ST segment depression
The highest mortality rate was observed in patients with simultaneous ST segment depression and frequent or complex extrasystole against the background of low tolerance.
7 people had this combination of stress test indicators, of whom 6 (85.7%) died during follow-up. The data obtained thus indicate the obvious advantages of the stress test for identifying patients most at risk of death from coronary artery disease. The results of risk stratification also show that a stress test is preferable for identifying individuals with a favorable prognosis.
Thus, the group with the lowest risk of death from coronary heart disease (mortality rate 1.7%) identified using stress test indicators was 233 people, or more than 3/4 of all those examined, while using ECG monitoring only 52 people were identified, i.e. i.e. 1/6 of those examined with the same favorable prognosis (mortality rate 1.9%).
The group of very low risk of death from coronary artery disease according to the stress test included people with high tolerance (regardless of the presence of ST segment depression and ventricular extrasystole), as well as patients with low tolerance, but without these disorders recorded using an ECG.
The group with the most favorable prognosis according to ECG monitoring data included patients in whom no ventricular extrasystoles were recorded during the day. In addition, the stress test indicators, in contrast to the monitor ones, made it possible to identify patients at risk of recurrent non-fatal myocardial infarction. These patients were characterized by the appearance of an angina attack during the test or a drop in systolic blood pressure, as well as depression of the ST segment when the heart rate reached more than 115 per minute during exercise.
The frequency of repeated non-fatal myocardial infarction in patients with this combination of stress test indicators was 8.9% and was more than 5 times higher than in the rest of the examined patients.
“Sudden death of patients with coronary heart disease”, N.A. Mazur
www.serdechno.ru
With a serious lack of oxygen in the myocardium, cascade changes appear at the biochemical level on the electrocardiogram - elevation or depression of the st segment.
Consider such changes as acute until arguments refute this statement.
In about one out of five cases, after the end of an attack of tachycardia, for some time (up to several weeks) there is a decrease in this segment of the arterial phase, prolongation of the QT interval and unmotivated T waves, expressing myocardial ischemia. With prolonged changes in the electrocardiogram, a conclusion about a small-focal infarction is possible.
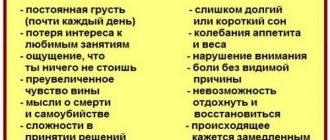
- Reduced concentration and attention are manifested in difficulty memorizing and low academic performance. Physical activity is also significantly reduced, to the point of stupor, which may be considered laziness. Adolescent and childhood depression is often accompanied by aggressive attacks and increased conflict, which hide self-hatred.
- The mood becomes better in the evening. Self-confidence disappears and self-esteem decreases. Due to these feelings, the patient moves away from society and strengthens his emerging feeling of inferiority. Long periods of depression in patients over 50 years of age are accompanied by deprivation and a clinical picture that is similar to dementia. Constant gloomy thoughts, a pessimistic attitude, an increasing sense of guilt, self-deprecation - a familiar state? It is this that is most often shown in all films, associating it with the depression of the Art. segment. And the patient, just like in all such films, thinks about causing harm to himself, or even comes to thoughts of suicide.
- The patient begins to sleep poorly, may have nightmares, and finds it very difficult to get up in the morning. Appetite worsens, and there is a frequent preference for carbohydrate foods over protein foods. The desire to eat may appear in the evening. A person in a state of depression has a distorted sense of time: for him it lasts a very long time.
- Another important sign is a reluctance to take care of oneself, which leads to an extremely sloppy appearance, at a minimum.
- Dilated pupils.
- Reduced elasticity of the skin, it becomes flabby.
- The patient seems much older than his years.
- Sexual desire increases, because this reduces the level of anxiety.
- At the genetic level, depression ct is caused by a pathology of the eleventh chromosome.
- With the biochemical path of development of this diagnosis, the exchange of catecholamines and serotonin is complicated.
- Loss of loved ones and relatives in adolescents over eleven years of age.
Journal "Emergency Medicine" 1(26) 2010
Introduction
Left ventricular myocardial strain syndrome (LVMS) - strain syndrome - is an electrocardiographic concept that includes ST segment depression turning into a negative asymmetrical T wave, described by Rykert and Hepburn in 1935 as a sign of LV hypertrophy [1].
A revision of this concept undertaken in 1981 by C. Beash et al. [2], suggested that changes in repolarization in left ventricular hypertrophy (LVH) without signs of coronary artery disease may differ from similar changes in coronary heart disease in several ways. Firstly, by a decrease in the J point, secondly, by the asymmetry of the T wave with a rapid return to the baseline, thirdly, by the positive final deviation of the T wave and, finally, fourthly, by the negative TV6 wave, which is greater than 0, 3 mV and greater than the T wave in V4. However, in clinical practice, such differentiation of signs of LV SUI due to its hypertrophy from ST-T changes in coronary heart disease is most often impossible. Previously, W. Kannel et al. [3] recognized that in LVH, the presence of ST-T changes is a risk factor for coronary pathology. Recently, ST-T changes have been assessed as a risk factor for the development of heart failure [4] in patients with arterial hypertension (AH). LV SUI is recognized as a predictor of cardiovascular death and mortality in hypertensive patients [4]. There is an opinion that aggressive antihypertensive therapy, leading to a significant decrease in both systolic blood pressure (SBP) and diastolic blood pressure (DBP), in the presence of impaired repolarization in the left precordial leads and voltage criteria for LVH, may increase the risk of cardiovascular death [5]. An increase in LV mass with a decrease in ejection fraction, according to echocardiography (EchoCG), leads to the development of heart failure [6]. However, it is impossible to verify precisely whether LV SUI in LVH in hypertensive patients is an independent predictor of the development of heart failure. P. Okin et al. (2007) [4], in a study of 8854 patients with hypertension, showed that LV SUI occurs more often in older people in the presence of other cardiovascular pathologies (primarily ischemic heart disease, myocardial infarction), diabetes mellitus, previous cerebral stroke, heart failure and peripheral vascular diseases. The exact reasons for the increase in cardiac mortality in LV SUI are unknown. However, there is a strong connection between strain syndrome and structural and functional disorders of the cardiovascular system. Changes include concentric hypertrophy, lower LV contractility, and higher myocardial oxygen demand, these factors may partly explain the poor prognosis of this syndrome. According to recent data from a population-based study, an increase in LV mass calculated from echocardiography and ST segment depression have independent prognostic significance [5]. When analyzing an electrocardiogram (ECG) with signs of LVH, there is still no consensus on the reasons causing changes in the ST segment. On the one hand, it is recognized that severe myocardial hypertrophy can cause a decrease in coronary reserve. In addition, many researchers have identified dysfunction of the coronary endothelium caused by hypertension. On the other hand, the postulate about the connection between ST segment depression and increased intracavitary pressure is not disputed. Finally, no one rejected the basic electrophysiological concept of interpreting ST changes in LVH as a result of changes in the direction of currents during the period of restoration of the transmembrane potential. The emergence of new technologies for dynamic monitoring of ECG, including Holter monitoring (HM), led to the emergence of the term “silent ischemia”. Initially, this term was used to characterize myocardial changes in patients with proven atherosclerotic narrowing of the coronary arteries. In this case, “silent ischemia” was understood as ST segment depression that met certain requirements (horizontal or oblique type of ST decrease, ST decrease at points J and J+80 ms by 1 mm or more, lasting at least 1 min, etc. ) and not accompanied by pain. Subsequently, any silent ST depression detected during dynamic monitoring of the ECG began to be called “silent ischemia” of the myocardium in the domestic literature [7]. This term began to be used to identify ST segment depression in patients with hypertension. This “silent ischemia” was explained either by a relative insufficiency of coronary blood supply with an increase in the mass of the LV myocardium, or by an increase in intracavitary and, accordingly, intramyocardial pressure. In addition, a number of hypotheses have been put forward about the remodeling of the coronary arteries and the possibility of spastic reactions of the coronary arteries in patients with hypertension. According to N.A. Mazura [7], “painless depression of the ST segment” in CM appears in patients with severe LVH and impaired diastolic function, who have areas with reduced myocardial perfusion on radioisotope scintigraphy.
