The control center of the pituitary gland is located in the hypothalamus. The adenohypophysis regulates five hormonal axes:
- Thyroid stimulating axis (thyroid gland) via TSH
- Corticotropic axis (adrenal cortex) via adrenocorticotropic hormone (ACTH)
- Gonadotropic axis (testes/ovaries) via follicle stimulating hormone (FSH) and luteinizing hormone (LH)
- Somatotropic axis (secretion of somatotropin or growth hormone (GH)
- Luteotropic axis: release of prolactin.
Hormones released in the neurohypophysis zone:
- Antidiuretic hormone (ADH or vasopressin)
- Oxytacin.
In pituitary insufficiency, individual or all hormonal axes may be affected. Additionally, the hypothalamus and pituitary gland may be considered a single functional unit, and damage to both regions may result in pituitary failure.
What is prolactin? Effects on women and men
There are many hormones that provide reproductive function in the body of both men and women. One of them is prolactin.
The name of the substance indicates that its main activity is related to lactation (pro lactation); the hormone prolactin in women is responsible for this process. It is important during fertilization and pregnancy.
In the body of men, this substance affects spermatogenesis. And few people know that prolactin is a stress hormone.
The main amount of prolactin is produced in the anterior lobe of the pituitary gland (adenohypophysis). This process is additionally controlled by the hypothalamus. The tissues of the central nervous and immune systems, placenta, and mammary glands also secrete this hormone in small quantities.
By its biochemical nature it belongs to peptide hormones, prolactin-like proteins. Almost all functions of the active substance are directly or indirectly related to reproduction. There are four forms of the hormone found in the body:
- monomeric prolactin (or “small” – molecular weight (MM) 22,000),
- dimeric (or “large” MW 50,000),
- three-dimensional (or “very large” MM 100,000),
- glycolyzed (MW – 25,000).
This transformation of the substance molecule is explained by the presence of three disulfide bridges, which give prolactin special chemical properties and the ability to undergo spatial modifications. Macroprolactin and monomeric substances exhibit different biological activities.
Monomeric prolactin has the highest degree of interaction with cell receptors; its share in the body is about 80%. in the blood of a large number of other forms of the hormone allows one to diagnose pathological conditions; normally they are present in the blood of healthy people, but in small concentrations.
To date, not all functions of prolactin are known. This is due to its different biological activities, which directly depend on the isoform of the substance. In medicine, there is a hypothesis that manifestations of the peripheral functions of the hormone are associated with them, but this issue has not yet been thoroughly studied.
Functions
Prolactin is produced in both sexes. The hormone affects the body of both women and men as follows:
- promotes the manifestation of secondary sexual characteristics,
- regulates sexual behavior,
- increases immunity,
- provides a balance of calcium, sodium, magnesium and water,
- released during stress to increase the body's adaptive capabilities,
- influences weight gain.
A relationship has been identified between prolactin and stress. Hormone levels increase significantly in any stressful situation. This applies to both nervous and physical stress. The concentration of the substance in the body of both women and men may increase in the presence of serious pathologies. In such cases, the endocrinologist should provide advice on hormonal therapy.
In men
In addition to the above-mentioned functions of prolactin, the specific effect of the pituitary hormone on the male body is to maintain reproductive and sexual health. The hormone has a direct effect on the formation and maturation of sperm.
Among women
The primary function of the lactation hormone in a woman’s body is the conversion of colostrum into breast milk in women in labor and the activation of its production. During the feeding period, the relationship between estradiol and prolactin is clearly expressed. The latter exhibits a contraceptive effect, suppressing the process of egg maturation.
In addition, the normal concentration of the substance is of decisive importance for the reproductive function of a woman:
- prolactin affects conception,
- ensures the attachment of the fertilized egg to the inner walls of the uterus,
- affects the normal course of pregnancy,
- promotes the active formation of glandular tissue of the mammary glands in the last trimester of pregnancy,
- reduces the pain threshold during labor,
- stimulates the newborn's first breath.
Reasons for the increase
All the reasons why prolactin can increase in women and men can be divided into three groups:
- Certain physiological conditions.
- Side effects of taking medications.
- Endocrine disorders.
A physiological increase in hormone concentration is observed:
- during night sleep (after 1-1.5 the level of the substance begins to increase),
- during sexual contact,
- with emotional overload,
- during active physical activity,
- as a result of excess protein foods.
