Focal neurological symptoms
(
focal neurological deficit
) is a term that refers to neurological symptoms characteristic of local damage to certain structures of the central or peripheral nervous system. Focal neurological symptoms in many cases are combined with general cerebral symptoms, which are a manifestation of diffuse damage [1]. Focal neurological symptoms allow not only to identify the presence of local damage, but also to carry out topical diagnostics, that is, to fairly reliably determine the area of damage based on knowledge of neuroanatomy.
Focal neurological symptoms are characteristic of a number of diseases, including traumatic brain injury[2], brain tumors, strokes, etc.[3]
Lesions of the cerebral cortex[edit | edit code]
Damage to the frontal lobe cortex[edit | edit code]
Left frontal lobe highlighted in red
Frontal lobe damage usually involves the motor system and can present with a variety of symptoms, depending on which part of the frontal lobe is affected:
- unsteady gait (unsteadiness when walking);
- muscle rigidity, difficulty in passive movements in the limbs (hypertonicity);
- paralysis of one limb (monoparesis) or two limbs on one side of the body (hemiparesis);
- paralysis of the head and eye movements
- a speech disorder in which a person has difficulty finding words, synonyms, cases, sound order, grammatical tense, that is, motor aphasia (Broca's aphasia);
- focal epileptiform Jacksonian seizures, that is, tonic or clonic spasms of the fingers or toes that are not accompanied by loss of consciousness;
- grand mal epileptic or tonic-clonic seizures;
- the appearance of “frontal psyche”, that is, personality changes such as disinhibition, foolishness (inappropriate jocularity), causeless rage, lack of initiative and indifference, apathy, akinetic mutism (“waking coma”, in which the patient does not speak, does not answer questions and does not comes into contact with others while maintaining consciousness), general lethargy, tendency to antisocial acts (arson, attacks);
- “frontal signs”, that is, a return to primitive reflexes such as the proboscis, grasping and palmo-oral reflexes;
- unilateral loss of smell (anosmia).
Damage to the parietal lobe[edit | edit code]
The left parietal lobe is highlighted in red.
Damage to the parietal lobe is manifested by disturbances in sensitivity and perception, including:
- impaired tactile sensitivity;
- violation of kinesthesia, that is, postural sensations (the sensation of changing the position of the body in space) and the sensation of passive movement;
- syndromes of sensory and visual neglect, that is, the inability to pay attention to things in certain parts of the sensory or spatial environment of a person, in its extreme form this can be “abandonment of a limb”;
- loss of the ability to read, write or count (dyslexia, dysgraphia, dyscalculia);
- loss of ability to find a specific place (geographic agnosia);
- loss of the ability to recognize familiar objects when feeling them with closed eyes (astereognosia - a type of tactile agnosia).
Damage to the temporal lobe cortex[edit | edit code]
The left temporal lobe is highlighted in red.
Signs of damage to the temporal lobe are manifested by defects in auditory perception, convulsive syndrome, hallucinations, etc., in particular, the following may be observed:
- deafness without damage to ear structures (cortical deafness);
- tinnitus, auditory hallucinations;
- loss of the ability to understand music or language - sensory aphasia or Wernicke's aphasia;
- amnesia (loss of long-term and/or short-term memory);
- other memory disturbances such as déjà vu;
- complex multimodal hallucinations;
- complex partial seizures (temporal lobe epilepsy).
Damage to the occipital lobe[edit | edit code]
The left occipital lobe is highlighted in red.
When the occipital lobe is damaged, the cortical part of the visual analyzer usually suffers, as evidenced by:
- complete loss of vision (cortical blindness);
- loss of vision with denial of loss (Anton-Babinsky syndrome);
- loss of perception of the same right or left halves of the visual field (homonymous hemianopsia);
- visual agnosia - inability to recognize familiar objects, colors or faces;
- visual illusions such as micropsia (objects appear smaller) and macropsia (objects appear larger);
- visual hallucinations displaying elementary forms, such as zigzags and flashes in one half of the visual field for each eye separately; they should be distinguished from temporal visual hallucinations, which display complex shapes and fill the entire visual field.
