Steps in the development of the pathological process
Microangiopathy of the brain is considered a fairly common pathology, which is characterized by impaired tone, the structure of the walls of blood vessels and capillaries directly in this organ.
As a result, the patient experiences a disrupted metabolic process of brain tissue. The more the disease progresses, the less elasticity of the vascular wall becomes, and the vascular lumen thickens and decreases. This can lead to obstruction of small vessels for intense blood flow. As a result, brain neurons suffer from a lack of blood flow, oxygen and glucose.
Once the vessels become weaker, they begin to break, which can cause subarachnoid hemorrhage. If there is no blood flow, then local death of neurons occurs, foci are replaced by gliosis, and scars form.
Treatment
Treatment of cerebral microangiopathy includes measures aimed at slowing the progression of the disease, restoring blood flow and brain function, and preventing the development of acute conditions. Therapy program:
- Normalization of blood pressure indicators.
- Regulation of lipid and carbohydrate metabolism in case of their violation.
- Correction of excess weight.
- Fighting physical inactivity and bad habits (smoking, alcohol abuse).
- A diet low in animal fats and salt.
Hypertensive drugs are indicated - mainly angiotensin receptor antagonists and inhibitors (substances that suppress, delay the process) of the angiotensin-converting enzyme, which have anti-inflammatory and antioxidant effects, increase the reactivity of small vessels in the brain.
Metformin is usually used to regulate hyperglycemia, and drugs from the statin group are used to lower cholesterol levels. To prevent thrombosis, antiplatelet therapy is carried out, most often with Dipyridamole alone and in combination with acetylsalicylic acid. Simultaneously with taking pharmaceuticals, physiotherapy procedures, therapeutic exercises, and massage are prescribed.
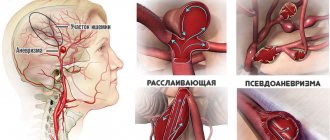
Angiopathy of cerebral vessels is a lesion of blood vessels caused by their innervation.
For some reason, the nerves that transmit the command to the vessels to change tone cease to do so properly. Blood circulation is impaired.
With prolonged angiopathy, irreversible changes in blood vessels occur, and hemorrhages are frequent. Why is the innervation of cerebral vessels disrupted? What diseases cause angiopathy?
With atherosclerosis, a change occurs in the inner lining of the arteries (lipids, complex carbohydrates, blood components, fibrous tissue accumulate) and the middle lining. Similar changes occur throughout the body. But, above all, in the brain. Moreover, plaques are not only deposited in the vessels, hemodynamic restructuring occurs due to stenosis and obliteration.
With atherosclerotic angiopathy, a number of interrelated pathological processes occur in the brain:
- the formation of atherosclerotic plaques of various structures and sizes in one or more arteries and subsequent changes in them;
- atherostenosis;
- narrowing and closing of the lumens of the arteries;
- atheroembolism;
- thrombosis in the area of the plaque or beyond it;
- structural changes in cerebral vessels under the influence of reduced or increased blood flow in them.
These pathological phenomena are observed at all important levels of the vascular system of the brain.
Signs of atherosclerotic angiopathy:
- weakening of short-term memory;
- headaches, noises in the head and dizziness;
- irritability;
- decreased concentration;
- sometimes fainting and insomnia.
Atherosclerotic changes in blood vessels are very diverse. And this must be taken into account when organizing treatment, the main goal of which is to create artificial blood flow to the vessels.
Vegetative-vascular dystonia refers to disorders of autonomic functions that vary in origin and manifestations. This syndrome is explained by a disorder of nervous regulation.
Innervation of blood vessels leads to angiopathy. Vegetative-vascular dystonia is common. Both children and adults get sick.
The prevalence of the syndrome in the modern world is explained by the crazy pace of life, which requires full dedication of internal strength, and frequent stress.
Causes of autonomic dysfunction:
- heredity (VSD in children);
- diseases of the nervous system;
- chronic pathologies (especially in cases where the process occurs in the cardiovascular, endocrine or gastrointestinal system);
- chronic stress;
- overstrain, overwork.
2. His psyche is not able to process this experience, therefore it represses the traumatic situation.
3. As a result, various somatoform disorders appear. Moreover, internal organs often become targets for neurotic attacks.
How does autonomic dysfunction manifest? Let's name the most common syndromes:
- cardiovascular (jumps in blood pressure, pulse, heart rate, pain in the heart region of varying intensity, not associated with physical activity);
- respiratory (difficulty breathing, rapid breathing, muscle spasms, dizziness, etc.);
- “irritable bowel” (any disorder of the digestive tract, from loss of appetite and nausea to abdominal pain);
- increased sweating of the palms and feet;
- frequent painful urination (without symptoms of urinary system diseases);
- sexual disorders (decreased libido, impaired erection and ejaculation in men; anorgasmia in women);
- slight persistent increase in temperature, chills (especially in children).
