Why does a pathological process develop?
For a major stroke, the reasons are the same as for smaller cerebral disorders:
- blockage of the vascular bed by a thrombus or atherosclerotic plaque;
- vessel damage.
Factors that provoke extensive cerebral infarction will be as follows:
- Atherosclerosis. Intravascular cholesterol deposits impede blood circulation, and a detached plaque can completely block the vessel.
- Thrombosis. Blood clots form on the walls of arteries in people with high blood viscosity. Separation of a blood clot and blocking of a vascular lumen by a clot is the cause of an acute ischemic attack. This pathology does not depend on age - it can develop at both 60 and 90 years.
- Hypertensive crises. Increases in pressure provoke vascular spasm, which does not always disappear after a decrease in blood pressure. Blood flow in a spasmodic cerebral vessel partially or completely stops.
Hemorrhage is provoked by other factors:
- weakness of the vascular wall;
- congenital vascular anomalies (pathological narrowings, kinks);
- aneurysm;
- head injuries.
The negative impact of provoking causes is enhanced by excess weight, endocrine pathologies and bad habits (smoking, alcohol).
Relatives who stand under the doors of the intensive care unit when their mother had a massive stroke at the age of 70 can hope for a more favorable ischemic form.
What can cause illness in an elderly person?
Doctors say that a stroke can occur at any age, but the likelihood of it happening is higher in older people, because they most often suffer from diseases that cause problems with blood vessels. These include:
- Arterial type hypertension. Most often, older women and men experience high blood pressure, which is practically incurable, so stroke after 80 years is a common occurrence.
- Kidney diseases.
- Disturbances in the functioning of the endocrine system.
- Diabetes of any type and vascular aneurysm.
- Atrial fibrillation, which is often diagnosed in older people. A blood clot in the heart easily travels to the brain and causes a stroke.
- Rheumatism.
- Any viral disease in severe form.
- Increased cholesterol levels, which provokes the formation of blood clots in blood vessels.
- Sedentary lifestyle. It cannot be classified as a disease, but it becomes the cause of their development. Someone can live for years without getting a stroke, while others end up in a hospital bed within a month of this lifestyle.
Stroke in old age is most often ischemic, when a blood vessel is blocked and circulation to the brain is disrupted. But a hemorrhagic stroke, which ruptures a blood vessel, leading to bleeding in the brain tissue, is also possible.
This is not to say that there are no age-related characteristics of stroke. So, the consequences for people aged 30 years and 80 years will have some differences:
- The clinical picture of the disease in a stroke over 70-80 years of age will be incredibly severe, and it is precisely this course of the disease that is a direct threat to the patient’s life. The chances of survival are minimal, because death occurs in more than 85% of patients, especially if it is a major stroke.
- Forecast. An older stroke survivor will always have a worse prognosis for regaining body function than a younger person. The saddest thing is that the signs of a stroke are primarily ignored by the patient himself for fear of upsetting the family. And this reduces survival and treatment of the disease to nothing.
- Diagnosis of ischemic stroke in the elderly is more common than hemorrhagic stroke. They are also more likely to have a major stroke than patients aged 30-40 years.
The cause of stroke in old age is most often vascular atherosclerosis, because with it atherosclerotic plaques close the blood lumen. A blood clot torn off by blood enters the brain, provoking an attack. A similar situation develops with atrial fibrillation. Often, vascular atherosclerosis can provoke dozens of micro-strokes per year in a patient, the attacks of which are invisible.
Survival in such a situation is almost impossible, because if the disease is not treated for such a long period, it will lead to a massive stroke, which at this age ends in death.
Important! You can prevent a major stroke if you quickly respond to the following signs of an impending illness:
- on the left or right the body goes numb, either entirely or partially;
- in a conversation, it is difficult for other people to understand an elderly person;
- Vertigo becomes common and even leads to falls or decreased vision.
A stroke at 80 years old, the prognosis of which will be positive, is a quick response to the symptoms of the disease and timely treatment. If a grandparent has a hemorrhagic attack, the symptoms will be as follows:
- severe headache accompanied by rapid breathing and wheezing;
- strong, intermittent heartbeat, leading to fainting or near-fainting;
- blood pressure rises sharply, while the face becomes very red;
- limbs and facial muscles go numb;
- the patient feels sick and vomits.
Important! Signs of this type of stroke develop rapidly, so the patient usually loses consciousness at the beginning of the attack.
Depending on the area of the brain where the hemorrhage occurred, the patient may lose hearing or vision, and if it is a major stroke, seizures may begin and a coma may occur.
If, for example, an ischemic stroke occurs on the right side, the symptoms will be as follows:
- severe headache with vomiting and nausea;
- it is difficult for the patient to make any movement due to almost absolute weakness;
- visual function decreases, often the picture bifurcates;
- vertigo with impaired spatial orientation;
- memory lapses, disturbances of touch and speech.
Important! Time in the case of ischemic stroke is extremely important, because the symptoms develop gradually and become acute in 5-6 hours.
Cerebral hemorrhage and its outcomes are always individual for each person, as is treatment. But most often, a stroke has 10 consequences, and how the patient will be treated depends on them:
- The body can be paralyzed either partially or completely.