The purpose of this study was to assess the relationship between LV SUI in patients with hypertension and ECG voltage signs of LVH, with heart rate (HR) with HM ECG, blood pressure level with bifunctional ECG and blood pressure monitoring, as well as with local contractility of the LV myocardium with stress echocardiography in patients with hypertension with unaffected coronary arteries.
Materials and methods
We examined 342 patients with hypertension. In 192 patients - 154 patients with stage I hypertension (SBP in the range of 140–159 mm Hg, DBP in the range of 90–99 mm Hg) and 38 patients with stage II hypertension (SBP in the range of 160–179 mm Hg) . and DBP - 100–109 mm Hg) - assessed the relationship of ST segment depression with ECG voltage criteria for LVH according to resting ECG-12 data. Of these, 180 patients with hypertension (144 with stage I hypertension and 36 with stage II hypertension) underwent a 24-hour ECG monitoring to study the nature of changes in the final part of the ventricular complex and their relationship with heart rate. Bifunctional blood pressure and ECG monitoring was performed in 122 patients (113 with stage I hypertension and 9 with stage II hypertension), and the relationship of ST changes with blood pressure levels was studied. Stress echocardiography was performed in 30 patients with stage I–II hypertension (18 patients with bicycle ergometer exercise and 12 patients with transesophageal electrical stimulation of the atria). All these 30 patients had intact coronary arteries according to coronary angiography (CAG).
We especially note that none of the hypertensive patients included in the study had clinical signs of coronary artery disease.
ECG-12 was recorded using a Megacard-B device. The change in ST was taken to be a shift of the J point by 1 mm in leads V5–V6, where the maximum ST shifts associated with impaired repolarization in LVH are detected. LVH was established when at least one of the two most informative voltage criteria for hypertrophy was met, namely the total Sokolov-Lyon index (for people under 40 years old - more than 40 mm, for people over 40 years old - more than 35 mm) and the Cornell voltage criterion (for women - more than 20 mm, for men - more than 28 mm). Holter and bifunctional monitoring were carried out using the Holter-DMS and Soyuz (Moscow) systems. The ST segment analysis was carried out using parameters based on fractional integrals of the first half of the ST-T segment, calculated on 16 averaged cardiac cycles with a correlation coefficient (at least 4 of them) exceeding 0.85. The threshold value of the ST segment displacement is taken to be a deviation from the baseline level of 0.1 mV. ST changes were assessed in lead MV5. For more details on the method for assessing ST displacement during HM ECG, see [8].
All ECG recordings were analyzed in automatic and interactive modes. Automatic analysis of ST changes was focused on the diagnosis of myocardial ischemia and therefore aimed at identifying ST changes specific to ischemia, namely a decrease in ST by 1 mm or more with a horizontal or oblique type of change. In the presence of persistent ST segment changes, comparison with an automatically selected representative QRST complex excluded a false diagnosis of ischemia. Therefore, in automatic ECG analysis, the term “ischemic ECG changes” referred only to pronounced short-term decreases in ST compared to the initial reference level, formally satisfying the ECG criteria for ischemia. The term was used primarily to alert the clinician to the presence of a corresponding episode of ST segment depression.
Each case of automatic detection of “ischemic ST changes” was monitored visually in interactive mode. The final decision on the presence of ischemic signs of ECG changes was made by the physician.
Stress echocardiography was performed on Vivid 7 (GE Healthcare) and Sonos 7500 (Philips) devices using stress packages. For details on the study, see [9].
results
Effect of LVH on ST segment depression
When comparing changes in the final phase of the ventricular complex with the severity of voltage signs of LVH in 192 patients with hypertension, the following was revealed. Of 154 patients with “mild” hypertension, changes in the ST segment on the resting ECG were detected in 24 cases, and in half of the patients they were detected in the presence of voltage criteria for LVH and in the same number - without signs of LVH. ST segment changes were absent in 130 cases, of which 25 patients had voltage criteria for LVH and 105 patients had no criteria for LVH. In this group of patients, the T waves were biphasic, flat or positive, i.e. they did not have the described signs of LV SUI. Of 38 patients with moderate hypertension, changes in the ST segment on the resting ECG were detected in 16 cases, 14 patients with voltage criteria for LVH and 2 without signs of LVH. ST segment changes were absent in 22 cases, of which 9 were in the presence of voltage criteria for LVH and 13 were in the absence of criteria for LVH. In 14 cases described above, ST changes were accompanied by biphasic or negative asymmetric T waves.
Thus, in grade I hypertension, voltage signs of LVH are detected in a quarter of those examined - 37 (24.0%) of 154 cases, and changes in the final part of the ventricular complex are even less common - in 24 of 154 (15.6%) cases, and they in half of the cases they are not accompanied by voltage signs of hypertrophy. With stage II hypertension, the frequency of occurrence of these and other signs increases: voltage signs of LVH are detected in 23 (60.5%) of 38 cases, and ST depression - in 16 (24.1%) of 38 cases, and much more often ST depression is accompanied by both voltage signs of hypertrophy and negative asymmetric T waves.
Thus, out of 40 cases with ST depression, signs of LVH were detected in 65% of those examined, ST changes without voltage criteria for LVH were found in 10.6% of cases. As we already noted in the introduction, one of the main factors influencing changes in the repolarization phase in patients with hypertension is an increase in the mass of the LV myocardium and, accordingly, the formation of its hypertrophy. However, there are observations when changes in the final part of the ventricular complex are not accompanied by an increase in QRS voltage.
