Selective serotonin and norepinephrine reuptake inhibitors, according to their pharmacokinetic properties, belong to the third generation of antidepressants. Used in the treatment of anxiety disorders and depressive conditions. The body tolerates taking such drugs relatively easily, so some of them are available without prescriptions.
Differing from the TCA group (tricyclic antidepressants), the selective blocker practically does not provoke anticholinergic/cholinergic side effects, only occasionally causing sedation and orthostatic hypotension. In case of overdose of the described drugs, the risk of cardiotoxic effects is lower, therefore such antidepressants are used in many countries.
A selective approach to treatment is justified by the use of SSRIs in general medical practice; they are often prescribed for outpatient treatment. A non-selective antidepressant (tricyclic) can cause arrhythmia, while selective inhibitors are indicated for chronic heart rhythm disturbances, angle-closure glaucoma, etc.
Classification of antidepressants
Depression has been known to mankind since time immemorial, as have ways to overcome it.
In ancient Rome, the famous physician Soranus of Ephesus used lithium salts to treat them, for example. Cannabis, opium, barbiturates, amphetamines are all numerous attempts to chemically manipulate the body to help people cope with emotional exhaustion. The first drug to combat depression was Imipramine, which was synthesized in 1948. To date, many antidepressants , which are currently classified. Depending on the general picture of the manifestation of the mental processes of patients:
- Thymiretics are used for depressed and depressed states;
- thymoleptics have a calming effect, so they are used when there is increased mental arousal.
According to their biochemical effects on the body, antidepressants are :
- non-selective action (for example, Melipramine, Amizol),
- selective action: blocking serotonin uptake (for example, Sertraline), blocking norepinephrine uptake (for example, Reboxetine),
- inhibition of monoamine oxidase: non-selective action (for example, Transamine), selective action (for example, Autorix).
There are other pharmacological groups of drugs against depression.
How do antidepressants work?
Antidepressants are able to control some processes that occur in brain cells. This organ consists of a huge number of nerve cells. The body and processes are the components of neurons. They transmit impulses between themselves using processes and through the synapse (the space that is located between two neurons).
Antidepressants were discovered by accident while testing drugs against tuberculosis
This space is filled with a special substance (mediator), through which information is transmitted from one neuron to another. About 30 mediators are currently known in biochemistry. But depressive states are associated, as a rule, with only three hormones that function as neurotransmitters: serotonin, dopamine, norepinephrine. The mechanism of action of antidepressants is aimed at regulating the concentration of these hormones in the brain and correcting its functioning, impaired as a result of depression.
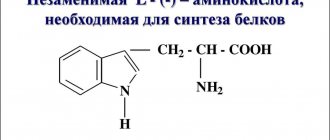
What is serotonin
Serotonin is one of the main neurotransmitters in the body. This is the name for biologically active substances that are formed as a result of certain reactions from amino acids, and whose task is to transmit nerve impulses between two cells (neurons). The transmission of such signals is carried out electrically during the transition of ions from one neuron to another.
Serotonin is produced in one of the parts of the brain, the pineal gland, and controls the functioning of the central nervous system. This makes it possible for the neurotransmitter to control many processes occurring in the human body (serotonin receptors are located not only throughout the nervous system of the body, but are also located on the walls of blood vessels in the digestive system, on the smooth muscles of the bronchi).
Thanks to serotonin, melatonin is formed in the body, which regulates the biological cycle (its deficiency often provokes insomnia). In addition, the neurotransmitter is responsible for regulating a person’s emotional state, preventing psycho-emotional disorders, creating a feeling of happiness and pleasure.
It is also responsible for the production of hormones, normalizes sexual function, takes an active part in preparing the female body for childbirth, promotes blood clotting, normal functioning of the gastrointestinal tract, and regulates brain function.
A deficiency, like an excess of serotonin, affects a person extremely negatively. The lack of a neurotransmitter makes it more sensitive to pain, the biological rhythm is disrupted, the state of the nervous system worsens, resulting in depression, obsessive disorders, and severe forms of migraine. Excess leads to hallucinations and schizophrenia.
To get a person out of this state and normalize the amount of serotonin, various antidepressants and psychotropic medications are used, the main purpose of which is to treat various forms of depression.