- Parts of the body, in particular limbs, become numb and cease to be felt.
- The patient cannot walk or navigate in space.
- Speech is difficult or completely absent.
- There is no swallowing function.
- Loss of hearing function, either partial or complete.
- Mental disorder.
- There is no control of urination and bowel movements.
- The patient needs constant monitoring and care.
- Death.
It is impossible to say what consequences a particular patient will have after a stroke. There are elderly people who lived happily after it, and there are those for whom the prognosis was unfavorable. Treatment and prognosis can be adjusted by assessing the presence of the following signs:
- If the cause is extensive hemorrhage occurring in the center of the brain, then the prognosis is death.
- Survival among those previously diagnosed with hypertension or atherosclerosis is usually minimal or with the most severe consequences.
- The prognosis is no less bad if the patient falls into a coma caused by swelling in the brain.
- Relapse is 100% fatal.
Treatment and rehabilitation can be effective if the following factors are observed in the patient:
- laboratory tests confirmed that the hematoma is small;
- there was no loss of consciousness;
- diseases of the cardiac system, atherosclerotic plaques of blood vessels in the neck and head have not been diagnosed;
- blood pressure is within standard values.
How positive the prognosis will be depends on the timely provision of qualified medical care. If this is done in the first six hours after the onset of the attack, then you should not prepare for the worst manifestation of the post-stroke condition.
It is the skillful and prompt actions of doctors that guarantee life and a positive prognosis for an elderly patient. Ischemic stroke always begins with transistor attacks, and if they are recognized in time, the development of pathology of cerebral circulation can be avoided, which often causes death or coma.
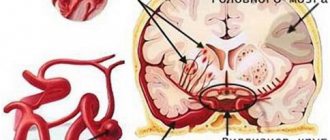
Types of major stroke
Acute cerebrovascular accidents are divided into ischemic and hemorrhagic. In the first case, the lumen of the artery closes, in the second, blood escapes from the damaged vessel. Various reasons lead to the development of these types of stroke. In addition, they differ in pathogenetic mechanisms and clinical presentation. Extensive stroke is divided into the following types:
- Hemodynamic. Vasospasm provokes a decrease in the amount of oxygen that reaches the brain tissue. The cause of this condition is often hypotension.
- Microocclusion. A stroke develops due to a local disturbance in blood flow.
- Lacunar. In the brain, due to increased pressure in the vessel, a cavity is formed. It is filled with liquid.
- Cardioembolic. Arrhythmias lead to the detachment of a blood clot. As a result of uneven contraction of the myocardium, blood turbulence occurs. The detached blood clot enters the brain vessel, causing the development of a stroke.
- Atherothrombotic. The cause of acute cerebrovascular accident is the blocking of the artery lumen by an atherosclerotic plaque. Atherosclerosis is formed due to changes in the lipid composition of the blood.
Although there are many types of stroke, a major one occurs when there is hemorrhage or ischemia. They have similar symptoms and progression rates, but the consequences will be different, as will the type of treatment. If with an extensive ischemic stroke the patient has a chance of full recovery, then with a large hemorrhagic stroke it is unlikely, and often people remain disabled due to hemorrhage.
An extensive ischemic stroke occurs due to blockage and thrombosis of blood vessels, as a result of which cells begin to starve without oxygen and die. In this case, lacunar, atherothrombotic, hemodynamic stroke, and micro-occlusion may develop. They are characterized by a sudden onset or a long period of development, so symptoms will appear gradually.
The main difference between a hemorrhagic extensive stroke is the rupture of blood vessels or aneurysms, hemorrhage in the brain, and the penetration of red blood cells through the walls of the heart. This happens suddenly and takes no more than four hours, during which all functions of the human body suffer. Often the process is painful, the patient may experience breathing and heart problems, speech impairment and even paralysis. Surviving this type of stroke is extremely difficult, especially after 50 years.
General description and types of pathology
A major stroke is a serious injury to the brain that affects a large part of the brain. Its blood supply is disrupted.
Due to oxygen starvation, toxic substances accumulate in the brain tissue, and degenerative processes begin. In most cases, such a violation leads to disability of the patient. The consequences of a massive brain stroke are extremely difficult to eliminate.
The differences between ischemic and hemorrhagic forms of the disease are analyzed by rehabilitation physician Sergei Nikolaevich Agapkin:
Table 1. Types of pathology
| Stroke form | Peculiarities |
| Major ischemic stroke | It is considered less dangerous. Poor circulation occurs due to short-term blockage of cerebral vessels by cholesterol plaques or a blood clot. Proper treatment helps to maximize recovery after injury. This type of extensive brain stroke leaves more room for survival. It also has an additional classification:
|
| Extensive hemorrhagic stroke | The prognosis is less encouraging. The chances of survival are very low. Death occurs in 89% of cases. Blood circulation is disrupted due to the fact that the vessel ruptures and biological fluid flows into the brain tissue. Next, swelling of the organ begins, due to which all vital human functions cannot be performed as before. Basically, the patient goes into a vegetative form of existence. Hemorrhagic stroke of the brain can be intracerebral and subarachnoid. |
| Stem | It affects only the base of the organ. However, this is where the vital centers are located. Such a defeat leads to the immediate death of a person. |
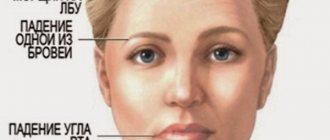
In addition, the disease can be classified according to its location:
- Stroke of the left hemisphere of the brain. It leads to paralysis of the right side of the human body. Speech is also impaired, problems with hearing and vision appear, and persistent mental pathologies are observed. The patient is not able to create logical chains of thinking or analyze the information he receives. He loses the ability to remember dates, names, and the ability to build a time sequence of events is impaired. Math skills suffer.
