
- decrease in skull volume - craniostenosis;
- pathological neoplasms, including tuberculomas, granulomas, keloids;
- congenital or acquired dropsy - hydrocephalus;
- destruction and death of nerve cells due to encephalopathies, meningitis;
- accumulations of pus - abscesses;
- a dangerous form of toxicosis during pregnancy - eclampsia;
- heart and pulmonary failure;
- fat and cholesterol deposits in the bloodstream - atherosclerosis;
- damage to the vascular chain and their consequences such as ischemia, strokes;
- abuse of alcohol, drugs, psychomotor stimulants;
- weather changes;
- a significant increase in body temperature - hyperthermia;
- age-related degradation changes;
- disorders of higher nervous activity.
High intracranial pressure: normal or pathological? Nausea, headache, deterioration of vision, hearing, memory and attention - these standard symptoms of brain hypertension can hardly be called normal or pleasant.
Consequences
It has been scientifically proven that 20-30% of the adult population suffers from the problem of blood pressure surges. With age, the percentage of damage increases and reaches 50-65%. There is even a table of risks for increased ICP.
The consequences of increased ICP can be characterized as follows:
- Irreversible organic damage to target organs (heart, brain, kidneys, blood vessels, fundus).
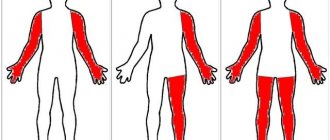
- Impaired coordination of movements.
- Weakness in arms and legs.
- Decreased visual acuity or loss of vision.
- Decreased cognitive functions of the brain, tension in the fontanelles, nosebleeds.
- The occurrence of stroke (quite rare, but it does happen).
- With a significant increase in advanced cases, the possibility of death cannot be excluded.
Normal in adults
[ads-pc-2]Doctors describe cerebral hypertension in four stages.
The normal intracranial pressure in adults is 10 mmHg. Art. at each “step” another 10 units are added.
The first stage is soft, weak. Appears at readings of 15-20 mmHg. Art. It is characterized by drowsiness and headaches with sudden movements, changes in body position, and coughing.
The second is moderate, average. Diagnosed at values of 21-30 mmHg. Art. Accompanied by tinnitus, apathy, lethargy.[ads-mob-1]
The third stage of intracranial hypertension of the brain is strong, pronounced. Fixed at readings of 31-40 mm Hg. Art. It is characterized by pulsating and shooting headaches, double vision of objects, and nausea.
The normal intracranial pressure in adults reaches 20 mmHg. Art. Anything higher results in symptoms that significantly worsen the quality of life.
The fourth is heavy, very pronounced. Installed at a value of 41 mmHg. Art. and more. It is recognized through the detection of symptoms of severe depression of consciousness, a clear decrease in muscle tone. Also characteristic are hiccups, vomiting, anisocoria - different pupil sizes.
How to determine intracranial pressure: diagnostic methods, norm and deviations
- April 1, 2019
- Neurology
- Tokmantseva Alena
Headaches caused by high or low blood pressure are familiar to everyone.
If I haven’t been there myself, then I’ve met with relatives or friends. But there is a disease in which pain and discomfort are present, but blood pressure is normal. In this case, the cause may be a change in ICP.
How to determine intracranial pressure and choose treatment methods can be found in this article.
What is intracranial pressure
Intracranial pressure is the force with which cerebrospinal fluid presses on the ventricles of the brain. It's called liquor. The pressure of excess fluid or lack of it causes pain.
Liquor protects the brain from mechanical damage. Fluid circulates from the ventricles of the brain to the spinal ventricle. There are situations when cerebrospinal fluid accumulates in some sections. For this reason, ICP increases.
Intracranial pressure and blood pressure may change together. ICP is a dangerous condition, sometimes life-threatening. Pathology can strike at any age. Infants and adults face this.
Symptoms of intracranial pressure
A distinctive feature of the disease, which makes it possible to identify intracranial pressure as the main cause of headaches, is the vivid manifestation of symptoms in the morning. In a lying position, pulsating pressure occurs in the temple area. The main symptoms of ICP are:
- headaches in one part of the head, usually temporal or occipital;
- nausea;
- dizziness;
- decreased vision;
- sweating;
- drowsiness;
- fatigue, apathy;
- surges in blood pressure.
