Cerebellar agenesis is an extremely rare condition. The term “cerebellar agenesis” describes the complete absence of this part of the brain, regardless of the underlying cause (etiology). As a rule, most patients have small remnants of the cerebellum, which is why the term “subtotal cerebellar agenesis” can be found in the literature. It is now known that cerebellar agenesis can be either congenital (a primary disorder of embryonic development) or secondary (due to the destruction of normally developed tissue).
Brain hypoplasia - causes
Brain hypoplasia is a congenital pathology. Genetic disorders, as well as the influence of various harmful factors on the body of a pregnant woman, can lead to its occurrence, for example:
- smoking;
- consumption of alcoholic beverages, drugs or toxic substances;
- ionizing radiation;
- some diseases (rubella, influenza, toxoplasmosis).
The impact of these factors is especially dangerous in the early stages of pregnancy, when the baby is actively forming and developing various organs, including the brain.
Brain hypoplasia - symptoms
With microcephaly, there is a sharp decrease in brain mass. In addition, other gross disturbances occur in it - the structure of the convolutions and internal structures changes. As a rule, the temporal and frontal lobes are more underdeveloped. The convolutions become flat - only large grooves remain, and small ones almost completely disappear. The pyramids of the medulla oblongata, cerebellum, brain stem and thalamus often decrease in size. With cerebral hypoplasia, the skull circumference is reduced. As a child grows, the bones of the facial skeleton grow faster than the brain. Almost all patients have signs of intellectual impairment. In addition, there is also a delay in physical development - children with microcephaly begin to hold their heads, sit and walk very late.
X-linked cerebellar hypoplasia
Visible signs usually include:
- Macrocephaly
is a proportional enlargement of the brain accompanied by deterioration of mental abilities. Symptoms may not be noticeable to a person. - A dysplastic face
is an abnormality in the size of certain organs or the contours of the entire face. - Congenital hypogenitalism
is defective development of the gonads. - High growth.
- Diffuse muscle hypotonia
is a decrease in muscle tone, often combined with paresis (weakening of voluntary movements). It usually appears due to damage to the cerebellar vermis. - The development of psychomotor functions is inhibited.
- Strabismus
- strabismus.
After several years, the following may be added:
- Myoclinic epilepsy -
bilateral seizures that begin some time after waking up. The disease debuts in adolescence. - Mental retardation.
- Ataxic syndrome
- loss of balance, dizziness. With generalized cerebellar hypoplasia, the degree of its severity is variable and may change over time.
Neuroimaging reveals:
- Expansion of extracerebral spaces
- cavities located outside the brain. - Ventriculomegaly
is an enlargement of the ventricles of the brain. - Atrophy of the caudate nucleus
, an integral part of the striatum (striatum), which regulates muscle tone, motor reactions and conditioned reflexes.
When cerebellar hypoplasia is detected, it is necessary to clarify the diagnosis (form of pathology).
The degree of organ underdevelopment affects the list of therapeutic measures and the prognosis of the disease. Microcephaly or brain hypoplasia is a decrease in brain size associated with underdevelopment of brain tissue. Very often, this pathology occurs against the background of some other defects in the development of the limbs, spinal cord, heart and a number of other internal organs.
Brain hypoplasia - treatment
Unfortunately, to date this disease has no cure. Therapy for microcephaly is symptomatic - it is aimed at “smoothing”, reducing the manifestations of some neurological symptoms. Life expectancy in patients with cerebral hypoplasia is reduced. And, unfortunately, there is practically no hope that the child’s brain will develop normally. Only a small proportion of children with microcephaly are able to study in auxiliary schools. The rest need constant care and supervision.
Cerebellar hypoplasia
Hypoplasia does not always affect the entire brain. In some cases, only some of its parts, such as the cerebellum, are affected. Cerebellar hypoplasia is a congenital malformation in which some functional areas of the cerebellum and/or its cortex are underdeveloped. Like any other type of hypoplasia, cerebellar hypoplasia occurs during fetal development. In more than half of all cases, the development of the disease is caused by genetic abnormalities. In other cases, the reason lies in the impact of certain negative factors on the body of a pregnant woman.
