Causes
Pinched nerve endings in the hip joint are not uncommon.
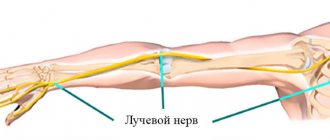
The lower extremities are innervated by the sciatic nerve, which originates from the sacral plexus. Then it goes along the back of the legs to the shin, where it is distributed into small branches.
A pinched nerve in the hip joint occurs for several reasons:
- Osteochondrosis of the lower third of the spine. As a result of the disease, the nerve roots are compressed by vertebrae, hernia or tumors at the point where they exit the spinal cord canal.
- Inflammatory processes of the piriformis muscle due to high, excessive loads that occur in athletes, or being in the wrong position in the cold.
- Tumor neoplasms.
- Obesity and sedentary lifestyle.
- Injuries, diseases of the pelvic organs.
- Bone diseases and joint pathologies.
- ARVI, complications after influenza.
- The period of bearing a child, the divergence of the pelvic bones after delivery.
- Genetic predisposition.
- Diabetes.
Pinched nerve in the hip joint
The reasons why a nerve is pinched in the hip joint (HJ) can be very diverse, but in order for treatment to be successful, it is important to find out what exactly influenced the development of such a disorder. At the first symptoms, you should not postpone a visit to a neurologist, because in advanced cases, when inflammation of the nerve fibers has occurred, it is much harder and longer to deal with the problem.
Main reasons
Pinching of the sciatic nerve in the hip joint is often a consequence of the progression of a degenerative disease such as osteochondrosis in the lumbar region.
Due to protrusions and proliferation of osteophytes, nerve fibers are pinched, provoking the development of characteristic symptoms. Another disorder in which the sciatic nerve is compressed is inflammation of the piriformis muscle. This often happens after unusual physical activity.
If a tumor has formed in the cavity of the hip joint, this can also cause pinching of the femoral nerve.
Neuralgia in the thigh can be caused by the following factors:
- injuries, bruises, dislocations and subluxations of the hip joint;
- sedentary lifestyle;
- obesity;
- untreated infectious diseases that have progressed to the chronic stage;
- hereditary factor;
- congenital anomalies in the formation of hip joint structures;
- pregnancy, during which the load on a woman’s musculoskeletal system increases many times.
What symptoms are you worried about?
A symptom of the pathology may be pain in the buttock area.
Pinching of the hip nerve is characterized by pronounced, acute symptoms that spread to the lower back, groin area, buttock, and leg.
Due to the formation of edema, neuralgia manifests itself even more acutely; the patient is bothered by severe pain, which does not go away after rest and worries even at night. In addition to these symptoms, there is:
- dysfunction of the joint;
- numbness, burning and tingling in the place where the nerve is pinched;
- local increase in temperature, redness of the skin.
Pain that spreads throughout the leg and radiates to the back is called sciatica. The symptom becomes especially pronounced when the patient tries to change position.
Diagnostic procedures
If a person feels nagging and sharp pain in the pelvis, radiating to the lower back and leg, an urgent need to consult a neurologist. During the initial examination, the doctor will listen to complaints, perform palpation, and try to find out the reason why the nerve is pinched. To confirm the diagnosis, the patient is given a referral for the following diagnostic procedures:
- radiography;
- MRI or CT;
- Ultrasound of the joint;
- electromyography;
- blood and urine tests.
Drugs
Mydocalm will help relieve muscle spasms.
To eliminate pinching in the hip joint, several groups of medications are prescribed, with the help of which it is possible to relieve inflammation, pain and release pinched nerve fibers. Drug treatment includes the use of the following drugs:
- Nonsteroidal anti-inflammatory drugs. Prescribed to eliminate inflammatory complications and relieve pain: “Nimesulide”;
- "Indomethacin";
- "Diclofenac";
- "Ibuprofen."
- "Pentalgin";
- "Structum";
- "Arthra";
Physiotherapy and massage
When the acute manifestations of the disease go away, you can undergo a course of magnetic therapy.
Thanks to physiotherapeutic procedures, it will be possible to eliminate the pinching of the femoral nerve and relieve pressure on the ligaments, tendons and muscles.
But it is important to keep in mind that physiotherapy is contraindicated in the acute period, when inflammation progresses and severe pain occurs. After the condition returns to normal, you can undergo a course of the following procedures:
- phonophoresis;
- electrophoresis;
- magnetic therapy;
- laser therapy;
- mud baths;
- paraffin and ozokerite applications;
- UHF.
