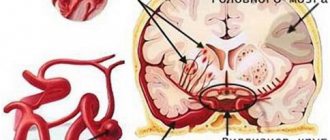
Strokes are severe lesions of brain tissue caused by acute disorders of cerebral circulation. Against the background of prolonged spasm of the great vessels or their blockage, the ischemic form develops, and with rupture of the vascular wall and subsequent hemorrhage, the hemorrhagic form develops. In the first case, the symptoms may increase gradually, but in the second they always appear abruptly. At the same time, cerebrovascular insufficiency gives quite serious complications, one of them is paralysis and impaired fine motor skills after a stroke.
The recovery of such patients takes a very long time, but rehabilitation measures are needed as early as possible. And they need to be done under the supervision of experienced doctors. The specialists of the Verimed clinic will help the patient return to a full life.
Paresis after stroke
Paresis after a stroke is a consequence that manifests itself after a cerebral hemorrhage and represents partial paralysis. Basically, unilateral paresis occurs, it is called hemiparesis.
About 75% of people who have had a cerebral infarction suffer from this consequence. Its main manifestations include: sensations of malaise in the upper and lower extremities. People with incomplete paralysis have problems performing everyday activities: eating, moving, monitoring personal hygiene, using a variety of objects.
Clinical picture
One of the classifications of lesions of incomplete paralysis is hemiparesis of the arms and legs.
Paresis of the lower extremities can lead to symptoms such as:
- lack of coordination in space;
- loss of balance;
- difficulty in movement.
Paresis of the upper limbs leads to muscle fatigue and the inability to use any objects without assistance.
A certain part of the brain is responsible for our every movement and activity of any organ. If the blood supply to this area is disrupted, the body loses the ability to resume this function, which is how paresis occurs during a stroke.
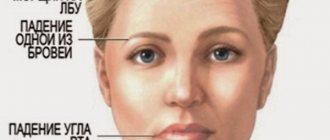
The left side of the brain is responsible for speech function. Due to circulatory disorders in the left hemisphere, right-sided paresis appears. Deviations of already formed speech may also appear.
Left-sided paresis can occur in a person as a result of injury or as a consequence of a massive stroke that damages the right hemisphere. It is responsible for human attention and memory.
In case of damage to the central motor neuron, central paresis manifests. Central paralysis is mainly characterized by: muscle spasticity, increased reflexes and an expansion of the range of their action.
Another manifestation of paresis after a stroke is spinal paresis.
Our boarding houses:
Treatment
You can improve your condition after incomplete paralysis, which occurs due to a cerebral hemorrhage, if you consult a doctor in a timely manner. To restore strength, a set of physical exercises, pharmacological agents, and changes in everyday life are used.
By using a variety of drugs, a long-term effect is achieved - maximum restoration of lost body functions. Sometimes it is worth spending more than one month or even a year on such rehabilitation.
Treatment methods
Poor circulation in the brain is already a fairly serious disease, but paresis after a stroke is difficult to rehabilitate, especially if it affects the central neuron. After incomplete paralysis, it is very difficult and often almost impossible for a person to return to his past life.
To improve the functioning of the upper and lower extremities, a physical therapy complex is used, which includes: daily exercises and stretching. All exercises are aimed at involving the affected parts of the body in everyday life. Gradually, the patient needs to try to use and strain the injured limbs more and more.
The first time physical therapy should take place in a medical institution, and only then the complex can be used at home with regular visits to the doctor and adjustment of exercises necessary for rehabilitation
The regimen and method of therapy directly depend on the degree of damage and the capabilities of the affected area of the body. Therefore, only a doctor can prescribe conservative treatment.
In addition to physical therapy and pharmacological agents, electrical stimulation is used for paresis after a stroke. This procedure is necessary to improve the activity of the affected areas, increasing the range of their functioning. Electrical stimulation is carried out using special pads. They are placed on the affected part of the body and pass an electrical charge. Electrical current helps move the paresis of the body parts.
Recently, transcranial magnetic stimulation is often used in medical practice - this is one of the types of electrical stimulation. It is not the upper or lower limbs that are affected by the electric charge, but the brain. Electric current enters the brain through the cortex and helps in the restoration of damaged parts that have not succumbed to irreversible processes.
Paresis after a stroke is mainly diagnosed using x-rays and computed tomography. First, the doctor must examine the patient, study the history and symptoms that bother him.
Prevention
Recovery from incomplete paralysis is not yet complete recovery. Clinical symptoms of the disease may recur. To prevent this from happening, there is prevention, which includes:
- normalization of physical activity;
- absence of dust in the room in which a person resides;
- avoiding hypothermia;
- timely treatment of other diseases;
- Seeing a doctor if you have an infectious disease or neurosis.
Paresis after a stroke, like hemorrhage itself, is a rather difficult process that requires long-term rehabilitation, especially in old age - there are nursing homes for this.
Placing a patient in a boarding house for the elderly is one of the keys to rapid recovery from circulatory disorders and eliminating the manifestations of incomplete paralysis.
The House of Kindness has new schemes and methods of treatment, as well as rehabilitation of patients after a stroke. In a nursing home, doctors and staff carefully monitor blood pressure and do everything possible to avoid repeated bleeding in the brain, the appearance of hemiparesis or plegia (complete paralysis).
In addition, patients live in cozy rooms with a specially designed individual nutrition plan for each.
What are fine motor skills?