Consequences
Many doctors consider abnormal variations in the structure of the circulatory system of the brain as predictors of epileptiform disorders. Consequences of a severe disease:
- Aneurysm formation.
- Rupture of the vascular wall with subsequent formation of a hemorrhage focus.
- Deterioration in cognitive abilities, general health and well-being.
- Stroke.
The development of a stroke is associated with deterioration of blood supply to a region of the brain or intracranial hemorrhage. After a stroke, only 20% of patients regain the ability to self-care. In other cases, the patient faces disability with a stable, pronounced neurological deficit. The mortality rate is 35-40%.
Cerebellar hypoplasia - symptoms and treatment
Symptoms of cerebellar hypoplasia are:
- Delayed physical and mental development. Children start sitting and walking late. Their speech development is delayed;
- Tremor (shaking) of the head and limbs, which often appears in the first year of life;
- Difficulty maintaining balance;
- Clumsy gait. Often, children with cerebellar hypoplasia can only move with assistance.
With age, the symptoms of the disease stabilize. And usually after 10 years of age, no further growth is observed. In some patients, cerebellar hypoplasia leads to the development of mental deficiency, accompanied by deafness and/or blindness. Unfortunately, medicine is currently unable to cure children with this disease. However, long-term social and motor rehabilitation - for example, classes with a speech therapist, occupational therapy, balance therapy, massage, physical therapy - can improve the condition of patients and instill in them self-care skills.
Even if a child has been given such a terrible diagnosis, there is no point in giving up. Such a baby, much more than other children, needs affection, attention and care - and mother’s love sometimes works wonders!
Causes of Dandy-Walker syndrome
Unfortunately, even modern medicine cannot yet answer with confidence the question of what reasons lead to the development of Dandy-Walker syndrome. Of course, there are some risk factors that in one case or another can lead to intrauterine defects. For the formation of this anomaly, an important role is played by:
- Viral diseases that the mother suffers during pregnancy (you should especially beware of infections in the first three months).
- Cytomegalovirus infection.
- Rubella.
- Diabetes mellitus or other diseases associated with metabolic disorders in the expectant mother.
Quite often, various pathologies of the fetus during intrauterine development appear in women who suffer from alcoholism or drug addiction. In most cases, it is these mothers who give birth to children with Dandy-Walker syndrome. If during an ultrasound the doctor sees that the fetus is developing abnormally, he recommends terminating the pregnancy. In very rare cases, Dandy-Walker syndrome develops for hereditary reasons.
[5], [6], [7], [8], [9]
Girls! Let's repost.
Thanks to this, experts come to us and give answers to our questions! Also, you can ask your question below. People like you or experts will give the answer. Thank you;-) Healthy babies to all! Ps. This applies to boys too! There are just more girls here ;-)
Did you like the material? Support - repost! We try our best for you ;-)
Vermis hypoplasia is a defect in the intrauterine development of the cerebellum, leading to a partial impairment of motor function; symptoms appear in the first days of the baby’s life.
The cerebellum (in Latin – “Cerrebelum”, which literally translates as “small brain”) is a part of the brain.
Located in the back of the brain, it is responsible for coordinating human muscle movements, maintaining balance in space and muscle tension, or tone, and also controls internal organs.
The small brain itself belongs to the autonomic central nervous system - the work of the cerebellum occurs unconsciously. The following definition applies to the cerebellar vermis - it is its middle part. It communicates between opposite lobules. The worm is responsible for a person’s ability to maintain a posture.
Hypoplasia of the cerebellar vermis leads to loss of the ability to stand and walk normally.
Hypoplasia of the cerebellar vermis in the fetus is manifested as a consequence of the influence of both hereditary factors of the parents and harmful factors on the fetus during the prenatal period. Hypoplasia develops more often if the following factors are present:
- Consumption of alcohol, toxic or narcotic substances;
- Radiation exposure;
- Diseases suffered by the mother during the first months of development.