Such medications have no particular effect on a healthy person, whereas after a course of therapy in a person suffering from depression, they improve mood, reduce or completely eliminate anxiety, apathy, melancholy, and emotional stress. This leads to psychological stability, normalization of biological rhythm, stabilization of sleep, and improvement of appetite.
What are SSRIs
In modern medical practice, the most popular drugs are the third generation - selective serotonin reuptake inhibitors. These drugs differ from traditional tricyclic drugs for depression by having fewer side effects and being more effective.
With an overdose of these drugs, virtually no cardiotoxic effect is observed. SSRIs are recommended for patients who have contraindications to the use of conventional antidepressants (for example, closed glaucoma, cardiac arrhythmias).
How the drugs work
One of the reasons for the manifestation of depressive states is a decrease in the concentration of serotonin in the brain . This important neurotransmitter, hormone is called the hormone of happiness, joy, pleasure. Moreover, its normal concentration provides a long-lasting, stable feeling of quiet happiness and harmony.
A serotonin reuptake inhibitor works to increase the concentration of the hormone serotonin in the brain . The active ingredients of this antidepressant selectively block (inhibit) serotonin in the brain. This process occurs directly at the synapse. That is, the reuptake of the hormone by the adhesive does not occur; this process is prevented by the drug.
Serotonin remains in place, so the circulation of nerve impulses continues. They activate cells that are suppressed by depression , softening its manifestation. The advantage of drugs in this group is that the dosage is immediately determined by the attending physician; there is no need to increase it, since the additional therapeutic effect does not depend on it.
When using a group of inhibitors, there is no point in monitoring the concentration of serotonin in the blood. An exception may be some diseases of patients, due to which the elimination of drugs from the body slows down.
How it works: antidepressants
- about the author
- Recent publications
Daria Shipacheva
Text writer. Medical geek. Yoga trainer
Daria Shipacheva recently published (see all)
- How it works: learning and memory - 10.26.2018 11:45
- How it works: light therapy - 09.28.2018 10:04
- How it works: testing the DVR/radar detector Neoline X-COP 9700s - 08/28/2018 15:10
In the “How it works” section, we consider well-known phenomena, discoveries and inventions from the point of view of science - and talk about complex research in simple words. The coldest month of winter is a good time to talk about depression and antidepressants
According to statistics, depression and anxiety disorders affect 17-20% of people at least once in their lives. Residents of large cities are in particular danger, constantly experiencing exorbitant loads and inhuman stress. Antidepressants are used to treat depression and anxiety. First of all, selective serotonin reuptake inhibitors (SSRIs). Many people refuse to drink them for fear of side effects and fear of getting hooked, perceiving them as a kind of “drug of happiness.” Let's look at how antidepressants actually affect the brain.
Biological origins of depression
In the 50s of the last century, scientists proposed the first hypothesis about the origin of depression. They noticed that low levels of norepinephrine in the brain (this was observed when taking certain drugs, for example, reserpine, a medicine for hypertension) leads to side effects such as lethargy, apathy and depressed mood. And after taking amphetamine, which increases the level of norepinephrine in the brain, completely opposite symptoms occur - the person becomes energetic and active. Sometimes even too active.
via WikiMedia Commons
In this regard, scientists have suggested that low levels of norepinephrine in the brain lead to depression, and high levels lead to the opposite effect, that is, mania. But later it turned out that norepinephrine is not the only substance that regulates mood. Similar effects—a transition to depression or to mania—were observed when the levels of serotonin and dopamine in the brain decreased or increased, respectively.
It turned out that depression is a complex condition that may be associated with the improper functioning of several neurotransmitters. It was necessary to find a drug that would have a complex effect on the brain. And scientists even managed to invent two such drugs. More precisely, two classes of drugs are tricyclic antidepressants and monoamine oxidase inhibitors (MAOIs).
What's wrong with first generation antidepressants?
Unfortunately, they turned out to have many side effects - precisely due to their complexity and indiscriminate effect on the brain.
Tricyclic antidepressants, in addition to receptors for norepinephrine and serotonin, also act on histamine, cholinergic and adrenergic receptors. Because of this, the drug causes a number of side effects: weight gain, dry mouth, decreased visual acuity, constipation, dizziness, decreased blood pressure (even fainting), drowsiness and lethargy.