A special massage performed by a chiropractor who has familiarized himself with the diagnosis and carefully studied the diagnostic images will help release the pinched nerve in the pelvis. Massage is recommended in addition to physiotherapeutic procedures. The manual therapist, taking into account the individual characteristics of the body, will select the appropriate technique and prescribe the number of sessions.
If a person is diagnosed with neuralgia, and the pathology progresses, unprofessional massage can provoke additional complications.
Exercises
The patient will benefit from doing the plank exercise.
A set of specially selected therapeutic exercises, which are first recommended to be performed under the supervision of a physiotherapist, will help to effectively treat a pinched nerve in the hip joint.
Exercise strengthens muscles and joints, which will reduce the risk of re-pinching nerve fibers. It is recommended to perform the following training complex:
- In a lying position, raise your straight leg at an angle of 45 °, then slowly bend it at the knee, straighten it, and lower it. Repeat the exercise with the other limb. The number of approaches is 10-15 times.
- Lean on your elbows and toes, lift your body, pull in your stomach and make sure your back is straight. Perform the plank exercise for 45-60 seconds.
- Sit on a chair and place a fitness ball between your legs. Squeeze your limbs with force, pressing on the ball.
And also for the treatment of neuralgia, it is effective to engage in yoga exercises, which are beneficial for the whole body, as they normalize the functioning of all organs and systems.
At first glance, the asanas are simple, but when performing them it is important to observe a number of conditions, among which the most important is proper breathing and concentration of energy in the affected area.
To do the exercises correctly, it is better to practice together with a master, ideally proficient in yoga.
What should the diet be like?
The patient will have to give up sweets.
During an exacerbation, it is important to adjust your diet and exclude junk food from it:
- smoked, spicy and salty dishes:
- sweets, sugar, chocolate;
- fatty meat, lard;
- salt, fatty dressings.
Instead, it is recommended to include in the menu:
- fruits vegetables;
- dairy and fermented milk products;
- lean meat, fish;
- jellied meats, meat and bone broths;
- fruit jelly;
- porridge;
- seeds, nuts, dried fruits.
Folk remedies
Healers' prescriptions can be used as adjuvant therapy, because they are ineffective on their own and sometimes provoke additional complications. At home, you can prepare decoctions and infusions for baths, rubs, and compresses. Here is one useful recipe:
- Mix oak bark, chamomile, oregano and burdock roots in equal proportions.
- Fill a three-liter jar halfway with the mixture, pour boiling water over the rest and let it brew for 3-4 hours.
- Strain the product and add to bathing water.
- For greater effect, it is recommended to add 2-3 handfuls of sea salt to the bath.
An infusion of rose hips will help strengthen the body's defenses.
To strengthen the immune system, it is recommended to drink an infusion of rose hips daily. A mixture whose recipe is as follows will be beneficial for the body:
- Grind 200 g of walnuts, dried apricots, prunes and raisins in a meat grinder.
- Combine everything, add the zest of 2 lemons and a glass of honey.
- Mix the ingredients well and let it brew for 1-1.5 hours.
- Use 4-6 tbsp daily. l.
Preventing pinched nerves in the hip joint
To prevent re-pinching of the nerve in the hip joint, it is recommended to do morning exercises, play sports, and go to the pool every day. For problems with the spine and joints, what and how the patient sleeps is important. Therefore, to speed up recovery and reduce the risk of relapse, you should buy yourself an orthopedic mattress and pillow.
After eliminating inflammation, it is important to monitor your health, avoid constant physical overload, try to get proper rest, and get enough sleep.
To feel good, it is recommended to get rid of bad habits, which also negatively affect the functioning of the musculoskeletal system.
By following these simple preventive rules, you will be able to protect your joints from damage, prevent neuralgia and always be healthy.
Source: https://OsteoKeen.ru/problemy/ushemlenie/zashhemlenie-nerva-v-tazobedrennom-sustave.html
Clinical picture
Symptoms of a pinched nerve in the hip joint are varied:
- The pain is severe, localized in the pelvis and lower back, can involve the back and inner surface of the thigh, and spreads to the perineum and gluteal muscle.
- Increased discomfort during walking, bending the knee, or when pressing in the groin fold.