The danger in smoking is not so much nicotine, but rather toxic substances that affect the process of laying down the neural tube - the embryo of the spinal cord and brain, as well as oxygen starvation - the abundant intake of carbon dioxide into the mother's blood.
Alcoholic beverages contain ethanol, which easily penetrates the placenta and concentrates in the fetus in the central nervous system. Ethanol decomposes to acetaldehyde, which is a mutagen and carcinogen, influencing genetic mutations and tumor formation. Acetaldehyde easily damages the blood-brain barrier, which protects the central nervous system from harmful substances and its own immune system.
Toxic substances can be classified as those that enter the body through the consumption of unhealthy foods or those that contain components of medications that are harmful to the baby. For the safety of the child, before consuming this or that product, you must make sure of the composition and harmfulness of its components to the fetus, and secondly, under no circumstances take medications on your own without a doctor’s prescription.
Radiation received by a mother during pregnancy is a serious threat to the unborn child, as it affects the DNA structure.
Radioactive isotopes, entering the body, are concentrated in the placenta and amniotic fluid, destroying the immune system, reproductive function of the fetus and its hormonal secretion glands. The type of isotope and the intensity of its radiation have a strong influence.
The health of the fetus will be affected by both radiation and radioactive isotopes that were exposed to or entered the woman’s body before pregnancy, since radiation tends to accumulate in tissues. Radiation can lead to various pathologies in the thyroid gland, which will affect future pregnancies.
A striking example of a disease is called rubelliosis, which is caused by the corresponding virus. A relatively harmless childhood disease can cause irreparable harm to the fetus in the first trimester of pregnancy. Hypoplasia in this case will be acute, spreading to both lobules. Flu is also a threat.
Symptoms
Since hypoplasia of the cerebellar vermis is a disease affecting the motor nuclei, the following manifestations are observed:
- Delay in the development of motor functions. Children with disabilities will be able to learn to sit and walk independently later than healthy ones. In such children it will be observed;
- Lack of coordination in the movement of the muscles of the trunk and limbs;
- Loss of smoothness in limb movements;
- “Chanted” speech, which differs from the usual one in its placement of stress in words according to the rhythm, and not according to the meaning of the sentence;
- Trembling in the limbs and head, which may appear in the first months of life;
- Problems maintaining balance both while standing and sitting;
- Problems with gait. Often hypoplasia leads to the need for support when moving;
- Disturbance in the smooth muscles of internal organs;
- Congenital blindness or;
- Depression of the child's respiratory function.
The most common illness in a child is ataxia, a disorder of gait and orientation in space. There will be a noticeable “drunkenness” and swaying in the gait.
Problems with the development of rotator muscles will manifest themselves when the eye is moved to extreme positions in the form of rhythmic twitching - nystagmus. Problems with mismatched movement of the muscles of the trunk and limbs are expressed in difficulties when trying to stand up or take a sitting position.
Symptoms develop according to underdeveloped centers. The spherical and corky bodies, which are responsible for muscle movement, being underdeveloped, will lead to loss of control of the trunk muscles. Hypoplasia of the dentate body or vermis leads to dysfunction of the limbs.
Symptoms, in addition to the immediately present ones - deafness and limbs, increase as the child grows older.
The increase stops by the age of 10, when the development of the worm decreases and the symptoms stabilize, allowing continuous maintenance therapy to be prescribed.
- Interesting read:
Symptoms
Cerebellar hypoplasia is symptomatically associated with neurological signs. Underdevelopment or reduction in size of its individual sections or the cerebellum as a whole negatively affects the entire brain and the central nervous system. This pathology manifests itself in the following:
- Inhibition in the development of motor type functions. Sick children are delayed in their development, they later learn to sit and move, and suffer from speech problems.
- Minimum level of coordination in the movement of the muscles of the trunk and limbs.
- Children's arms and legs cannot move smoothly.
- Speech takes on the character of “chanting.” Sick children place stress in accordance with the rhythm, without connection with the meaning of the sentences and phrases being formed.