The main treatment is psychotherapeutic. Plus a healthy lifestyle. For persistent angiopathy, a course of drug treatment is necessary.
There is no uniform classification of angiopathy. Scientists have put forward many hypotheses regarding the division of this pathological process into forms.
Its treatment directly depends on what type of vascular damage occurs. In this regard, it is customary to highlight:
- Microangiopathy of the lower extremities is a lesion of small vascular formations that are part of the microvasculature (arterioles, capillaries, venules, arteriovenular anastomoses). It is predominant in the structure of all causal mechanisms for the development of angiopathy of this localization. Very often combined with other vascular lesions: retinopathy (retinal dysfunction), nephropathy (renal blood flow disorders).
- Macroangiopathy is a structural and functional transformation of arterial structures of medium and large caliber, which is characteristic only of lesions of the vessels of the lower extremities.
Angiopathy of cerebral vessels is a disease, the essence of which is a decrease in vascular tone, as a result of which the structure and function of their walls are disrupted.
The pathogenetic component of this condition may be different, but the outcome in each case is the same - the death of tissue cells that nourished the vessel is observed.
There are several forms of angiopathy, including:
- angiopathy as a result of diabetes mellitus;
- angiopathy as a result of arterial hypertension or hypotension;
- angiopathy of the hands and feet;
- retinal angiopathy;
- arterial angiopathy;
- traumatic form of the disease;
- cerebral angiopathy.
Among the factors that can cause the development of angiopathy are the following:
- Traumatic injuries;
- Cervical osteochondrosis;
- Smoking;
- Increased intracranial pressure;
- Blood diseases;
- Disorders of nervous regulation, which is responsible for the tone of the walls of blood vessels;
- Unfavorable working conditions;
- Elderly age;
- Diabetes;
- Intoxication of the body;
- Arterial hypertension;
- Congenital features of the structure of the walls of blood vessels.
The most important structure of the eye, the retina, quickly responds to the slightest disturbance in the blood supply system. Angiopathy is not an independent disease; it serves as a signal of a disease that has a negative effect on the eye vessels.
Pathological processes in the body cause damage to the walls of the eye vessels, their modification and disruption of the structure.
The main risk factors for all forms of angiopathy:
- congenital features of the walls of blood vessels;
- diseases of the hematopoietic system;
- metabolic disorders;
- intoxication;
- traumatic injuries;
- overweight;
- elderly age;
- presence of bad habits;
- passive lifestyle.
Symptoms
These are the common symptoms that patients present with most often. Below we will look at the two most dangerous variants of angiopathy - diabetic, as well as a variant affecting the lower extremities.
Signs of the pathological process depend mainly on the location of the lesion.
Depending on this, you may experience:
- Reduced visual acuity up to its complete loss;
- Pain in the head;
- Burning sensation in the lower extremities;
- Pain in the legs, followed by intermittent claudication;
- Repeated cases of intense nosebleeds, as well as from the gastrointestinal tract;
- Hematuria – blood in the urine;
- Skin changes in the form of petechiae or telangiectasias;
- Hemoptysis;
- Trophic disorders such as increased dryness of the skin or its peeling, up to gangrene.
The clinical picture of angiopathy of the extremities depends on the stage of the process, the age of the patient and his general condition.
The course of angiopathy is divided into several stages depending on the severity of the process. The effectiveness of subsequent treatment directly depends on the stage of the disease.
- I Art. – absence of clinical signs, except for atherosclerotic changes in the arteries during examination.
- II Art. – stage of intermittent claudication. When walking a certain distance, muscle soreness appears, forcing the patient to stop and rest. Sometimes the pain may be replaced by weakness or heaviness in the legs.
- III Art. – painful sensations appear not only when walking, but also at rest, and even in a lying position. In this case, changing the position of the leg, as a rule, helps the pain disappear.
- IV Art. – the most severe stage, with the development of superficial ulcers and areas of necrosis.
Among the main signs of angiopathy are the following:
- periodic sensations of “crawling”, numbness and burning in the legs;
- pain when walking (usually disappears at rest), intermittent claudication, which makes it impossible to walk long distances;
- bleeding from the nose, gastrointestinal tract, bronchi, multiple hemorrhages on the skin, the appearance of spider veins on the legs;
- disorders of tissue trophism, characterized by peeling and laxity of the skin up to the appearance of necrotic and gangrenous areas;
- deterioration of vision up to its loss.
