What is malformation?
Disturbances in the connections of veins, lymph nodes and arteries form during embryonic development. Excessive vascular connections occur in venous, arterial or lymphatic structures, capillaries change shape, which leads to redistribution of blood and the development of secondary disorders that are associated with a lack of nutrients and oxygen.
The severity of symptoms depends on the characteristics of the pathology, the location of the affected areas and the size of the central vessels.
Due to structural disturbances, the vascular walls become thicker and the veins increase in volume. The walls of coiled vessels are fragile and vulnerable, which increases the risk of spontaneous hemorrhage.
Arteriovenous malformations are among the most common types, are more severe and affect mainly men, but pathologies of the brain and spinal vessels are more often diagnosed in women.
The disease may not manifest itself for a long time . The first symptoms appear at 20-40 years of age or in childhood.
The older the patient, the higher the likelihood of a positive outcome: if a vascular malformation was detected after the age of forty, there is a high probability of curing it completely, and malformations in children are severe.
The most dangerous malformations are those that affect vascular structures:
- Brain;
- Intestines;
- Spinal cord.
Pathology can be localized in any part of the body. The incidence of damage to the upper or lower limb is 5-20%. The vessels of the neck and head are affected with a frequency of 5-14% of all malformations.
Malformation
Clinic of arteriovenous malformations of the brain [edit | edit code]
- The hemorrhagic type of the disease occurs in 50 - 70% of cases. This type of course is characterized by the presence of arterial hypertension in the patient, a small size of the malformation node, its drainage into the deep veins, as well as an AVM of the posterior cranial fossa.
- The torpid type of flow is typical for patients with a large AVM, its localization in the cortex, blood supply from the branches of the middle cerebral artery.
In 50% of cases, it is the first symptom of AVM, which causes death in 10–15% (with aneurysms up to 50%) and disability in 20–30% of patients [2].
The annual risk of hemorrhage from an AVM is 1.5 - 3%. During the first year after hemorrhage, the risk of recurrence is 6% and increases with age [3].
Development mechanism and reasons
The pathology is formed during the period of intrauterine development, when vascular structures are formed. This occurs in the first trimester or at the beginning of the second under the influence of negative factors.
| Genetic factors | This malformation occurs due to disorders in genes, can be inherited and accompany genetic diseases (Osler disease, Merritt syndrome). |
| Excessive exposure to radiation | Radiation causes changes in genes and general developmental disorders, and this is possible even before pregnancy: when an egg is irradiated, the DNA structure can be disrupted, which will affect the offspring. Minor ion exposure is not harmful, but receiving excessive doses (in accidents, after man-made disasters, long-term radiation therapy) will most likely lead to the development of various pathologies, one of which includes arterial and venous malformations. |
| Infectious lesion | Infections, especially those that are severe, can cause disruption of fetal development. These include measles, influenza, rubella, hepatitis, and chicken pox. |
| Diseases of a pregnant woman | Chronic diseases in women, such as diabetes, HIV infection, hepatitis C, bronchial asthma, negatively affect the development of the fetus. |
| Intoxication | There is an extensive list of toxic substances (mercury, benzene, lead, drug overdose, gasoline), exposure to which leads to the development of various vascular defects. |
| Use of drugs during pregnancy that negatively affect the fetus | These include some antibiotics, tranquilizers, vitamin A and D in excess doses. |
| Bad habits | Smoking, drugs and alcohol significantly increase the risk of developing various vascular defects, including malformation. |
| Unfavorable environment | Children who were born in environmentally unfavorable areas have a significantly increased likelihood of developing various pathologies. |
The risk of developing a malformation increases when the fetus is injured in the first trimester of pregnancy.
Site of malformation
Causes
The genetic predisposition to AVM and the facts of its inheritance are unknown. It is believed that AVM is not a hereditary disease. In arteriovenous malformations, most often, there is no capillary network, resulting in direct shunting of blood from the arterial basin to the system of superficial and deep veins. The main mechanisms of the pathological effect of arteriovenous malformation on the brain: - Rupture of pathologically altered vessels of the tangle or aneurysms of the arteries feeding the AVM. - Chronic circulatory failure caused by arteriovenous shunting. - Normal perfusion pressure breakthrough syndrome.
Classification
The Schobinger classification is used to assess the severity of pathology and select the optimal treatment tactics.
| Stage | Clinical picture |
| 1. Peace | The skin over the affected area is reddish in color and hot to the touch. Ultrasound reveals the presence of blood discharge from the artery into the venous flow. An AVM in appearance resembles a benign vascular neoplasm. |
| 2. Rapid growth | All the signs of the first stage are preserved. There is an expansion of arteries and veins in diameter, the arteries are actively pulsating. |
| 3. Destruction | All symptoms of the second stage remain. Symptoms of tissue nutritional disorders, ulceration, and bleeding are also observed. |
| 4. Decompensation | All symptoms of the third stage persist, cardiovascular failure develops, the left ventricle is enlarged. |
Pathology at birth may look like a birthmark, in some cases it may not be recognized in a timely manner, so it is important to know what vascular malformations are, why they are dangerous and what diagnostics are necessary.