Differences in the effects of stroke on the right and left side
- Stroke of the right hemisphere of the brain. Due to extensive hemorrhage, sensitivity is lost on the left side. Memory and vision also suffer. Speech may be preserved, but the ability to nonverbally process information is impaired. Imagination, spatial orientation, figurative memory, and emotions suffer (the victim’s condition can hardly be called adequate).
First aid should be provided to the patient within 3 hours after the hemorrhage. Otherwise, his chances of survival drop to a few percent.
At-risk groups
Stroke is a pathology that can occur in people of any age group. But this is especially dangerous for people who fall into the following risk factors:
- People under 40 years of age who smoke a lot, abuse alcohol and take drugs;
- People from 40 to 60, and men after 50 years are more susceptible to this disease than women, but after 60 years the rates level out;
- People over 60 years old - at this age, as a rule, there are already plaques on the vessels, which significantly increase the risk of pathology. In addition, older people often suffer from hypertension, which leads to rupture of the vascular wall.
Thus, provoking factors can be combined into the following subgroups:
- advanced age;
- arterial hypertension;
- heart diseases;
- stress;
- bad habits;
- cholesterol imbalance;
- excess weight;
- hereditary predisposition;
- diabetes.
Chances of Survival
Doctors have identified several factors on which the life of a person facing a stroke depends:
- Age - the younger the body, the faster the regeneration processes occur and the greater the chance of full recovery.
- Health status – in the presence of chronic diseases of the cardiovascular system, the chances of life are reduced to a minimum.
- The presence of bad habits - if a person smokes or abuses alcohol, the rehabilitation process can be complicated.
- Speed of medical care - if the patient is in a medical facility 2-3 hours after an attack, there is every chance of saving life.
- Features of care - when a person is surrounded with love and care, all the necessary care is constantly provided, rehabilitation can speed up several times.
It’s paradoxical, but in practice there are cases where the persistent desire of relatives literally brought patients back to life after a stroke, so even in the most difficult situations you should always hope for the best.
Thus, a major stroke entails more severe consequences, rehabilitation for which has its own characteristics.
The chances of survival depend largely on age and speed of assistance.
The consequences of a major stroke can be very unpredictable, so it is difficult to predict what exactly a person will have to face during the rehabilitation period.
Impaired motor activity is one of the most common consequences of a stroke. Gymnastics after a stroke helps restore fine motor skills, as well as get back on your feet.
We will consider the risk factors for ischemic and hemorrhagic stroke in detail below.
Other complications after an attack
Literacy and the quality of rehabilitation undoubtedly play a huge role in the rate of recovery. The chances of surviving the consequences of a major stroke in this context will depend on the patience, effort and care of the patient's family members. But no matter how hard friends and relatives try, cerebrovascular accidents can have an extremely negative impact on the brain centers, as a result of which the patient’s quality of life will leave much to be desired.
In addition to the above problems encountered during a stroke, other complications can negatively affect the patient’s recovery:
- Digestive disorders - they are caused by the patient’s bedridden state, as well as non-compliance with the diet. Constipation is especially dangerous - because of it, acts of defecation are accompanied by an increase in pressure.
- Atrophy of cartilage and muscle tissue - occurs against the background of prolonged lack of physical activity.
- Bedsores are ulcerative formations on the skin that can cause an inflammatory process if the necessary hygiene procedures are not followed.
- Pneumonia is a consequence of weakened immunity and insufficient ventilation in the premises.
Often, with an extensive cerebral infarction, complications begin to develop. It could be:
- swelling of the brain - most often diagnosed;
- weakening of the immune system and the development of congestive pneumonia against this background;
- the development of inflammatory processes in the urinary tract, which is explained by the emergence of difficulties with self-care in patients;
- problems with joint mobility, which is explained by prolonged periods of lying down;
- the appearance of bedsores against the background of constant lying, which provokes a serious disruption of blood flow with subsequent death of individual sections of tissue;
- deterioration of blood circulation and, as a consequence, the development of thrombosis;
- decreased tone in the intestinal walls, which results in a problem such as constipation.