MAO inhibitors act somewhat differently, but their activity also causes a lot of side effects. Monoamine oxidase is an enzyme that is involved in the destruction of substances of the monoamine class. Monoamines are serotonin, melatonin, histamine, adrenaline, dopamine and norepinephrine. MAO inhibitors prevent the enzyme from breaking down monoamines, which causes more of them to appear in the brain. There is more serotonin, dopamine and norepinephrine needed by a depressed person - but also more histamine, melatonin and adrenaline. Hence, again, problems with sleep and digestion, dry mouth, dizziness, low blood pressure, weight gain and low libido.
via PixaBay.com
But in the case of MAO inhibitors, this is not even the worst thing. These drugs interact with a substance called tyramine. This causes a strong increase in blood pressure - even death. Therefore, when taking this type of antidepressant, you need to adhere to a strict diet, excluding from it all foods containing tyramine: cheeses, red wine and beer, smoked meats, legumes, caviar and others. In addition, MAO inhibitors react with many medications, which can cause unpredictable side effects.
Since treatment with tricyclic antidepressants and MAO inhibitors caused too many “side effects”, which were sometimes worse than depression itself, a more effective and selective drug had to be invented.
Selective serotonin reuptake inhibitors
Drugs from the SSRI group, as their name suggests, act on serotonin receptors very selectively. Namely, they prevent the reuptake of serotonin by the neurons that produced it. Thanks to this, the concentration of serotonin in the brain increases, and the symptoms of depression gradually go away.
Today, SSRIs are the most common and prescribed antidepressants. This group includes drugs such as fluoxetine (best known under the brand name Prozac), paroxetine (Paxil), sertraline (Zoloft), escitalopram (Cipralex).
via PixaBay.com
Over time, it became clear that SSRIs are not so selective and act indirectly on receptors other than serotonin. Therefore, while taking SSRIs, especially in the first weeks, side effects are also observed. Most often these are nausea, dizziness, drowsiness, digestive disorders and decreased libido. But all this cannot be compared with the “side effects” from drugs of the previous generation. In addition, over time, some of these negative effects disappear.
Medicines from the SSRI group are not interchangeable. Each of them has its own set of indications and side effects, and only a psychiatrist can determine which drug is best suited in each specific case. This is not an easy task, and it is not always possible to find the right medicine the first time.
The agony of choice
So far, scientists have not come up with an analysis that would allow them to choose the appropriate antidepressant. Work in this direction is underway; There are genetic tests that can show which medicine will be absorbed better or worse. But still, the doctor makes a decision mainly on the basis of the patient’s clinical picture, taking into account the possible “side effects” of the drugs.
Often people with depression think that their psychiatrist is prescribing medications at random. Let's find out what doctors actually use when choosing this or that remedy.
Paroxetine
This antidepressant, in addition to its main effect, has some sedative effect. Therefore, paroxetine is used not only to treat depression, but also to combat anxiety disorders. Depression often goes hand in hand with various forms of anxiety and panic attacks. If a person has severe anxiety in addition to depression, paroxetine is the drug of first choice.
via WikiMedia Commons
The disadvantages of paroxetine stem from its advantages - it more often than other drugs leads to such “side effects” as drowsiness, lethargy and dizziness. Paroxetine also reduces libido more than other SSRIs and makes it more difficult to achieve orgasm. In addition, paroxetine has the most severe withdrawal syndrome. For some time after stopping taking the drug, a person may experience nausea, foggy consciousness, a feeling of “currents” throughout the body and other unpleasant symptoms.
Fluoxetine
Unlike paroxetine, this medicine gives a rather stimulating effect. Thanks to this, it is well suited for those whose main problem is apathy. But for those who have anxiety, fluoxetine is not very indicated - it can increase it. Stimulant antidepressants should also not be prescribed to those who have suicidal thoughts: at first, when depression has not yet passed and strength has already appeared, a person may decide to commit suicide.
Compared to other SSRIs, fluoxetine causes minimal disturbances in libido. Another “bonus” of fluoxetine is a decrease in appetite. But many people already lose their appetite due to depression - fluoxetine is not suitable for such people, because it can increase the exhaustion of the body.