Coughing or sneezing makes the pain worse. Decreased vision depends on the degree of pressure. In dangerous cases, complete blindness occurs. Other manifestations may include the following:
- swelling of the eyelids;
- bruises under the eyes;
- hearing loss;
- noise in ears;
- increased salivation;
- pain in the heart or stomach.
Causes of high blood pressure in adults
Symptoms of intracranial pressure are not specific. Similar signs may indicate other diseases. A study is required to make a diagnosis. ICP appears at any age. Adults, as a rule, have concomitant diseases that are causes of ICP:
- The presence of tumors in the brain.
- Circulatory disorders.
- Severe poisoning.
- Overweight.
- Excessive intake of vitamin A.
- Migraine.
- Encephalitis.
- Hydrocephalus.
- Meningitis.
- Stroke.
- Brain hypoxia.
- Thrombosis of the venous sinuses.
- Traumatic brain injuries.
- Late toxicosis of pregnant women.
These causes do not always lead to ICP, but their presence increases the risk of developing the disease.
Intracranial pressure in children
In children, ICP can occur in the womb. The reasons for this are the following:
- disturbance in brain development;
- improper outflow of cerebrospinal fluid;
- infections that the baby contracted in utero;
- excessively rapid closure of the fontanel;
- hypoxia during childbirth, causing cerebral edema;
- hydrocephalus;
- trauma during childbirth;
- difficult course of labor.
A neonatologist knows how to determine intracranial pressure in a newborn. A timely diagnosis allows the child to develop without any problems. Up to 2 years, ICP may temporarily increase due to the following factors:
- weather changes;
- prolonged crying;
- with significant physical activity.
Diagnosis of intracranial pressure in an infant is carried out in the presence of the following symptoms:
- unexpected scream;
- frequent crying at night;
- irritability;
- aggression;
- bright veins on the head;
- head growth is not proportional to age;
- drowsiness, lethargy, apathy;
- bulging fontanel;
- eyes are always lowered;
- trembling;
- delayed physical or psychological development;
- refusal to eat;
- regurgitation.
After the age of 3 years, signs of ICP are:
- frequent headaches at night and in the morning;
- nausea;
- developmental delay;
- decreased vision;
- lack of coordination;
- large forehead;
- walking on tiptoe.
With a sharp jump in intracranial pressure, vomiting, fainting, and convulsions occur. Diagnosis of intracranial pressure in children is carried out as follows:
- Measuring head circumference. Its rapid growth and inconsistency with age indicate brain disease.
- An examination of the fundus by an ophthalmologist can identify disorders of the optic nerve that occur with ICP.
- If the fontanelle is open, an ultrasound scan of the brain is performed. For older children, computer or magnetic resonance imaging is used.
- Doppler ultrasound can detect vascular disorders.
- In newborns, intracranial pressure can be determined using the Ladd monitor. It reveals pulsation in the crown.
Diagnostic methods
Faced with frequent headaches, people do not know where to go and which doctor measures intracranial pressure. The main observation of the patient is carried out by a neurologist, because this pathology affects the central nervous system. Additionally, you will have to visit an ophthalmologist for a fundus examination.
Intracranial pressure can be determined by two methods:
- invasive;
- non-invasive.
The first is a direct method, requiring sterile conditions, expensive equipment and highly qualified physicians.
Non-invasive ones have become widespread due to their safety and reliability. Allows you to identify changes in the structure of the brain. Detect tissue neuroactivity.
Invasive methods
Invasive methods for diagnosing intracranial pressure in adults are carried out as follows:
- A catheter is inserted into the ventricle of the brain and fluid is withdrawn. The information content of this method is the highest.
- The use of a subdural screw is indicated in emergency cases. The procedure is complex and risky. A screw is inserted through a special hole in the skull to determine the ICP.
- The intraventricular method allows you to measure ICP through a special hole in the skull. If necessary, the cerebrospinal fluid can be pumped out.
- The epidural method allows you to determine the level of pressure, but does not remove excess fluid.
- Intraparenchymal sensors consist of a thin wire. The method is the least traumatic. Allows you to control ICP in a hospital setting. But the method is not always reliable.
All methods carry a risk of developing infectious diseases. These methods are used when absolutely necessary.