Fine motor skills are clear, purposeful movements of the hands and fingers, controlled by the central nervous system. They are possible only with impeccably coordinated work of the brain, organs of vision and impulse-conducting nerves. There is an inextricable connection between motor activity and cognitive functions. Therefore, to fully restore fine motor skills after a stroke, not only the development of muscles and joints is required, but also exercises aimed at activating mental processes.
Paralysis of limbs as a consequence of stroke
Stroke refers to damage to individual structures or tissues of the brain. As a result, functional changes occur in this organ, which subsequently affect the body’s processes controlled by the nervous system. Stroke can be ischemic or hemorrhagic. In the first case, we are talking about restriction of blood flow of a certain origin, which leads to a decrease in tissue respiration, and conditionally becomes the cause of the development of necrotic changes in the future. In the second case, we are talking about hemorrhage in the brain tissue. Such a violation of the hemodynamics of the structures of higher nervous activity can result from a number of reasons.
When such hemorrhage occurs during a hemorrhagic stroke, the consequences can be very diverse. They depend on the location of the lesion and the functions of the anatomical structure that was damaged. The stronger the hemorrhage, the worse the functioning of this structure will be. Cases are often observed when the intensity of the work of a part of the brain not only decreases, but disappears. In such situations, large-scale and long-term rehabilitation measures are carried out, which are aimed at restoring such functions.
Ischemic stroke: consequences, violations
However, this fact does not mean that full functioning of the body from the moment of a stroke is impossible. Rehabilitation tactics, as well as timely initiation of therapy in the acute phase, will achieve some positive aspects, namely, partial restoration of function. And this is the main direction of rehabilitation, that is, to teach the patient to use the remaining functional reserves of the body to perform work or self-sufficiency.
Content
General characteristics of the consequences of stroke
With a stroke, the consequences are the result of damage to an area of the brain that is responsible for some function. This process is irreversible, because even if the patient is immediately taken to the intensive care unit, brain damage continues. It is almost impossible to stop this, although it is possible to reduce the size of the damage and save the patient’s life.
With a pathology such as ischemic stroke, the consequences should be differentiated into several categories. Among them:
- Disorders of the motor innervation of the limbs and areas of the body;
- Sensitivity disturbances in an area of the body;
- Speech disorders;
- Loss of vision;
- Damage to the auditory cortex and hearing impairment;
- Pathologies of regulation of vascular tone at the level of the brain stem.
Motor disorders in ischemic stroke
This category of consequences is irreversible or partially reversible if the extent of damage does not affect most of the precentral gyrus of the brain. This area is responsible for motor innervation, and therefore its damage causes central paresis of a muscle or an entire limb.
Types of paresis during stroke:
- Right-sided hemiparesis;
- Left-sided hemiparesis;
- Monoparesis of the limb;
- Tetraparesis of the limbs.
Limb paresis is a loss of motor innervation, due to which the patient cannot make normal and coordinated movements in the joints. Moreover, if a right-sided stroke is noted in the brain, then left-sided paresis is noted in the periphery. Recovery from this lesion is lengthy and requires a number of physiotherapeutic and massage procedures.
Sensory impairment is also an example of consequences after a stroke. As a result of the lesion, the postcentral gyrus, that is, the highest cortical analyzer of all types of sensitivity, suffers. As a result, the patient does not feel touch, temperature, or pain in the affected limb. Therefore, with a pathology such as a stroke, the disability group is assigned in most cases, since the patient cannot perform physical or specialized work.
Speech disorders
This category of consequences may occur due to damage to the speech center or motor speech center. For this reason, the patient is unable to engage in full speech contact. In the future, this trend continues, which needs to be corrected as part of rehabilitation measures. These include learning audiological language and communicating through it.
Visual impairment
Due to the excessive susceptibility of the visual centers to ischemia in a pathology such as stroke, the prognosis is unfavorable. Damage in the occipital region is a key factor in the failure of the visual centers, and therefore the patient cannot see for the rest of his life. In this case, the process is often bilateral, since the cortical vision analyzers are located in close proximity. Therefore, with a hemorrhagic stroke, bilateral vision loss is observed, while the ischemic variant of the pathology often affects one eye.
It is also worth noting that the visual pathways intersect in a unique way. From one eye, the outer part goes to one cortical analyzer, and the inner part goes to the other. Therefore, if the visual cortex is damaged on one side, the outer segment of vision (temporal) of one eye and the inner (nasal) of the other eye are lost. This condition is called quadrant hemianopsia and is characterized by the absence of binocular vision, that is, the ability to identify three-dimensional objects and measure the distance to them.
This category of consequences of a stroke is more rare and manifests itself, as a rule, together with a defect of the vestibular apparatus. At the same time, this is quite painful for the patient, because nystagmus appears. This can be seen even at the stage of resuscitation or preclinical course, that is, until the person receives help. With a pathology such as a stroke, therapy cannot restore damage to the auditory analyzer, and therefore the patient will experience this condition for life.
Vascular disorders
This group of consequences, as a rule, does not manifest itself for a long time, since as a result of damage to the vasomotor center, a person dies after being disconnected from life support devices. Loss of this function does not allow the patient to live independently and therefore leads to death. This is one of the most dangerous consequences of a stroke.
Peripheral and central paralysis
Post-stroke paralysis of the lower extremities, depending on the genesis of the lesion, can be central or peripheral. In the first case, the pathological condition is manifested by conditions under which the muscle fibers are in a state of constant tension. Depending on the location of the greatest damage, one or another group of motor fibers may be impaired to a greater or lesser extent. This occurs due to damage to the first neuron of the reflex arcs for this purpose. This anatomical structure is located in the gray matter of the brain, so the etiology of the disorder is clear. Central paralysis keeps the muscles in constant hypertonicity. In the absence of rehabilitation therapy in this direction, spasticity develops in such places over time, up to a complete loss of functional abilities . Therefore, such paralysis is also called spastic.