According to the type of vascular pathology, according to the Hamburg classification, all malformations are divided into:
- Arterial;
- Venous;
- Lymphatic;
- Capillary;
- Shunt arteriovenous;
- Combined.
When assessing the risks of surgical removal, the Spetzler-Martin classification is used, in which each characteristic of the pathology is assigned a certain number of points.
| Diameter | Less than 3 centimeters - 1 point. |
| From 3 to 6 centimeters - 2 points. | |
| Over 6 centimeters - 3 points. | |
| Accommodation | Within the boundaries of vital areas (certain centers of the brain and spinal cord) - 1 point. |
| Outside the boundaries of vital areas - 0 points. | |
| Venous drainage | In veins that are located deep - 1 point. |
| In the area of superficial veins - 0 points. |
The sum of points indicates the level of risk during surgery. With a score of 5 points, the malformation is considered inoperable.
The pathology can be localized anywhere in the body, but the most common forms are:
- Malformation of cerebral vessels;
- Facial malformation;
- Malformation of internal organs (intestines, lungs, kidneys and other organs);
- Spinal malformation;
- Limb malformation.
Types of arteriovenous malformations
Symptoms
The symptoms of malformations are varied and depend on the location, features, size and other characteristics.
The following symptoms are observed:
- With a spinal injury , acute pain occurs in the spinal area, nausea, muscle weakness, severe fatigue, and pain in the head are observed.
- Pulmonary damage is characterized by the development of heart failure due to lack of oxygen, breathing is impaired and rapid. Chest pain and coughing up blood also occur.
- Arterial-venous malformation of the extremities. Pigmented areas of brown or pink color are noticeable on the skin, and dilation of the veins on the outside is observed (especially when the leg is affected). The limb grows rapidly, and during physical activity pain, burning and a feeling of heaviness occur.
- Liver damage. Soreness and feeling of heaviness in the right hypochondrium, nausea and vomiting, organ growth.
- Skin disorders. Discoloration, ulcers, thickening. The size and shape of the spot may vary.
Arteriovenous malformation of cerebral vessels is accompanied not only by general symptoms, but also by focal ones, which depend on the location of the vascular malformation.
Common symptoms include:
- Headache,
- Increased intracranial pressure,
- Dizziness;
- Weakness.
Symptoms depending on the location of the pathology:
- Cerebellum. There are disturbances in gait and coordination.
- Frontal lobe. Deviations in mental abilities, gait disturbance, inadequate behavioral reactions, slurred speech, convulsive syndrome.
- Temporal lobe. Problems with understanding speech, unilateral visual impairment, seizures.
- Base of the brain. Strabismus, blindness of varying severity, paresis, paralysis.
Localization of pathology in the brain
Complications
If treatment of the malformation is not started on time, the following consequences may be observed as the disease progresses, depending on the location of the pathology.
Brain hemorrhage. There is a rapid deterioration in health, acute pain in the head, impaired consciousness (comatosis, confusion, stupor), focal symptoms - partial or complete blindness, hearing impairment, paralysis, pathological changes in sensitivity.
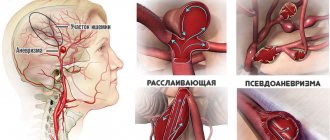
After the first hemorrhage, the risk of developing a second one increases. The cause of hemorrhage is an aneurysm formed on the walls of the vessel.
An artery affected by an aneurysm becomes vulnerable and can rupture at any time.
Progression of focal symptoms. Symptoms associated with the location of the lesion in the brain gradually worsen, and new ones appear.
It is possible to develop serious impairments of basic functions: hearing, vision, memory, thinking, coordination.
Pulmonary hemorrhage. Rapid breathing, cough with blood, decreased blood pressure, bluish skin.
Rupture of hepatic vessels. Blood is thrown into the abdominal cavity, acute pain occurs, hemodynamics rapidly drops, and shock develops.
Irreversible changes in the limb. If severe damage to the skeletal and muscular system is observed, amputation may be required.
Extensive malformation in an advanced form, localized in the spinal cord or brain, can be fatal.
Diagnostics
The primary diagnosis of AVM is carried out by a neurologist, who collects anamnesis, interviews the patient, measures pulse and blood pressure, and, if a malformation is suspected, sends for additional examinations.
Diagnosis of pathology includes:
- Ultrasound examination. It makes it possible to characterize the blood flow in the affected area and make an accurate diagnosis, but it is useless if the malformation is located deep in the tissues, in the brain, in the bones.
- MRI and MR angiography. They are used when it is necessary to clarify the diagnosis and obtain more information about the pathology. This type of study is informative for damage to internal organs and the brain. Can be done at any age.