Non-invasive methods
How to determine intracranial pressure using non-invasive methods:
- By displacement of the eardrum. As ICP increases, it shifts due to the pressure of the endolymph in the cochlea of the hearing aid.
- Cochlear microphony is based on changing the vibrations of high-frequency sound. This method does not show pressure, but records its changes. Not used for traumatic brain injuries due to the lengthy examination.
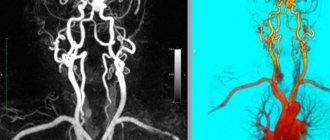
- Transcranial Dopplerography is an ultrasound method that allows you to determine the speed of blood flow through the vessels. Pulsation indirectly indicates the presence of high ICP. This method has no contraindications, but is incompatible with vascular drugs, alcohol and smoking.
- Examination of the fundus to detect swelling.
- Magnetic resonance imaging can determine the presence of intracranial pressure.
These methods have few contraindications and do not provide accurate results. Only invasive methods can determine whether ICP is normal. What is the normal level of intracranial pressure in adults? This is 10-15 mm Hg. Art. At 25 mm Hg. Art. the condition becomes dangerous, more than 35 – fatal.
Measuring intracranial pressure at home
Patients wonder how to measure intracranial pressure at home. This cannot be done outside the hospital. All methods require special equipment or intervention in the body. At home, one can only assume the presence of ICP based on the symptoms of the disease. The diagnosis is made by a neurologist after diagnosis.
Consequences of the disease in children
With a constant increase in intracranial pressure in children, the blood supply to the brain is disrupted and vasoconstriction occurs. This leads to developmental delays. With timely treatment, the disease does not affect the child’s future life. Without treatment, serious consequences are possible:
- mental disorders;
- stroke;
- speech disorder;
- physical lag behind peers;
- epilepsy;
- lack of coordination;
- hydrocephalus;
- paralysis;
- decreased vision;
- weakness;
- breathing disorder.
Intracranial pressure, which led to complications, leads the child to disability. In some cases, death occurs.
Treatment methods
A neurologist knows how to determine intracranial pressure and how to treat it. Depending on the cause of ICP and the age of the patient, an appropriate treatment regimen is selected. Diuretics, vascular and sedatives are used. Prescribe an appropriate diet and exercise.
Diuretics remove excess fluid from the body through the kidneys. Due to this, the amount of cerebrospinal fluid is reduced. Diuretics will not bring the desired result if the cause of ICP is a tumor, aneurysm or injury. In this case, surgery will be required. A doctor must prescribe medications. Self-medication is unacceptable.
If ICP is formed as a result of excessive formation of cerebrospinal fluid, then shunting is performed and the excess fluid is pumped out.
When treating with medications the following is used:
- diuretics;
- neuroprotectors;
- diacarb;
- hormonal drugs;
- drugs to reduce cerebrospinal fluid.
Limit salt intake to avoid fluid retention in the body. You should avoid fatty foods and give preference to plant foods rich in vitamins. Drink herbal teas that have a mild diuretic effect.
Prevention of ICP
To prevent intracranial pressure, the following rules should be followed:
- drink the amount of fluid recommended by your doctor;
- ensure intake of vitamins with food or complexes;
- walk more, ventilate the room;
- avoid heavy loads and stressful situations;
- engage in moderate physical activity;
- Night sleep should be at least 8 hours;
- avoid sudden changes in climate and time zones;
- do not fly by air;
- sleep on high pillows with your head elevated;
- get up immediately after waking up;
- If possible, massage the collar area.
Prevention and maintaining a healthy lifestyle is the best tool for avoiding complications with intracranial pressure.
Source: https://SamMedic.ru/448538a-kak-opredelit-vnutricherepnoe-davlenie-metodyi-diagnostiki-norma-i-otkloneniya
What causes an increase in ICP?
The anatomical features of the human body imply the occurrence of certain physiological reactions to external and internal stimuli.
Under normal, resting conditions, the skull contains:
- brain tissue - 77.5%;
- cerebrospinal fluid (CSF) - 7.5%;
- venous blood - 7.5%;
- arterial blood - 7.5%.
An increase in the content of any component of the balance entails an immediate jump in ICP, while the self-regulation system does not always work properly.[ads-mob-2]
What causes increased intracranial pressure? For example, it grows after injury, when brain tissue becomes inflamed and swollen. The cause may be excessive production and poor outflow of cerebrospinal fluid.