Peripheral paralysis is also a consequence of the onset of brain damage due to disruptions in its hemodynamics. Unlike central paralysis, in which nerve impulses can enter the tissues in a pathologically transformed form (generated by the spinal cord, not the brain), with peripheral paralysis the signals do not reach the affected area at all. This leads to a complete absence of motor activity in such an anatomical region, or a significant decrease in its functional potential. In such cases, restorative therapy and rehabilitation, which are aimed at improving the general condition of the patient, are not always effective.
How to cope with manifestations?
Spasticity is the first to affect a person who has lost motor activity. This is due to prolonged immobility of the hands - the muscles lose their elasticity and shorten slightly. Paralysis further enhances the tone.
The resulting spasticity hinders movement; to improve the condition, it is recommended to follow the rules:
- the position of the hands must be constantly changed;
- carry out special exercises throughout the day to stretch muscles;
- due to the fact that low ambient temperature causes increased spasticity, the patient’s living room should be quite warm;
- getting used to cold temperatures is necessary, but is done gradually;
- The massage is carried out exclusively with patting movements.
Restorative gymnastics should be both active and passive. The latter is performed with an assistant. For this reason, close people play the main role in the rehabilitation of the patient.
How to prevent the development of paralysis
The development of paralysis, which occurs as a consequence of the post-stroke condition, can be prevented by specialized rehabilitation therapy. Immediately after an injury to the blood circulation of the brain tissue, many disturbances in the functional activity of certain parts of the human body usually occur. This causes the patient to remain on bed rest. Rehabilitation therapy is carried out during this period, but it is largely pharmacological. Physical activity of even low intensity can harm the general condition, since in many cases during such a period there is no complete stabilization of vital signs.
Speaking about how to develop a paralyzed leg after a stroke, starting from a few weeks after the onset of the disease, it is worth noting that during this period the range of means of rehabilitation therapy expands significantly. Drug treatment continues, but it is often combined with passive exercises of the affected limbs. This refers to the use of physical activity of moderate intensity, which is carried out using external mechanical influence. Since the patient in such conditions is too weak and cannot perform such actions on his own, such passive gymnastics is carried out with the help of the patient’s relatives or medical staff of the medical institution where such a patient is located.
2-3 weeks after a stroke, other methods of rehabilitation are added to drug therapy and passive gymnastics. This refers to the use of electrophoresis, magnetic procedures, laser light, acupuncture, hirudotherapy (leeches) and the like. The use of such restorative methods helps to improve the general condition and accelerate regeneration processes in the affected areas.
The process of restoring the body and preventing the occurrence of paralysis during the period of post-stroke recovery requires a fairly long rehabilitation time. At the same time, patients learn to walk again, since such functions are often lost after injury. Training often takes place with the participation of outside help. In this case, moral support and participation in the recovery process of the patient’s relatives is important, helping to improve the general psychosomatic state of the patient.
Patient care
In case of left-sided paralysis after a stroke, not only rehabilitation therapy plays an important role, but also patient care. This is the task of the medical staff and the patient’s relatives. What do we have to do:
- Regularly change the position of the victim to prevent bedsores and pneumonia.
- The paralyzed person needs to be turned over and rubbed every 2.5 hours.
- The bed must be constantly straightened to avoid wrinkles and changed if it is wet.
- Arms and legs should not hang from the bed, otherwise there will be joint deformation. You can place a chair next to the bed if your limbs fall down.
In case of paralysis, the patient must undergo long-term rehabilitation. No one can give an exact time frame for complete recovery - this is an individual process that depends on many factors. In difficult cases, patients lose their ability to work and become disabled. The sooner treatment is started, the higher the likelihood of a positive outcome with complete restoration of motor functions.
Massage of a paralyzed leg
Massage is an important component of the rehabilitation process after a stroke. Its use makes it possible to prevent or to a certain extent neutralize paralysis of the legs, as well as other consequences of this kind that arise after brain damage. Sessions of the procedure also have a preventive effect on the onset of certain pathologies in the post-stroke period, improve overall well-being, equalize hemodynamic parameters, etc.
Massage sessions are recommended not immediately after a stroke, but after some time, when the body begins to recover on its own. If we are talking about ischemic pathology of the brain without significant complications, restorative therapy can be carried out for 2-4 days . After hemorrhagic pathology, massage is carried out no earlier than 6-8 days. The number of sessions and the individual characteristics of their implementation are determined depending on the patient’s condition and are prescribed by a rehabilitologist.
The first procedures should last a few minutes. Gradually, long-term can increase to 15-20. The course lasts at least 10 lessons. Usually the number reaches 15 or even 20. The sequence of massage movements should be the same each time to achieve a greater therapeutic effect, and performed systematically, that is, at regular intervals.
Before performing massage procedures on a paralyzed area of the body, the patient must take a shower and then dry thoroughly. During the session in the room, you need to ensure that the temperature is maintained at a favorable temperature. This helps the patient relax. After the massage, it is recommended to rest for about 20-30 minutes so that the body regains the energy expended. After all, as a result of a severe injury, the body is very exhausted, and any physical exercise, even of low intensity, is perceived by it as a significant load.
Text of the book “Life after a stroke. A real experience of recovery after a “strike”, accessible to everyone!”