What are these focal neurological symptoms?
Clinical signs are conventionally divided into three categories - general, mental, and focal neurological. Symptoms include high temperature, poor appetite, chills, headache and dizziness, drowsiness and weakness - these signs are characteristic of diseases that differ in cause, developmental features, and complications.
Focal neurological symptoms are a set of signs that the doctor studies in order to determine the exact location of the affected area of the brain. Damage to the frontal lobe cortex is indicated by a sharp increase in muscle tone, speech disorder and the inability to perceive it, tremors of the head and limbs, as well as impaired coordination of movements.
If the parietal side of the brain is affected, the patient’s sensitivity and quality of brain activity decrease, and the patient loses the ability to write. The manifestation of epileptic seizures, sudden memory loss and the development of deafness with damage to the temporal lobe.
Mental symptoms predominantly accompany neurological symptoms and much less often develop as an independent pathology. Insomnia, chronic anxiety, and causeless irritability indicate a mental disorder.
Damage to the extrapyramidal nervous system[edit | edit code]
| This section is not completed. You will help the project by correcting and expanding it. |
Cerebellar lesion[edit | edit code]
Main article: Cerebellum § Symptoms of lesions
Cerebellar lesions usually cause problems with balance and motor coordination and may present with the following symptoms:
- ataxia - unsteady and clumsy movements of the limbs or torso;
- inability to coordinate fine motor skills (tremor, poor finger-nose test);
- dysdiadochokinesia - the inability to perform rapid alternating movements, for example, quickly bend and straighten fingers; voluntary eye movements are inhibited in extreme positions and lead to saw-tooth movements (nystagmus).
Brainstem stroke
Conservative therapy
Acute disorders of cerebral circulation of the brainstem zone require urgent hospitalization in a specialized vascular center or neurological hospital - optimally in the first 3 hours from the moment of onset.
The basis of therapy is conservative measures, which begin at the prehospital stage with the provision of emergency care, oxygenation, symptomatic correction (hypotensive, anticonvulsant). Early treatment helps improve the prognosis even with severe lesions. Restoration of vital functions, including mechanical ventilation, is carried out in the intensive care unit, where, after determining the characteristics of the brainstem stroke, specific treatment begins. It is aimed at restoring blood flow through the vessels of the vertebrobasilar bed, preventing complications and eliminating them, minimizing the risk of relapse, and normalizing basic physiological and biochemical constants. The key areas of drug therapy are:
- Intravenous thrombolysis.
The administration of thrombolytic agents (recombinant plasminogen activator) is indicated in the most acute period of the ischemic process. Despite the high efficiency of recanalization of arterial stenoses, such treatment has many contraindications and increases the risk of hemorrhagic complications. - Anticoagulants and antiplatelet agents.
The progressive course of brainstem stroke requires the use of anticoagulants - first low-molecular-weight heparins, then oral agents. They are also prescribed for preventive purposes after stabilization of cerebral hemorrhages. In all cases of acute brain stem ischemia, antiplatelet agents (acetylsalicylic acid) are required. - Neuroprotectors.
To improve cerebral perfusion, increase the regenerative potential of the affected nervous tissue, and accelerate the recovery of impaired functions, neuroprotectors are used. These include vasoactive (vinpocetine, pentoxifylline), neurotrophic agents (a complex of cerebral peptides or animal blood hemoderivat), antioxidants (thioctic acid, ascorbic acid, inosine).
Neurorehabilitation
Early comprehensive rehabilitation is of utmost importance for eliminating the consequences of brainstem stroke and restoring the functional capabilities of patients. The medical direction is based on ongoing neuroprotective therapy, spasticity and contractures are treated with muscle relaxants, and concomitant emotional and mental disorders are corrected with antidepressants.