The utilization of cerebrospinal fluid is delayed by displaced vertebrae and plugs in the subarachnoid ducts. Poor health appears due to stagnation of venous blood due to pinched or clogged blood vessels.
The strength of the flow of blood entering the brain generally depends on many factors:
- systemic arterial, atmospheric pressure;
- body position in space;
- quantity and quality of “working” vessels;
- volume, composition, density (blood);
- pathological reactions of vasoconstriction, vasodilation - narrowing and dilation of arteries, respectively.
What causes increased intracranial pressure? Doctors call the main causes pathologies of brain tissue, including age-related, traumatic, tumor, as well as disturbances in the flow of liquor and blood.
Norm
The pressure inside the skull is measured in millimeters of mercury or water column. The norm for an adult is in the range from 3 to 15 mm. In childhood, slightly reduced blood pressure is considered normal. An increase in cerebrospinal fluid volume leads to intracranial pressure. An increase of more than 30 mm can lead to severe damage to brain tissue and even death.
It is not possible to measure the pressure inside the skull at home; this requires the use of special instruments.
Increased ICP: symptoms
At each subsequent stage, the severity of the symptoms of intracranial hypertension increases. First, headache, apathy and lethargy appear.
As ICP progresses, more severe symptoms occur:
- hearing and vision impairments;
- Cushing's triad - high systolic pressure with low breathing and pulse;
- confusion or memory loss, disorientation;
- vestibular disorders accompanied by nausea and vomiting;
- epileptic syndrome;
- Posotonic reactions, including disturbances of muscle and respiratory reflexes, hiccups.
In case of ICP, using the methods of tomography, neurosonography, echoencephalography, rheoencephalography, doctors record significant changes in the cranium.
There is a narrowing of the cerebrospinal fluid spaces of the supratentorial and subtentorial localization with the simultaneous occurrence of the syndrome of the “tight” postcranial fossa. “Spurs” of the posterior horns of the lateral ventricles are formed, the Virchow-Robin spaces expand, and the cerebellar tonsils become sharpened. Flattened forms of the pons and pituitary gland are observed.
Increased intracranial pressure when diagnosing the symptoms of brain dislocation syndrome - severe displacement of its structures - is life-threatening. For example, infringement of the medulla oblongata due to dislocation of the cerebellar tonsils leads to complete blocking of circulatory and respiratory functions, and therefore to death.
What sensations accompany high ICP?
Severe migraine is reported in almost all patients with increased intracranial pressure. It is usually nonspecific and varies in type, location and frequency. The pain is usually described as diffuse, worse in the morning, and aggravated by the Valsalva maneuver. Symptoms of high intracranial pressure in men or women are quite variable. It should be noted that men are more likely to experience severe migraines than women.
Pain with high ICP is more common in the morning
Patients with diplopia most often complain of horizontal displacement of images. Horizontal diplopia is a symptom of false localized paralysis. Vertical diplopia is extremely rare.
Patients also report pulsatile tinnitus. It is a rhythmic sound heard in one or both ears, with a pulsating synchronous rhythm that can be aggravated by a certain position of the body in space. Other signs of intracranial pressure are not clinically significant. In some cases, symptoms do not appear for a long time and therefore patients do not seek medical help.
If any of the above syndromes appear, you should urgently consult a specialist. The occurrence of unfavorable sensations may be a sign of an impending stroke.
Blood pressure and intracranial pressure: what's the difference?
Nutrition of brain tissue is a priority task for the body, for which it proportionally strains the muscles, respiratory and cardiovascular systems. However, cerebral circulation, corrected by autoregulatory mechanisms, is relatively autonomous, “protected” from the systemic one.
The main regulators of cerebral circulation, in addition to cerebrospinal fluid, can be called:
- the tortuous shape of the elastic feeding arteries, which increases friction and slows down the flow;
- receptors of the vestibular apparatus;
- mechanoreceptors of pressure and stretching of blood vessels;
- chemoreceptors, which signal changes in the chemical composition of the blood;
- physiologically active substances that enhance or limit tone and vascular permeability;
- vascular smooth muscle cells that contract and dilate depending on mean arterial pressure (BP).