- Limbs and head are shaking. Tremor can manifest itself from an early age with cerebellar hypoplasia - almost from the first days of life.
- Difficulty maintaining balance in any position - both sitting and standing.
- Difficulty in moving independently, which requires constant support from an accompanying person.
- Malfunctions in the functioning of the smooth muscles of internal organs.
- Problems with hearing and vision, including deafness and blindness. This situation may be congenital, but can develop as one grows older.
- Malfunctions of the respiratory and cardiac organs.
- Increased aggressiveness and hysteria.
- Difficulties in social adaptation.
Signs appear from birth and become most clearly noticeable before the age of ten. Although the pathology after this age limit does not progress very quickly, problems with the functioning of internal organs and systems can have a negative impact on the baby’s growth.
Sometimes it is possible to detect cerebellar hypoplasia in adulthood. This is evidence of the insignificance of damage to the cerebellum. With a mild form of the disease, its signs are often not noticeable in childhood; there is only a slight impairment of fine motor skills and coordination.
Treatment
Despite medical advances over the past few decades, worm hypoplasia is incurable.
Very often, hypoplasia in a child leads to death in the first months of life. All therapeutic actions carried out are aimed at containing the disease, as well as developing lost functions. Therapy may include:
- Physical therapy that helps develop coordination;
- Massage courses;
- Classes with a speech therapist;
- Balance therapy aimed at restoring balance and coordination;
- Occupational therapy, instilling in children communication and work skills.
This allows not only to improve the general condition, but also to carry out important measures for social adaptation and acquiring self-care skills. If a person does not possess these skills, then this will not allow him to become independent and will need support and constant care all his life.
When the disease affects young patients, it is scary, and diseases that develop during pregnancy, which include cerebellar vermis hypoplasia, are doubly scary. Therefore, expectant mothers need to seriously think about their lifestyle during pregnancy, but first things first...
So, hypoplasia of the cerebellar vermis in the fetus, or simply microcephaly, is characterized by a decrease in the size of the cerebellum itself, or one of its lobes, which ultimately entails irreversible consequences for the body and its full development.
The dash indicates the cerebellum with hypoplasia
At risk are girls who, during pregnancy:
- drink alcohol;
- smoke;
- take drugs;
- exposed to radioactive radiation;
- suffered an infectious disease (rubella, toxoplasmosis, etc.).
In addition to the above, you can add expectant mothers who eat food that is harmful to the health of the fetus during pregnancy, but, as a rule, junk food does not have such an effect compared to alcohol, but in the aggregate it can lead to various anomalies.
Alcohol
Abuse of alcoholic beverages affects the fetus through ethanol. This substance independently penetrates into the central nervous system of the fetus (CNS), where, as a result of prolonged exposure, it can influence the formation of tumors and also affect the blood-brain barrier, making it weaker and thereby exposing the child’s body to even greater risk.
The blood-brain barrier is a kind of wall that protects the central nervous system from harmful infections that can affect it through the blood.
Smoking
In the process of smoking, the greatest danger for the formation of such an ailment as fetal hypoplasia is caused by toxic substances, and not nicotine. These substances affect the very process of formation of the spinal cord and brain, in particular, the formation of the neural tube. For this reason, cerebellar hypoplasia in a newborn may not be the only anomaly.
Addiction
Many films have already been made about the dangers of drug addiction and even more books have been written, so we can confidently say that cerebellar hypoplasia in children can develop as a result of drug use, as well as in the case of uncontrolled use of medications. It is no coincidence that some tablets contain a note stating that their use is possible only in extreme cases, if the positive effect for the mother is greater than the potential harm for the baby.
Radioactive substances
Radiation is dangerous for an adult, but what about an immature baby. Hypoplasia of the cerebellar vermis in the fetus can develop due to excessive exposure of the pregnant mother to radiation or excessive time spent in places with an increased radioactive background. The radioactive isotopes themselves accumulate in the amniotic fluid and placenta, and can change the structure of DNA, and it is easy to guess that with excessive irradiation of the body, fetal hypoplasia can be the mildest diagnosis of all possible consequences.