Characteristics of dynamic changes in the ST segment according to HM ECG data
Of the 180 monitored patients with hypertension, 34 were found to have ST segment depression in lead MV5: 15 in patients with stage I hypertension and 19 in patients with stage II hypertension. In the latter, ST depression turned into a negative asymmetric T wave, i.e. there were signs of strain syndrome.
Two types of ST changes were identified. The first type is short periods of transient ST depression in lead MV5 in the absence of persistent depression, or a significant (more than 1.5 mm compared to baseline) worsening of existing depression. This ST depression turned into biphasic, flattened or positive T waves, i.e. did not meet the criteria for LV SUI. The second type is constant ST segment depression of more than 1 mm throughout the entire day (more precisely, the presence of ST depression for at least 75% of the recording time). This depression was accompanied by the registration of negative asymmetric T waves, i.e. could be classified as LV SUI. In total, type 1 depression occurred in 8 out of 34 cases with depression. Moreover, in patients with stage I hypertension, such episodes of ST depression were detected in 7 out of 15 cases, of which in 6 cases - with increased heart rate, and in one case - with unchanged heart rate. In the group of patients with stage II hypertension, a short episode of ST depression in the absence of persistent depression was detected in only 1 case with an increase in heart rate.
Each increase in rhythm is accompanied by a slight increase in ST depression. Maximum depression is observed at 18:14 when the rhythm increases to 125 beats/min and the degree of depression is less than 1 mm on the 1st and 2nd recording channels.
Depression of the first type demonstrates persistent ST depression of less than 1 mm in a patient with “mild” hypertension. At 8 hours 50 minutes, during an increase in the rhythm to 110 beats/min, a more pronounced depression of the horizontal ST segment was recorded with a decrease in the J point to 1.5 mm, lasting 80 ms from the J point. According to traditional criteria, this type can be assessed as ischemic.
Depression of the second type (persistent ST segment depression) was identified in 26 of 34 cases. At the same time, in patients with stage I hypertension, this type of depression was found in 8 (53.3%) of 15 cases, and in patients with grade II hypertension - in 18 (94.7%) of 19 cases. In the first group, a pronounced worsening of ST depression against the background of persistent depression was detected in 2 cases; in one of them - when the heart rate increases, and in the other - when the rhythm slows down. In the second group, a pronounced worsening of ST depression against the background of persistent depression was detected in 4 patients, all with increased heart rate.
There may be persistent ST depression with negative asymmetric T waves, independent of heart rate dynamics. Throughout the day, oblique ST depression is detected (J point up to 1.5 mm), turning into a negative T wave.
Severe persistent ST depression up to 2–3 mm. CM was performed in a 52-year-old patient with stage I hypertension. At moments of tachycardia, ST segment depression increases to 5–6 mm. Its slanting type, turning into a negative T wave, fits the criteria for both LV SUI and ischemia.
Thus, in CM patients with stage II hypertension, constant depression of the ST segment with a negative T wave is more often detected. In patients with “mild” hypertension, short episodes of ST depression, without negative T waves, associated with increased rhythm, predominate. Worsening ST depression in persistent depression is most often rhythm-dependent.
Bifunctional monitoring of ECG and blood pressure, correlation of ST changes with blood pressure levels
As we found, in 43% of cases, ST segment depression is associated with the presence of voltage criteria for LVH. However, there remains a fairly large percentage of cases (10.5%) in which ST segment depression is not accompanied by voltage criteria for hypertrophy. Let us recall that the examined patients did not have clinical signs of ischemia (distinct pain syndrome). Therefore, the question arises about other reasons for ST changes in patients with hypertension, first of all, whether in these cases ST changes are manifestations of LV SUI during extreme increases in blood pressure. To answer this question, a group of 35 patients with hypertension was examined using bifunctional monitoring.
In 9 cases, it was possible to identify ST depression and deep negative T waves with an increase in heart rate or rise in blood pressure.
Only in 1 case, depression of the ST segment was detected during increases in blood pressure and did not have a direct connection with an increase in heart rate: at maximum blood pressure, a significantly greater decrease in ST was observed than at maximum heart rate. In cases 2–4 and 6–9, the level of ST decrease increased with an increase in heart rate. In example No. 5, with an increase in heart rate and a rise in blood pressure, the depression reached –2 mm at a normal heart rate, but at maximum blood pressure there was a similar depression, i.e. it can be assumed that the main factor causing the development of LV SUI was an increase in blood pressure. It should be noted that the patients taken into the study had “mild” or moderate hypertension. Perhaps, at higher levels of blood pressure rise, the percentage of detection of LV SUI would be higher.
Dynamics of ST according to the results of EchoCG [9]
30 patients with “mild” hypertension and suspected ischemic heart disease were selected. All patients underwent coronary angiography, which revealed no stenosing lesions of the coronary arteries in any of the 30 cases. According to stress echocardiography, in no case was the appearance of ischemic disorders of LV contractility noted, i.e. all samples were regarded as negative. The ECG in 9 of these patients showed a typical strain syndrome: a decrease in the ST segment by 1 mm or more with deep negative asymmetric T waves.
Discussion
Hypertension is often accompanied by the formation of hypertrophy of the left heart, which is manifested by specific ECG changes in the voltage of the ventricular complex and the appearance of strain syndrome. Similar changes in patients with LVH with normal coronary arteries have been described [10].