In the absence of pathologies, indicators of changing arterial and intracranial pressure practically do not correlate. Autoregulatory mechanisms are capable of blocking cerebral hypertension during blood pressure surges within the range of 60-170 mm Hg. Art.
ICP is the force of action of cerebrospinal fluid on brain tissue and cranial vaults. Blood pressure is the blood pressure generated by the cardiovascular system. The difference is obvious.
Blood pressure and intracranial pressure: what's the difference? The flow of blood obeys the general laws of hydrodynamics. It moves from an area of high pressure to an area of low pressure.
The normal level of perfusion - blood supply to the brain - is characterized by 60-70 mmHg. Art. Moreover, it is calculated as the difference between arterial, intracranial and venous pressure.[ads-mob-1]
Diagnosis of intracranial pressure
ICP level is measured in several ways:
- Study of brain function using CT or MRI;
- Insertion of a catheter connected to a pressure gauge into the tissue of the spinal cord or brain;
- Ultrasound of the brain, in children under 1 year of age - neurosonography (ultrasound through the parietal fontanel);
- Echoencephalography;
- Fundus examination to diagnose papilledema.
The choice of method for measuring intracranial pressure depends on the patient’s age and characteristics of the disease. Diagnosis of ICP in children under one year of age is carried out using echoencephalography and neurosonography. Patients with symptoms of acute cerebral circulation are prescribed an MRI, an examination of the condition of the fundus by an ophthalmologist.
Increased ICP and decreased blood pressure
This situation is familiar to many hypotensive people - people with pathologically low blood pressure levels. Hypotension can be physiological or acquired, temporary. The main cause of the disease is autonomic vascular dysfunction caused by disorders of nervous activity.
Increased intracranial pressure and low blood pressure are formed simultaneously with:
[ads-pc-3]
- brain injuries with large blood losses;
- the presence of pathological formations;
- cerebral vasospasm - compression of cerebral vessels;
- the action of physiologically active substances, chemicals;
- increased secretion of cerebrospinal fluid, disturbances in its outflow.
Increased intracranial and low blood pressure can be symptoms of serious endocrine disruptions, as well as diseases that destroy the brain. If such conditions occur frequently, it is necessary to undergo a thorough medical examination.
Visual impairment
Another characteristic sign of increased ICP may be impaired visual perception. This can be manifested by double vision, blurred objects, passing attacks of complete loss of vision, fog before the eyes, and decreased light perception. These symptoms indicate compression of the optic nerves as a result of increased ICP.
With increased ICP, the shape of the eyeball can change, up to such a strong protrusion that it becomes impossible to close the eyelids. Dark circles form under the eyes due to congested veins.
Nausea and vomiting also often accompany increased ICP. In this case, vomiting does not alleviate the patient’s condition. Intracranial pressure can increase with some common events, such as bending, sneezing, and stress. However, such an increase is short-term and quickly passes on its own, without causing discomfort. If the pressure does not decrease, then we should talk about a chronic form of increased ICP.
Increased headache pressure from the point of view of traditional medicine
Popularly, “dropsy of the brain” is treated with diuretic herbs and avoidance of substances that excite the nervous system.
From the point of view of traditional medicine, increased headache pressure is a sign of advancing old age, forcing one to give up active activities.
The need to wean yourself from caffeine-containing drinks, alcohol, salt, and cigarettes is promoted not only by official medicine, but also by alternative medicine. Herbalists strictly prohibit the use of teas containing aralia, gorse, rhodiola, immortelle, lemongrass, bearberry, and ginseng.
From the point of view of traditional medicine, increased headache pressure is a condition that is subject to feasible correction. In addition to diuretics, popular healers advise eating more foods containing potassium and magnesium.
Complications
Increased ICP in chronic form tends to intensify over time, and therefore requires correct and timely therapy. In the absence of this, the disease can lead to such serious complications as:
- Paralysis.
- Speech impairment.
- Stroke.
- Mental abnormalities.
- Epilepsy.
- Blindness.
- Impaired motor function, namely coordination.
In women who are overweight at a young age, increased ICP can go away on its own without specific therapy. However, you should not hope for this and it is better to consult a doctor to conduct the necessary examination and make the correct diagnosis, as well as exclude more serious diseases.