Almost all people who have experienced a massive cerebral infarction/hemorrhage experience persistent impairment of motor, sensory, cognitive, and speech functions.
| Type of neurological deficit | Possible consequences of a major stroke |
| Paresis, paralysis of arms, legs, lower face |
|
| Impaired coordination, balance deficit |
|
| Visual impairment |
|
| Loss of sensation |
|
| Decrease in intelligence |
|
| Memory disorders |
|
| Speech disorders |
|
With a major stroke, it is quite difficult to eliminate the consequences of the stroke. Few people achieve full recovery. Rehabilitation helps many people achieve good results: the ability to take care of themselves independently or with minimal assistance, communicate, and lead a moderately active life. Without it, a person is often doomed to remain deeply disabled.
Restoring function after a major stroke takes a long time. Motor disorders can be eliminated in six months, memory and thought processes can be improved in a year. It takes the longest to restore speech – 2-3 years.
The rehabilitation program may include:
- kinesiotherapy;
- massages;
- physiotherapy;
- classes with a speech therapist-aphasiologist, neurologist, psychologist;
- special exercises for eyes, articulation;
- gaming techniques to improve coordination, memory, thinking;
- communication;
- learning memory techniques.
Consequences of a stroke
A patient who has suffered a stroke usually has the following consequences, many of which are irreversible:
- Motor: problems with sensitivity in the limbs, with their mobility, impaired swallowing, increased tone of muscle tissue.
- Poor coordination of movements and balance, constant dizziness.
- Problems with spatial orientation and memory.
- Visual: partial or complete loss of vision, visual field defects, astigmatism.
- Hearing problems.
- Persistent dementia, impaired logical thinking, changes in the patient's behavior and personality, emotional and speech difficulties.
- Mental disorders, depression.
- Violation of the functionality of analyzers.
It is impossible to completely get rid of all the consequences of a major stroke. However, the sooner treatment is started, the more functions will be restored.
How patients are treated
The therapy selected for the patient is influenced by whether a large stroke is bilateral or unilateral, as well as on which side the pathological focus is localized. Treatment is selected individually, but there are general rules:
- Improving blood supply to the brain. For this purpose, vasodilators and nootropics are used.
- Blood pressure control. Crises will negatively affect cerebral blood flow, so antihypertensive medications are selected.
- Prevention of thrombosis. They give it in tablets or give injections of blood-thinning medications.
How does treatment occur if vital functions are impaired or the patient is in a coma? These patients are connected to artificial life support, which means that a machine breathes for the person, and nutrition is given through a tube or administered by drip.
How does it manifest?
The clinical picture of a stroke depends on which hemisphere of the brain is affected by the pathology. However, the following symptoms are characteristic of all types and types of the disease:
- sudden headache and almost fainting;
- body cramps;
- partial memory loss;
- speech, hearing, vision disorders;
- decreased coordination of movements;
- cardiopalmus;
- the presence of sticky cold sweat and significant redness of the facial skin;
- loss of consciousness.
Attention!
If a person has lost consciousness, it is recommended that you perform an eye pupil light test yourself. Here the reaction of the pupils to a light stimulus is monitored. If the pupil does not constrict, it means that we are talking about a major stroke.
Mechanism of violation
Another name for ischemia is cerebral infarction. As a result of a sharp restriction of blood supply, brain tissue dies. This condition often occurs due to rupture of an atherosclerotic plaque, blockage of the lumen of a vessel by an embolus or thrombus.
The cause of atherosclerosis is the deposition of cholesterol in the inner layer of the artery. A blood clot forms due to increased blood viscosity. This condition often occurs against the background of concomitant diabetes mellitus and tumor formations. A cerebral infarction develops due to a sudden cessation of blood flow to the brain tissue.
With the development of ischemic stroke of the left hemisphere, sensory disturbances and motor disorders appear on the right. Damage to the right hemisphere is accompanied by speech disorders. General cerebral symptoms include dizziness, nausea, loss of consciousness, and in rare cases, coma. Specific signs of ischemic stroke are considered to be a decrease or complete loss of sensitivity in the right half of the body, limited or absent movements in the limbs, problems with swallowing, and drooping of the corner of the mouth.
Among the main causes of hemorrhagic stroke are:
- uncontrolled arterial hypertension;
- excessively thin blood;
- congenital deformations of the vascular wall.
Rupture of blood vessels with subsequent leakage of blood into the brain cavity most often provokes a sharp rise in blood pressure. In addition to the listed etiological factors, aneurysm, traumatic brain injury, physical or emotional stress can cause hemorrhagic stroke.
Hemorrhagic stroke is characterized by a sudden and rapid onset. Symptoms include severe headache, rapid breathing, confusion, and possible development of coma. The skin becomes cold to the touch, the corner of the mouth droops, and blood pressure rises. Against the background of hemorrhage in the brain, the tone of the muscles of the limbs decreases, strabismus may appear, the pupils dilate, and swallowing is impaired. Hemorrhagic stroke has a less favorable course and is often accompanied by complications.
An extensive stroke differs from a localized form of the disease. They consist in the fact that other types of strokes are characterized by blockage of blood vessels in the brain (ischemic type of disorder) or hemorrhage (hemorrhagic), in which large vessels are damaged, and with an extensive stroke, the lesions are localized in several parts of the brain.
Because of the extensive damage to the brain, patients with a major stroke have little chance of survival, and survivors have little chance of regaining lost function.