An increase in the voltage of the ventricular complex, associated with an increase in the mass of the LV myocardium due to an increase in the size of cardiomyocytes and, accordingly, an increase in the potential gradient on the cell membrane, is an established and unquestioned fact [11]. In this regard, systems for quantitative assessment of LVH using voltage criteria of the waves of the ventricular complex have been developed. With a clear and harmonious system of explanations for the increase in the voltage of the ventricular complex with experimentally simulated changes in the depolarization process in LVH, the observed disturbances in the repolarization phase in the form of strain syndrome do not have such a convincing justification. The most acceptable point of view on the discrepancy between the polarity of the ventricular complex and the ST segment and T wave in LVH can be recognized as a change in the direction of movement of the repolarization front due to a delay in recovery processes in the epicardial layers. Otherwise, one should assume the existence of a certain repolarization component that does not spread in space [11]. The great clinical and prognostic significance of repolarization phase disturbances in LVH forces us to see local (subepicardial) or diffuse (subendocardial) blood flow disturbances in the causes of these changes and explain these disturbances from the standpoint of myocardial ischemia. At the same time, clinical experience shows that repolarization disorders are more pronounced the greater the degree of hypertrophy, i.e. in the presence of ST-T changes and large QRS amplitude (various positive voltage criteria for LVH) in the absence of clinical coronary syndrome, an increase in mortality rates [4, 5, 12] may reflect the general hemodynamic situation, most likely associated with the development of signs of heart failure, rather than coronary incidents. When diagnosing acute coronary syndrome (ACS), ST-T changes against the background of a large amplitude of the QRS complex are more likely to indicate it, i.e. ACS, absent [13]. In our material, in 43% of cases in the presence of voltage criteria for LVH, there are changes in the final part of the ventricular complex of the LV SUI type. Only in 10.6% of cases such changes in the terminal part of the ventricular complex were not accompanied by voltage signs of hypertrophy. Our HM ECG also revealed in 28.8% of cases depression of the ST segment and negative T waves according to the type of LV SUI in patients with hypertension. Moreover, the degree of its severity, morphological features (horizontal type of depression exceeding 1 mm) and the tendency to increase the degree of depression most often with an increase in rhythm and less often with increases in blood pressure do not allow excluding ECG myocardial ischemia. Modern views on the mechanisms of strain syndrome in patients with hypertension have changed largely due to myocardial scintigraphy and stress echocardiography in such patients. According to photon emission computed tomography with thallium-201, this category of individuals exhibits myocardial perfusion defects in the anterior, apical or inferior walls of the LV during exercise, which disappear at rest. Similar changes in perfusion are also found in individuals without hypertensive syndrome, but who have complaints of chest pain. The widely held point of view that in patients with hypertension and complaints of chest pain there are microvascular disorders of the blood supply, established by myocardial scintigraphy, is not confirmed by CAG studies, which do not detect changes in the coronary arteries [14]. The work [15] shows that both normotensive and hypertensive patients with complaints of heart pain on the ECG during exercise have ischemic ECG changes. At the same time, according to stress echocardiography, no areas of ischemia and disturbances in the movement of the ventricular walls are found. Other authors also indicate the absence of signs of myocardial ischemia according to stress echocardiography with dobutamine in hypertensive patients with a positive ECG response to stress [16]. However, a number of other studies have shown that according to stress echocardiography in patients with hypertension, zones of transient contractility disorders (ischemic in nature) can be identified with intact coronary arteries according to the results of coronary angiography [17]. In our study, a positive ECG response to stress in hypertensive patients with intact coronary vessels during stress echocardiography was also not accompanied by impaired myocardial contractility.
With stress echocardiography, there is no dependence of local myocardial contractility on the presence or absence of LVH in hypertensive and nonhypertensive patients. As a rule, neither one nor the other exhibits local contractility disorders [14, 18]. It should be noted that, according to our data, ST depression during stress echocardiography often accompanied cases with a pronounced increase in SBP without impaired local contractility of the LV myocardium, which indicates the possibility of developing LV SUI. With an isolated increase in DBP, such a pattern was not observed. The sensitivity and specificity of stress echocardiography, according to the literature, is higher in cases of hemodynamically significant lesions of the coronary arteries [19]. With stenosis of small coronary arteries (diameter less than 2.6 mm), the sensitivity of stress echocardiography is slightly reduced [17]. Constriction of prearterioles in patients with ST depression and clear coronary arteries can lead to the development of small focal ischemic foci, which are more difficult to detect with stress echocardiography, but are determined by myocardial scintigraphy [20]. A negative result of stress echocardiography is associated not only with the small size of ischemic foci, but also with the restraining effect of adjacent non-ischemic segments, which can cause inward passive systolic motion of the LV walls [20]. Despite the absence of stenosis in the large epicardial arteries, myocardial perfusion disturbances are found in hypertensive patients, especially if they have LVH [21]. It should be noted that the mechanism of myocardial ischemia is multifaceted and consists of several factors: 1) damage to the epicardial coronary arteries; 2) reduction of coronary reserve, especially with LVH; 3) damage to the microvasculature [21]. In our study, there is not always a connection between the presence of LVH criteria and changes in ST-T on the resting ECG, which indicates, first of all, that the presence of LVH is not found in all hypertensive patients and LVH itself does not always lead to changes in the repolarization phase. Similar data were obtained in a number of works [15, 18]. The influence of relative coronary insufficiency in LVH on ST-T changes is still being discussed [22]. However, there are studies in which the authors do not find a connection between a decrease in coronary reserve and the severity of LVH [23, 24]. According to our previously published data [25], in deceased patients with malignant hypertension and no signs of coronary artery disease, along with a significant increase in heart mass, there was a proportional increase in the diameter of the coronary arteries.
It follows from this that myocardial hypertrophy and increased extravascular compression are not the only mechanisms for the development of microvascular dysfunction and myocardial perfusion disorders in patients with hypertension. Structural or functional changes in the coronary microcirculation can lead to arterial wall resistance [26, 27]. Moreover, with myocardial hypertrophy, due to an increase in the diameter of cardiomyocytes, the ratio of intracellular to extracellular volume becomes greater, which leads to a decrease in the number of capillaries per 1 mm2 of myocardial cross-sectional area. Capillary rarefaction during LVH in patients with hypertension underlies functional and structural changes in microvascularization [28]. This is facilitated by disruption of endothelium-dependent vascular relaxation in coronary resistance vessels. Endothelial dysfunction causes inhomogeneous myocardial perfusion [29–32].
Conclusion
In patients with moderate hypertension, compared with patients with “mild” hypertension, voltage criteria for LVH and LV SUI are significantly more often detected.
In CM patients with moderate hypertension, ST depression is permanent. The worsening of ST depression against this background in 60.5% of cases is associated with an increase in heart rate. In patients with “mild” hypertension, ST depression is transient and rhythm-dependent. Classical ECG criteria for myocardial ischemia identified by HM ECG do not appear to be associated with damage to the large coronary arteries. The ischemic type of changes in the ST segment during stress echocardiography most often manifests itself with a pronounced increase in SBP. Perhaps this is a manifestation of strain syndrome of the LV myocardium.
How does depression develop?
Recent research in the field of st segment depression has helped to compose three options for the development of anxiety and arterial hypertension:
The National Heart Center conducted a number of studies. In patients with arterial hypertension, an increased degree of anxiety was observed and there was a high risk of depression when the patient changed his group from the first to the third.
After analyzing the medical records of inpatients, we found that doctors could have made mistakes when prescribing treatment for patients with hypertension. Due to the fact that attention was paid to the patient's anxiety extremely rarely, the ability of antihypertensive drugs to resist the disease fell further and further. While taking medication to suppress the agitated state of the brain, which was rarely consulted by doctors, blood pressure returned to normal. Naturally, as soon as the medicine was stopped, the disease returned.