Learning to get up and sit down
Simple everyday activities familiar to an ordinary person are very difficult to reproduce after a stroke. We have to restore, for example, the transition from a sitting position to a standing position, that is, standing up.
You need to stand up like this: before you begin to straighten your knee and hip joints and raise your pelvis, you need to tilt your body forward so that your shoulders are above the line of your knees, and your feet are moved back beyond this line. Then the lifting of the whole body will occur without much expenditure of strength and energy. If the paretic leg is not strong enough or the tone in it is too high, then it is necessary to help the patient by providing opposition at the knee level of the affected leg (with your knee, hand or object).
The reverse transition - from a standing position to a sitting position - is carried out in exactly the same way, but in the opposite direction: first the knee and hip joints bend, and then the body and shoulders bend forward.
This allows you to sit down gently, without shaking (“plumping”) of the entire body. Learning to walk
It is somewhat more difficult to learn to walk after a stroke.
Do you remember the funny children's poems by S. Ya. Marshak: “Once upon a time there lived a man with crooked legs, and for a whole century he walked along a crooked path...”? They also seemed funny to me for a long time, until it affected me personally. So, in order not to become such a character, you should thoroughly work on yourself, first by taking up walking.
A person who has had a stroke must be re-taught the proper mechanics of walking. They usually start with the skills of flexing the shin with a vertical position of the thigh. First, you need to fix the thigh and create a support for it. Only after mastering this movement can one learn to flex and move the hip forward with simultaneous free extension of the lower leg while dorsiflexing the foot.
In the first stages, all of these actions are performed only with the help of a loved one, who, sitting on a small bench, holds the thigh and straightens the lower leg of the stroke victim, and then accompanies him while walking, holding and lifting the lower leg using a bandage or other traction. Walking with a cane initially does not hinder such learning, but even facilitates it.
Spasm of the leg muscles makes it difficult to bend the hip and knee joints when walking. The gait in such cases is awkward, since great efforts are made to move the weakened leg forward. These excess forces will increase unwanted muscle tone in the paralyzed arm as well. The increase in spasticity in the leg will be facilitated by attempts to transfer body weight to the front of the foot rather than to the heel. There is no need to do this. When a paralyzed foot hangs down and turns inward, this may initially be due to primary muscle weakness, but if the necessary measures are not taken, this position may become fixed due to the development of contractures.
In addition, when standing and walking, many people place their body weight on the forefoot. As a result, the toes become so bent that walking and standing become painful. If you use soft rubber pads to spread your fingers wide apart, this will prevent or eliminate a spasm that has already occurred. Straightening the toes eliminates spasticity of the entire foot. The toes can be spread wide apart using rubber or fabric pads. In such cases, I used inserts between the fingers intended for pedicure.
It is very useful to train your step using the following simple device, the principle of which is similar to that of a sling or slingshot. Take an elastic rubber bandage 5 m long and tie it with both ends to the bed on either side of the headboard. A handkerchief in the form of a loop for the leg is tied to the middle of the bandage (it is also the place where it is folded). The affected leg is inserted into this makeshift fabric stirrup and the rubber bandage is tightened. Then, due to the resistance of the elastic material, the foot is pulled towards the head of the bed. The resistance force of the rubber can be adjusted using the end of the rubber bandage hanging down to the leg.
Feeling the hardness of certain areas of the foot, I kneaded them by rolling the foot on a piece of a shovel handle with a diameter of 5–7 cm. Then I replaced this improvised massager with a special massage-corrective roller.
Restoring hand function
Restoring normal function to the affected hand involves increasing its strength and making its movements more precise.
To restore the accuracy of hand movements, it is necessary to eliminate all phenomena of spasticity. Movement in the shoulder and elbow joints should be restored as much as possible first, since the muscles and tendons stretch from the shoulder to the hand.
The shoulder pain that people often experience after a stroke is not usually due to shoulder subluxation. These pains are caused by tension in the muscles and ligaments due to incorrect positioning of the arm and the inability to lift it. Therefore, in the first days after a stroke, measures should be taken to maintain the scapula in a free position. The condition of the upper limb, its functions and range of movements in the future depend on this. It is also recommended to raise the arm up and rotate it outward at the shoulder joint. You should strive to keep your arms extended forward more often with your hands clasped and your palms turned outward. Sitting at the table and leaning on it with clasped hands, try to stretch them as far as possible across the table.
In the early stages of rehabilitation treatment, a paraplegic shoulder device may be needed to help prevent the muscles and ligaments that support the arm from becoming overstretched. To do this, you can use a roller made of soft material (a piece of cotton or woolen material, sponge rubber) with a diameter of about 10 cm. It is placed in the armpit of the paralyzed arm, including when in a vertical position.
It is not recommended to use a sling bandage. In this case, the elbow is bent, the arm is pressed to the body and turned inward, the palm is lowered (typical signs of a flexion spasm). As a result, spasticity in the arm does not decrease, but, on the contrary, increases, which increases the risk of developing subluxation of the shoulder joint. Moreover, in a bent position, the swelling of the arm increases. However, if the arm remains weak and hangs down when the victim sits or stands (the arm swells), a wide sling-like bandage can be used to support the elbow and the entire arm.
If the forearm muscles are sluggish, rough massage techniques and patting (to “wake up” the muscles), as well as vigorous acupressure of biologically active points located on the wrist will help - a few seconds for each point. If there is spasticity, acupuncture is effective; the massage should be stroking and squeezing.
A stroke victim should be taught to support, fix the paralyzed arm and move it in space from various positions, leaving the hand free to perform functional movements. I will describe the following useful exercises here.