Precomatose states during stroke
When a coma does not develop immediately, but over several hours, signs of its development can be noted:
- the patient is conscious, but does not seem to understand what is happening to him, he is stunned;
- he complains of pain in his head, he feels sleepy;
- there is an increase in temperature;
- general weakness, impaired movement in the limbs, their coordination;
- speech disorder;
- partial memory loss;
- delirium, confusion;
- vomiting, sometimes convulsions.
Often a precomatose state is accompanied by memory loss
These are the symptoms of so-called precomatose states:
- Stupor. State of stun, lack of understanding of what is happening.
- Somnolence. A state reminiscent of sleep, but the patient’s eyes can be open, with great difficulty you can rouse him, but he immediately stops reacting to others again.
- Sopor. It is not possible to wake the patient, but his corneal and swallowing reflexes are preserved, and he can open his eyes.
Unfavorable signs during the development of a coma are: different diameters of the patient’s pupils (anisocoria), poor reaction to light and the “doll’s head and eyes” symptom.
This reflex, also called oculocephalic, occurs when the patient's head is turned to one side and the eyes move in the opposite direction. This indicates damage to brain stem cells.
Some authors do not distinguish precomatose states, but consider them to be the first degree of coma. Already with the development of a precomatous state, the patient’s chances of survival are significantly reduced and amount to 30–85%.
Prevalence and development
According to statistics, more than 400 thousand patients with this diagnosis are registered in Russia every year, and 35% of them die. Around the world, there are approximately 12 million people affected by this disease every year.
A major stroke develops due to the formation of blood clots in large vessels. They cause either narrowing of the lumen or rupture of the vessel. In both cases, the disease develops.
The disease is dangerous for any age category (except children), but the causes of its occurrence and risk factors vary slightly.
- Young people (up to 40 years old). At this age, hemorrhagic major stroke is more common. Young people who abuse drugs and cigarettes are at risk.
- Middle-aged people (40-60 years old).
Men aged 40-50 years are more susceptible to this disease than women, but by the age of 60 the rates level out. The thing is that men aged 40-50 years are 19% more susceptible to atherosclerosis than women. By age 60, this percentage drops to almost zero. - Elderly people (over 60 years old).
At this age, the risk of occurrence is very high (increases almost 18 times). In people over 60 years of age, plaque forms on the inner surface of blood vessels, which leads to blockage or rupture and subsequent bleeding. Heart disease leads to the formation of blood clots. In older people, blood pressure can be high for a long time, which eventually leads to rupture of blood vessels.
People with diabetes and heart disease are more likely to have a stroke. Any vascular pathologies and heart diseases (blood flow disorders) also increase the risk of developing the disease.
Stupefaction: what is this condition, a moderate and deep sense of consciousness in the head
Impaired consciousness is expressed in quantitative and qualitative changes.
Towards quantitative syndromes
disturbances (depression) of consciousness include: stupor, stupor, coma.
Quantitative disturbances of consciousness (depression of consciousness) develop due to morphological or pronounced metabolic changes in the brain, and are accompanied by a decrease in the level of wakefulness, motor activity, intellectual functions, up to complete depression and switching off of consciousness.
Total information
Rupture of a blood vessel. Hemorrhagic stroke is an acute emergency condition that occurs when blood penetrates from the vascular bed into the substance of the brain, under its membranes, or into the ventricles. Compared to ischemic stroke, it occurs in only 15%, and in Finland and Japan it is twice as common as in European countries.
Stun
Stun
- a decrease in consciousness in which limited verbal contact with the victim is maintained against the background of an increase in the threshold for perception of external stimuli and a decrease in one’s own mental activity.
Moderate stun
accompanied by slowing down, difficulty, impoverishment of mental activity, and a decrease in the ability for active attention.
Verbal contact with the victim is preserved, but answers to questions are delayed; sometimes it is necessary to repeat the question or pat the victim, who carries out the commands correctly, but slowly.
The patient is lethargic, quickly exhausted, his facial expressions are impoverished, his motor reaction to pain is purposeful, orientation in his own personality is preserved, orientation in the area, and especially in time, may be impaired.
Deep Stun
accompanied by constant drowsiness with rare episodes of motor activity, a sharp difficulty in mental activity.
Verbal contact with the victim is severely difficult, answers can only be obtained after persistent requests, they are monosyllabic in nature - “yes”, “no”, while the victim is able to provide his information: full name, age. It is possible to repeat the same word multiple times.
The victim is able to follow basic commands: open his eyes, show his tongue, etc. The coordinated defensive reaction to pain is preserved, but orientation in place and time is absent.
Nullification
(cloudy consciousness) - a mild degree of stupor, can be observed in the first stages of stun, reminiscent of a state of mild alcoholic intoxication - the victim experiences carelessness, lability of consciousness, absent-minded attention, while the victim may give answers to questions after a while and at random.
Doubtfulness
(state of half-asleep) - is a type of stupor, characterized by minimal motor activity.
The victim lies motionless with his eyes closed, makes no complaints, speech contact is minimal, only with persistent external influence. The patient gives correct answers to simple questions, but does not understand complex questions.