First, let's recap the possible symptoms of ST segment depression:
How is st shown on an ecg?
Potassium deficiency is detected on the cardiogram by a pronounced U wave with ST segment depression.
Atrial repolarization is noted in leads avf, 3, 2 with a decrease in st. The same situation can be seen with pulmonary emphysema.
It is not always possible to see such a disease based on clinical symptoms. It is rarely possible to detect pathology during a medical examination. A symptom can be called pain, the source of which is located behind the sternum.
A healthy person has no pathologies, because his heart responds adequately to increased load. With physical activity, arterial hypertension decreases, in rare cases increasing systolic pressure.
ST segment depression: causes and treatment methods
A downward displacement of the ST segment relative to the isoelectric line (depression) is a reason for a more detailed examination of the patient, since the presence of such a change allows one to suspect ischemia of the heart muscle.
It should be remembered that analysis of this segment alone in isolation from the overall picture of the electrocardiogram is not informative enough. A correct conclusion is possible only after a comprehensive detailed analysis of the recording in all leads.
A segment on a cardiogram is a section of the curve located between adjacent teeth. The ST segment is located between the negative S wave and the T wave.
The ST segment is a part of the electrocardiogram waveform that reflects the period during which both ventricles of the heart are fully involved in the excitation process.
The duration of the ST segment on the ECG depends on the heart rate and changes with it (the higher the heart rate, the shorter the duration of this section on the cardiogram).
Each section of the electrocardiographic curve has its own diagnostic value:
Element
Meaning
The same shape and size of a positive P wave and its presence before each QRS complex is an indicator of normal sinus rhythm, the source of excitation in which is localized in the atrio-sinus node. With a pathological rhythm, the P wave is modified or absent
Determined by the process of excitation of the interventricular septum (depolarization of the interventricular septum)
Reflects the excitation of the apex of the heart and the adjacent areas of the heart muscle (depolarization of the main part of the ventricular myocardium) in leads v 4, 5, 6, and in leads v1 and v2 - reflects the process of excitation of the interventricular septum
It is a reflection of the excitation of the interventricular septum adjacent to the atria (basal) (depolarization of the base of the heart). On a normal electrocardiogram it is negative, its depth and duration increase with complete blockade of the left bundle branch, as well as the anterior branch of the left bundle branch.
Is a manifestation of the processes of repolarization of the ventricular myocardium
An unstable element of the electrocardiographic curve, recorded after the T wave and appearing due to short-term hyperexcitability of the ventricular myocardium after their repolarization
The duration of this interval indicates the speed of electrical impulse transmission from the atrial myocardium to the cardiac muscle of the ventricles of the heart.
Displays the progress of the process of distribution of excitation throughout the ventricular myocardium. Lengthens with right bundle branch block
Reflects the saturation of myocardial cells with oxygen. Changes in the ST segment indicate oxygen starvation (hypoxia, ischemia) of the myocardium
Conducting electrical impulses; an increase in the duration of the segment indicates a disruption in the conduction of impulses along the atrioventricular pathway
This interval reflects the process of excitation of all parts of the ventricles of the heart; it is commonly called electrical ventricular systole. Prolongation of this interval indicates a slowdown in impulse conduction through the atrioventricular junction
On a normal cardiogram in the limb leads, the ST segment has a horizontal direction and is located on the isoelectric line. However, its position is also recognized as a variant of the norm, slightly above the isoelectric line (one and a half to two cells). This picture on the electrocardiogram is often combined with an increase in the amplitude of the positive T wave.
When analyzing an electrocardiogram, the greatest attention is paid to this segment when coronary heart disease is suspected and when diagnosing this disease, since this section of the curve is a reflection of oxygen deficiency in the heart muscle. Thus, this segment reflects the degree of myocardial ischemia.
The conclusion about ST segment depression is made when it is located below the isoelectric line.
The descent of the ST segment below the isoline (its depression) can also be recorded on the cardiogram of a healthy person; in this case, the position of the electrocardiogram curve in the ST segment does not fall below half a millimeter of the isoelectric line.
When analyzing an electrocardiogram, it is necessary to take into account that modifications of some of its elements can be caused by medications that the patient is taking, as well as deviations in the electrolyte composition of the blood.
Downward displacement of the ST segment relative to the isoelectric line is a nonspecific sign. This electrocardiographic phenomenon is observed in various leads in a number of conditions:
A change in the ST-T complex in the form of its displacement down relative to the isoelectric line can be caused by a complex of reasons. For example, in a patient with myocardial hypertrophy (of any origin) and receiving therapy in the form of cardiac glycosides, there is a possibility of acute subendocardial ischemia.
Detection of ST segment depression is the reason for a thorough analysis of the electrocardiogram recording in all leads for a more accurate diagnosis of the location of the lesion.
In typical cases, myocardial ischemia (hypoxia) is manifested by pressing pain, discomfort, and burning in the chest area. Irradiation of pain to the back and left upper limb is typical. A painless form of myocardial ischemia is also possible, manifested by feelings of discomfort in the chest space, tachycardia, a decrease or increase in blood pressure, heartburn, and shortness of breath.
In the differential diagnosis of ischemic myocardial damage with VSD, the features of the clinical picture are taken into account: vegetative-vascular dystonia is characterized by ST depression in a young patient, more often in women, against the background of an increase in heart rate, in the absence of symptoms typical of angina pectoris. In this case, changes in the electrocardiogram are regarded as “nonspecific” or as “signs of increased influence of the sympathetic nervous system.”
With transient ischemia, Holter monitoring (recording an ECG during the day) helps make a diagnosis. The Holter displays all episodes of oxygen starvation of the heart muscle of patients that occurred during the day.
In order for treatment to be effective, it is necessary to act directly on the cause of hypoxia, which is determined using special examination methods. Possible reasons are:
When treating myocardial ischemia, complex therapeutic regimens are used, consisting of the following drugs described in the table:
neurofob.com
What does ST segment depression mean in an electrocardiogram?
- July 23, 2018
- Psychiatry
- Evdokimova Irina
Sometimes in the transcript of the electrocardiogram the doctor writes about ST-segment depression. In some cases, this is a sign of pathology, but it can also be a normal variant. Patients do not always understand this term, so you should understand in more detail the reasons for this ECG result.
What is the ST segment?
An ECG shows the electrical processes that occur in the heart muscle during contraction and relaxation. If you look at the result of the study, you can see a line with many teeth. A straight segment is called an isoline, and the distance between two adjacent teeth is called a segment.
The ST segment represents the interval from the end of the S wave to the beginning of the T wave. This segment shows the state of the heart muscle at the time of contraction of both ventricles. Normally, the segment lies completely on the isoline and does not deviate from it. If the segment is located below the isoline, then doctors talk about depression of the ST segment.