Fluoxetine “gains momentum” more slowly than other SSRIs: you will have to wait about four weeks for the first effect (with other drugs in this group, two are usually enough). And in general, it is weaker than all other SSRIs. But fluoxetine takes a long time to be eliminated from the body, so it’s not so scary if a person forgets to take the pill on time. For the same reason, fluoxetine does not have a severe withdrawal syndrome.
Sertraline
This drug is considered optimal in terms of the combination of price, effectiveness and side effects. If the patient does not have any special circumstances or contraindications, he will most likely be prescribed sertraline.
via WikiMedia Commons
It moderately reduces sexual desire, does not greatly increase the risk of weight gain, improves sleep, and has a moderate stimulating effect. And in general it is well tolerated by the body. True, sertraline causes diarrhea more often than other SSRIs.
Escitalopram
This antidepressant begins to work faster than others. Like paroxetine, it helps people with depression accompanied by severe anxiety and has a calming effect. At the same time, escitalopram does not have so many side effects. In particular, it does not increase drowsiness and lethargy as much and causes fewer sexual problems.
The main disadvantage of escitalopram is its high price, which is at least twice the cost of other SSRIs.
SSRI
There is another, improved version of antidepressants - selective serotonin and norepinephrine reuptake inhibitors. As the name suggests, they also act on norepinephrine receptors. Due to this, they should be more powerful than SSRIs, but there is no clear evidence for this.
via PixaBay.com
For example, one of the most popular SSRIs, venlafaxine, turned out to be more effective than fluoxetine. But since fluoxetine is the weakest of the SSRIs, it is not a fact that venlafaxine is superior in effectiveness to other drugs in this group. But venlafaxine costs about the same as most SSRI drugs.
Another SSRI, duloxetine, works no better than other antidepressants and is even less well tolerated than SSRIs (especially compared to escitalopram). Its only bonus is that it is somewhat effective against fibromyalgia, a pain syndrome that often accompanies depression. At the same time, duloxetine is approximately one and a half times more expensive than escitalopram.
Atypical antidepressants
Among them, for example, bupropion - it blocks the reuptake of dopamine and increases the level of norepinephrine. Bupropion may be used with an SSRI for additional stimulant effects.
To treat or not to treat?
Scientists who conducted a large meta-analysis of studies of antidepressants concluded that SSRIs and venlafaxine are effective only for very severe depression. And for patients with moderate to mild depressive symptoms, these pills are no more effective than a placebo. So it makes sense to take antidepressants only when there is no way to “get out” on your own. And this must be determined by a psychiatrist.
via PixaBay.com
However, there is a risk that the effect of SSRI treatment will wear off over time. Between 9 and 57% of patients who take a maintenance dose of an SSRI experience periodic relapses. As a solution, doctors suggest using the lowest dose for maintenance therapy and increasing it when depressive symptoms return.
Not everyone needs constant use of antidepressants, but only people with endogenous recurrent depression - those who have had three or more depressive episodes in a row. Most often, the reason for this is a genetic predisposition to improper functioning of neurotransmitters and their receptors. These patients typically require lifelong support in the form of pills. For other people, a year of taking antidepressants is usually enough to recover and restore the balance of neurotransmitters; so the fear of getting hooked on them is most often not justified.
Cover photo: PixaBay.com
Similar
When are SSRIs prescribed?
Drugs in this group are prescribed for:
- deep depressive disorders;
- stress, panic attacks, neurotic anxiety;
- manias, phobias;
- obsessive-compulsive neuroses;
- bulimia;
- alcoholism;
- chronic pain syndrome;
- emotionally unstable personality disorder.
The effectiveness of treatment largely determines the timeliness of therapeutic measures. For minor manifestations of depressive conditions, there is no significant difference between the effectiveness of treatment with tricyclic antidepressants and SSRIs. But the effectiveness of the latter in the treatment of advanced nervous disorders has been proven by medical practice.
SSRI drugs do not have a therapeutic effect immediately. Depending on the severity of the disease and the individual characteristics of the body, positive dynamics are observed in the second, fifth, and sometimes only the eighth week from the start of taking the medicine.
The daily dosage depends on the rate of elimination of drugs from the body. Most often, the drug is prescribed to be taken once a day, since the half-life of most SSRIs is more than a day.
Restrictions and contraindications
Serotonergic antidepressants should not be taken by persons under the influence of alcohol or drugs.