The patient can be brought out of a state of doubt for a short time with the help of persistent external stimuli.
First aid for stunning:
- Treatment of the underlying disease.
- Normalization of electrolyte metabolism, elimination of signs of dehydration if present.
- Normalization of acid-base status.
- Detoxification therapy.
- Normalization of metabolic processes in the brain. Nootropic drugs are prescribed for this purpose.
Restoration of motor functions
It is advisable to begin work on the rehabilitation of motor activity from the first days after the ONMC manifesto. It all starts with placing the sore limbs in a certain position. At the same time, they are secured with the help of a splint or sandbags.
The dominant role in restoring motor activity of the limbs belongs to the exercise therapy complex. Methods of its implementation, in addition to position therapy, gymnastics with passive exercises and learning to walk, include special sets of exercises that are aimed at different muscle groups.
Massage is no less important.
The use of modern biofeedback simulators, as well as verticalization systems, is relevant - their use allows you to significantly reduce the time required for the rehabilitation of motor skills.
At home, people also undergo rehabilitation and take medications, thanks to which they can achieve what was not done in terms of restoring lost functions in a medical institution.
It is clear that only with the help of medication it will not be possible to fully restore motor activity - it is necessary to perform a whole set of exercises, however, the patient makes the main progress in this direction in a specialized rehabilitation center, where there is all the necessary equipment. At home, he simply “polishes” his restored skills.
Sopor
Stupor is a deep depression of consciousness in which the victim retains coordinated defensive reactions, opening the eyes in response to stimuli.
The victim lies with his eyes closed; he can be briefly brought out of a drowsy state.
In this case, the patient is motionless or makes automatic stereotypic movements, reaching with his hand to the place of application of painful irritation, and a painful expression on his face may appear as a pain response.
Coma is a complete shutdown of consciousness without any signs of mental life, while the victim cannot be brought out of this state with the appearance of any signs of mental activity.
- Moderate coma
(coma I) - the victim has a preserved reaction to painful stimuli (flexion and extension movements of a dystonic nature), while protective motor reactions are not coordinated, the patient does not open his eyes, pupillary and corneal reflexes are preserved, abdominal reflexes are depressed, tendon reflexes are variable. Increased pathological foot reflexes and reflexes of oral automatism. - Deep coma
(coma II) - there are no reactions to external stimuli, various changes in muscle tone are observed, spontaneous breathing and cardiovascular activity are preserved even if they are severely impaired. - Terminal coma
(coma III) - bilateral mydriasis, diffuse muscle atonia, severe disturbances of vital functions, respiratory rhythm and frequency disorders, apnea, tachycardia or bradycardia, blood pressure is not determined.
Characteristics of the condition
Stupidity refers to quantitative syndromes of impaired consciousness. Such conditions develop as a result of a sharp change in metabolism in the head and are characterized by disruption of the sleep-wake cycle. The state of stunning always leads to a decrease in motor activity, up to absolute inhibition and switching off consciousness.
Stunning is a slowing down of all mental processes and disruption of verbal and visual contact with the outside world.
Typically, mild and moderate stunning are temporary conditions resulting from certain medical conditions. A healthy person can also feel a feeling of stupor: this can be caused, for example, by regular lack of sleep. In this situation, the patient needs to get some sleep and establish a work-rest routine.
Causes of stupor also include:
- traumatic brain injuries;
- intoxication due to taking medications;
- stroke;
- oxygen starvation of the brain;
- poisoning due to an overdose of sleeping pills;
- complication of diabetes mellitus;
- severe bacterial and viral infections: meningitis, viral hepatitis, encephalitis;
- heat or sunstroke;
- dehydration and lack of electrolytes;
- tumors or metastases in the head;
- electric shock;
- alcohol poisoning;
- drug overdose;
- seizure or epilepsy;
- severe allergies.
Stupidity is most often a symptom of the disease; it is often confused with another disorder of consciousness - delirium. The clinical picture for both syndromes is similar, however, with delirium, vivid delusional hallucinations occur, which are not inherent in the state of stunning.
With progressive deafness, it is extremely important to establish the cause of the syndrome.
To do this, a comprehensive diagnosis is carried out:
- visual examination of the patient: measurement of pressure, temperature, pulse, analysis of pupil movement;
- cardiogram for heart rate analysis;
- chest x-ray;
- blood and urine tests;
- determination of biochemical indicators of liver function;
- X-ray of the skull if a head injury is suspected;
- electroencephalography to determine the level of mental activity;
- toxicological analysis for intoxication;
- Ultrasound of the vessels in the head that supply the brain.
The most informative answer is provided by computed tomography or MRI. Regardless of the stage of deafness, the patient must be hospitalized in the neurological department.
Diagnostic approach
Diagnosis comes down to the study of clinical symptoms that can be detected during examination of the patient.
Pulse and pressure are measured, corneal and tendon reflexes, muscle tone, response to pain, and more are checked. During the initial examination, subcoma is distinguished from stunning and coma.