Does this indicate a dangerous heart pathology? It all depends on the degree and type of segment decline. The electrocardiograph records the examination results on checkered paper.
If the ST segment is located no more than half a cell below the isoline, then this is a variant of the norm and occurs in healthy people. This result is considered acceptable in both precordial and limb leads.
A stronger decrease in the segment may indicate cardiac pathology.
Why is the ST segment reduced?
The causes of ST segment depression are divided into coronary and non-coronary. Coronary causes include conditions associated with insufficient blood supply (ischemia) to the heart muscle. These are different types of coronary heart disease and myocardial infarction. Non-coronary causes include:
- lack of potassium in the body (hypokalemia);
- secondary myocardial lesions in non-cardiac pathology;
- paroxysmal supraventricular tachycardia (ST segment depression can be up to 8 mm);
- taking certain medications (cardiac glycosides, antiarrhythmics, phenothiazines);
- hypertrophy of the left ventricle of the heart;
- vegetative dystonia;
- mitral valve prolapse;
- emotional stress;
- intense breathing (hyperventilation).
Types of segment reduction
When making a diagnosis based on electrocardiogram results, the type of ST segment depression must be taken into account. In cardiology, there are several types of such deviations:
- oblique;
- oblique;
- horizontal.
Oblique and horizontal depressions may indicate the presence of cardiac pathology. An oblique decline sometimes occurs in healthy people.
Oblique and horizontal type of decline
If the segment between the teeth is an oblique line directed downwards, then in this case they speak of oblique depression of the ST segment. Such electrocardiogram readings are considered pathological. This indicates myocardial ischemia. Another reason for this result may be left ventricular failure.
https://www.youtube.com/watch?v=-Ru4g_VXwko
A sign of insufficient blood supply to the heart muscle is horizontal depression of the ST segment. What it is? The segment between the S and T teeth is parallel to the isoline. This ECG result is also a marker of ischemia.
The status of the ST segment is checked in two adjacent leads. That is, the electrodes of the cardiograph are connected to two points located nearby, on the chest or on the limbs. And if a decrease in the segment was detected twice, then this, as a rule, indicates ischemia.
Oblique descent type
Oblique ST-segment depression is a deviation in the electrocardiogram when the line between the teeth is directed upward. This usually happens with tachycardia. This phenomenon may be temporary, for example when your heart rate increases after exercise. In this case, changes in the electrocardiogram do not indicate pathology.
But if a high T wave is observed on the electrocardiogram along with oblique ST segment depression, this may indicate a disease. This ECG result occurs in the acute stage of myocardial infarction, with left ventricular hypertrophy, hyperkalemia.
Why do an ECG?
Analysis of the state of the CT segment in the electrocardiogram remains a very relevant method of modern diagnostics. Using an ECG, you can detect cardiac pathologies in the early stages and begin their therapy. Therapeutic practice shows that the treatment and prognosis of many of these diseases depend on the stage of pathology at which they are diagnosed.
Timely diagnosis of cardiac pathologies will protect against serious complications
It is possible to assess how strongly the CT segment has shifted only in combination with other cardiac parameters. Depression or elevation in itself does not necessarily indicate pathology; it may be part of the norm.
When considering the results of electrocardiography, one cannot ignore the symptoms that appear. Displacement of the CT segment may be associated with non-coronarogenic changes in the myocardium.
Important! In rare cases, segment displacement may be a sign of acute coronary syndrome. This requires emergency medical attention.
Features of treatment and prognosis
To confirm the diagnosis, additional examinations are necessary. You will have to tell your doctor about any medications you are taking: medications can affect heart function. Blood samples must be provided for analysis. If there are blood clotting disorders, you should also tell your doctor about them. Conduct studies of the coronary arteries. Holter monitoring may be required. Assess the condition of the lungs and sinus rhythm. In addition, pay attention to concomitant symptoms and the general clinical picture.
Treatment depends on the cause. If myocardial ischemia is noted, antiplatelet agents, nitrates, adrenergic blockers, and statins are prescribed. If medications are not effective enough, surgical methods of intervention are used: coronary artery stenting, coronary artery bypass grafting. You should reduce body weight if you are overweight, walk in the fresh air more often, exclude foods with a lot of fat and sugar, and give preference to natural foods.
With VSD, it is necessary to normalize the state of the nervous system. Prescribe the amino acid Glycine to get rid of the neurotic component. In addition, doctors often prescribe nootropic and sedatives. Corvalol and potassium supplements may be prescribed. In addition, you should give up bad habits (smoking, drinking alcohol), normalize your diet, follow a drinking regime, avoid stress, and get enough rest.
The doctor must decide what to do. Self-medication is unacceptable, because it may lead to undesirable consequences.
Prevention methods include a healthy lifestyle. In addition, you should regularly visit doctors to promptly detect emerging pathologies and treat them. The prognosis is more favorable if there is a mild form of pathology.
General information about segment offset
When a person is healthy, his ECG is normal. Elevation of the st segment (rise) or decrease may indicate pathologies within the body. Normally, the st segment is located on an isoline, although there is a certain range of acceptable values.
ST depression is acceptable in limb leads up to 0.5 mm. Indicators greater than or equal to 0.5 in leads V1-V2, 0.5 are considered a deviation.
St segment elevation in the limb leads should be less than 1 mm. For leads V1-V2, the norm is up to 3 mm, and for V5-V6 – up to 2 mm.
Where does this information apply?
Knowing the norm of st segment elevation on an ECG helps in diagnosing some serious cardiac pathologies: myocardial infarction, coronary heart disease, myocardial hypertrophy, LV aneurysm, pericarditis, myocarditis, PE, etc.
Thus, during heart attacks there is no decrease in the st segment. This indicator can increase to 2-3 mm when the norm is up to 1. In addition to the growth of the CT segment, a pathological Q wave may appear on the electrocardiogram picture.
It is effective to use a troponin test when a heart attack is suspected. When a significant displacement of the CT segment occurs, the latest analysis allows us to clarify the diagnosis. If the test is negative, the patient has not had a heart attack, and acute ischemic disease requires treatment.
Recommendations for interpreting electrocardiograms
To correctly establish a diagnosis and prescribe effective treatment, it is important for a cardiologist to carefully read the electrocardiogram. There are some rules, taking into account which you can help the patient efficiently.
How he reads the ECG and what treatment he chooses depends on the experience of the cardiologist.
First of all, the ability of the heart to conduct electrical impulses is analyzed. The frequency and rhythm of the pulse are calculated, and the regularity of heart contractions is assessed. The cardiologist then pays attention to the work of the pacemaker and determines how well the impulses travel along the conduction pathways of the heart.