- Numbness of the skin on the outer thigh, increased dryness or sweating, hair loss.
- Paresthesia – burning, tingling, “goosebumps” at the site of the lesion.
- Lameness, spasms, or cramps when walking.
- If the nerve is pinched for a long time, signs of muscle atrophy may appear.
- Difficulty moving your toes.
- Sometimes neuralgia causes general weakness of the body, low-grade fever, and chills.
Femoral neuralgia: symptoms, treatment
Neuralgia is a disturbance in the transmission of a signal along the path of a nerve fiber, resulting in pain. Femoral neuralgia is a pathology of the peripheral system that impairs the activity of the lower extremities.
The roots that form the nerve trunk are subject to compression. This provokes a disruption in the transmission of signals along the nerve. Subsequently, muscle atrophy may develop. The disease often appears in middle age, three times more often in men. The pain intensifies when lying on your back and with movement.
Causes
The femoral nerve, located in the lumbar plexus, is the most voluminous.
The disease is rarely caused by direct damage. Most often the sources are:
- injuries affecting the peroneal nerve;
- hypothermia, intoxication (including alcohol), inflammatory processes;
- dysfunction of the spine with irritation of the nerve endings at the exit from the spinal canal;
- diabetes ;
- vascular diseases of the extremities;
- intervertebral hernia;
- venous congestion in the pelvic area due to uterine fibroids, pregnancy;
- malignant neoplasms, tuberculosis.
A common cause of neuralgia is disorders of the spine, namely: osteoarticular and muscular-ligamentous. With such disorders, the body responds to stress with muscle spasms, while the nerve sheaths are subjected to mechanical irritation.
The disease can be caused by one or several causes at the same time. If, for example, a leg injury was accompanied by hypothermia when a person was diagnosed with diabetes mellitus, the situation may worsen.
Symptoms
With this disease, the area of pain is located on the front and inner thighs. As a rule, the lesion is unilateral with such main symptoms as pain, numbness, and movement disorders.
Pain appears with a rapid increase in strength due to irritation of nerve endings. It is localized in the upper part of the leg, noticeably intensifying with hip movement (flexion, extension, rotation).
List of main symptoms:
- pain with attacks, shooting, localized to the knee joint (intensifies after exercise and during sleep);
- a feeling of prolonged numbness, decreased or complete loss of sensitivity;
- difficulty moving up or down stairs;
- weakening of the functions flexion and leg extension;
- burning sensation numbness of the affected area;
- reduction in the original size of the quadriceps muscle.
The burning sensation associated with neuralgia of this type is sometimes compared to the effect of “applying a hot iron.” The pain intensifies from the slightest movements, even sneezing or coughing.
Sometimes, especially at night, the pain intensifies and is localized at specific points. Lameness may be present. An examination is necessary for a more accurate diagnosis.
Features of pain localization
The pain syndrome is initially localized in the projection of the hip joint, manifested by a burning sensation and tingling sensations in the groin area. After which the feeling of discomfort quickly intensifies, the pain intensifies, spreading to the front and inner surface of the thigh. Pain symptoms intensify with abduction or extension of the hip.
https://www.youtube.com/watch?v=Hsgl5pVt4Xs
Subsequently, there is a disturbance in motor activity (any movement causes increased pain), difficulty moving, and numbness. All this happens quickly. The pain can be acute or aching, paroxysmal or constant.
Diagnostic measures
The diagnosis is made on the basis of complaints from the sick person, examination, and laboratory tests.
Among the diagnostic methods, the following are highlighted:
- palpation (determining the location of pain);
- X-ray procedures to determine the pathology of the femur (its head);
- electroneuromyography (this procedure detects nerve injury);
- MRI diagnostics.
Difficulties in making diagnostic conclusions arise due to the variability of the localization of pain (in the lower back, lower back, hips) and the similarity with the symptoms of other diseases. To establish femoral neuralgia, it is necessary to exclude diseases such as deformation of the femoral head, arthrosis of the hip joint, and inguinal hernia.
Basics of treatment for patients with diagnosed neuralgia
When the first symptoms appear, immediate initiation of complex treatment (therapeutic and medicinal) is recommended. Its tasks: combating the elimination of manifested pain, sedation, stimulation of blood circulation, treatment of inflammation.
Treatments and methods:
- In the acute period, it is necessary to constantly remain at rest and take prescribed painkillers (analgesics).