• Pick up a stick, rope or rolled up towel. Holding it in front of the victim, teach him to grab and release it, to intercept the stick or towel with his hands from bottom to top. In this case, the paralyzed arm should be straightened and extended forward (anti-spastic position).
• Ask the victim to place his hand over yours (palms touching without pressure) and follow the movements made by your hand. To make this task easier for him, advise him to think about the mechanics of such movements in the corresponding joints. The patient's internal responses should be slow and clear. For example: “I think about my elbow... I look at it... I bend my elbow...” The victim’s assistant can say the same thing out loud. If the patient has difficulty following these commands, demonstrate the required movement yourself. It's best to start with a simple sequence of movements or a series of actions. Encourage the victim to independently repeat these movements many times.
• Give the victim various objects and plastic materials (for example, plasticine or modeling wax, molding clay, pieces of rubber of different shapes, balls of different sizes, etc.). This will allow him to regain experience in handling objects of different weights, shapes and structures, after which he will be ready to move on to practicing different ways of picking up and holding things. All exercises must be performed alternately with both hands.
The victim must learn to use the arm as a point of fixation for trunk movements (movement of the torso relative to the arm). For example, sitting on the edge of the bed and placing his feet on the floor, the patient raises his buttocks, straightening his arms, transferring his body weight to the paralyzed arm, which is in different positions, straightened at the elbow joint. With a healthy hand, he can perform various actions on the paralyzed side of the body and, conversely, with a paralyzed hand - on the healthy side. Both activate bilateral motor functions.
I did this. Above the doorway I attached a handle-bracket, into which I inserted a piece of rope 2 m long. Holding the ends of the rope with both hands, I pulled it through this bracket. The sore arm was secured with a loop to prevent it from falling. The purpose of this exercise was to learn to raise the arm as high as possible and keep it in a vertical position in a straightened state. At first, the diseased hand remained passive, then it “won” the healthy hand in this competition.
Then I changed this exercise somewhat - I began to perform it with my back to the rope and raising both arms behind my back.
My fingers remained naughty for a long time.
They could not take various objects - mugs, cups, plates, forks or spoons. At first I learned to move a stick with my hands using interceptions, then I tried to throw it up with my injured hand and catch it in flight. Diagnosis and restoration of hand functions
How to assess the condition of the hand
The condition of the hand is diagnosed by doctors by examining each of the five fingers. First, the hands are assessed at rest: if the fingers are closer to the extended position, then it is assumed that the extensors are stronger than the flexors. If the fingers are closer to the position bent into a fist, the flexors are most likely stronger. After this, the range of motion in all joints of the hand and fingers is studied, that is, whether the full range of motion is achievable, how easily the fingers bend and extend under the influence of external force.
Then muscle tone is assessed. If you quickly bend your fingers and they strongly “spring” into extension, the tone of the extensors is increased. If you lightly tap your fingers on the pads of the victim’s bent fingers (for extension), and in response the fingers clench into a fist, then the tone of the flexors is increased.
Active movements are then assessed. To do this, fully extend the fingers and ask the victim to bend them. The hand is completely bent into a fist and asked to open it.
After diagnosis, specialists draw up a recovery program. First, the mechanics of bones and joints are restored, then involuntary movements, after which you can engage in voluntary movements. The emphasis is always on those muscles that work worse. Strong (or stronger) muscles, according to experts, are pointless and harmful to exercise. If the fingers do not have the full range of passive movements, then you need to start with restoring these movements, but you cannot overdo it, since the hand does not like violence.
Warmth to the rescue
To eliminate contractures, with the help of external force (the hand of a loved one), the fingers must be fully extended and bent. Thermal procedures, such as paraffin baths or hot compresses, contribute to this.
The easiest way is to use hot water and a woolen cloth. To do this, take an old woolen scarf or handkerchief, dip it in hot (39–42 °C) water, squeeze it lightly and wrap your hand up to the elbow. Place cellophane and a blanket or piece of blanket sewn into cellophane on top. Leave this compress on for 10–15 minutes.
Immediately after this procedure, it is recommended to dry the skin, rub the entire hand, then rub each finger separately, then the hand (along the tendons), then the forearm (along the muscles and tendons, moving from the wrist to the elbow). Then each joint, starting with the nail phalanx, should be “unlocked” by gentle pulling and rotation. Then each joint is pumped: springy flexion is performed and straightening again. And it is recommended to do this 3-5 times for each finger joint. It is important to remember that the physical force applied should not be too strong.
Otherwise, the effect may be the opposite: injured tissues will tighten the contractures even more.
If the fingers are in a position of extreme flexion or if the voluntary strength of the flexors is greater than that of the extensors, only the extensors need to be exercised. That is, if the finger flexors are stronger, then it is not recommended to exercise the flexors so as not to increase spasticity.
Hard gloves for finger straightening
To avoid curling your fingers, you can use various devices in addition to the exercises. I will describe one of these passive devices that I used. It’s not at all difficult to make: you will need a small piece of plywood inserted into a cloth bag and a pair of old gloves. Both gloves with fingers spread out must be sewn on both sides to the plywood bag.
The principle of using this unique simulator is as follows. In the case where the flexor tone is higher, you need to strive to unclench your fist or not allow it to clench again. This is possible if the fingers are spread wide apart and pads made of foam rubber, foam, etc. are inserted between them. In my case, these were gloves fixed on a piece of plywood covered with fabric.
For severe spasticity, use a glove that allows you to place your hand, pressing it against the base with the inside of your palm and the pads of your fingers. When you have achieved some straightening of the fingers, use the glove on the other side of the base - so that you put the brush into it, orienting it with the back of your hand and the knuckles of the knuckles towards the plywood.