Then specialists determine what caused the person to fall into stupor. To do this, the patient is examined to find: head injuries, hemorrhages, alcohol odor, rashes, injection marks, and more. Body temperature, blood pressure, and blood glucose levels are measured. An electrocardiogram is taken.
Next, medical records are studied, the patient’s personal belongings are examined, relatives are interviewed, and other activities are carried out in order to find out about the patient’s other diseases, such as diabetes, liver failure, and epilepsy.
Source: //medspina.ru/kosti-i-sustavy/oglushenie-pri-insulte.html
Rehabilitation and prevention of complications
Full recovery after a major stroke is only possible if the patient is young, does not have serious illnesses, and important centers are not affected. This happens in 3-5% of victims.
Rehabilitation after a major stroke has the following goals:
- if possible, restore impaired functions (whether the brain is restored depends on the severity of the pathological process);
- provide the patient with adequate care (prevention of bedsores, prevention of diseases caused by a sedentary lifestyle);
- social adaptation (it is necessary to teach a person to live with the disorders that have arisen, to find something to do to prevent depression)
- the work of exercise therapy doctors, speech therapists and other specialists.
Whether it is possible to recover from an attack or whether a person will remain disabled forever depends on many factors. And in most cases, with large cerebral injuries, even with good care and competent actions of doctors, recovery is impossible.
What can cause illness in an elderly person?
Doctors say that a stroke can occur at any age, but the likelihood of it happening is higher in older people, because they most often suffer from diseases that cause problems with blood vessels. These include:
- Arterial type hypertension. Most often, older women and men experience high blood pressure, which is practically incurable, so stroke after 80 years is a common occurrence.
- Kidney diseases.
- Disturbances in the functioning of the endocrine system.
- Diabetes of any type and vascular aneurysm.
- Atrial fibrillation, which is often diagnosed in older people. A blood clot in the heart easily travels to the brain and causes a stroke.
- Rheumatism.
- Any viral disease in severe form.
- Increased cholesterol levels, which provokes the formation of blood clots in blood vessels.
- Sedentary lifestyle. It cannot be classified as a disease, but it becomes the cause of their development. Someone can live for years without getting a stroke, while others end up in a hospital bed within a month of this lifestyle.
Stroke in old age is most often ischemic, when a blood vessel is blocked and circulation to the brain is disrupted. But a hemorrhagic stroke, which ruptures a blood vessel, leading to bleeding in the brain tissue, is also possible.
This is not to say that there are no age-related characteristics of stroke. So, the consequences for people aged 30 years and 80 years will have some differences:
- The clinical picture of the disease in a stroke over 70-80 years of age will be incredibly severe, and it is precisely this course of the disease that is a direct threat to the patient’s life. The chances of survival are minimal, because death occurs in more than 85% of patients, especially if it is a major stroke.
- Forecast. An older stroke survivor will always have a worse prognosis for regaining body function than a younger person. The saddest thing is that the signs of a stroke are primarily ignored by the patient himself for fear of upsetting the family. And this reduces survival and treatment of the disease to nothing.
- Diagnosis of ischemic stroke in the elderly is more common than hemorrhagic stroke. They are also more likely to have a major stroke than patients aged 30-40 years.
The cause of stroke in old age is most often vascular atherosclerosis, because with it atherosclerotic plaques close the blood lumen. A blood clot torn off by blood enters the brain, provoking an attack. A similar situation develops with atrial fibrillation. Often, vascular atherosclerosis can provoke dozens of micro-strokes per year in a patient, the attacks of which are invisible.
Survival in such a situation is almost impossible, because if the disease is not treated for such a long period, it will lead to a massive stroke, which at this age ends in death.
Important! You can prevent a major stroke if you quickly respond to the following signs of an impending illness:
- on the left or right the body goes numb, either entirely or partially;
- in a conversation, it is difficult for other people to understand an elderly person;
- Vertigo becomes common and even leads to falls or decreased vision.
A stroke at 80 years old, the prognosis of which will be positive, is a quick response to the symptoms of the disease and timely treatment. If a grandparent has a hemorrhagic attack, the symptoms will be as follows:
- severe headache accompanied by rapid breathing and wheezing;
- strong, intermittent heartbeat, leading to fainting or near-fainting;
- blood pressure rises sharply, while the face becomes very red;
- limbs and facial muscles go numb;
- the patient feels sick and vomits.
Important! Signs of this type of stroke develop rapidly, so the patient usually loses consciousness at the beginning of the attack.
Depending on the area of the brain where the hemorrhage occurred, the patient may lose hearing or vision, and if it is a major stroke, seizures may begin and a coma may occur.
If, for example, an ischemic stroke occurs on the right side, the symptoms will be as follows:
- severe headache with vomiting and nausea;
- it is difficult for the patient to make any movement due to almost absolute weakness;
- visual function decreases, often the picture bifurcates;
- vertigo with impaired spatial orientation;
- memory lapses, disturbances of touch and speech.
Important! Time in the case of ischemic stroke is extremely important, because the symptoms develop gradually and become acute in 5-6 hours.