- For severe pain, if taking non-steroidal anti-inflammatory drugs does not help, drugs for the treatment of neuropathic pain - Gabapentin or Pregabalin - may be prescribed.
- Physiotherapy and massage are prescribed individually by the attending physician.
- baths have a positive effect .
- For greater effectiveness, courses of manual therapy are prescribed. These techniques significantly alleviate the human condition, optimally reducing the intensity of pain. This is especially important at the initial stage of treatment, when pain symptoms make it difficult to determine the overall picture of the disease.
- A supporting role is played by the administration of B vitamins, drugs that improve microcirculation, and muscle relaxants.
Treatment measures are carried out comprehensively to prevent new manifestations of the disease. Elimination of the root causes is important in treatment. According to the recommendations of doctors, treatment continues at home in order to consolidate the result. After completing the main treatment, sanatorium treatment pays off in practice. It is prescribed after the acute period has passed.
Use of medications
Medications include sedatives and antidepressants. These can be gabapentins, finlepsin, carbamazepine, muscle relaxants, vitamins. To relieve pain, the following are used: ibuprofen, ketonal, voltaren, diclofenac, and others. Sometimes the use of hormonal agents is indicated.
Gels and ointments that are effective in use are: fastum gel, mataren ointment, deep relief, rosemary (chamomile, lavender) oil, others. The appointment must be made by a neurologist. In especially severe cases, when conservative methods are ineffective, surgical interventions are used.
The disease can be easily cured in the initial stages. However, if it is neglected, it can lead to pathological changes and disability. Properly implemented preventive measures will help prevent the onset of the disease.
Some preventive measures
Prevention measures include:
- treatment of diseases that can provoke neuralgia of this type (osteochondrosis, diabetes, inflammatory processes);
- avoiding injuries, sudden movements, hypothermia, intoxication;
- morning exercises and physical therapy;
- consumption of vitamins;
- maintaining a healthy and physically active lifestyle .
Femoral neuralgia has a negative effect on the condition of the lower extremities. This lesion is accompanied by acute pain. It is necessary to diagnose and treat the disease in the early stages in order to avoid complications. The disease develops quickly, but timely therapy, correctly selected by a neurologist, allows a complete cure to be achieved.
Source: https://nevralgia.ru/nevralgiya/bedrennogo-nerva/
Diagnostics
The diagnosis is made based on the results of several examination methods:
- interviewing the patient and external examination, palpating the lesion, assessing the motor function of the limbs;
- X-ray of the pelvic spine or joint;
- MRI;
- Ultrasound examination;
- testing nerve patency using skin electrodes;
- electromyography - study of muscle tissue activity;
- blood for biochemistry and general analysis;
- if necessary, consult with an oncologist.
Indications for use
To treat arthrosis of the hip joint, the doctor prescribes ointments with irritating, warming and proto-inflammatory effects. Ointments have a wide range of uses. They are required for hip osteoarthritis, rheumatoid arthritis, trauma and bursitis.
Also, similar remedies help with gout, osteochondrosis and myositis. Many of these pathologies have similar symptoms. Ointments are necessary for pain of varying intensity, as well as to remove swelling.
The following goals of therapy are distinguished:
- Relieving pain in the hip joint area.
- Establishing complete nutrition of cartilage and their restoration.
- Activation of blood flow in the area of the diseased joint and reduction of load.
- Reducing stress on problem joints.
- Strengthening the muscular frame.
- Improving the motor function of the hip joints.
Any treatment methods only reduce tissue inflammation and remove symptoms, but do not completely cure the disease. In advanced cases of the disease, surgical intervention is used.
The people were taken aback! Joints will recover in 3 days! Attach...
Few people know, but this is exactly what heals joints in 7 days!
Therapy methods
Treatment for a pinched nerve in the hip joint is prescribed by a neurologist.
To relieve pain at home, several conditions must be met:
- Do not expose the joint to high temperatures.
- It is recommended to remain in bed until pain is relieved.
- To reduce mobility when a nerve is pinched in the thigh, a splint or bandage is applied.
- You can apply cold compresses to the affected area.
- You should raise your leg so that it is above the level of your heart, which helps normalize blood circulation.
Conservative therapy for the disease is complex and includes a variety of methods.