The stress hormone prolactin gives the highest levels in the appropriate situation, which is why it has this name. Natural causes of a significant increase in the hormone are pregnancy and breastfeeding; such indicators are considered normal.
High hormone levels are observed with long-term use of drugs:
- high-dose oral contraceptives,
- antidepressants,
- anti-vomiting medications,
- drug for the treatment of ulcers and hypertension,
- psychotropic medications.
Endocrine disorders associated with increased prolactin include:
- Benign tumor of the pituitary gland (prolactinoma).
- Thyroid dysfunction. It can be caused by a disturbance in the concentration of thyroid-stimulating hormone (TSH), which is secreted by the pituitary gland. This hormone has a direct effect on the production of thyroxine and triiodothyroxine (the main thyroid hormones). Stable TSH and prolactin levels are very important during pregnancy.
- Multiple ovarian cysts.
An indirect effect on the increase in prolactin is exerted by malignant neoplasms, chronic diseases of the genital organs, herpes zoster, liver and kidney diseases, and pathological production of the hormone by other tissues.
Frequent headaches, depression, weight gain, decreased performance, emotional instability, sleep disturbances are common symptoms of increased hormone concentrations (hyperprolactinemia).
In non-pregnant and non-lactating women, high prolactin causes infertility, soreness of the mammary glands, their swelling and unreasonable secretion of milk, signs of osteoporosis are observed, and hair growth on the face, legs, and chest is activated.
Testosterone is a prolactin antagonist. In men, when the concentration of the latter increases, impotence and infertility occur, sexual desire decreases, the mammary glands increase in size, and premature hair loss on the head begins.
Reasons for the downgrade
The age-related decrease in prolactin levels is physiologically justified. But there are other reasons that lead to a decrease in hormone levels in women and men:
- heredity (genetic pathology of the pituitary gland, hypothalamus),
- increased secretion of the gonads (for example, with polycystic ovary syndrome),
- tumors and operations on the pituitary gland,
- head injuries and damage to the pituitary region,
- irradiation,
- past infectious diseases (for example, mumps in men),
- taking certain medications.
Signs of low prolactin are manifested in dysfunction of the reproductive system, mental disorders are recorded, and metabolic processes fail. Women and men develop infertility, obesity, sleep disturbances, frequent headaches, and nervous disorders in the form of phobias and obsessive fears.
Women may have self-abortions in the early stages, a small amount or complete absence of milk, and cycle disruptions. Reduced prolactin (hypoprolactinemia) is a rare phenomenon, occurs unnoticed, and the combination of symptoms is individual in nature.
To determine the concentration of prolactin, a biochemical blood test is performed, which is taken from a vein.
To obtain reliable results, the test must be taken on an empty stomach in the morning from 8 to 10, and a number of preparatory measures must be followed (exclude stress factors, sexual intercourse, exposure to excessive heat and cold). Limitations are due to the fact that the level of the substance changes during the day and is influenced by external factors.
A laboratory blood test is not the only method for determining the concentration of the active substance. A more reliable result is obtained when conducting a complex of medical studies. In case of significant deviations from normal indicators, the following is additionally carried out:
- MRI of the brain. The area of the pituitary gland and hypothalamus is examined. Contrast if necessary.
- Radiography. Skeletal bones are analyzed for irritation.
- General examination of the thyroid gland. The activity of the pituitary gland is associated with the secretion of thyroid hormones.
- Ultrasound. The condition of the kidneys, liver, ovaries, and mammary glands is diagnosed to identify possible pathologies.
- Determination of cholesterol and blood sugar levels for overweight patients.
- Additional examination by an ophthalmologist. Recommended if pathologies are detected after MRI.
Treatment
Prolactin concentrations can be stabilized using drug therapy, traditional medicine, and lifestyle adjustments. The treatment regimen depends on the diagnosed root cause of the disease, so a set of therapeutic measures is selected individually.
In case of minor deviations from the norm and in the absence of pathologies of internal organs, drug therapy is not required. You need to follow simple rules:
- sufficient physical activity, special practices (for example, yoga),
- normalization of weight,
- proper nutrition, enriched with vitamins and minerals,
- eliminating stress factors.
If the levels are too high, drug therapy is prescribed. The drug and its dosage are determined only by the doctor. If the increase in hormone levels is associated with prolactinoma, surgery is performed to remove the tumor.