In case of hypersensitivity to the active substance or minor components, their use is also unacceptable.
Selective drugs are contraindicated for persons with epilepsy, cardiovascular diseases, renal or liver failure.
Most medications are prohibited in childhood. It is unacceptable to combine the use of several antidepressants at once, the pharmacological properties and comparative characteristics of which are similar.
Each type of medication has individual contraindications and restrictions.
Withdrawal syndrome
Within a few days after completion of treatment, the patient may experience a number of unpleasant symptoms - withdrawal syndrome.
It usually goes away on its own after some time, but sometimes the patient may need additional help.
A more pronounced neurotransmitter deficiency syndrome is observed with SSRI drugs that have a short half-life.
Signs of its onset are the following conditions:
- fatigue and weakness,
- headache and dizziness,
- disorientation in space,
- myalgia,
- asthenia,
- nausea accompanied by vomiting,
- stool disorder,
- tremor,
- muscle cramps,
- panic attacks, increased anxiety,
- sleep disturbance,
- mania,
- heart rhythm disturbance.
An interesting fact is that withdrawal symptoms are similar in patients taking medications to treat depression and people using antidepressants to treat anxiety.
To avoid negative manifestations, experts recommend gradually reducing the dosage of the medication used, and then completely stop using it.
The optimal withdrawal period is 4 weeks.
If tranquilizers were taken for one year or more, then the established time period increases.
What SSRIs are not compatible with
The main danger of using SSRI antidepressants is serotonin syndrome.
It is accompanied by muscular, autonomic and mental disorders, which have a high risk of death.
To prevent the syndrome, it is unacceptable to take SSRIs together with MAO inhibitors.
Combinations with the following types of drugs can lead to the same condition:
- tetracyclic antidepressants,
- herbal remedies with the addition of St. John's wort,
- Levodopa,
- antimigraine drugs,
- mood stabilizers,
- atypical antipsychotics.
If you have previously used any medications, you must wait at least two weeks before starting to take an SSRI.
Depending on the type of drug, this period may be changed. Replacing Fluoxetine with Paroxetine requires a break of 2-3 weeks. For older patients, this period increases to 8 weeks.
Side effects
Side effects include some disorders of the digestive system - nausea, vomiting. When using selective serotonin reuptake inhibitors, the following may occur:
- anxiety;
- anxiety;
- dizziness;
- fast fatiguability;
- sleep disturbance;
- sexual disorders.
Reactions to taking blockers depend on the individual characteristics of the body.
If the patient has problems with the liver or kidneys, selective serotonin reuptake inhibitors should be used with caution . Serotonin receptors are located in the human body not only in the brain, but also in the spinal cord. There are many of them in the gastrointestinal tract, respiratory system, and on the walls of blood vessels. When using inhibitors, the above conditions develop, which usually disappear after a month. That is, side effects are observed only in the first stages of taking inhibitors.
Side effects of medications are associated with an increase in the amount of the neurotransmitter serotonin in the brain , which affects mental activity. Medical practice describes cases of the appearance of suicidal thoughts and mania during treatment with inhibitors in adolescents. This manifestation has not been proven in adult patients.
This reaction is individual in nature; among SSRIs, you can choose drugs that do not affect the activation of the psychomotor sphere and have a sedative effect.
If the SSRI regimen involves a high dosage, serotonin syndrome may develop, which causes convulsions, fever, and heart rhythm disturbances. In this case, the drug is discontinued. Third generation antidepressants easily replace each other, so if treatment is not effective, you can choose another drug. If any of the family members used inhibitors and achieved positive results, it makes sense to opt for this drug.
For the treatment of complex mental disorders and chronic depression, SSRIs are prescribed together with other medications, for example, tranquilizers, tricyclic antidepressants. Complex therapy requires strict adherence to the doctor’s recommendations regarding the regimen and dosage of medications. There are known cases of death due to overdose.
SSRI drugs
The list of SSRI drugs is extensive. Today they are in great demand for treating depression, improving mood, and normalizing sleep. These medications are available and sold without prescriptions in online pharmacies. The most common are:
- Paroxetine;
- Fluvoxamine;
- Sertraline;
- Cipramil;
- Fluoxetine.