Infectious diseases
Cerebellar hypoplasia in a newborn can develop as a result of such a harmless disease as rubella. However, it is harmless only in childhood, and during pregnancy it is the number one enemy for a young mother. If this disease is diagnosed in the first trimester, doctors in 90% of cases send the girl for an artificial termination of pregnancy; in the second and third trimester, drug treatment is used, but it is usually ineffective.
Toxoplasmosis, in turn, is no less dangerous, but it causes missed abortion. It is transmitted from cats, rodents, birds, however, if the pathogen has not passed through the cat’s body, it does not pose a danger to humans. Dangerous processes are launched in the cat’s body and an ordinary virus turns into a serious disease.
Diagnostics
Usually the disease is detected during pregnancy through ultrasound diagnostics. Subsequent monitoring of the child is carried out by a neurologist. He may prescribe treatment or rehabilitation procedures.
Unfortunately, cerebellar hypoplasia is considered an incurable disease, and children who are born with it rarely survive beyond the age of one year. All procedures that are carried out with such a child are aimed at restoring lost functions and curbing the development of the disease. Treatment methods include:
- exercises aimed at developing coordination; massage; to maintain speech, classes are held with a speech therapist; It is also recommended to communicate with such children as often as possible and instill in them various hobbies, such as drawing or origami, which develop fine motor skills of the fingers.
https://www.youtube.com/watch?v=ytdevru
For example, if a person is running and sees an obstacle ahead, he will definitely jump over it or at least try to do so.
Despite the fact that many muscles are involved in a jump, they all work at lightning speed, as a single whole.
The cerebellar vermis is a body in the middle of the cerebellum that controls balance, maintaining a certain posture, and gait. Very often people say that someone’s gait is one way, and someone else’s is completely different. Indeed, the regulatory function of the cerebellar vermis shows itself exclusively individually.
Pathologies of the cerebellar vermis contribute to the loss of this function; walking turns into chaotic scattered asymmetrical movements.
This pathology can be cerebellar hypoplasia. Cerebellar hypoplasia usually manifests itself in the womb and often occurs along with other bodily disorders, in particular, interruptions in heartbeat, breathing, digestion, disruptions in the endocrine system, etc.
Cerebellar hypoplasia in the fetus is the underdevelopment of this part of the brain and, as a consequence, a decrease in the cerebellum and the brain as a whole in weight and volume.
Therefore, relatives and friends must spend all their time with the patient.
Adaptation in society is also difficult for a child, since he even looks different from healthy children.
Moreover, the disease usually progresses, in particular, even more mental deficiency develops, and vision and hearing deteriorate over time. However, you should never leave your child in trouble! Despite his mental retardation, he feels everything, and his consciousness perceives everything.
There have been cases in the world when children with this pathology reached adulthood, although doctors called it a local miracle.
Cerebellar hypoplasia still needs to be distinguished from complete cerebral hypoplasia, which is symptomatically and clinically even more serious and dangerous. Hypoplasia is caused by a breakdown in genes or hereditary transmission, mainly from parents.
Also in medicine, pituitary hypoplasia, or empty sella syndrome, is also distinguished, which is symptomatically similar to other brain pathologies.
The development of cerebellar vermis hypoplasia is diagnosed during such stages. First, the doctor collects and analyzes the complaints of the baby or his parents and evaluates the symptoms. As a result, a symptomatic and clinical description is formed, which becomes the basis for suspicion in formulating the diagnosis of “Cerebellar Hypoplasia”.
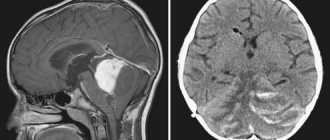
Instrumental diagnostics using MRI and CT scans of the brain, ultrasound or electroencephalography.
Diagnosis of cerebellar hypoplasia consists of two stages. At the first stage, the doctor interviews the child’s parents about complaints and symptoms. Thus, it provides a preliminary symptomatic and clinical picture, which can serve as the basis for suspicion of cerebellar hypoplasia.