- Computed tomography and CT angiography. They are used when pathology is localized in the bones.
- Scintigraphy. It is used in the diagnosis of pulmonary malformation in an advanced form and in cases of damage to the extremities.
- Angiography. Helpful in determining treatment methods and plan.
A general and biochemical blood test, coagulogram, echo-EG (), and Doppler sonography are also indicated.
In addition to a neurologist, consultation with a neurosurgeon, ophthalmologist and vascular surgeon may be required.
Based on the results of the diagnostic examination, a diagnosis is made and treatment tactics are determined.
Diagnosis of malformation
Treatment[ | ]
It is mainly treatable by endovascular surgery.
Principles of providing surgical care to patients with AVM.
- Complete treatment of patients with AVM requires the possibility of three main treatment options - surgical, embolization, radiosurgery.
- The decision on treatment tactics and surgical intervention for AVM should be made by a surgeon with personal experience in this field.
- When discussing the issue of indications for active methods of treatment of patients with AVM, they proceed from the ratio of the risk of spontaneous course of the disease and the risk of complications of a particular treatment method.
- The main goal of any type of intervention is complete obliteration of the malformation to prevent intracranial hemorrhage.
Treatment
The treatment of arteriovenous malformation is based on removal of the main vascular source of pathology.
There are the following methods for removing pathological areas:
Cavity or open surgical interventions , during which the abnormal area and the nearest affected areas are completely removed.
But this method of surgical treatment is difficult to carry out if the pathological process has spread widely or is localized in areas where total removal is difficult (face and neck area). In such situations, combined methods are used.
During surgical interventions of this level, the presence of several qualified doctors of different specialties is necessary: a vascular surgeon, a traumatologist, a neurosurgeon.
Laser therapy successfully removes superficial abnormal areas.
The method is often used in the treatment of malformations in children and allows you to restore the aesthetic appeal of the skin. X-ray endovascular operations. A material in the form of a solution, powder or gel is introduced into the vessel that needs to be turned off from the system, clogging it.
This treatment procedure is carried out in several sessions.
Over time, the patency of the vessel is restored, and repeated treatment is required, so the method is used autonomously only in cases where it is difficult to use other methods.
Radiosurgery. High-precision equipment - a gamma knife - is used to excise the affected area.
Before use, the affected area is precisely determined, and the directed beam destroys abnormal structures. For uncomplicated malformations, one session is sufficient, but serious disorders require long-term treatment.
Drug therapy shows low effectiveness in the treatment of AVM. Medicines are used that alleviate the main symptoms and suppress vascular growth.
Tissue biopsy
Diagnosis of cavernous angioma
Treatment of cavernoma should always begin with a full diagnosis, the scheme of which doctors determine individually for each patient. General diagnostic techniques may include the following types of studies:
- Detailed blood tests (for the presence of an inflammatory process, anemia), as well as cerebrospinal fluid tests (for the presence of hemorrhages in the cerebrospinal fluid).
Instrumental diagnostics:
- angiography method - x-ray examination of blood vessels using contrast fluid. The resulting image will help detect the degree of narrowing or destruction of brain vessels, identifying changes in the vascular wall and identifying weak points. This diagnostic procedure is prescribed to determine circulatory disorders in the brain. It allows you to clearly determine the location, volume and shape of the angioma, as well as detect the damaged vessel. Diagnostics are carried out in a specially equipped room. First, the doctor administers local anesthesia, after which he inserts an elastic catheter into the vessel and moves it to the affected area. The contrast agent introduced into the circulatory system disperses through the vascular network, after which the doctor takes several photographs, which subsequently establish the diagnosis;
- The computed tomography method is a very popular painless procedure that does not cause discomfort, and at the same time is quite informative. It is usually performed either with or without the use of a contrast agent. As a result, the doctor receives detailed layer-by-layer X-ray images in the form of two-dimensional images, which allows a detailed examination of the pathology. The procedure is carried out only in special rooms with the appropriate equipment - a tomograph;
- The magnetic resonance imaging technique is somewhat reminiscent of computed tomography, but instead of X-rays, it uses radio waves and magnetic radiation. The images are detailed and three-dimensional. The procedure is non-invasive, provides comprehensive information about the disease, but is relatively expensive;
- The electroencephalography method allows you to study the biological potentials of the brain, as well as determine where the angioma is located and what its size is. If a tumor is present, the doctor detects a change in the signal sent to the brain structures.
Nutrition for malformation
After treatment, the patient should adjust their lifestyle, give up bad habits and change their diet: this is necessary for better recovery and prevention of relapses.
Food with excess salt, fatty and fried foods, and smoked foods are contraindicated. If the patient is overweight, this has an adverse effect on the vascular structures. In such cases, you should discuss weight loss methods and nutrition with your doctor.
It is important to include healthy foods rich in valuable substances in your diet: fish, vegetables, nuts, fruits, berries. A small amount of alcohol is allowed, but drinking it in excess is unacceptable.