- Angioprotectors (Troxerutin). The drugs are used to reduce the permeability of vascular walls and normalize metabolic processes.
- Hemostatics (Ditsinon). Help prevent or stop spontaneous hemorrhage.
- Antispasmodics (No-spa). Medicines eliminate pain caused by vascular spasm.
- Biogenic stimulants (Solcoseryl). Accelerate metabolism and healing processes, improve the condition of the walls of veins and arteries.
- Nootropics (Pantogam, Nootropil). They increase the resistance of nerve cells to hypoxia and restore the functions of the central nervous system.
- Anticoagulants and antiplatelet agents (Heparin, Aspirin). Prescribed for cerebral angiopathy caused by increased blood clotting.
- Carotid endarterectomy. The affected vessel is dissected, and blood clots or atherosclerotic deposits are removed through the resulting incision.
- Angioplasty with stenting. A probe equipped with a balloon is inserted through a puncture in the femoral artery. Under X-ray control, the device is moved until it reaches the affected area. Installing a stent helps maintain the required diameter of the artery.
- Trepanation of the skull. It is performed for bleeding in the brain. The operation is aimed at removing the hematoma and reducing the severity of edema.
Causes and provoking diseases
Cerebral microangiopathy syndrome can develop against the background of other pathologies. The disorder occurs as a result of the following diseases and conditions of the human body:
- Thrombosis . Blood flow is disrupted due to the formation of clots.
- Necrosis . Cells and tissues die.
- Hyalinosis . Hyaline deposition occurs.
- Fibrinoid swelling . Vascular permeability becomes increased and, as a result, destruction of connective tissue is observed.
Microangiopathy of the brain can also be provoked by:
- anomaly in the structure of the vascular wall;
- smoking;
- drinking alcohol;
- poor blood clotting;
- injury;
- infectious diseases that negatively affect the condition of blood vessels;
- diseases of the endocrine system;
- high blood pressure;
- diseases of the cardiovascular system;
- toxic substances;
- old age.
Angiopathy of the lower extremities treatment with folk remedies
Medicinal tea
Ingredients:
- hawthorn;
- arnica;
- elecampane root;
- blueberry;
- nettle leaves.
Preparation and use:
- Mix a collection of herbs weighing 15 grams and pour boiling water over it. Let it brew for about an hour.
- Strain and take before meals.
Herbal compress
Ingredients:
- calendula flowers;
- linden buds;
- ground nettle leaves.
Preparation and use:
- Pour boiling water over the collection and leave.
- Wrap the herbs in gauze, apply to clean feet and secure. Leave for 20 minutes.
- Rinse with warm water and put on socks.
- Repeat 3 times a day.
Not united by the brain
In modern medicine, there are several types of microangiopathy:
- Cerebral microangiopathy. The pathological process is observed directly in the brain. It is characterized by a long-term disruption of cerebral blood flow, which occurs against the background of atherosclerosis or high blood pressure. It has symptoms of encephalopathy, ischemia and lacunar infarction, which lead to damage to the gray matter. Signs of the disease appear in later stages, helping to distinguish it from other brain disorders.
- Diabetic . Occurs due to persistently elevated glucose levels. As a result, there is damage to small vessels that provide blood flow to internal organs. There are several clinical forms of this type of pathology.
- Lesions in the legs . The patient has damage to the capillaries of the lower extremities. It is characterized by slow blood flow, impaired tissue nutrition, and damage to certain areas of the legs. If immunity is reduced, then the pathology begins to progress.
- Microangiopathy of the liver . The patient experiences changes in the vascular wall, impaired blood clotting and slow blood flow. As a result, blood clots form, blood viscosity increases, and platelets are activated.
Diabetic microangiopathy
This form of microangiopathy develops due to an increase in blood glucose levels above normal levels. Against this background, patients experience damage to the walls of small-caliber vessels (venules, capillaries and arterioles) located in close proximity to the body tissues. In this case, the clinical picture completely depends on the location of the lesion.
Microangiopathy of the diabetic type is one of the most dangerous manifestations of diabetes mellitus. This is due to the fact that the pathology provokes a disruption in the processes of tissue nutrition and the removal of various metabolites from them. As the disease progresses, vasoconstriction occurs, signs of oxygen starvation of tissues become more pronounced, and the course of the disease worsens significantly.
Irreversible narrowing of the walls of blood vessels is a consequence of:
- Damage to the membranes of small arteries;
- Endothelial proliferation;
- Thickening of basement membranes;
- Accumulations of mucopolysaccharides in the walls of arteries.