The doctor also asks you to practice with the child, asking him easy tasks to maintain balance and correct coordination of movements. You may also need the help of an ophthalmologist, psychologist, etc.
https://www.youtube.com/watch?v=upload
The child can be given logical and thinking exercises, during which the presence of mental and intellectual retardation is revealed. With damage and reduction of the cerebellum, this is also of great importance.
Finally, doctors also resort to technological procedures, for example, magnetic resonance or computed tomography of the brain, ultrasound or electroencephalography of the brain. All of them can play a decisive role in correctly constructing a diagnosis and prescribing effective and correct treatment, which is why the importance of diagnosis is very great.
Symptoms
Such a serious anomaly as hypoplasia of the cerebellar vermis in the fetus has special symptoms, since the cerebellum in the brain is one of the most important organs, responsible for many functions.
Main signs of the disease:
- tremor of the limbs;
- declarative speech (the child speaks as if shouting slogans);
- lack of smooth movement;
- inconsistency of limbs when moving;
- developmental problems (such children may begin to sit and walk later than their peers);
- inability to move without adult support;
- deafness or blindness.
Since the cerebellum has a rather complex structure, damage to its individual parts can lead to certain consequences, for example, hypoplasia of the medial parts of the cerebellar hemispheres entails disorders associated with the organs of vision (the child may remember visual information worse).
In addition to disorders associated with motor and physical changes, parents may notice that with hypoplasia of the cerebellar vermis, the baby’s head is smaller than that of his peers. This occurs as a result of a smaller brain volume, and since the brain is smaller, the formation of a bone plate around it does not occur as usual. Over time, the skull will enlarge and various cranial deformities may develop.
Features of treatment
Cerebellar hypoplasia in infants is a serious disease and there are cases of death at an early age, however, this is not a dogma and people live with this disease.
Undoubtedly, such children need the care and support of adults more than usual, since some functions are inaccessible to them or are difficult to perform.
Unfortunately, an effective treatment for a disease such as fetal hypoplasia has not been found to date, so it is of a therapeutic nature.
Therapy for hypoplasia in a child:
- occupational therapy (instilling work skills in the child);
- speech therapy classes;
- massage courses;
- social development;
- physiotherapy;
- therapy aimed at restoring the child’s balance.
The treatment options listed above will help the baby live painlessly in society in the future.
Among other things, there are cases of cerebellar hypoplasia in adults. This happens, as a rule, if the affected area was insignificant and did not entail any special changes in a person’s life.
Treatment in adulthood, in the absence of other pathologies, may differ slightly, but the treatment program listed above remains unchanged.
Prevention
The main preventive measures to help prevent the development of cerebellar hypoplasia during pregnancy are maintaining a healthy lifestyle and being attentive to your health.
Undoubtedly, it is not worth taking things to the point of absurdity, but it is important to remember that balance is necessary in everything. Even half a glass of good red wine once a month will not only not harm the child’s body, but will even have a beneficial effect.
But half a cigarette smoked once a month will already have a negative effect on the fetus, so you need to approach everything headlong and with caution.
Take care of your health and the health of your little ones.
Major defects of cerebellar development that damage predominantly the hemispheres (Robain et al. 1987) or almost equally the hemispheres and vermis constitute a heterogeneous group of rare abnormalities with varying pathology and clinical manifestations (Sarnat and Alcala, 1980; Robain et al., 1987; Altman et al., 1992). Cases of probable atrophy and congenital pontocerebellar atrophy are discussed in a separate article on the website.
Diagnosis is controversial, as many apparent malformations are actually acquired diseases resulting from destructive or metabolic processes (Sener, 1995; Boltshauser, 2004). Correct classification of cerebellar developmental defects is difficult. Friede (1989) argues that the classic division of neocerebellar versus paleocerebellar hypoplasia is artificial and in many cases it is more appropriate to speak of aplasia of the anterior or posterior lobe of the cerebellum.