When choosing a drug, it is worth analyzing the effect of the drug:
| SSRI drugs | Antidepressant effect | Additional therapeutic effect | Manifestation of side effects |
| Paroxetine | Significant | Sedative | Significant |
| Fluvoxamine | Moderate | Sedative | Significant |
| Sertraline | Moderate | Anxiolytic | Moderate |
| Cipramil | Weak | Anxiolytic | Weak |
| Fluoxetine | Weak | Disinhibiting | Moderate |
Paroxetine
Of all the serotonin reuptake inhibitors, Paroxetine is the most effective drug . It is prescribed in an initial concentration of 10 mg or 20 mg. In some cases, the dosage is gradually increased to 50 mg per day. Take the medicine once a day. The half-life of Paroxetine occurs in almost a day. Within a week of taking the drug, a stable concentration is achieved. The drug may cause slight weight gain.
Fluvoxamine
For manifestations of depression in combination with increased anxiety, Fluvoxamine is prescribed. The effectiveness of this drug appears almost immediately after the start of administration and subsequently has a smooth effect on the patient. The drug has proven itself positively in the manifestation of obsessive-compulsive disorder neuroses, social phobias (including in children), and in combination with other drugs has proven itself well in the treatment of schizophrenia.
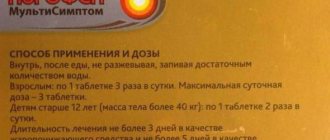
The initial concentration of the drug is 50 mg once a day; it is recommended to take the drug in the evening. The initial dosage can be increased to 100 mg, the maximum amount is 500 mg (in this case, the regimen includes several doses of the drug). Within 5-7 days, the effective concentration of the active substance is achieved. Fluvoxamine has the largest number of side effects.
Sertraline
Indications for the use of Sertraline are mild depressive states . It does not affect psychomotor functions and has a weak antiphobic effect. The drug is prescribed for the treatment of obsessive-compulsive disorder. It gives a good therapeutic effect and can prevent relapse and the development of depression in the future.
The initial dose of Sertraline is 50 mg per day. The dosage can be gradually increased to 200 mg (50 mg per week). The half-life of the active substance is affected by the age of the patient . With prolonged use of the drug, addiction develops.
Cipramil
Tsipramil is most often prescribed for the treatment of depressive conditions that arise as a result of chronic somatic diseases. In addition, it is indicated for elderly patients who have suffered a cerebral stroke.
The initial dose of Tsipramil is 20 mg per day. The drug is taken once a day in the morning . In most cases, this dose of the drug has a good therapeutic effect. The daily concentration can be increased to 60 mg, depending on the severity of the patient's condition .
In the practice of using Tsipramil, its interaction with other drugs is not described. The half-life of the inhibitor is 30 hours. Among the most common side effects are nausea and headache, but they are observed only in the initial stages of taking the drug.
Fluvoxamine
Fluvoxamine (fevarin), as a selective serotonin reuptake inhibitor, has a distinctly activating, mood-enhancing effect, it calms, stabilizes the activity of the autonomic system and can be recommended for a combination of depression and anxiety. In addition, the positive aspect of fluvoxamine treatment is its relatively rapid onset and smooth action, which, as a rule, contributes to the establishment of a good relationship between the patient and his attending physician.
Fluvoxamine is prescribed in a dose of 50 mg. per day once in the evening. The dose of the drug can be increased to 100 mg. (average dose of effectiveness) for 5-7 days. If necessary, the dosage of the drug can be further increased at intervals of 2-4 weeks (maximum daily dosage - 500 mg), starting with a dose of 150 mg. the drug is prescribed several times a day.
The active metabolites of fluvoxamine are unknown. The average half-life is 20 hours, plasma concentrations are not proportional to the dose taken
In most cases, symptoms of an anxiety disorder are eliminated earlier than those of a depressive disorder. This was clinically manifested by an improvement in the general condition of the patients, leading them to greater composure, confidence and external calm. The effectiveness of this drug is noted in patients with obsessive disorders and social phobia, in particular in childhood.
Adding fluvoxamine to atypical neuroleptics can reduce the severity of primary negative symptoms in patients with chronic schizophrenia. At the same time, comparative studies have shown that among the group of selective serotonin reuptake inhibitors, it has the greatest number of side effects (Freemante N., et al., 2000), sertraline has the least (Edwards J., Anderson I., 1999 ).