At first, you will have to put on such gloves with the help of someone else, then you will be able to do it yourself. As a result, the fingers gradually straighten.
This device should be worn as often as possible during the day, whenever possible (at least 30-60 minutes). It is very difficult to sleep with such a glove on your hand all night - for example, I could not.
Finger exercises
Finger exercises are very important when recovering from a stroke. The following finger exercises are recommended and should be done regularly if possible.
1. While sitting or lying down, place your fingers on your knees and spread them slightly. Start lifting one finger of both hands in turn. It’s okay if one arm doesn’t work yet, that’s why gymnastics is needed to restore its mobility.
It is suggested to start the exercise with the little finger, ending with the thumb, then go in the opposite direction. Repeat the exercise, depending on your success, 10–12 times. The less success you have, the more you will have to work.
2. While sitting or lying down, keep your fingers on your knees, spreading them slightly. Now twist each finger in turn (on both hands at the same time), first in one direction, then in the other. These movements are not entirely easy even for healthy people. But it is fine motor skills that improve brain function; it is no coincidence that such an exercise is useful for absolutely everyone. It is recommended to repeat it 7-10 times.
3. Connect the fingers of both hands into a lock and alternately lift the same fingers of both hands (thumb on the left hand, then thumb on the right hand, etc.), then in reverse order. Repeat the exercise 10-12 times.
4. Continuing to keep your fingers locked, make a “wave” with your hands. The elbows should also be involved in this exercise. The exercise time is 30–60 seconds.
To develop fine motor skills, it is very good to use a small “hedgehog” massage ball. The smaller the ball, the more effort you will have to expend when working with it, the greater the effect will be. The exercise consists of playing with a ball: you can throw it from hand to hand, spin it around your hands, or simply massage your palms and fingers with it. This workout should last at least 3-5 minutes.
Other devices will also be useful: rosary beads, copper balls with magnets for practicing finger movements, a rubber expander ring for developing strength in the hands (Fig. 4).
Rice. 4
Restoring everyday skills
Of no small importance is a group of exercises aimed at restoring skills in handling simple everyday objects - clothing, dishes, communications equipment, as well as various writing utensils. So, for example, the motor act of writing can be carried out on paper and a slate board, with a pencil, brush or chalk, in a lying, sitting or standing position, at different speeds.
When performing movements with the hand of a paralyzed arm, its elbow should rest on the table until normal muscle tone is restored in the arm. It is necessary to regularly train clenching the hand into a fist, bending (extending) the arm at the elbow joint, bending the hand at the wrist joint forward (backward), rotating the hand, folding the hands with the palms straightened and spread apart, including the thumb (the healthy hand helps the movements of the paralyzed hand ). You should also practice connecting the fingertips of both hands and pressing them on each other, rolling a cylindrical object (bottle, can, pencil, battery) with your palms, connecting the fingertips as if to grasp objects. It is also necessary to practice precise movements, including grasping small objects (for example, when building a toy tower from small component parts), pinching grips (as when grasping a pen).
In particular, it is better to practice wrist extension while sitting, with your elbows on the table. Both palms are joined and clenched, and the fingers are straightened. Extension of the paralyzed palm is trained. At first, these movements are performed passively with the help of the healthy hand, and then gradually more and more actively, and now the healthy hand provides increasing resistance. It’s good to stand at the table and roll an object made of some soft material along the table, pressing it with your palm. When the object moves away, the fingers straighten, and when it comes back, they relax and bend slightly. In the same position, the palm of the paralyzed hand is pressed against the surface of the table, all fingers are open and straightened. Then you need to straighten the hand and tear it off the table. The base of the palm should be left pressed to the surface.
Wrist flexion is trained by connecting the palms of both hands with straightened fingers. The hand of the affected hand is bent forward, the healthy hand is used to create measured resistance to its movements. The forearm of the paralyzed arm lies on the table, palm facing down. Then we bend the hand, raising the palm up and leaving the fingers in contact with the surface of the table.
It is helpful to transfer your body weight to your fingertips when you stand in front of the table. The pads of your fingers, including your thumb, should be pressed firmly against the surface of the table. Then you need to lean on your fingertips and gradually increase the load on them with the weight of your body, while controlling their position.
Finger pinch and spread can also be practiced by grasping a small ball tightly in your palm and then releasing it, opening your palm and straightening your fingers.
It is useful to hold a piece of some spongy substance (for example, foam rubber) in your healthy hand and pinch off small pieces from it with the fingers of your paralyzed hand. To grasp, the thumb and index, thumb and middle, etc. fingers are used in turn.
It is also recommended to roll a piece of elastic material between your thumb and index finger.
As you can see, there are a great many such useful exercises.
And you can probably come up with your own. A little ingenuity and you can do it! Prevention of recurrent stroke
Even if you feel well, never forget about preventing another stroke!
The likelihood of developing another stroke is very high, especially during the first year after treatment. And a second stroke in most cases (about 50%) leads to death. To avoid this, it is necessary to take strict preventive measures.
Be sure to use the capabilities of the currently widespread ultrasound diagnostic devices for blood vessels, including those feeding the brain. The first stage is Doppler ultrasound.
This is followed by
duplex scanning
- a method that allows you to evaluate the structure of the inner surface of the vessel, identify atherosclerotic plaques, analyze their volume and structure, highlighting those that can cause a stroke. The sensitivity of duplex scanning is higher, it gives a better image, and therefore the possibility of a mistake by a doctor who does not have the highest qualifications is also less.