At the same time, as a result of an increase in osmotic pressure caused by an increase in the level of fructose in the blood and excessive water intake, patients experience an increase in edema in the cells, and due to impaired metabolism of proteins and fats, the condition of the blood vessels suffers.
The most characteristic manifestations of this type of microangiopathy are:
- Diabetic nephropathy (occurs in about a third of patients and is characterized by impaired renal function, swelling of the kidneys, and the presence of large amounts of protein in the urine);
- Diabetic angioretinopathy (damage to the vessels of the retina of the eyeball);
- Microangiopathy of vessels located in the lower extremities.
Clinical picture
Cerebral microangiopathy at the initial stage is asymptomatic, so its diagnosis becomes more complicated. This pathological process can manifest itself with a number of symptoms:
- memory impairment;
- consciousness becomes cloudy;
- causeless weakness of the body;
- frequent and intense headaches.
These disorders occur due to poor blood flow in the capillaries of the brain. The development of symptoms occurs gradually. First, unreasonable weakness occurs, which may be accompanied by a headache.
In this situation, painkillers do not have the desired positive effect. Then gradually the patient begins to suffer from insomnia at night, and drowsiness during the day.
After the disease begins to progress, the patient experiences absent-mindedness, forgetfulness and inattention. The thinking process is disrupted. In parallel, focal signs of cerebral microangiopathy are observed:
- unsteady gait;
- violation of movement coordination;
- convergence disorder;
- the diameter of the pupils is completely different;
- other pathological reflexes.
Symptoms
The clinical picture often proceeds without a trace and slowly. The progression of the disease leads to micro-strokes and total dementia.
- Headache. 70% of patients complain about it. Frequent headache is an early sign of progressive amyloid angiopathy of the brain. Pain is often located where foci of angiopathy have arisen.
- Nausea and vomiting. Occurs in 30-40% of patients.
- Convulsive seizures. Observed in 25% of patients. The nature of seizures and epileptic equivalents depends on the location: in the motor cortex - limb spasms, in the parietal cortex - illusions and simple hallucinations.
- Intracerebral hemorrhages. They occur in 17% of patients. The peculiarity of strokes is that they are prone to recurrence. Most often, hemorrhage occurs in the frontal, occipital and parietal lobes. The severity of strokes with amyloid angiopathy varies: from spontaneous numbness of half the body to deep coma.
- Mental disorders. Most often, the intellectual properties of a person are affected. As the disease progresses, intelligence gradually decreases, up to profound dementia. In addition to intelligence, memory decreases and attention wanders.
- Transient neurological disorders. They are manifested by absence seizures, paresthesias, epileptiform seizures, and visual hallucinations. Absence is a temporary loss of consciousness while maintaining muscle tone from 1 to 60 seconds. After this, the patient comes to his senses and does not know that he will stand for several seconds in a disconnected state. Paresthesia is a sensitivity disorder in which the patient feels like goosebumps are crawling up his arms, tingling and numbness are felt. Epileptiform seizures are sudden shaking of the arms or legs.
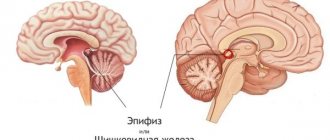
Diagnostics and medical care
When diagnosing, an MRI is performed, which helps to examine the brain tissue and its vascular network. If a patient develops this pathology, then signs of arterial hypoplasia are clearly visible. Foci of infarction are also visible.
It is recommended that the patient undergo Doppler ultrasound. At the same time, a blood test is taken.
Treatment of cerebral microangiopathy is carried out comprehensively.
- The patient is required to be prescribed medications that normalize blood pressure ;
- to eliminate the lack of oxygen in the brain tissues, it is necessary to take antihypoxants ;
- to reduce lipid levels it is necessary to take statins and sequestrants;
- nootropics are used to improve brain nutrition , and drugs based on nicotinic acid improve blood flow.
It is worth considering the fact that timely treatment helps to stop the development of the disease. This is important in old age, since in this case the pathological process is accelerated.
More information about the treatment of cerebrovascular diseases:
Development mechanism
The pathological process is based on a whole group of disorders. There are three main points.
- Changes in the nervous regulation of vascular tone. As a rule, it is represented by insufficient functional activity of the central and peripheral systems.
It is accompanied by weak impulse transmission, because the arteries, veins, capillaries are in reduced tone, but at the same time a spasm often develops, that is, a narrowing of the structures and disruption of local blood flow.