Neurorehabilitation involves the use of kinesiotherapy, exercise therapy, and massage. Modern hardware technologies are being introduced into everyday practice in the form of robotic simulators operating using a biofeedback mechanism. Cyclic exercises allow you to activate the patient, restore movement, coordination and walking function. The possibilities for comprehensive rehabilitation are expanded by physical procedures, psychotherapy, social and labor adaptation.
Surgery
Radical correction of brainstem ischemic stroke involves the use of intravascular recanalization methods. Taking into account the clinical situation, selective intra-arterial thrombolysis, mechanical or aspiration thrombectomy, balloon angioplasty with stenting of extracranial vessels can be used. After intracranial hemorrhage with dislocation of brain structures, the hematoma is removed and decompressed through hemicraniectomy. Ventricular drainage surgery helps eliminate acute hydrocephalus.
Experimental treatment
Given the low level of evidence for existing drugs for neuroprotection, a search for new drugs is being conducted. The possibilities of antagonists of glutamate and NMDA receptors (eliprodil, selfotel), cytoprotective agents (lubeluzole), antioxidants (tirilazide) are being studied. Methods of stereotactic and endoscopic removal of hematomas require further study; ventricular thrombolysis and local hemostasis with recombinant factor VIIa are at the testing stage.
Damage to the limbic system[edit | edit code]
The left half of the limbic system is highlighted in red.
Damage to the limbic system includes memory loss or impairment and may include the following symptoms:
- loss or confusion of long-term memory to focal neuropathy (retrograde amnesia);
- inability to form new memories (anterograde amnesia);
- loss or decrease in emotionality (apathy);
- loss of smell (anosmia);
- loss of ability to make decisions and learn new skills.
What is important to know about dysfunction of the midline structures of the brain
Dysfunction is a disruption in the functioning of any part of the body, organ or an entire system of the human body, leading to corresponding problems. When it comes to middle structures, it is immediately impossible to deny their importance for humans. They regulate many processes, such as breathing or body temperature.
How does the pathological condition manifest itself?
What signs will occur with the development of dysfunction affecting the midline structures depend on the location of the affected tissues and cells in the brain. The nervous and endocrine systems are most often affected.
The nervous system often develops a disorder of skin sensitivity. Usually there is an increased sensitivity to painful stimuli, when even the slightest impact provokes not just discomfort, but pronounced pain. Tremor (trembling of the limbs) often occurs.
On the part of the endocrine system, hormonal disruptions are observed, which can be accompanied by hyperthermia, as well as disturbances in the functioning of the vascular system, which is expressed by a tendency to low or high blood pressure (see Hypertension). A serious problem is also early puberty, associated with a dysfunctional state of the mid-stem structures of the brain.
A sign that can accompany both endocrine disorders and deviations in the functioning of the nervous system is mood lability. The person begins to behave atypically, his emotional state easily moves from hysterics with tears to uncontrollable laughter. There are no reasons for such mood swings.
When dysfunction is present in young children
In children, the dysfunctional state of the median structures has the addition of “minimal” in the diagnosis. This pathological condition is observed quite often and is manifested by a wide range of symptoms, which include:
- severe headaches;
- excessive physical activity and increased excitability of the nervous system;
- constant nervous and irritable state;
- disorder of motor and speech functions, their slowdown;
- mental retardation;
- impairment of memory and attention.
All of the above can cause other deviations that have significant consequences. Such diseases most often include epilepsy and other significant disorders of the nervous system.
Treatment
In the treatment of dysfunction of the median structures, the main role is played by a neurologist, who chooses the optimal scheme for restoring the functions of this part of the brain in a child.
The current approach is the use of neuropsychological and pedagogical correction, when the emphasis is on modifying the child’s behavior and emotional response. If there is no effect, tranquilizers, antidepressants, psychostimulants and nootropics are prescribed. The selection of medications is strictly individual and requires taking into account the characteristics of the child’s body.
Doctors also use vitamin supplements and physical therapy in the therapeutic regimen. Preference is given to manual therapy, kinesitherapy, as well as acupuncture and electrical stimulation. There are some traditional methods of treatment, but their use should be strictly discussed with the doctor and act only as an auxiliary therapy, and not as the main one.