After these studies, the cardiologist evaluates the position of the electrical axis and examines the rotation of the heart around the longitudinal, transverse and anteroposterior axis. At the same stage, the P wave is assessed.
The next stage of deciphering the electrocardiogram is to consider the state of the QRS-T complex. When assessing the ST segment, the J point (the moment the S wave transitions to the ST segment) is important.
The shape of the arc that the J point forms to the end of the ST segment determines the presence of pathology. If it is concave, then the deviation is benign. Convex is a sign of myocardial ischemia.
ST segment: what is it and what is it responsible for
In electrocardiography of the heart, a segment is the portion of the curve located between adjacent teeth. The ST segment is located between points S and T. The S wave should always be located below the isoelectric line (it is negative), the T wave is most often located above (positive). The condition of the site needs to be assessed holistically; Most often, this segment of the graph can be used to determine how well oxygen saturates the myocardium.
A post shared by LEGAL PSYCHOLOGIST (@alenushkalen) on Apr 3, 2019 at 12:17am PDT
The size of the area under study can be different: the more frequent a person’s heartbeats, the shorter it is. Reflects the period when both ventricles are in an excited state. The area must be horizontal. Most often it is located approximately at the level of the isoelectric line, but in rare cases it can be located slightly higher, which is also considered a variant of the norm.
Causes of cardiac changes
Myocardial infarction and other serious cardiovascular pathologies do not develop overnight. Perhaps the person neglected the alarming symptoms for some time, or did not follow the recommendations of the attending physician. Some did not take such a diagnosis as coronary artery disease seriously, underestimating the risks of the pathology.
Abnormalities in electrocardiogram results may appear for various reasons. Most often, this study provides a reliable picture of the work of the heart muscle. Although errors do occur, they are very rare.
Important! ST segment depression symptoms sometimes appear even in healthy people. If, in addition to changes in the ECG, there are no negative symptoms, we can talk about the physiological norm. Although periodic visits to a cardiologist and monitoring of heart condition should not be neglected.
Deviations from the norm in the electrocardiogram picture may appear if the procedure is performed incorrectly. This situation is possible if the electrodes are applied incorrectly. In this case, there is not enough contact, and the device records unreliable data.
Other non-cardiac causes of ECG abnormalities:
The development of any pathology can be stopped subject to timely diagnosis and proper treatment. To do this, if the slightest unpleasant symptoms appear in the heart area, it is recommended to visit a therapist to get a referral for examination. This way you can prevent the development of serious and dangerous pathologies.
lechiserdce.ru
Nonspecific depression
A decrease in the distance between the S and T waves is not always associated with coronary heart disease. This can be observed both normally and in conditions where the blood supply to the myocardium is not impaired. Typically, such a decrease is caused by non-coronary causes. In this case, doctors talk about nonspecific ST-segment depression.
Such changes in the electrocardiogram can be observed under the following conditions:
- mitral valve prolapse;
- taking cardiac glycosides, diuretics, psychotropic drugs (the ST segment has a trough-shaped shape);
- vegetative-vascular dystonia;
- left ventricular hypertrophy;
- hypokalemia;
- tachycardia;
- cardiac conduction disorders;
- hyperventilation;
- inflammation of the pancreas;
- water and electrolyte disturbances;
- Wolff-Parkinson-White syndrome (a disease with periodic attacks of tachycardia).
In some cases, there are mixed causes of ST segment depression. For example, a patient may suffer from left ventricular hypertrophy and at the same time use cardiac glycosides. This can lead to the development of myocardial ischemia.
How to determine if you have depression?
- Communication with such a person often comes down to discussing his past problems. The patient’s speech itself is slowed down, and the formulation of ideas becomes a difficult task for him.
- During the examination, patients look at the light or out the window. Gestures are directed towards oneself, hands are pressed to the chest. During anxious depression, the hands are pressed to the throat, a Veragut fold is observed in facial expressions, and the corners of the mouth are lowered. When manipulating objects, actions will be fussy. The voice becomes lower and quieter, long pauses appear between each word, and low directiveness is noted.
Such reasons can indirectly confirm the diagnosis of st interval depression:
- Tachycardia.
- Constipation.
- The brittleness of nails and hair is significantly increased.
- Due to cravings for foods rich in carbohydrates, weight may increase uncontrollably.
What can cause depression?
When making a diagnosis, the doctor is based on the reasons given by the patient. But you should always check for possible mental disorders. With such violations, the clinical picture will be disrupted.
In current realities, st depression and arterial hypertension should be monitored by both a psychiatrist and a cardiologist. Naturally, it is important that the patient himself participates in the course of treatment, because it is he who uses the drugs and follows the regimen that the doctor prescribed for him.
Depression of the heart - what is it?
Analysis of the state of the CT segment in the electrocardiogram remains a very relevant method of modern diagnostics. Using an ECG, you can detect cardiac pathologies in the early stages and begin their therapy. Therapeutic practice shows that the treatment and prognosis of many of these diseases depend on the stage of pathology at which they are diagnosed.
Timely diagnosis of cardiac pathologies will protect against serious complications
It is possible to assess how strongly the CT segment has shifted only in combination with other cardiac parameters. Depression or elevation in itself does not necessarily indicate pathology; it may be part of the norm.
When considering the results of electrocardiography, one cannot ignore the symptoms that appear. Displacement of the CT segment may be associated with non-coronarogenic changes in the myocardium.
How to determine if you have depression?
- Reduced concentration and attention are manifested in difficulty memorizing and low academic performance.
Physical activity is also significantly reduced, to the point of stupor, which may be considered laziness. Adolescent and childhood depression is often accompanied by aggressive attacks and increased conflict, which hide self-hatred. - The mood becomes better in the evening. Self-confidence disappears and self-esteem decreases.
Due to these feelings, the patient moves away from society and strengthens his emerging feeling of inferiority. Long periods of depression in patients over 50 years of age are accompanied by deprivation and a clinical picture that is similar to dementia.Constant gloomy thoughts, a pessimistic attitude, an increasing sense of guilt, self-deprecation - a familiar state? It is this that is most often shown in all films, associating it with the depression of the Art. segment. And the patient, just like in all such films, thinks about causing harm to himself, or even comes to thoughts of suicide.
- The patient begins to sleep poorly, may have nightmares, and finds it very difficult to get up in the morning. Appetite worsens, and there is a frequent preference for carbohydrate foods over protein foods. The desire to eat may appear in the evening. A person in a state of depression has a distorted sense of time: for him it lasts a very long time.
- Another important sign is a reluctance to take care of oneself, which leads to an extremely sloppy appearance, at a minimum.
- Communication with such a person often comes down to discussing his past problems. The patient’s speech itself is slowed down, and the formulation of ideas becomes a difficult task for him.