In folk medicine there are no recipes that are directly aimed at regulating hormone levels. Herbal medicinal raw materials have a symptomatic effect, have a sedative effect, or are aimed at reducing weight.
There are no special therapeutic measures to correct low prolactin; only symptomatic treatment is carried out.
Nutrition
To lower prolactin levels, you need to follow a special diet. The emphasis should be on products that contain:
- Folic acid. It improves the absorption of proteins and stimulates the production of sex hormones. Liver, meat, spinach, parsley, eggs.
- Vitamin B12, the sources of which are poultry, beef, sea fish, liver and other offal, dairy products. The B12 they contain is well absorbed in the presence of calcium.
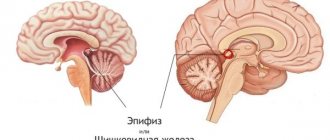
Location of the gland
Location of the pituitary gland in the skull
Topographically, it is located approximately in the very center of the head.
The weight of the pituitary gland is only about 1 gram, and its dimensions do not exceed 14-15 mm.
The pituitary gland has an oval shape and is located in an isolated bone bed (sella turcica), which also has an oval shape. The pituitary gland is surrounded by bone formations on three sides - front, back and bottom. On the sides of the pituitary gland are the cavernous sinuses - hollow cavities consisting of sheets of dura mater, inside which pass such important vessels as the carotid arteries and nerves, most of which control the movement of the eyeballs.
From above, the cavity of the sella turcica is also limited by a fibrous layer of the dura mater - the diaphragm, which has a hole in the center, through which the pituitary gland, through the pedicle, is connected to one of the parts of the brain - the hypothalamus. Figuratively speaking, the pituitary gland hangs on a stalk (stem) like a cherry on a stem.
As a rule, the pituitary gland occupies the entire volume of the sella turcica, but there are various options when it occupies only half of it or, on the contrary, the pituitary gland increases in size, even slightly extending beyond the upper boundaries of the sella turcica.
The bone box that forms in the sphenoid bone and acts as protection for the pituitary gland from various injuries is called the sella turcica. It is located next to the arterial basin with its carotid arteries and venous sinus. The pituitary fossa is intended to house the pituitary gland.
The separation of the pituitary gland and hypothalamus is facilitated by a special diaphragm (formed from a process of the dura mater of the brain). At the same time, the diaphragm acts as an intermediary between the infundibulum of the hypothalamus of the diencephalon and the pituitary gland. For this purpose, there is a special hole in its center. What is the pituitary gland responsible for in women? More on this later.
How to cure pituitary adenoma
Treatment is prescribed taking into account all clinical symptoms, progression and secretory activity of the pituitary adenoma.
When diagnosing somatotropinoma, corticotropinoma, gonadotropinoma and macroadenoma, most patients undergo surgical removal together with radiation therapy. But if somatotropinoma does not produce pronounced symptoms, its growth is suppressed without resorting to surgery.
When a prolactinoma is detected, which in a laboratory blood test shows a prolactin level of more than 500 ng/ml, they initially try to suppress its activity with medications, and only if there is no therapeutic effect, an operation is performed, regardless of the level of hormones.
By analyzing the research results, the treating specialist receives an accurate idea of why an adenoma is dangerous and what pharmacological agents should be chosen.
Appointed:
- dopamine receptor agonists Parlodel, Cabergoline (analogue of Dostinex), Norplorak, Bromocriptine;
- serotonin blockers Dolasetron, Tropisetron;
- inhibitors of hormones produced by the pituitary gland - Somatostatin, Lankreotide, Okreotide;
- cortisol secretion inhibitors Cytadren, Mitotane, Ketoconazole.
If the pituitary adenoma responds to drug therapy, then the prognosis based on statistical data is as follows:
- hormonal levels are normalized in 30–32% of patients;
- tumor reduction or stopping its growth is achieved in almost 55–57%;
- in the case of corticotropinoma, remission is observed in almost 80 patients out of 100.
How to treat pituitary adenoma if medications do not help. In this case, they resort to a surgical solution to the problem, using:
- Transsphenoidal (endoscopic) excision of a pituitary adenoma, performed with general anesthesia and penetration to the tumor area through the nasal passages. The operation is performed if a growth is detected that does not extend beyond the contours of the sella turcica by more than 20 mm, or micro- and macroadenomas are detected that do not compress adjacent tissues.