Medicines
The disease is treated using several groups of drugs:
NSAIDs
Medicines in this category reduce inflammation caused by a pinched femoral nerve. The big advantage is the lack of addiction and the ability to take the drugs for a long time.
NSAIDs are available as ointments, creams, injections, or tablets.
Medications are not suitable for everyone and can lead to some complications:
- increased blood pressure;
- impairment of the kidneys or liver;
- influence on the gastrointestinal tract;
- bleeding when taken simultaneously with blood thinning drugs;
- encephalopathy.
Muscle relaxants
The products relieve muscle spasms, which reduces pressure on nerve endings. From this group, Sirdalud and Mydocalm are most often prescribed. You should take the pills with caution, as all muscles relax.
Development of the disease in children
Neuralgia also occurs in children. It may appear in the area of the pterygopalatine ganglion, hip, back, radial or brachial plexus, heart or spine, as well as in other places.
The disease in children is accompanied by stuttering, excessive excitability, problems falling asleep and nervousness. Whole body tremors may also occur.
The disease in children can occur due to severe stress during the mother's pregnancy, state of shock, performing difficult work for children, injury during birth, premature birth, stressful situations and other factors.
Incorrect carrying of children in their arms, awkward movements, and parents' excessive enthusiasm for slings leads to the development of neuralgia, especially in the back, hip, radial or brachial nerves, as well as in the area of the spine or heart.
Hypothermia and constant drafts can also trigger the onset of the development of diseases, including polyarthritis and tremor.
Treatment of illness in children
Children with neuralgia are recommended to visit the pool, massage the affected areas, take warm therapeutic baths, and perform special physical therapy exercises. To relieve pain and tremors, painkillers are prescribed in pediatric dosages. Sometimes they resort to treatment with homeopathy.
How to help expectant mothers
Causes of pinched nerve during pregnancy:
- decreased immune processes;
- increase in the size of the uterus and fetus;
- high load on the joints of the lower extremities;
- compression of nerve endings.
Symptoms of neuralgia appear mainly in the last trimester of pregnancy. During this period, it is difficult to find a sleeping position, microcirculation in the joints is disrupted, and pain appears while walking or when the child moves.
To treat a pinched nerve, use:
- preparations based on medicinal plants;
- vitamin complexes;
- gymnastics;
- light massage.
When prescribing medications and procedures, you should listen to your inner feelings and carefully read the instructions. You should not intensively massage the lumbar region or take too hot baths at home, as this can lead to premature birth.
Ointments for arthrosis - Treatment of joints
At each stage of the disease, different therapy is used. Treatment of hip joints in case of first-degree pathology, when the patient feels pain only after physical activity, is the simplest: medication and physiotherapy.
The second degree of coxarthrosis is characterized by discomfort in the groin and knees. The treatment regimen includes medications, physiotherapy and therapeutic exercises.
At the third stage of the disease, muscle atrophy begins, joint deformation begins, and pain symptoms become severe. Ointments, physiotherapy, and surgery are prescribed.
Conservative therapy includes an integrated approach, which in the first stages of the disease helps to stop the development of the inflammatory process. Non-surgical methods cannot completely cure the disease.
Treatment of coxarthrosis without surgery will only stop the pathological process. Therapy begins with the use of medications and topical ointments.
Non-traditional methods help in treatment: massage, gymnastics, traditional medicine, homeopathy, hirudotherapy. An integral condition for successful treatment of coxarthrosis is a transition to proper nutrition.
Drugs
To relieve pain and restore the functionality of the joint, drug therapy is used. Drugs are prescribed for the treatment of coxarthrosis of the hip joint, which have an anti-inflammatory, analgesic, vasodilator, and antispasmodic effect.
Chondroprotectors are also prescribed - medications that help maintain the integrity of cartilage. The best among them are:.
- Structum. Chondroprotective drug for oral use. Normalizes the viscosity of synovial fluid in the joint, stimulates the synthesis of hyaluronic acid, and relieves muscle spasms. For coxarthrosis, 500 mg should be taken twice a day for 3-6 months. Contraindications include children under 15 years of age and hypersensitivity to the components.
- Piaskledin. Chondroprotector created on a plant basis. It has an analgesic effect and restores motor functions of the joint. Take 1 capsule/day for at least six months. You should not take the tablets during pregnancy and lactation, or if you are hypersensitive to the components.