Total cerebellar aplasia is an exception (Glickstein, 2004). The interesting thing is that it does not always manifest itself with clinical symptoms. In reality, cerebellar remnants are probably always present (Gardner, 2001) and the term “hypoplasia” or “atrophy” is more accurate than “agenesis.” Cerebellar agenesis has been reported in association with diabetes insipidus (Zafeiriou et al., 2004). Hypoplasia is less common and may be predominantly unilateral.
In some cases, it is limited to specific structures, such as the lobule of the hemisphere. Often accompanied by anomalies of the deep cerebellar and brain stem nuclei and dysplasia of the inferior olive. In some cases, there is hydrocephalus (Friede, 1989), and other pathological changes are possible, for example, agenesis of the corpus callosum or arenencephaly.
Unilateral aplasia (Boltshauser et al., 1996; Kilickesmez et al., 2004) is less common and is often asymptomatic. May be accompanied by an ipsilateral facial angioma and various cerebral and/or peripheral vascular abnormalities in PHACES syndrome (Pascual-Castroviejo et al. 2003, Bhattacharya et al. 2004).
Clinical manifestations are extremely unstable.
They may be completely absent or manifest as ataxia, imbalance and other cerebellar symptoms. Characterized by mental retardation to varying degrees. Some cases are represented by ataxic cerebral palsy. In most cases, movement disorders predominated, but some patients showed signs of autism or microcephaly. Cerebellar atrophy of unknown origin in an 8-year-old girl, predominantly affecting the vermis.
The lower part of the worm may be completely missing. The diagnosis of cerebellar hypoplasia is usually based on radiological methods. Diffuse hypoplasia can be difficult to distinguish from the Dundee-Walker variant on CT, and megacistern is often mistaken for cerebellar hypoplasia. Differential diagnosis includes visualization of the cerebellar falx, which characterizes the cisternae pattern, and the complete presence of the cerebellar vermis on sagittal MRI images.
Some cases of cerebellar hypoplasia are part of genetic syndromes, but complete definition is still a long way off. Some features are due to congenital ataxia with different types of transmission, while additional features are present in other cases (Al Shahwan et al., 1995). An association with chromosomal aberration has been reported (de Azevedo-Moreira et al., 2005, Harper et al., 2007).
Other unusual cerebellar malformations:
1. Tectocerebellar dysraphism
(Mori et al., 1994, Dehdashti et al., 2004) is a complex developmental anomaly that includes an inverted cerebellum developing within the fourth ventricle, vermis hypoplasia, and an occipital cephalocele.
2. Rhombencephalosynapsis
(Toelle et al., 2002) refers to congenital fusion of the cerebellar hemispheres with midline fusion of the dentate nuclei and aqueductal atresia. Patients with mild symptoms live long.
Complex cerebellar malformations due to cephalocele may result from ischemic destruction of a previously normally formed cerebellum due to arterial compression by a diverticulum of the fourth ventricle.
3. Dentato-olivar dysplasia
is responsible for neonatal tonic seizures resembling Ohtahara syndrome found in several patients (Harding and Boyd, 1991, Robain and Dulac, 1992). A genetic origin of the pathology is suggested (Harding and Sorr, 1997).
Asked by: Ilya
Gender: Male
Age: 40
Chronic diseases: not specified
Hello. She suffered a traumatic brain injury as a child (10 years old). After it, attacks began similar to dizziness, not frequent. After the examination, no deviations were identified. Attacks similar to dizziness have been ongoing for 30 years, during which time studies were carried out and the diagnosis was made: MRI 2013: Hypoplasia of the cerebellar vermis with compensatory expansion of the retrocebellar space. MRI 2014 of the cervical spine: Intervertebral osteochondrosis of the cervical spine. Retrocebellar cerebrospinal fluid cyst. Rheoencephalography 2003: Pulse blood filling of cerebral vessels is within normal limits. The tone of large-diameter arteries is moderately increased and labile. Peripheral resistance at the level of arterioles is increased. Venous outflow from the cranial cavity is within normal limits. . ENT-healthy. Ultrasound of the arteries is normal. I was in the hospital diagnosed in 2013: Hypoplasia of the cerebellar vermis with vestibulocoordination disorders, asthenovegetative syndrome, decompensation. Extract from 2020: Hypoplasia of the cerebellar vermis with mild coordination disorders. During attacks, blood pressure rises, heart rate increases, everything “floats” and spins before your eyes; there is a feeling of instability. The quality of life is reduced due to attacks that occur 5-6 times a day (previously it was much less common). There are no symptoms without seizures, my balance is normal, my head is normal, my hands don’t shake, I feel like an ordinary person. Tell me how it can be cured or whether it is already incurable. The doctors don’t say anything and prescribe me only for dizziness, but the medications don’t help at all (betagistine, glycine).