All about motor hyperactivity disorder and attention deficit disorder: signs, causes and treatment.
Find out about Farah's disease: causes, symptoms, diagnosis and treatment of the pathology.
Summarize
If a dysfunctional state of nonspecific midline structures located in the brain appears in a child and is mild in severity, the prognosis is favorable. In such a situation, chances are that the problem will resolve itself as the little patient matures, and by adolescence there will be nothing to worry about.
When the pathology is more severe, and the disorders strongly affect the state of the nervous and endocrine systems, a certain correction is required. If you follow the doctor’s recommendations and work with the child, dysfunction can be overcome without consequences for his adult life.
(1 5,00 of 5) Loading...
Source: https://golmozg.ru/stroenie/disfunkciya-sredinnyh-struktur.html
Notes[edit | edit code]
- Lovell MK, Franzen MD
Neuropsychological assessment // Neuropsychiatry of Traumatic Brain Injury (English) / Silver JM, Yudofsky SC, Hales RE. - Washington, DC: American Psychiatric Press, 1994. - P. 152-153. — ISBN 0-88048-538-8.. — “Although brain injuries are often described as diffuse or focal in nature, in reality many traumatic brain injuries have both focal and diffuse components.”. - Thiruppathy SP, Muthukumar N.
Mild head injury: revisited // Acta Neurochir (Wien). - 2004. - Vol. 146. - P. 1075-1082. - PMID 15744844. - Thal GD, Szabo MD, Lopez-Bresnahan M. et al.
Exacerbation or unmasking of focal neurologic deficits by sedatives (English) // Anesthesiology (English) Russian.. - Lippincott Williams & Wilkins (English) Russian., 1996. - Vol. 85. - P. 21-25. - PMID 8694368.
| This is a draft article on neurology. You can help the project by adding to it. |
Forms of the disease
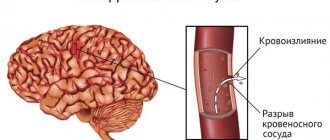
Depending on the location of the hemorrhage, the following types of hemorrhagic strokes are distinguished:
- subarachnoid - bleeding comes from the vessels of the arachnoid membrane, blood flows into the subarachnoid space (i.e., the space between the arachnoid and soft membranes);
- intracerebral - the hematoma is located in the thickness of the brain tissue;
- ventricular - blood enters the cerebral aqueduct or ventricles;
- mixed - combines characteristics of two or more species.
Depending on the duration of the pathological process, the following stages of hemorrhagic stroke are distinguished:
- The sharpest. Lasts the first 24 hours from the moment of hemorrhage. It is critical that qualified medical care be provided during this period.
- Spicy. It begins one day after the stroke and lasts 3 weeks.
- Subacute. It begins on the 22nd day of the disease and lasts up to 3 months.
- Early recovery. From three months to six months.
- Late recovery. From six months to a year.
- Stage of long-term consequences. It begins a year after the stroke and lasts until its consequences disappear, in some cases for life.
Possible consequences of hemorrhagic stroke and complications
The formation of a hematoma in the area of the ventricles of the brain causes disturbances in cerebrospinal fluid dynamics, as a result of which cerebral edema rapidly progresses, which, in turn, can lead to death in the first hours of hemorrhage.
The most common variant of the disease is bleeding into the brain parenchyma. Blood permeates the nerve tissue and causes massive neuronal death. The consequences of a hemorrhagic stroke in this case are determined not only by the location of the pathological focus, but also by its size.
After extensive hemorrhage, the following complications are observed in the long-term period:
- impaired movement of the limbs, lack of coordination;
- lack of sensitivity in the affected areas of the body;
- swallowing disorders;
- dysfunction of the pelvic organs;
- difficulties in the process of perceiving, processing and remembering information, loss or decrease in the ability to generalize and logical thinking;
- speech, counting, and writing disorders;
- various mental and behavioral disorders (disorientation in space, anxiety, detachment, suspiciousness, aggressiveness).