Use drug therapy. Do not forget to control the structure of the blood, avoiding its strong thickening and possible thrombosis. Hirudotherapy and blood thinning medications will help with this. Such drugs, in particular, include aspirin
or its more expensive analogue
ThromboAss.
However, you should remember that aspirin tablets irritate the gastric mucosa and can, in addition to a stroke, give you an ulcer. There is also a point of view that the use of aspirin as a means of primary prevention is effective only in women over 45 years of age. This drug does not have a similar effect on men.
In addition to aspirin, medications such as Cavinton, Alisat, Trental, and Sermion prevent the formation of blood clots.
The effective impact of
tanakan,
, has already been discussed above.
I will also mention the expensive but very effective drug Plavix
tablets.
Remember to monitor your blood pressure and use medications to lower it daily.
Remember that from now on your destiny is to wear hats in hot and cold weather, avoiding overheating or hypothermia of your head, since poor circulation after a stroke has made you more vulnerable to temperature changes. Protect stroke-damaged limbs, which are already prone to chilly, from cold and frost.
You will have to avoid your previously favorite Russian bath or Finnish sauna - due to the high temperature effect on your body. By the way, bathing in the bathroom should not take place in hot water (within 29–34 °C).
It is necessary to monitor your body’s reactions during flights and long-distance travel, while staying in other climatic zones.
Lack of overwork and adequate sleep are the keys to full restoration of health. Avoid extremes. It is not at all necessary to monitor your blood pressure and the functioning of your body in general; you should not fall into panic and suspiciousness at minor deviations from the norm. On the other hand, you cannot completely give up control over the state of the body during its stabilization.
And one last thing. Pay attention to your psycho-emotional state. Constantly monitor your emotions and control them. Become kinder and more sympathetic. Put yourself in the shoes of others from time to time and try to understand what causes their irritation towards you. Once you find out the reason for the complaints against you, you may react to them completely differently.
We believe in God and pray to Him when we feel bad. But as soon as it gets better, we begin to forget about Him and then we again find ourselves vulnerable to various misfortunes. Remember this. Perhaps it's time to rethink your attitude towards religion.
Why does pain occur?
The most common symptom after a stroke is pain. It can have different localization, severity and characteristics of morphological manifestations, and also have a central and peripheral origin. Speaking about the last statement, we mean the anatomical part of the nervous system, the pathological focus in which causes a feeling of pain.
Pain in a paralyzed leg after a stroke is usually considered paretic. It expresses its greatest manifestations when the affected structures begin regeneration processes. From a morphological point of view, such unpleasant sensations occur when the brain begins to send nerve impulses to muscle fibers. The latter, due to their inability to function normally, act by corresponding pathologically altered mechanisms, which in turn cause pain in the paralyzed limb.
In general, such pain is a relatively good sign, as it indicates the beginning of the rehabilitation process. The feeling of such genesis can be enhanced by various external factors, such as movements, injuries, psychosomatic disorders, and the like.
Folk remedies for paralysis
Along with the use of rehabilitation and drug therapy, various traditional methods of combating complications of leg paralysis are often used. Most often these are substances of natural origin that exert their influence through external or internal contact with the affected organism.
Traditional methods of combating the consequences of a stroke include, for example, the use of:
- Medicinal plants from which tinctures or compresses are made. The second component of the mixture is most often medical alcohol.
- Milk, since it has a hypotonic effect, that is, it prevents the development of recurrent stroke. Use about 200 ml orally every evening before bed.
- A solution with mumiyo, marsh herb cudweed and valerian rhizomes. Fill with warm water and then infuse in a dark, dry place. Use warmed three times a day.
- A mixture of honey, mint and kombucha infusion. After preparation, apply in courses.
- Treatment with essential oils. For example, ylang-ylang oil or tea tree oil are added a few drops to a bath that is applied to the affected area.
This is not a complete list of drugs that are used for paralysis of the leg after a stroke. The effectiveness of this treatment, as well as its expediency, has not been proven to date. However, the use of such methods as additional ones improves the general condition of the patient, as well as the dynamics of the development of recovery processes. If traditional therapy is not combined with pharmacological therapy, as well as rehabilitation procedures, the effectiveness of such an effect is very doubtful.
One of the dangerous consequences of a stroke for a person is complete or partial paralysis of the body. The second option is easier to deal with, especially if the upper limb is paralyzed. We will discuss how to properly restore a hand after a stroke in the material below.
ethnoscience
For quick recovery from paralysis after a crisis, alternative medicine is also useful. They are not a panacea, and only enhance the effect of taking basic medications. Blood circulation is normalized, the immune system is strengthened, and the condition of the nervous system improves. Several popular and effective recipes:
Bay leaf. Grind fresh or dried leaves into powder. Pour three tablespoons of raw material into a glass of pure sunflower or olive oil. Leave for a week in a dark place. The prepared product is used to treat diseased parts of the body in the morning and evening.
Sage is used internally. For one heaping tablespoon of dry raw materials – 250 ml of boiling water. Leave covered for an hour. Filter. Drink half a glass in the morning on an empty stomach.
Any folk remedy should be used only as prescribed by a doctor. If side effects occur, stop taking and seek medical help.
Massage
For left-sided paralysis, one of the effective treatment methods is massage. During the procedure, the paralyzed part of the body is stimulated, pain is reduced, muscle tone is improved, and bedsores are prevented, which are inevitable with paralysis.