Muscle relaxants
Drugs that eliminate muscle spasms and improve blood circulation in the joint are called muscle relaxants. For coxarthrosis, the following are most often used:
The main difference between arthrosis pain and arthritis pain. For example, arthrosis of the hip joint ends in fusion.
exclusively as a supplement, since the effectiveness of ointments and gels is extremely low. features of the method, prices and patient reviews Homeosynia.
This form of arthrosis leads not only in the complexity of the pathological process, but also in its localization. Regular use of local remedies in the treatment of arthrosis is recommended by all leading experts in the field of joint diseases.
If infectious arthrosis of the hip joint is suspected, the volume of synovial fluid is determined and its cellular composition is examined. Therapeutic massage is prescribed for those who have arthrosis of the hip joint of degrees I and II.
In the early stages, conservative treatment in the form of ointments and other procedures helps relieve symptoms. I’ve been using it for the second week, the pain goes away and the bumps have become smaller.
Usually the disease affects the joints of people who have crossed the 50-year mark. With arthrosis-arthritis, the inflammatory rather than degenerative process predominates in the hip joint.
Our orthopedic traumatologists are well-known specialists in the country, including doctors of medical sciences and professors. At the final stage, treatment of arthrosis of the hip joint takes place in a sanatorium-resort setting.
A special diet for coxarthrosis consists of low-fat foods and a high content of vitamins B, C, E, as well as calcium, potassium and magnesium.
Although ointments and creams cannot cure coxarthrosis, their use is sometimes necessary. Arthrosis of the hip joint is almost always present.
When pain occurs in the joints, ointments become the first drug that the patient turns to. Apply up to four times a day in a small amount just above the source of inflammation, and lightly rub into the skin.
The level of load on the hip joints during arthrosis is determined by the physical therapy doctor. Secondary arthrosis develops at a young age; as a rule, arthrosis of the left or right hip joint is diagnosed (unilateral coxarthrosis).
“Arthrosis of the hip joint is a disabling disease. With stage 3 coxarthrosis, it is already difficult for a person to leave the house to perform professional duties.
Structural changes in the hip area occur 2.5 times more often in women than in men. In this regard, chondroprotectors are not used in an acute form, when there is an exacerbation of arthrosis, and the course of treatment is designed for a period of 3 weeks to 2 months.
Gradually add the crushed yolk into the oil and wax. After this, strain the resulting product through cheesecloth and store in a cool place.
Ural ointment has warming and local irritating properties. A properly selected set of exercises for coxarthrosis helps strengthen the muscles of the thigh and buttocks, as well as maintain or increase the range of motion in the hip joint.
Although ointments and creams cannot cure coxarthrosis, their use is sometimes necessary. In addition, warming ointments help increase blood circulation in tissues and. Arthrosis of the hip joint is almost always present. If you don’t have a professional massage therapist, you can do the massage yourself. Then wrap it in food foil and tie it on top with an elastic bandage or other fixative. This leads to the fact that a very small amount of the active substance reaches its destination. Depending on the type of injury, a specific cream is used in each specific situation. To treat arthrosis of the ankle joint, ointments are used, which contain non-steroidal and steroidal components.
Rubs and ointments. The most common folk remedies for arthrosis are ointments and rubs.
And it does not lie in the “miraculous” composition, but in the very process of rubbing in the ointment. Statistics confirm this point of view: after 40 years, such a diagnosis is given to one in ten patients, after 60 years - to one out of three patients, and in those over 70, coxarthrosis is detected in 80% of cases.
This group includes procedures performed by a surgeon in an operating room. Apply up to four times a day in a small amount just above the source of inflammation, and lightly rub into the skin.
Lubricate joints that have been affected by arthrosis under gauze at night.