Dizziness, nausea, pale skin, incoordination, numb part of the back of the head. Severe dizziness, arms and legs either don’t move or become numb, pale skin everywhere, numb part of the back of the head, sometimes there is confusion, nausea, weakness, with such attacks there is severe irritability and anger, sometimes you walk and don’t understand anything what’s happening, like a zombie, the condition is very scary, it’s like you’re going to die, they once diagnosed spondyloarthrosis of the cervical spine, and now the spine also hurts in the lumbar region, I can’t lie on my stomach for a long time, my spine hurts, and when It hurts when pressed, what could it be? Is this related to spondyloarthrosis, or something else? Maybe the brain damage has already started? I can’t get to the doctor, the appointment is long, so I turned to you, please help me with advice!
Partial agenesis of the cerebellar vermis in the fetus, what is it?
Sonographic diagnosis of Classic Dandy-Walker syndrome is quite simple starting from the second trimester of pregnancy, and the earliest diagnosis using transvaginal echography described in the literature dates back to 14 weeks. Ultrasound examination in a sectional plane of the head passing through the cerebellum will reveal that the enlarged cisterna magna is connected to the fourth ventricle through a defect of the cerebellar vermis.
In addition, borderline or overt ventriculomegaly is often detected, as well as combined anomalies of the central nervous system and other organs and systems.
However, in cases of partial agenesis of the cerebellar vermis, limited to its lower parts, the traditionally used section through the cerebellum may not reveal changes, and the most careful examination will be required to diagnose the defect. In order to exclude the presence of this condition, it is necessary to ensure by scanning the lower parts of the cerebellum that the lower part of its vermis separates the fourth ventricle from the cisterna magna.
The criteria differentiating the condition of megacistern magna and the Dandy-Walker variant in the fetus have not yet been precisely defined. The first of them can be suspected if the diameter of the cisterna magna exceeds 10 mm, and the second, when a thin connection can be detected between the fourth ventricle and the cisterna magna. When establishing these diagnoses, the researcher requires attention and caution.
At the beginning of the second trimester of pregnancy, an echographic image of a normally developed cerebellum may give the impression of the presence of pathology, since the relatively large fourth ventricle and the incompletely formed lower parts of the cerebellar vermis may create the erroneous impression of its defect at this gestational age. Thus, diagnosing this defect at this stage of pregnancy is imprudent.
In such cases, a repeat examination is recommended at 18 weeks or later, in the second or even third trimester. It is important to note that scanning at an angle that is too acute can also give the impression of a significantly enlarged cisterna magna and even a defect in the cerebellar vermis. The cause of this artifact remains unclear. It is believed that it may be due to the presence of fluid in the cerebellar recess, which tends to widen slightly anteriorly and has a very thin covering membrane.
Connection Images of the superior cerebellar recess and adjacent tonsils give the impression of a connection between the fourth ventricle and the cisterna magna, similar to that described by CT scans of the Dandy-Walker variant.
Assessing the anatomy of the posterior fossa using the median longitudinal plane may be useful in such cases because it allows visualization of the vermis in the sagittal plane. However, it seems unlikely that even this approach will accurately identify subtle cerebellar dysgenesis as accurately as described in postnatal MRI studies. According to our data, the vast majority of fetuses that had isolated enlargement of the cisterna magna or an echographic picture suspicious for a small defect of the cerebellar vermis were absolutely healthy at birth, which was confirmed by neurosonography and clinical assessment.