- Transcranial removal involving craniotomy. It is carried out if the tumor becomes more than 100 mm in diameter, affecting adjacent sections.
Diagnostics
Diagnosis of a pituitary tumor is one of the main treatment procedures. If a pituitary tumor is suspected, the following diagnostic methods are used:
- blood and urine tests to determine hormone levels;
- ophthalmological examination to diagnose the size and direction of the tumor;
- analysis of spinal cord fluid for protein compounds that may indicate the development of cancer;
- hardware diagnostics MRI and CT of the brain, allowing to identify small adenomas and their location.
In addition to general and biochemical blood tests, the following tests are used for better diagnosis:
- Stimulation of adrenocorticotropic hormone - administration of ACTH, which actively stimulates the adrenal glands, and checking the level of cortisol in the blood; if the production of ACTH is blocked by the adenoma, then the adrenal glands do not secrete cortisol in response to stimulation;
- Carrying out a metyropane test - the patient takes 3 grams of metyropane before bed and takes the result in the morning; an increase in hormone levels in the morning indicates the effect of adenoma on hormone synthesis;
- Conducting an insulin tolerance test - using insulin to lower sugar levels; with the development of an adenoma, there will be no secretion of growth hormone and ACTH.
Particular attention is paid to pregnant women. During pregnancy, diagnosis of the disease occurs with extreme caution. Magnetic resonance imaging methods are excluded and are performed only after childbirth. Otherwise, the patient is prescribed examinations by an ophthalmologist, neurologist, blood and urine tests. An increase in tumor size can be judged by a decrease in breast milk production.
In childhood, pituitary adenoma appears quite rarely. If the first signs occur, you should immediately consult a doctor and not self-medicate.
Treatment methods for pituitary gland problems
The earlier the disease is detected, the greater the chances of a positive solution to the problem. Treatment is prescribed by specialists - a neurosurgeon and endocrinologist - based on the results of examinations, when the type of pathology, its size and location are identified.
There are several ways to treat a tumor:
- Medication. Medications are prescribed whose action is aimed at shrinking adenomas, as well as regulating the level of hormones in the blood.
- Surgical intervention. An effective method associated with penetration into the area of the inflammatory process through the sinuses. This allows you to avoid incisions and the risk of infection of the body during surgical operations.
- Radiation therapy. It is used in cases where surgical intervention is not possible. In modern medical practice, a radiosurgical method is used, which involves the use of a cyberknife. It irradiates the affected area from all sides and avoids invasive intervention in the body. The dose is selected individually, taking into account the characteristics of the tumor, as well as the patient’s condition.
In some cases, mixed types of treatment are used to achieve maximum effect in a short time.
When deciding on a treatment option, it is important to consider all components of the process. Taking medications must be agreed with your doctor. Self-medication and self-prescription of medications is prohibited.
Conservative treatment is popular in the presence of minor disorders of the pituitary gland. When a benign tumor (adenoma) develops, dopamine agonists, analogues or somatropin receptor blockers and other drugs can be used. The choice of a specific medication depends on the stage of benign formation and the rate of progression of all unpleasant symptoms. Drug therapy is considered ineffective, since a positive result from its use is observed only in 25-30% of cases.
Treatment of problems with the pituitary gland, accompanied by a lack of certain hormones, occurs with the use of hormone replacement therapy:
- with the development of secondary hypothyroidism, which is accompanied by TSH deficiency, the use of L-thyroxine is necessary;
- if there is a deficiency of the hormone somatotropin in children, treatment with recombinant growth hormone is indicated;
- for ACTH deficiency, glucocorticoids are used;
- if the concentration of LH or FSH is insufficient, the use of estrogens with gestagens for women and testosterone for men is indicated.
Hormone replacement therapy often lasts for life, since it is unable to eliminate the causes of the disease, but only affects unpleasant symptoms.
Hormone replacement therapy in women
If there are no visual impairments and abnormalities in blood tests for hormones, then an enlargement of the pituitary gland requires only observation. Patients are prescribed tomography and repeated blood tests, examination by a neurologist and an ophthalmologist once a year. If an adenoma is detected, then depending on its size and hormonal activity, the doctor chooses treatment tactics:
- removal through the nasal passages (endonasal transsphenoidal adenomectomy) – performed when there is an increased level of hormones with corresponding symptoms, signs of compression of the optic nerves, high intracranial pressure;
- surgery with opening of the skull - a large tumor that cannot be removed by endonasal access, since there is a possibility of damage to neighboring brain structures.