First you need to warm up the muscles with light massage movements. You can’t put too much pressure on the muscles or tap. Everything needs to be done slowly, smoothly. After heating the tissues, kneading and vibration are used. The massage ends with light strokes.
The direction of the massage should be along the lymphatic drainage. When working on the back, you should not touch the spinal column. The optimal duration of the procedure is 10-20 minutes.
Exercise therapy
The main task of rehabilitation measures after left-sided paralysis is the normalization of motor activity. The main way to achieve this is physical therapy. Exercises are prescribed individually for each specific case by a physical therapy doctor. As a rule, the complex includes flexion-extension movements of the limbs, joint rotations, and stretching.
Lack of sensitivity in the hands after a stroke - how does this happen?
Initially, before restoring a limb after apoplexy, it is necessary to understand the mechanism of development of paralysis. A stroke is a sudden and sometimes long-term disruption of blood flow in the vessels of the brain (in a certain area). It is difficult to predict which hemisphere it will be and which part of it. In turn, impaired blood circulation in the brain is formed either as a result of rupture of an artery or as a result of its thrombosis. As a result, neurons (aka cells) of the brain, along with blood and red blood cells, do not receive enough nutrition, and therefore oxygen. At this moment their death begins. Brain cells responsible for the mobility of the upper and/or lower extremities, the mobility of facial muscles, the functioning of sensory organs, etc. can die.
Important: a less favorable prognosis for recovery in patients with paralysis of the left side of the body, since in this case the right hemisphere of the brain is affected. With this pathology, the patient’s speech is not impaired, which complicates the initial diagnosis, and therefore takes away the patient’s precious time. The longer the patient does not receive first aid, the greater the consequences will be, and the more difficult the recovery will be. Therefore, if a patient’s left arm does not work after a stroke, then recovery should be more persistent and lengthy.
Causes of upper limb paralysis
Partial or complete paralysis of the upper limbs in a patient occurs against the background of inflammatory processes in the area of the left hemisphere of the brain, frontal lobe or cerebellum. They are responsible for high-quality motor activity of the limbs. Moreover, the patient may experience both complete immobility of the limbs and partial disturbances in the form of tremor, lack of response to external stimuli, and partial hypotonicity of the arm muscles.
Doctors distinguish two types of paralysis:
- Central. It is formed against the background of a malfunction of the entire nervous system after a stroke.
- Peripheral. Here only some nerve endings are affected.
Important: the recovery period for a patient with paralysis of the arms can take up to 1.5–2 months. However, the result is worth it.
Types of paralysis
Before you begin rehabilitation therapy and exercises for the hands and fingers for a stroke, you should be prepared for the fact that rehabilitation for older people is somewhat more difficult. The fact is that side effects of limb paralysis are also decreased muscle tone, bedsores, and muscle paresis. All this will have to be dealt with comprehensively. However, doctors advise starting to work with the patient’s arm literally on days 2–3 in order to avoid additional thrombosis in insensitive limbs.
When the left side of the body is paralyzed, the patient experiences the following types of numbness and decreased sensitivity:
- Hepaesthesia. Characterized by decreased sensitivity of the entire left side of the body.
- Hemiplegia. Paralysis of the left leg and arm. Sometimes the facial muscles are affected.
- Hemianopsia. Decreased vision or complete loss of vision.
Important: left-sided paralysis is observed in patients with stroke more often than right-sided paralysis.
When the right side of the body is paralyzed, the patient experiences the following types of paralysis:
- Synkinesis. Spontaneous twitching and movements of a paralyzed arm or leg.
- Motor aphasia. Speech disorder, complete or partial.
- Paralysis of facial nerves and muscles.
- Movement coordination disorders.
- Difficulties in logical thinking, writing and reading, memory disorders.
Diet food
For any type of stroke, it is recommended to follow a diet. This will reduce lipid levels in the body and speed up recovery. In addition, the diet reduces weight, which speeds up the process of returning to normal range of motion during paralysis. It is necessary to prepare boiled or steamed meat, fish, and lean poultry. Enrich the table with vegetables and fruits - raw or baked, low-fat dairy products. Porridge and greens are healthy. Coffee, strong tea, carbonated water, fried, sour and salty foods should be removed as much as possible. Avoid alcohol completely.
Treatment
When a person has apoplexy, the transmission of nerve impulses is disrupted. The main task of rehabilitation measures is to restore the hand’s ability to receive these impulses and send them back to the brain. To do this, it is necessary to restore blood circulation in the hand and metabolism in its cells. It is for this purpose that special massages, gymnastic exercises and exercise equipment for the arm after a stroke are provided.
Advice: all manipulations during a patient’s recovery after a stroke must be consistent and systematic. In this case, it is advisable to carry out the entire complex of therapy at a temperature that is comfortable for the patient, but not in a hot room, but in a slightly cool room. And all exercises that relieve muscle spasms should be done only while exhaling.
Therapeutic actions
When prescribing drug therapy to a patient after an apoplexy, the following drugs are prescribed to restore the body:
- "Lioresal" (aka "Baclofen"). The drug actively inhibits the transmission of nerve impulses that lead to contraction of the arm muscles. As a result, muscle tone subsides, and the muscles are ready to receive a massage. The pain subsides.
- "Tizanidine." The drug has a similar effect to the first one, eliminates pain, but the effect of its use lasts much less. Therefore, most often “Tizanidine” is used to relieve symptoms, but not for quality treatment.
- Klonopin or Valium. They also actively reduce muscle spasticity.
- Phenol. Neutralizes muscle spasms.
- Botox injections. Also works against spasm. Injections are given into the spine or arm muscle.