Cerebral hemorrhage and its outcomes are always individual for each person, as is treatment. But most often, a stroke has 10 consequences, and how the patient will be treated depends on them:
- The body can be paralyzed either partially or completely.
- Parts of the body, in particular limbs, become numb and cease to be felt.
- The patient cannot walk or navigate in space.
- Speech is difficult or completely absent.
- There is no swallowing function.
- Loss of hearing function, either partial or complete.
- Mental disorder.
- There is no control of urination and bowel movements.
- The patient needs constant monitoring and care.
- Death.
It is impossible to say what consequences a particular patient will have after a stroke. There are elderly people who lived happily after it, and there are those for whom the prognosis was unfavorable. Treatment and prognosis can be adjusted by assessing the presence of the following signs:
- If the cause is extensive hemorrhage occurring in the center of the brain, then the prognosis is death.
- Survival among those previously diagnosed with hypertension or atherosclerosis is usually minimal or with the most severe consequences.
- The prognosis is no less bad if the patient falls into a coma caused by swelling in the brain.
- Relapse is 100% fatal.
Treatment and rehabilitation can be effective if the following factors are observed in the patient:
- laboratory tests confirmed that the hematoma is small;
- there was no loss of consciousness;
- diseases of the cardiac system, atherosclerotic plaques of blood vessels in the neck and head have not been diagnosed;
- blood pressure is within standard values.
How positive the prognosis will be depends on the timely provision of qualified medical care. If this is done in the first six hours after the onset of the attack, then you should not prepare for the worst manifestation of the post-stroke condition.
It is the skillful and prompt actions of doctors that guarantee life and a positive prognosis for an elderly patient. Ischemic stroke always begins with transistor attacks, and if they are recognized in time, the development of pathology of cerebral circulation can be avoided, which often causes death or coma.
Treatment
If an extensive cerebral infarction is diagnosed, treatment begins immediately. The patient is hospitalized; if the condition is severe, he is transferred to intensive care. Support and correct basic vital functions. If the person cannot breathe, tracheal intubation is performed and a ventilator is connected. Doctors monitor the pressure and install a catheter in the bladder. Solutions are administered and, if necessary, parenteral nutrition is provided.
If the patient has pulmonary edema, then glucocorticosteroids (Prednisolone) are administered. To reduce areas of tissue death and save the viability of brain tissue, hemodilution is performed with a solution of rheopolyglucin, which thins the blood. The drug Trental improves cerebral circulation. They also normalize heart rhythm.
Important information: How long do they live after a repeated (secondary) stroke and what are its consequences in men?
To prevent the development of thrombosis, thrombolytics and anticoagulants (Heparin) are administered. Be sure to monitor the blood coagulation system to prevent bleeding. They restore the functioning of nerve cells with the drugs Cerebrolysin and Cortexin, which improves the motor ability of the affected limbs.
The operation is prescribed if the aorta ruptures and a cerebral hemorrhage occurs. During surgery, the accumulation of blood is removed.
Rehabilitation
After competent comprehensive treatment, the patient is indicated for rehabilitation in order to restore lost functions of the body and systems. Doctors don’t even talk about the complete restoration of all lost abilities. But with certain efforts on the part of doctors and relatives, the patient’s condition can be significantly improved. The complex of rehabilitation measures usually includes:
- Drug therapy to maintain vascular elasticity and restore blood flow.
- Massage. Aimed at restoring blood circulation in paralyzed areas of the body.
- Physiotherapy. Helps to recover, strengthens the muscles of paralyzed limbs and returns them to motor activity.
- Acupuncture. Allows you to achieve a good general strengthening effect.
- Diet. The patient's diet should consist of lean meat and fish, plant foods and dairy products.
- Fresh air.
Important!
The recovery process can last from one month to 2 or more years, depending on the extent of the patient’s brain damage.
What does the patient's life depend on?
The following factors influence a favorable prognosis for survival after a major stroke:
- Age category of the patient. After 65 years of age, the risk of death increases significantly.
- What concomitant diseases caused the cerebral hemorrhage?
- Primary attack or repeated. If a stroke has previously occurred, the patient has a greater than 90 percent chance of dying.
- Type of disease. In the hemorrhagic form, it is important in which area the hemorrhage occurred: in the brain tissue (intracerebral stroke) or between the membranes (subarachnoid).
- What brain structures were affected (damage to vital segments leads to death in 95 percent of cases).
- What body functions will be lost, and in which vessel the damage occurred (if a large vessel ruptures, the chances of survival rapidly decrease).
- Area of hemorrhage.
- How quickly assistance was provided, and whether the patient received additional injuries, for example, due to a fall.
- Is consciousness retained or has the patient fallen into a post-stroke coma, in which the likelihood of recovery is reduced to zero.
- Is there swelling of the brain matter?
Each of these factors affects a patient's life after a stroke. If we take into account patient survival statistics, about 25 percent die in the first days after an attack, and half of patients with this diagnosis die within the next year.
Approximately 5% of patients recover their condition and health after a major stroke. But about a quarter of them will suffer a second, more dangerous attack in the coming year.
A favorable prognosis can be expected in people under 45 years of age who have not previously shown signs of cerebrovascular accident.