- radiation therapy is prescribed for inactive tumors (does not produce hormones), for elderly patients, or for contraindications to surgery; radiation is also indicated after surgical removal of a large adenoma;
- cryodestruction - inserting a probe through the nasal passage into the pituitary gland and applying cold to it to destroy the tumor;
- medications - somatostatin, which suppresses the formation of growth hormone, Parlodel and Dostinex for high prolactin, Peritol to inhibit cells that produce corticotropin and somatotropin.
After surgery, hormonal deficiency may occur. To correct it, analogs of natural hormones are used - levothyroxine, hydrocortisone, estradiol, testosterone. The same tactics are needed if the cause of the enlargement of the pituitary gland is diseases of the glands of the endocrine system.
Violation of hormone secretion
Many factors, both mechanical and chronic diseases, can affect the functioning of the pituitary gland. They lead to the formation of a tumor, adenoma or prolactinoma. The reasons that provoked the development of pathology:
- surgery in which the pituitary gland was damaged;
- severe traumatic brain injuries when the gland is affected;
- infection of the membranes of the brain tissue (tuberculosis, meningitis, encephalitis);
- long-term use of hormonal drugs;
- hypothyroidism or hypogonadism;
- intrauterine teratogenic effect on fetal development;
- insufficient blood supply or, on the contrary, hemorrhage;
- irradiation for cancer of organs or blood.
Adenoma is characterized as a benign formation, reaching up to 5 millimeters in size. It can compress the gland, causing it to enlarge, which interferes with the full functioning of the pituitary gland. Another negative feature of the tumor: it itself is capable of producing hormones.
With an excess or deficiency of hormones, serious pathologies develop, in some cases death is possible. Most often, the reasons for this process are:
- tumors, including hormonally active ones;
- meningioma or aneurysm;
- traumatic brain injuries;
- vascular damage and hemorrhage due to stroke;
- errors during surgical interventions;
- uncontrolled use of drugs;
- developmental defects;
- necrosis;
- irradiation;
- autoimmune disorders.
The initial stages of the disease often have symptoms that are similar to other pathologies not related to the functioning of the endocrine system. For example, chronic fatigue, headaches, disrupted menstrual cycles, decreased visual acuity, sudden weight changes, signs of dehydration and extreme thirst may indicate both excessive exercise, an incorrect diet or allergic diseases, and excessive or insufficient production of hormones by the pituitary gland.
The absence of any symptoms is also quite common in the first stages of dysfunction of the pituitary gland. A person can only find out about her problems after a diagnosis is made after the characteristic signs of a disease caused by a decreased or increased amount of hormones produced appear.
Folk remedies
Treatment of pituitary adenoma with folk remedies is not the most effective method of influencing the capsule. The fact is that most often patients waste time on ineffective methods. In the case of pituitary adenoma, traditional methods not only do not help, but even harm.
If the doctor has made a diagnosis, you should not waste time on ineffective methods. It is necessary to adhere to the methods prescribed by the attending doctor. If you want to use folk remedies, then first obtain his approval. Only proper treatment will help curb the growth of the tumor.
Vasopressin (ADH)
Vasopressin (also called antidiuretic hormone - ADH) has two functions in the body. It has an antidiuretic effect, i.e. enhances the reabsorption of water in the collecting ducts of the kidneys and, in addition, it affects the smooth muscle of arterioles (small blood vessels that arise from arteries), i.e.
Thus, hormones of the posterior lobe of the pituitary gland, when produced insufficiently, can cause diabetes insipidus (antidiuretic effect), in which up to 15 liters of fluid can be lost per day (excreted in the urine). This loss must be constantly replenished. People with diabetes insipidus experience constant thirst.
Complications
Consequences rarely appear. Usually this is bleeding, disruption of the movement of cerebrospinal fluid, injury to brain tissue. The reasons for this are different. Infection with viruses leads to meningitis. Patients will receive information about possible consequences from their attending physician. The possibility of complications should not become an obstacle to treatment. Any other development of events will result in death.
The postoperative period after tumor removal is positive. 3 days after the operation the patient is discharged. Further observation is carried out by an endocrinologist. If necessary, hormone therapy and massage are prescribed. Patients are prescribed a special diet. Avoid drinking alcohol, fatty foods and salt. They are able to resume the activity of remaining cancer cells.