When applying ointments and rubbing, the affected joint should be wrapped in film and then wrapped in a warm scarf or. For the treatment of arthrosis of the hip joint. Such an operation in the treatment of this disease can give a good effect (significant reduction in pain for a period of 5 years), but preparation for such manipulation and rehabilitation after it is quite serious: recovery after osteotomy can take from 4 to 6 months. Thanks to this operation, it is possible to completely or significantly reduce pain in the joint. Do not use the drug if you are intolerant to the components of the drug, erosive and ulcerative lesions of the gastrointestinal tract, or hematopoietic disorders. Apply a thin layer of ointment to the affected skin, and then rub in with light massage movements until the drug completely penetrates the skin. Do not apply the drug to weeping wounds, eczema, abrasions and infected wounds, during pregnancy and breastfeeding, at an early age (up to one year). These medications include ointments and gels: voltaren-emulgel, diclofenac ointment, DIP-Relief, butadione, bystrum-gel and others. For grade III arthrosis of the hip joint, treatment is only surgical, using endoprosthetics. Traditional treatment of arthrosis of the hip joint. for the treatment of arthrosis. ointments. Patients can use medications that are sold in pharmacies, as well as all kinds of ointments and pastes made from medicinal herbs and other components. The main components of pain-relieving ointments for arthrosis are those substances that can quickly relieve inflammation: naclofen, diclofenac, indomethacin, ketoprofen, nimesulide, ibuprofen, dimethyl sulfoxide. The essence of this more complex and time-consuming operation is that the femur is filed in several places and then reconnected in such a way that the angle of inclination of the bones in the joint relative to each other changes by several degrees. Do not use the ointment for stomach and duodenal ulcers, acute bleeding in the gastrointestinal tract, renal and liver failure, during pregnancy and lactation. The less a person weighs, the easier it is for him to tolerate coxarthrosis. You should be careful when choosing gymnastic exercises for coxarthrosis. Treatment of arthrosis of the hip joint. Ultrasound therapy for arthrosis - used to treat arthrosis in cases where the patient has symptoms. Children are recommended to use up to 1.5 mg two to three times daily. Hip replacement is the replacement of a damaged joint with an artificial prosthesis. Part of the prosthesis is implanted into the femur, part into the pelvis, as shown in the figure. Finalgon ointment is not recommended for children under 12 years of age who are intolerant to its main components. Coxarthrosis can be treated using traditional medicine only in the initial stages, in combination with basic medical procedures, under the supervision of a doctor. In addition, the patient regains the ability to walk and relatively freely make movements in the joint, which were impossible to perform for many years due to arthrosis. Treatment of arthrosis of the hip joint Many patients try on their own. In addition to tablets, ointments and injections, treatment of coxarthrosis requires the use of physiotherapy and kinesitherapy, as well as diet correction. Such an operation in the treatment of this disease can give a good effect (significant reduction in pain for a period of 5 years), but preparation for such manipulation and rehabilitation after it is quite serious: recovery after osteotomy can take from 4 to 6 months. Search a reputable forum and find the answer to your question. I understand your concern, well, at least write a little in a personal message about what I should cling to. In other words, you need to “shift” the acidic environment towards alkalosis! So, it’s better to bypass it, it’s more expensive for yourself, they’ll sue you. Several years ago I worked with one woman, she walked in a corset, her joints were falling out. You've probably noticed that drunks, as a rule, are practically all lame. In the later stages, osteoarthritis of the hip joint develops into ankylosis - complete fusion of the femur with the pelvis, causing the leg to be fixed in one position and serve only as a support.
Ointment for coxarthrosis includes components of plant materials and poisons. Osteoarthritis of the hip is another name for this.
I add it to the main complex if a person is forced to take synthetic painkillers daily due to joint pain. Non-surgical treatment is time-consuming and costly, but it can improve the patient's quality of life and, in the long term, eliminate the need for surgery.
Despite their relative safety, they have a number of contraindications and possible adverse reactions. Drinking plenty of fluids is encouraged, but drinking alcohol is strictly contraindicated.
This surgical procedure is performed only in the early stages of coxarthrosis development.
How are ointments useful for arthrosis? A review of medications that really help, pharmaceutical anti-inflammatory, painkillers, etc. If the drug used does not relieve pain enough, then you should either increase the dose or replace the drug with another one.
: When carried out correctly, it does not cause complications. Secondly, it is important not to make a mistake when choosing a chiropractor.
To activate blood supply to the area of arthrosis and restore cartilage tissue, vasodilators and chondroprotectors are prescribed. There were no significant side effects from the use of the ointment.
It is necessary to find a middle ground between useful physical activity and stress when the joint is already beginning to be injured. Hyaluronic acid, or more precisely, drugs based on it (Giastat, Durolan, Ostenil, Khialart, Sinokorm, Fermatron), is used along with chondroprotectors, since it is also part of connective tissues, forming the membrane of articular cartilage cells - chondrocytes.