- Next comes the hormonal factor. A group of specific substances is responsible for the normal functional activity of blood vessels: cortisol, adrenaline, aldosterone, angiotensin-2, and partially renin, which is an intermediate compound.
All of them, when synthesized excessively, provoke disruption of the normal functioning of arteries and other vessels.
When the factor is corrected, the pathological process quickly disappears and the blood flow returns to normal.
Metabolic abnormalities should be considered in a broader context; other metabolic processes also play a role.
- The third factor, which is somewhat less common, is infection.
In this case, narrowing and destruction of one, or very rarely several, vessels is observed; a clear localization of the disorder can be detected, which is extremely difficult, if not impossible, to do in other cases.
Typically, this form of angiopathy is the result of phlebitis, or vasculitis.
It is extremely rare that an isolated factor in the development of the disease is discovered. Much more often, doctors have to deal with a whole group of reasons.
The problem is that these disorders, one way or another, give rise to other pathogenetic mechanisms, and the longer the condition exists, the more complex it becomes both in terms of diagnosis and treatment.
Conclusion - at the first symptoms of a disorder or if one is discovered during an examination, you need to urgently consult a doctor.
Profile specialists - vascular surgeon (or general practitioner, if there is none in the access area), hematologist. It is possible to involve other doctors.
Consequences and prevention
The prognosis for this diagnosis will largely depend on the patient’s age group, the extent of the lesion, concomitant diseases and the timeliness of therapy. If you ignore the development of the disease, cerebral insufficiency may develop, which will lead to death.
The health of the entire body depends on the condition of the blood vessels. Even if minor changes or disturbances are observed, pathologies will arise that may be incurable. Therefore, it is worth paying attention not only to correctly selected treatment, but also to preventive measures, which include:
- healthy lifestyle;
- proper and balanced nutrition, it is advisable to adhere to a salt-free diet;
- exclusion of stressful situations and intense physical activity;
- rejection of bad habits;
- a properly structured work and rest schedule.
The above measures are simple, and if you follow them, you can avoid many problems with blood vessels.
It is worth remembering that cerebral microangiopathy of the brain is a serious disease that must be treated immediately. The sooner therapy is prescribed, the greater the likelihood of avoiding complications.
The role of vegetative-vascular dystonia
One of the key factors in the occurrence of vasopathy is autonomic dysfunction. Abbreviated as VSD, that is, vegetative-vascular dystonia. This condition is caused by a disorder in nerve regulation. According to the latest data, every 5 people suffer from VSD. Moreover, both adults and children, including infants, are prone to this disease.
Among the provoking factors of autonomic dysfunction are:
- Hereditary burden, when even a newborn child has a predisposition to the process;
- Diseases of the central nervous system;
- Chronic stress;
- Prolonged fatigue and overstrain.
VSD indicates the close connection that exists between the nervous system and internal organs. Violation of one link leads to disruption of another. Thus, long-term stress causes diseases of various human organs. Its target may be the heart or respiratory system, gastrointestinal tract or urination.
The most common syndromes that occur with VSD are combined into the following list:
- Cardiovascular, associated with rhythm disturbances, fluctuations in blood pressure, pain in the cardiac region of different localization without physical activity;
- Endocrine, which is manifested by increased sweating of the feet and palms - hyperhidrosis;
- Respiratory with increased respiratory rate, difficulty breathing, dizziness, muscle spasms;
- “Irritable bowel”, which combines a variety of gastrointestinal disorders - nausea, loss of appetite, restless sensations;
- Urinary, manifested by frequent and painful diuresis;
- Sexual disorders with erectile dysfunction and decreased libido, female anorgasmia and lack of male ejaculation;
- Intoxication with attacks of chills and a slight but steady increase in body temperature.
Types of retinal angiopathy
There is no uniform classification of angiopathy.
Scientists have put forward many hypotheses regarding the division of this pathological process into forms. The most popular is the clinical classification, which divides angiopathy into types depending on the cause that caused it: Among the varieties of the disease, the following are distinguished:
Its treatment directly depends on what type of vascular damage occurs. In this regard, it is customary to highlight:
- Microangiopathy of the lower extremities is a lesion of small vascular formations that are part of the microvasculature (arterioles, capillaries, venules, arteriovenular anastomoses). It is predominant in the structure of all causal mechanisms for the development of angiopathy of this localization. Very often combined with other vascular lesions: retinopathy (retinal dysfunction), nephropathy (renal blood flow disorders).
- Macroangiopathy is a structural and functional transformation of arterial structures of medium and large caliber, which is characteristic only of lesions of the vessels of the lower extremities.