Possible complications include the appearance of ulcers in the gastrointestinal tract. They develop due to damage to the nervous system. Ulcerative wounds lead to bleeding, which leads to the death of the patient. But the disease occurs rarely. After the tumor is eliminated, diabetes insipidus may occur. As a result, kidney function is impaired.
Repeated removal surgery is accompanied by high risks. Getting rid of adenoma is difficult. Scarring and inflammation increase, and brain tissue is severely damaged. Patients who relapse are susceptible to serious side effects and mortality. To avoid difficulties at the first stage, surgery and radiation therapy are combined to effectively remove the adenoma.
Oxytocin
Thus, the hormone oxytocin affects the contraction of the uterine muscles during childbirth. On the surface of cell membranes there are special receptors sensitive to oxytocin. During pregnancy, this hormone does not rise to a level that can cause contractile activity of the uterus. Only immediately before the birth itself, under the influence of the female hormones estrogen, sensitivity to oxytocin increases and childbirth occurs. It also causes the myoepithelial cells located in the mammary glands to shrink, which stimulates milk production.
The effect of oxytocin on the male body has not been sufficiently studied. It is believed that it is able to influence the functioning of the intestinal walls, gallbladder and bladder.
Hypogonadism
This disorder occurs when the anterior lobe of the pituitary gland fails to produce the hormone gonadotropin. This disease is also called Kallmann syndrome.
In this case, the following violations arise:
- delayed puberty;
- infertility;
- decreased libido;
- underdevelopment of the reproductive system, defective formation of the genital organs.
Important. Lack of gonadotropin affects only the functioning of the reproductive system.
One of the types of hypogonadism is hypogonadotropic hypogonadism. In this case, a deficiency of gonadotropin, follitropin and lutropin is diagnosed. Violations in adolescents are quite serious. Girls do not have breasts before the menstrual cycle begins, and boys do not grow genitals. Children do not show all signs of puberty.
Fertile eunuchoid syndrome is a consequence of hypogonadism. It develops as a result of lutropin deficiency. Often the disease is congenital. A small amount of lutropin causes testosterone deficiency, which leads to infertility.
Important. The condition can be improved by administering human chorionic gonadotropin if there are no congenital malformations of the reproductive system.
Diabetes insipidus
Occurs when there is a deficiency of vasopressin (antidiuretic hormone), which is synthesized in the posterior lobe of the pituitary gland.
Symptoms of the disorder:
- intense thirst;
- excretion of a large amount of daily urine (up to 25 l);
- dry skin;
- swelling;
- sweating
Note. All of the above symptoms appear due to impaired renal function as a result of vasopressin deficiency.
The disease can be caused by infections, brain injuries, or pituitary tumors.
Oxytocin, etc.) in the gland decreases or completely stops. Each of them is responsible for the functioning of a specific endocrine gland, so if there is insufficient quantity, a malfunction occurs throughout the body.
Hypofunction of the pituitary gland leads to the development of disorders at any age, in most cases this occurs with brain injury, genetic pathologies or heavy bleeding.
Useful video
- Hormones for endometriosis: which tests are taken...
Hormones for endometriosis are always analyzed. They are analyzed to prescribe treatment. And to delay the spread of the disease, they choose the IUD and contraceptives. Which hormones are elevated and which are deficient in fibroids and endometriosis? - Male hormone preparations: what are the dangers, the harm from...
For congenital diseases or disorders of the testicles and pituitary gland, male hormone preparations are prescribed. They increase the natural level, for men this contributes to the treatment of infertility, muscle growth, and normal functioning of the glands. How dangerous and harmful are male hormone preparations?
- Hypothalamus: tests, other diagnostics, how to check...
If the hypothalamus is not working properly, tests will help identify the cause of the hormone production disorder. Diagnostics includes instrumental and laboratory studies. How to test the hypothalamus?
- Melanostimulating hormone (melanotropin): how...
In the body, melanostimulating hormone not only gives pigmentation to the skin, hair, and mucous membranes, but also acts as a kind of protection from rays. It is also called melanotropin. What is the effect of excess and deficiency?
- Resistance to thyroid hormones: syndrome...
Mostly, resistance to thyroid hormones occurs as a hereditary pathology, less often - from gene mutations. There is both a syndrome and a total one. Treatment is predominantly symptomatic.