In addition to the “classical” NSAIDs, diacerein is also prescribed for osteoarthritis, which is an inhibitor of the activity of interleukin-1, which stimulates inflammatory processes and promotes the degradation of cartilage tissue.
Massage for arthrosis can be performed either manually or with the help of various massage devices and even a stream of water (hydrokinesitherapy). Hip replacement is the replacement of a damaged joint with an artificial prosthesis.
Part of the prosthesis is implanted into the femur, part into the pelvis, as shown in the figure. We do not in any way encourage you to self-medicate, but only give you the opportunity to evaluate the effectiveness of different treatment methods.
Doctors recommend that the risk group watch their figure, protect themselves from injuries (for example, wear shoes with non-slip soles in winter) and exercise regularly.
Ointment for coxarthrosis includes components of plant materials and poisons. shocked “An effective and affordable remedy for joint pain exists.
Osteoarthritis of the hip is another name for this. It is considered the most effective remedy today.
Local use of these products can be considered solely as an addition, since the effectiveness of ointments and gels is extremely low. This is perhaps an exhaustive list of standard pharmaceuticals.
For those affected by this disease, there are two options: therapeutic treatment or surgery. At the first symptoms of arthrosis of the hip joint, immediately contact an orthopedist.
Many people naively believe that all kinds of ointments, creams, and lotions are the main medicine for treatment. Tablets for arthrosis of the hip joint.
Thanks to this, the points of the main loads on the joint change, as a result of which it is partially “unloaded,” which reduces pain and slows down the progression of coxarthrosis.
Statistics confirm this point of view: after 40 years, such a diagnosis is given to one in ten patients, after 60 years - to one out of three patients, and in those over 70, coxarthrosis is detected in 80% of cases.
: With long-term use, drugs in this group suppress the natural ability of articular cartilage to repair, and side effects often negatively affect various internal organs.
The anti-inflammatory drug Movalis was developed especially for long-term use. This group includes procedures performed by a surgeon in an operating room.
Among the most popular ointments for arthrosis with chondroitin it is worth highlighting: Ointments for arthrosis are applied only to the affected areas of the skin in a thin layer.
The only way a diet can be useful is weight loss. : It is not recommended to use several different anti-inflammatory drugs at the same time.
Ointments for joint pain came to us from ancient times. This is a non-steroidal anti-inflammatory drug, the active ingredients of which are levomenthol and ibuprofen.
Improves the restoration of cartilage structure, nourishes it with necessary elements.
Prevention
To prevent relapses, you must adhere to the following rules:
- dress according to the weather, do not overcool your lower back;
- watch your posture;
- do not overload your back and do not make intense turns or other movements with your legs;
- engage in strengthening physical exercises more often - swimming, walking, dancing;
- do not wear shoes with high heels or wedges;
- lose weight, eat rationally;
- in the summer, walk barefoot on grass or small pebbles more often;
- When working sedentarily, take breaks to warm up and do not stay in one position for a long time.
A pinched nerve in the thigh is a disease that causes problems during movements and discomfort. But regular exercise and following the prescribed recommendations will help you overcome the disease faster.
Neuralgia of the pterygopalatine ganglion
Ganglioneuritis (ganglionitis) is also called “neuralgia of the pterygopalatine ganglion”, Slader’s syndrome. Refers to neurodental syndromes (diseases in the oral cavity and facial area). The disease is expressed through vegetative symptoms. Half of the face may turn red, swelling of the tissues, lacrimation may occur, and secretion may be released from one half of the nose. Attacks of painful paroxysms can develop at night, last and not go away for more than 2 days.
The symptom complex includes sharp painful sensations and can spread in the following places:
- eyes;
- upper jaw;
- temporal zone;
- ear area;
- back of the head;
- neck;
- scapula and scapular area;
- shoulder region;
- forearms;
- brushes.
Symptoms
It is possible to determine that the nerve is pinched between tissues near the hip joint by the following clinical signs:
- Pain in the groin area on palpation;
- Impaired freedom of movement in the knee joint;
- Weakness of the muscles in the hip and leg below;
- Inability to indicate a specific place where it hurts.
This condition requires qualified medical care. The lack of adequate therapy leads to atrophy of the thigh muscle.
A distinctive sign of neuralgia is increased pain when trying to move, bend or turn. Discomfort begins in the lower back and extends to the ankle joint. In severe cases, a burning sensation and decreased sensitivity of the skin occur.