- During the examination, patients look at the light or out the window. Gestures are directed towards oneself, hands are pressed to the chest. During anxious depression, the hands are pressed to the throat, a Veragut fold is observed in facial expressions, and the corners of the mouth are lowered. When manipulating objects, actions will be fussy. The voice becomes lower and quieter, long pauses appear between each word, and low directiveness is noted.
Such reasons can indirectly confirm the diagnosis of st interval depression:
- Dilated pupils.
- Tachycardia.
- Constipation.
- Reduced elasticity of the skin, it becomes flabby.
- The brittleness of nails and hair is significantly increased.
- The patient seems much older than his years.
- Due to cravings for foods rich in carbohydrates, weight may increase uncontrollably.
- Sexual desire increases, because this reduces the level of anxiety.
General information about segment offset
When a person is healthy, his ECG is normal. Elevation of the st segment (rise) or decrease may indicate pathologies within the body. Normally, the st segment is located on an isoline, although there is a certain range of acceptable values.
ST depression is acceptable in limb leads up to 0.5 mm. Indicators greater than or equal to 0.5 in leads V1-V2, 0.5 are considered a deviation.
St segment elevation in the limb leads should be less than 1 mm. For leads V1-V2, the norm is up to 3 mm, and for V5-V6 – up to 2 mm.
The cardiogram is analyzed only by a doctor
Knowing the norm of st segment elevation on an ECG helps in diagnosing some serious cardiac pathologies: myocardial infarction, coronary heart disease, myocardial hypertrophy, LV aneurysm, pericarditis, myocarditis, PE, etc.
Thus, during heart attacks there is no decrease in the st segment. This indicator can increase to 2-3 mm when the norm is up to 1. In addition to the growth of the CT segment, a pathological Q wave may appear on the electrocardiogram picture.
It is effective to use a troponin test when a heart attack is suspected. When a significant displacement of the CT segment occurs, the latest analysis allows us to clarify the diagnosis. If the test is negative, the patient has not had a heart attack, and acute ischemic disease requires treatment.
It is not always possible to see such a disease based on clinical symptoms. It is rarely possible to detect pathology during a medical examination. A symptom can be called pain, the source of which is located behind the sternum.
If it is present, the doctor carefully examines the source of pain, using the Metelitsa classification:
- No pain in the pit of my stomach.
- Physical activity is accompanied by pain in the chest.
- Pain in the pit of the stomach, which makes physical activity impossible.
- Pain that dissipates with Nitroglycerin.
Additional visual characteristics of the diagnosis are cold sweat and skin, its blueness, rapid breathing, and muscle fatigue.
To assess the ability of the heart muscle to respond to an increase in contraction frequency, tests using physical activity must be performed.
A healthy person has no pathologies, because his heart responds adequately to increased load. With physical activity, arterial hypertension decreases, in rare cases increasing systolic pressure.
In the presence of a previous myocardial infarction, myocardial ischemia is called an important reason for low blood pressure. With pathologically frequent contractions of the heart, reduced functional cardiac capabilities indicate ventricular dysfunction. This situation occurs when using cardiotropic drugs.
What can cause depression?
- At the genetic level, depression ct is caused by a pathology of the eleventh chromosome.
- With the biochemical path of development of this diagnosis, the exchange of catecholamines and serotonin is complicated.
- Neuroendocrine development manifests itself when the rhythm of the pituitary gland, hypothalamus and limbic system, as well as the pineal gland is disrupted, which is why the level of production of releasing hormones and melatonin is reduced. Daylight is involved in the creation of these hormones - the less of it, the worse the production.
- Between the ages of twenty and forty, there are increased spikes in depression.
- A sharp decline in a person's social class.
- Presence of suicide in the family.
- Loss of loved ones and relatives in adolescents over eleven years of age.
- The risk group includes people with increased conscientiousness, diligence and anxiety.
- Naturally, stressful events and problems with satisfying sexual desires also lead to depression.
- Some doctors add homosexuality and the period after childbirth to this.
How does depression develop?
Recent research in the field of st segment depression has helped to compose three options for the development of anxiety and arterial hypertension:
- Due to somatovegetative disorders, depression begins and hypertension additionally develops. Due to increased nerve impulses, pressure increases in the smooth muscles of peripheral vessels. In this option, neurocircular dystonia or hypertension is treated, but the initial alarming factor remains unknown.
- Arterial hypertension develops, and only then anxiety depression is added. This disease is considered a more dangerous form for treatment. Using electrocardiography, the brain component can be identified, which will allow the diagnosis of the disease.
- In the third and final version, depression manifests itself as a complication of arterial hypertension. Due to increased symptoms, hypertension and depression, unique clinical pathologies arise, which allows for accurate diagnosis.
The National Heart Center conducted a number of studies. In patients with arterial hypertension, an increased degree of anxiety was observed and there was a high risk of depression when the patient changed his group from the first to the third.
After analyzing the medical records of inpatients, we found that doctors could have made mistakes when prescribing treatment for patients with hypertension. Due to the fact that attention was paid to the patient's anxiety extremely rarely, the ability of antihypertensive drugs to resist the disease fell further and further.
When making a diagnosis, the doctor is based on the reasons given by the patient. But you should always check for possible mental disorders. With such violations, the clinical picture will be disrupted.
In current realities, st depression and arterial hypertension should be monitored by both a psychiatrist and a cardiologist. Naturally, it is important that the patient himself participates in the course of treatment, because it is he who uses the drugs and follows the regimen that the doctor prescribed for him.
Recommendations for interpreting electrocardiograms
To correctly establish a diagnosis and prescribe effective treatment, it is important for a cardiologist to carefully read the electrocardiogram. There are some rules, taking into account which you can help the patient efficiently.
How he reads the ECG and what treatment he chooses depends on the experience of the cardiologist.
First of all, the ability of the heart to conduct electrical impulses is analyzed. The frequency and rhythm of the pulse are calculated, and the regularity of heart contractions is assessed. The cardiologist then pays attention to the work of the pacemaker and determines how well the impulses travel along the conduction pathways of the heart.
After these studies, the cardiologist evaluates the position of the electrical axis and examines the rotation of the heart around the longitudinal, transverse and anteroposterior axis. At the same stage, the P wave is assessed.
The next stage of deciphering the electrocardiogram is to consider the state of the QRS-T complex. When assessing the ST segment, the J point (the moment the S wave transitions to the ST segment) is important.
The shape of the arc that the J point forms to the end of the ST segment determines the presence of pathology. If it is concave, then the deviation is benign. Convex is a sign of myocardial ischemia.
How to analyze the causes of depression?
Let's explain the rules that doctors use when observing the electrocardiogram of a patient suffering from coronary artery disease: